Clinical Assessment of Flexible and Non-Metal Clasp Dentures: A Systematic Review
Abstract
1. Introduction
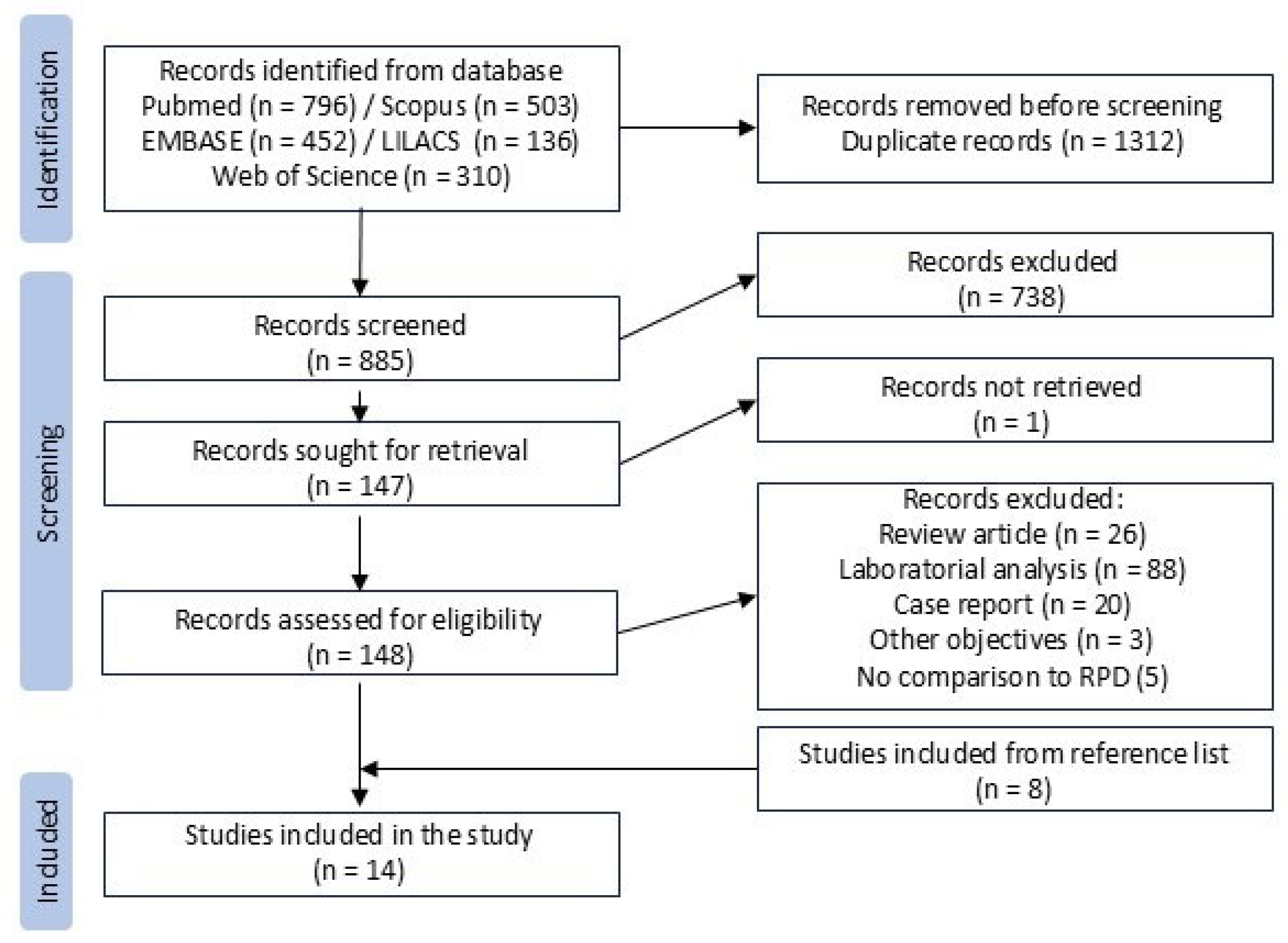
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Data Collection Process
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| RPD | Removable Partial Denture |
| NMCD | Non-Metal Clasp Denture |
| PEEK | Polyetheretherketone |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROSPERO | International Prospective Register of Systematic Reviews |
| PICO | Population, Intervention, Comparator, and Outcomes |
| CT | Clinical Trial |
| NS | Not Specified |
| SDA | Shortened Dental Arch |
| CoCr | Cobalt–Chromium Alloy |
| VAS | Visual Analog Scale |
| OHRQoL | Oral Health-Related Quality of Life |
| OHIP | Oral Health Impact Profile |
| IQR | Interquartile Range |
| s.d. | Standard Deviation |
References
- Mendoza-Carrasco, I.; Hotta, J.; Sugio, C.Y.C.; Procópio, A.L.F.; Urban, V.M.; Mosquim, V.; Foratori-Junior, G.A.; Soares, S.; Neppelenbroek, K.H. Nonmetal clasp dentures: What is the evidence about their use? J. Indian Prosthodont. Soc. 2020, 20, 278. [Google Scholar] [CrossRef]
- Pun, D.K.; Waliszewski, M.P.; Waliszewski, K.J.; Berzins, D. Survey of partial removable dental prosthesis (partial RDP) types in a distinct patient population. J. Prosthet. Dent. 2011, 106, 48–56. [Google Scholar] [CrossRef]
- Hill, E.E.; Rubel, B.; Smith, J.B. Flexible removable partial dentures: A basic overview. Gen. Dent. 2014, 62, 32–36. [Google Scholar]
- Fueki, K.; Ohkubo, C.; Yatabe, M.; Arakawa, I.; Arita, M.; Ino, S.; Kanamori, T.; Kawai, Y.; Kawara, M.; Komiyama, O.; et al. Clinical application of removable partial dentures using thermoplastic resin—Part I: Definition and indication of non-metal clasp dentures. J. Prosthodont. Res. 2014, 58, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Benso, B.; Kovalik, A.C.; Jorge, J.H.; Campanha, N.H. Failures in the rehabilitation treatment with removable partial dentures. Acta Odontol. Scand. 2013, 71, 1351–1355. [Google Scholar] [CrossRef] [PubMed]
- Wadachi, J.; Sato, M.; Igarashi, Y. Evaluation of the rigidity of dentures made of injection-molded materials. Dent. Mater. J. 2013, 32, 508–511. [Google Scholar] [CrossRef]
- Stafford, G.D.; Huggett, R.; MacGregor, A.R.; Graham, J. The use of nylon as a denture-base material. J. Dent. 1986, 14, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Wieckiewicz, M.; Opitz, V.; Richter, G.; Boening, K.W. Physical properties of polyamide-12 versus PMMA denture base material. BioMed Res. Int. 2014, 2014, 150298. [Google Scholar] [CrossRef]
- Ben-Ur, Z.; Matalon, S.; Aviv, I.; Cardash, H.S. Rigidity of major connectors when subjected to bending and torsion forces. J. Prosthet. Dent. 1989, 62, 557–562. [Google Scholar] [CrossRef]
- Fueki, K. Non-metal clasp dentures: More evidence is needed for optimal clinical application. J. Prosthodont. Res. 2016, 60, 227–228. [Google Scholar] [CrossRef]
- Ito, M.; Wee, A.G.; Miyamoto, T.; Kawai, Y. The combination of a nylon and traditional partial removable dental prosthesis for improved esthetics: A clinical report. J. Prosthet. Dent. 2013, 109, 5–8. [Google Scholar] [CrossRef] [PubMed]
- Saad, E.; Harby, N.; Baraka, O. Clinical and Radiographic Comparison between Acetal Resin and Cobalt-Chromium Partial Dentures in Kennedy’s Class I Situations. J. Dent. Med. Sci. 2021, 20, 20–25. [Google Scholar]
- Khurshid, Z.; Nedumgottil, B.M.; Ali, R.M.M.; Bencharit, S.; Najeeb, S. Insufficient evidence to ascertain the long-term survival of PEEK dental prostheses: A systematic review of clinical studies. Polymers 2022, 14, 2441. [Google Scholar] [CrossRef]
- Lo Russo, L.; Chochlidakis, K.; Caradonna, G.; Molinelli, F.; Guida, L.; Ercoli, C. Removable partial dentures with polyetheretherketone framework: The influence on residual ridge stability. J. Prosthodont. 2022, 31, 333–340. [Google Scholar] [CrossRef]
- Kim, J.H.; Choe, H.C.; Son, M.K. Evaluation of adhesion of reline resins to the thermoplastic denture base resin for non-metal clasp denture. Dent. Mater. J. 2014, 33, 32–38. [Google Scholar] [CrossRef][Green Version]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Yoon Jm Liu, Y.; Sun, Y.; Ye, H.; Zhou, Y. Clinical evaluation of a one-piece polyetheretherketone removable partial denture fabricated using a novel digital workflow: A self-controlled clinical trial. J. Prosthodont. 2024, 33, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Fueki, K.; Inamochi, Y.; Yoshida-Kohno, E.; Wakabayashi, N. Short-term effect of thermoplastic resin removable partial dentures on periodontal health: A randomized cross-over trial. J. Prosthodont. Res. 2022, 66, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Fueki, K.; Inamochi, Y.; Yoshida-Kohno, E.; Wakabayashi, N. Cost-effectiveness analysis of prosthetic treatment with thermoplastic resin removable partial dentures. J. Prosthodont. Res. 2021, 65, 52–55. [Google Scholar] [CrossRef]
- Nakai, N.; Kurogi, T.; Murata, H. Oral health–related quality of life of conventional removable partial dentures, unilateral nonmetal clasp dentures, and shortened dental arch with 2-or 3-tooth unilateral distal extension tooth loss in the mandible: A randomized, crossover, clinical trial. J. Prosthet. Dent. 2024, 131, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Koli, D.K.; Jain, V.; Nanda, A. Stress distribution and patient satisfaction in flexible and cast metal removable partial dentures: Finite element analysis and randomized pilot study. J. Oral Biol. Craniofacial Res. 2021, 11, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Vozza, I.; Manzon, L.; Passarelli, P.C.; Pranno, N.; Poli, O.; Grippaudo, C. The effects of wearing a removable-partial-denture on the bite forces: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 11401. [Google Scholar] [CrossRef] [PubMed]
- Sadek, S.A.; Elawady, D. Impact of removable partial denture type on patient satisfaction and abutment survival rate-RCT. Maced. J. Med. Sci. 2019, 7, 2513. [Google Scholar] [CrossRef]
- Manzon, L.; Fratto, G.; Poli, O.; Infusino, E. Patient and clinical evaluation of traditional metal and polyamide removable partial dentures in an elderly cohort. J. Prosthodont. 2019, 28, 868–875. [Google Scholar] [CrossRef]
- Fueki, K.; Yoshida-Kohno, E.; Inamochi, Y.; Wakabayashi, N. Patient satisfaction and preference with thermoplastic resin removable partial dentures: A randomised cross-over trial. J. Prosthodont. Res. 2019, 64, 20–25. [Google Scholar] [CrossRef]
- Aljabri, M.K.; Ibrahim, T.O.; Sharka, R.M. Removable partial dentures: Patient satisfaction and complaints in Makkah City, KSA. J. Taibah Univ. Med. Sci. 2017, 12, 561–564. [Google Scholar] [CrossRef]
- Fueki, K.; Yoshida-Kohno, E.; Wakabayashi, N. Oral health-related quality of life in patients with non-metal clasp dentures: A randomised cross-over trial. J. Oral Rehabil. 2017, 44, 405–413. [Google Scholar] [CrossRef]
- Hundal, M.; Madan, R. Comparative clinical evaluation of removable partial dentures made of two different materials in Kennedy Applegate class II partially edentulous situation. Med. J. Armed Forces India 2015, 71, S306–S312. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, T.; Baraka, O.A.; Badawy, M.M. Comparison between Acetal Resin and Cobalt-chromium Removable Partial Denture Clasps: Effect on Abutment Teeth Supporting Structures. Int. J. Prosthodont. Restor. Dent. 2011, 2, 147–154. [Google Scholar] [CrossRef]
- Fueki, K.; Ohkubo, C.; Yatabe, M.; Arakawa, I.; Arita, M.; Ino, S.; Kanamori, T.; Kawai, Y.; Kawara, M.; Komiyama, O.; et al. Clinical application of removable partial dentures using thermoplastic resin. Part II: Material properties and clinical features of non-metal clasp dentures. J. Prosthodont. Res. 2014, 58, 71–84. [Google Scholar] [CrossRef] [PubMed]
- Montero, J.; Castillo-Oyagüe, R.; Lynch, C.D.; Albaladejo, A.; Castaño, A. Self-perceived changes in oral health-related quality of life after receiving different types of conventional prosthetic treatments: A cohort follow-up study. J. Dent. 2013, 41, 493–503. [Google Scholar] [CrossRef]
- Tumrasvin, W.; Fueki, K.; Ohyama, T. Factors associated with masticatory performance in unilateral distal extension removable partial denture patients. J. Prosthodont. Implant. Esthet. Reconstr. Dent. 2006, 15, 25–31. [Google Scholar] [CrossRef]
- Polyzois, G.; Lagouvardos, P.; Kranjcic, J.; Vojvodic, D. Flexible removable partial denture prosthesis: A survey of dentists’ attitudes and knowledge in Greece and Croatia. Acta Stomatol. Croat. 2015, 49, 316. [Google Scholar] [CrossRef]
- Arda, T.; Arikan, A. An in vitro comparison of retentive force and deformation of acetal resin and cobalt-chromium clasps. J. Prosthet. Dent. 2005, 94, 267–274. [Google Scholar] [CrossRef]
- Macura-Karbownik, A.; Chladek, G.; Żmudzki, J.; Kasperski, J. Chewing efficiency and occlusal forces in PMMA, acetal and polyamide removable partial denture wearers. Acta Bioeng. Biomech. 2016, 18, 137–144. [Google Scholar]
- Akinyamoju, C.A.; Dosumu, O.O.; Taiwo, J.O.; Ogunrinde, T.J.; Akinyamoju, A.O. Oral health-related quality of life: Acrylic versus flexible partial dentures. Ghana Med. J. 2019, 53, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Akinyamoju, C.A.; Ogunrinde, T.J.; Taiwo, J.O.; Dosumu, O.O. Comparison of patient satisfaction with acrylic and flexible partial dentures. Niger. Postgrad. Med. J. 2017, 24, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]

| Study (Authors and Year) | Type of Study | Patients (n) | Age (Mean/Range) | Kennedy’s Classification | Comparison Groups |
|---|---|---|---|---|---|
| Yoon et al., 2024 [18] | Crossover CT 1 | 15 | 29–81 | Class I, II, and III | RPD 2 × NMCD 3 |
| Fueki et al., 2022 [19] | Crossover CT | 24 | 67.3 ± 7.6 | Class I, II, and III | RPD × NMCD |
| Fueki et al., 2021 [20] | Crossover CT | 24 | 67.3 ± 7.6 | Class III | RPD × NMCD |
| Nakai et al., 2024 [21] | Crossover CT | 24 | 59.0 | Class II | RPD × NMCD |
| Kumar et al., 2021 [22] | Parallel CT | 22 | 42.5 ± 7.5 | Class I | RPD × Flexible |
| Saad et al., 2021 [12] | Parallel CT | 14 | NS 4 | Class I | RPD × Flexible |
| Vozza et al., 2021 [23] | Parallel CT | 120 | >65 | Class I | RPD × Flexible |
| Sadek & Elawady, 2019 [24] | Parallel CT | 42 | 45–60 | Class II mod. 1 | RPD × Flexible |
| Manzon et al., 2019 [25] | Retrospective | 120 | 73 | Class I/II × III/IV | RPD × Flexible |
| Fueki et al., 2019 [26] | Crossover CT | 24 | 67.3 ± 7.6 | Class I, II, and III | RPD × NMCD |
| Aljabri et al., 2017 [27] | Retrospective | 60 | 51.2 | NS | RPD × Flexible |
| Fueki et al., 2017 [28] | Crossover CT | 24 | 67.3 ± 7.6 | Class I, II, and III | RPD × NMCD |
| Hundal & Madan, 2015 [29] | Parallel CT | 30 | 25–45 | Class II | RPD × Flexible |
| Mohamed et al., 2011 [30] | Parallel CT | 20 | NS | Class III mod. I | RPD × NMCD |
| Authors and Year | RPD Group | NMCD Group | Flexible Group | |
|---|---|---|---|---|
| Framework/Clasp | Framework | Clasp | ||
| Yoon et al., 2024 [18] | CoCr 1 | PEEK 2 | PEEK | × |
| Fueki et al., 2022 [19] | CoCr | CoCr | Polyester | × |
| Fueki et al., 2021 [20] | CoCr | CoCr | Polyester | × |
| Nakai et al., 2024 [21] | CoCr | CoCr | Polyester | |
| Kumar et al., 2021 [22] | CoCr | × | × | Polyacetal |
| Saad et al., 2021 [12] | CoCr | × | × | Polyacetal |
| Vozza et al., 2021 [23] | CoCr | × | × | Polyamide |
| Sadek & Elawady, 2019 [24] | CoCr | × | × | Polyamide |
| Manzon et al., 2019 [25] | CoCr | × | × | Polyamide |
| Fueki et al., 2019 [26] | CoCr | CoCr | Polyester | × |
| Aljabri et al., 2017 [27] | CoCr | × | × | Polyamide |
| Fueki et al., 2017 [28] | CoCr | CoCr | Polyester | × |
| Hundal & Madan, 2015 [29] | CoCr | × | × | Polyamide |
| Mohamed et al., 2011 [30] | CoCr | CoCr | Polyacetal | × |
| Authors and Year | Follow-Up (Months) | Groups | Redness of the Mucosa Surrounding Abutment Teeth | Plaque Index | Gingival Index | Probing Pocket Depth | Tooth Mobility | Abutment Bone Loss | Abutment Teeth Health |
|---|---|---|---|---|---|---|---|---|---|
| NMCD | |||||||||
| Fueki et al., 2022 [19] | 3 | RPD | × | 22.4 ± 28.5 | 8.3 ± 13.1 | 1.7 ± 0.4 | 6.3 ± 22.4 | × | × |
| NMCD | × | 24.0 ± 24.4 | 9.9 ± 14.3 | 1.8 ± 0.3 | 4.2 ± 14.1 | × | × | ||
| Mohamed et al., 2011 [30] | 12 | RPD | × | × | × | × | × | 0.6 ± 0.2 | × |
| NMCD | × | × | × | × | × | 0.4 ± 0.1 | × | ||
| Flexible Dentures | |||||||||
| Saad et al., 2021 [12] | 12 | RPD | × | × | 2.5 ± 0.5 | 4.1± 0.7 | × | 0.9 ± 0.1 | × |
| Flexible | × | × | 1.2 ± 0.7 | 2.7 ±0.4 | × | 0.7 ± 0.1 | × | ||
| Manzon et al., 2019 [25] | 12 | RPD Class I/II | 35% | 35% | × | × | × | × | 95% |
| Flexible Class I/II | 65% | 65% | × | × | × | × | 85% | ||
| 12 | RPD Class III/IV | 40% | 40% | × | × | × | × | 100% | |
| Flexible Class III/IV | 60% | 60% | × | × | × | × | 95% | ||
| Sadek & Elawady, 2019 [24] | 24 | RPD | × | × | × | × | × | × | 71.4% |
| Flexible | × | × | × | × | × | × | 100% | ||
| Hundal & Madan, 2015 [29] | 6 | RPD | 0% | × | × | × | × | × | × |
| Flexible | 0% | × | × | × | × | × | × |
| Authors and Year | Evaluation Tool | Kennedy’s Classification | RPD Prosthesis | NMCD/Flexible Prosthesis |
|---|---|---|---|---|
| Maximum Bite Force | ||||
| Vozza et al., 2021 [23] | Digital dynamometer | Class I in one arch | 22 kg | 15 kg |
| Class I in both arches | 18 kg | 11 kg | ||
| Chewing Ability Satisfaction | ||||
| Yoon et al., 2024 [18] | VAS 1 | Classes I, II, and III | 80.8 ± 2.6 | 82.2 ± 3.2 |
| Manzon et al., 2019 [25] | Questionnaire | Classes I and II | 4 (20%) | 6 (30%) |
| Classes III and IV | 2 (10%) | 2 (10%) | ||
| Discomfort/Pain During Mastication | ||||
| Manzon et al., 2019 [25] | Questionnaire | Classes I and II | 5 (25%) | 11 (55%) |
| Classes III and IV | 3 (15%) | 6 (30%) | ||
| Authors and Year | Kennedy’s Classification | Follow-Up | Methodology/Parameter | Satisfaction | ||
|---|---|---|---|---|---|---|
| RPD | NMCD | Flexible | ||||
| Yoon et al., 2024 [18] | Classes I, II, and III | 1 week | VAS (mean satisfaction score) | 71.5 ± 4.65 | 73.8 ± 3.9 | × |
| Fueki et al., 2021 [20] | Class III | 3 months | OHIP 1-49 [median (IQR 2)] | 28 (31) | 10.5 (11) | × |
| Nakai et al., 2024 [21] | Class II | 2 weeks | OHIP-49 (mean ± s.d.3) | 60.6 ± 28.9 | 42.7 ± 21.2 | × |
| Fueki et al., 2019 [26] | Classes I, II, and III | 3 months | VAS (mean satisfaction score) | 81.0 ± 17.4 | 87.3 ± 15.5 | × |
| Fueki et al., 2017 [28] | Classes I, II, and III | 3 months | OHIP-49 (mean ± s.d.) | 25.7 ± 20.7 | 16.3 ± 17.2 | × |
| Hundal & Madan, 2015 [29] | Class II | 6 months | Questionnaire score [0 to 3 (more satisfied)] | 1.5 ± 0.5 | × | 2.07 ± 0.6 |
| Kumar et al., 2021 [22] | Class I | 12 months | OHIP-14 (mean ± s.d.) | 16.9 ± 3.3 | × | 13.63 ± 2.4 |
| Saad et al., 2021 [12] | Class I | 12 months | Questionnaire score [0 to 3 (more satisfied)] | 1.42 ± 0.53 | × | 2.71 ± 0.48 |
| Manzon et al., 2019 [25] | Classes I and II | 12 months | Questionnaire (prevalence of satisfied answers) | 40% | × | 95% |
| Classes III and IV | 12 months | Questionnaire (prevalence of satisfied answers) | 35% | × | 100% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mendes Senna, P.; Mourão, C.F.; Teixeira Rodrigues, C.R.; Zarranz, L.; Jorge, M.Z.; Romasco, T.; Batista Cordeiro, W.J. Clinical Assessment of Flexible and Non-Metal Clasp Dentures: A Systematic Review. Prosthesis 2025, 7, 91. https://doi.org/10.3390/prosthesis7040091
Mendes Senna P, Mourão CF, Teixeira Rodrigues CR, Zarranz L, Jorge MZ, Romasco T, Batista Cordeiro WJ. Clinical Assessment of Flexible and Non-Metal Clasp Dentures: A Systematic Review. Prosthesis. 2025; 7(4):91. https://doi.org/10.3390/prosthesis7040091
Chicago/Turabian StyleMendes Senna, Plinio, Carlos Fernando Mourão, Carlos Roberto Teixeira Rodrigues, Laila Zarranz, Mônica Zacharias Jorge, Tea Romasco, and Wayne José Batista Cordeiro. 2025. "Clinical Assessment of Flexible and Non-Metal Clasp Dentures: A Systematic Review" Prosthesis 7, no. 4: 91. https://doi.org/10.3390/prosthesis7040091
APA StyleMendes Senna, P., Mourão, C. F., Teixeira Rodrigues, C. R., Zarranz, L., Jorge, M. Z., Romasco, T., & Batista Cordeiro, W. J. (2025). Clinical Assessment of Flexible and Non-Metal Clasp Dentures: A Systematic Review. Prosthesis, 7(4), 91. https://doi.org/10.3390/prosthesis7040091








