Abstract
Background/Objectives: Partial maxillectomy frequently results in severe impairments of oral functions, such as difficulties in chewing, speech, swallowing, and facial appearance. Immediate prosthetic rehabilitation is challenging because soft tissue healing is typically required before impression taking. This study aimed to (1) develop a comprehensive digital workflow for fabricating immediate obturator prostheses using preoperative data and (2) assess their early clinical effectiveness in restoring oral functions after surgery. Methods: In this prospective clinical study, 20 patients undergoing partial maxillectomy from January 2023 to January 2025 were enrolled. A digital workflow combining cone-beam computed tomography (CBCT), intraoral scanning, CAD/CAM design, and 3D metal printing was implemented. Obturator prostheses were digitally designed preoperatively and inserted immediately post-resection. Functional outcomes were postoperatively evaluated after one month using the Obturator Functioning Scale (OFS), which measures functional, speech, esthetic, and psychosocial aspects. Results: The digitally fabricated immediate obturator prostheses were successfully placed intraoperatively in all patients. Most participants reported mild to moderate difficulties, with speech-related issues being the most common, while esthetic concerns were minimal. Masticatory function was satisfactorily restored in 75% of cases, and 60% of patients experienced minimal fluid leakage during swallowing. No significant differences were found between genders. Patients with larger defects tended to report greater functional challenges. Conclusions: The digitally planned immediate obturator prosthesis provides a practical and effective solution for early rehabilitation following partial maxillectomy. This digital workflow reduces patient discomfort, restores key oral functions, and facilitates psychosocial recovery.
1. Introduction
Partial maxillectomy, a frequently performed surgical procedure to treat both benign and malignant tumors of the maxilla, often leads to complex midfacial defects. These defects significantly impair critical oral functions such as mastication, speech articulation, swallowing, and the separation between the nasal and oral cavities, while also affecting facial aesthetics and the patient’s psychological well-being. Several classification systems have been developed to categorize these defects, among which the Brown classification is commonly used [1]. This system classifies maxillary defects based on the following two dimensions: the vertical extent of the resection (ranging from alveolar involvement to orbital exenteration) and the horizontal component (from unilateral to bilateral or anterior involvement). It offers a standardized framework for describing defect severity and is widely applied in both surgical and prosthetic planning. Effective prosthetic rehabilitation through maxillary obturator prostheses has been widely accepted as a standard approach to restore these lost functions and support patient reintegration into society [2]. The degree of functional loss and difficulty with prosthetic adaptation varies among individuals and is influenced by multiple factors. In addition to defect extent, personal attributes such as gender, psychological resilience, and social context may also play roles in a patient’s capacity to adapt to the prosthesis and achieve functional recovery [3].
In conventional workflows, a definitive obturator prosthesis can only be fabricated several months after surgery, once soft tissues have fully healed and stabilized. However, during this interim period—between surgical resection and definitive rehabilitation—patients still require a transitional obturator to regain basic oral functions and maintain the contour of soft tissues. This transitional prosthesis plays a crucial role in restoring mastication, speech, and swallowing functions, while also supporting facial structures and reducing the risk of tissue collapse or scar contracture. The fabrication of this interim prosthesis traditionally relies on taking an impression shortly after surgery. Yet, this step presents significant clinical challenges, such as the presence of exposed bone and unhealed soft tissue often resulting in pain, bleeding, and poor patient cooperation, leading to a compromised impression accuracy. Additionally, the subsequent laboratory procedures typically delay prosthesis delivery for one or more days, prolonging the time that patients remain without functional rehabilitation [4]. During this early postoperative window, many patients experience considerable discomfort, impaired oral function, and psychosocial distress, all of which negatively impact recovery and quality of life [5].
In the past decade, digital technologies have rapidly transformed the landscape of maxillofacial prosthodontics, offering innovative solutions to these challenges. Advanced digital workflows, including three-dimensional imaging, computer-aided design/computer-aided manufacturing (CAD/CAM), and additive manufacturing, are being applied to obturator design and production [4,6,7,8,9]. Today, intraoral scanners and cone-beam computed tomography (CBCT) can capture the detailed geometry of the maxillectomy defect, and specialized CAD software is used to virtually design obturator prostheses that precisely fit a patient’s anatomy [10,11,12]. These digitally planned immediate obturators can be inserted intraoperatively, restoring essential functions and soft-tissue support at the earliest possible time point [13]. In fact, a 2024 systematic review found that obturators fabricated with digital techniques were associated with a shorter working time and higher patient satisfaction than those made by traditional methods [4].
While these digital innovations are highly encouraging, current challenges prevent them from being universally implemented in maxillofacial prosthetic practice. One practical hurdle is that not all clinical scenarios or centers are readily amenable to a fully digital workflow. Furthermore, access to the necessary digital infrastructure such as scanners, software, 3D printers, and expertise may be limited in some settings, slowing the adoption of all-digital techniques. As a result, the use of digital workflows in obturator fabrication has, so far, often been partial—for example, employing digital design but conventional impressions, or vice versa.
Several case reports and technical papers have illustrated the feasibility of digital workflows in immediate obturator fabrication [14,15]. These approaches have shown a promising accuracy, improved prosthesis fit, and reduced need for postoperative adjustments. However, most reports remain technical in nature or limited to individual cases. To date, few clinical studies have systematically evaluated the functional and patient-centered outcomes of digitally planned obturators inserted immediately following craniofacial surgery. Furthermore, there is limited evidence on patient-centered outcomes—including the functional performance, comfort, and psychosocial well-being of such digitally produced prostheses in larger patient populations [15].
This study was designed with the following two main objectives: (1) to establish a digital workflow for designing immediate obturator prostheses based on preoperative planning and (2) to evaluate the early clinical outcomes of these prostheses in restoring oral function, speech, esthetics, and social reintegration following partial maxillectomy.
2. Materials and Methods
2.1. Study Design
This was a prospective clinical study conducted at the Department of Prosthodontics, Hanoi Medical University and the National Hospital of Odonto-Stomatology, Hanoi, Vietnam, from January 2023 to January 2025. Ethical approval was obtained from the Institutional Review Board for Ethics in Biomedical Research at Hanoi Medical University (No. 1557), and informed consent was signed by all participating patients.
2.2. Patient Selection
This prospective clinical study enrolled patients who underwent partial maxillectomy for benign or malignant maxillary tumors between January 2023 and January 2025. The inclusion criteria were patients aged between 18 and 70 years with sufficient remaining dentition—two posterior teeth and two anterior teeth on the non-defect side—to provide stable support for the obturator prosthesis.
The exclusion criteria included severe systemic diseases contraindicating surgery, previous maxillary reconstruction or prosthetic rehabilitation, significant cognitive impairment, and inability to comply with postoperative follow-up.
2.3. Digital Workflow
The digital workflow applied in this study was developed by the authors based on their clinical experience in maxillofacial prosthetics.
2.3.1. Data Collection
The patients underwent maxillofacial cone-beam computed tomography (CBCT) or computed tomography (CT) scanning (64 slices or more) with a wide field of view capturing the entire craniofacial region from the forehead to below the chin, with data exported as DICOM files.
Teeth impressions, including upper and lower dental arches and bite registrations in maximum intercuspation, were digitally captured using a Trios 3 intraoral scanner (3Shape, Copenhagen, Denmark), with files exported in STL format. Scans were performed before and after tooth preparation (Figure 1).
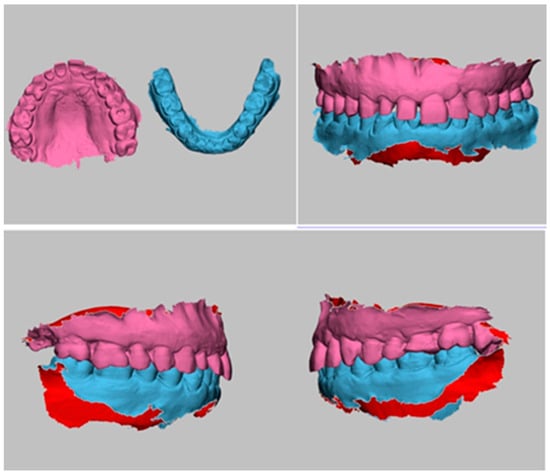
Figure 1.
Digital 3D models of maxilla, mandible, and occlusal bite registration.
2.3.2. Segmentation
CT scan data in DICOM format were segmented to isolate the skull, upper jaw, and lower jaw structures, removing unnecessary anatomical regions and converting the segmented data into 3D STL format using Materialise Mimics software version 23.0 (Materialise NV, Leuven, Belgium) (Figure 2).
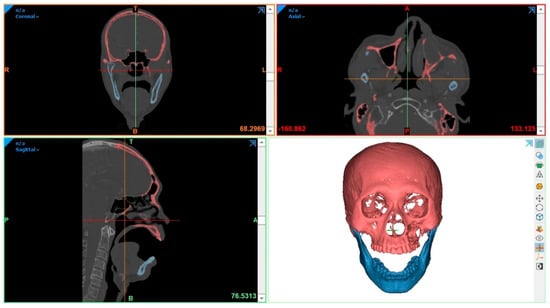
Figure 2.
Segmentation of CT scan data.
2.3.3. Superimposition
Subsequently, these 3D skull–jaw files were precisely overlapped and aligned with intraoral scan data based on identifiable dental landmarks, ensuring an accurate anatomical correlation (Figure 3).
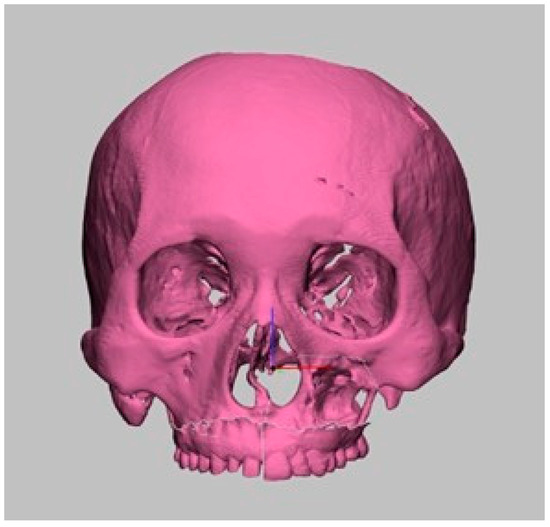
Figure 3.
Superimposition of CT-derived and intraoral scan data.
2.3.4. Design of Bone Cutting Guide
Surgical bone cutting guides were digitally designed according to the preoperative virtual surgical plan using Materialise 3-matic software version 16 (Materialise NV, Leuven, Belgium) (Figure 4).
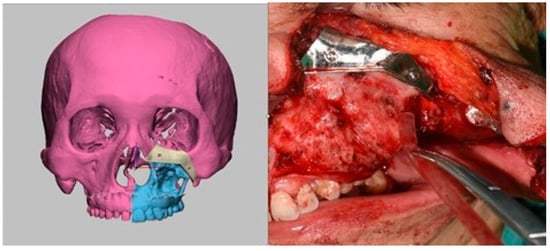
Figure 4.
Digital design and intraoperative use of bone cutting guide.
2.3.5. Obturator Prosthesis Design
The obturator prosthesis was digitally designed in two stages based on the virtually simulated maxillary defect. First, two metal retentive copings were planned using Exocad DentalCAD 3.2 (exocad GmbH, Darmstadt, Germany) software to fit over the prepared abutment teeth, which had been reduced prior to design. These copings featured projecting extensions toward the defect side, serving as a keying structure to provide both mechanical retention and precise alignment with the removable obturator segment (left image, Figure 5). Next, the framework base was designed in 3Shape Dental System (3Shape A/S, Copenhagen, Denmark), incorporating coverage of the palatal vault and perforations along the defect side to facilitate acrylic retention and reduce weight (right image, Figure 5). This digital workflow ensured precise adaptation to the remaining dentition and allowed for subsequent wax-up and tooth arrangement on the printed model.
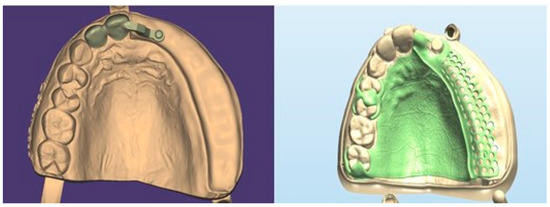
Figure 5.
Obturator prosthesis design.
2.3.6. Prosthesis Fabrication
The metal framework of the obturator prosthesis and the retentive copings were fabricated using 3D metal printing (Riton Dual-150, Guangzhou Riton Additive Technology Co., Ltd., Guangzhou, China) to ensure rigidity, precise adaptation, and long-term intraoral durability. The copings were subsequently layered with ceramic to anatomically replicate the prepared abutment teeth and provide seamless esthetic integration. After ceramic build-up, the metal base was seated on the diagnostic model and locked onto the coping extensions to verify accurate fit and alignment. The defect-engaging extension was then sculpted in wax, and artificial teeth were manually arranged according to the occlusal scheme. The complete assembly was processed using conventional heat-cured acrylic resin. The final steps included polishing and quality control to ensure that the prosthesis was clinically ready for immediate intraoperative insertion (Figure 6).

Figure 6.
Fabrication process of the immediate obturator prosthesis showing metal framework assembly, wax-up, tooth arrangement (a–c), and final acrylic processing (d,e).
2.4. Surgical Procedure and Immediate Prosthesis Insertion
Most resections were performed via the Weber–Ferguson approach, which provides wide access to the maxilla and orbital floor, particularly for tumors extending superiorly to the infraorbital nerve or involving the orbit. All procedures were conducted under general anesthesia and guided by preoperative virtual planning to ensure accurate oncologic margins. When feasible, the infraorbital rim and adjacent soft tissues were preserved. Soft tissue closure was achieved using local mucosal advancement flaps. No cases required free flap reconstruction. Immediate obturator insertion was performed intraoperatively in all patients. Two cases (classified as IIb and IIc) were approached via a transoral route. Prosthesis fit was evaluated clinically for the accuracy of adaptation and retention. Necessary minor adjustments were recorded and performed intraoperatively (Figure 7). These included relieving pressure spots, trimming overextended flanges, and, in some cases, applying auto-polymerizing acrylic resin to improve peripheral adaptation and patient comfort during the early healing phase.
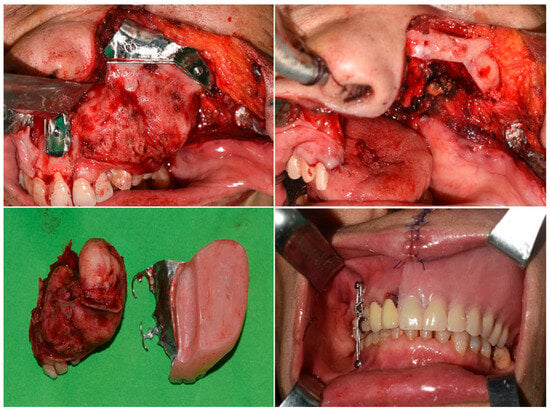
Figure 7.
Surgical procedure and immediate prosthesis insertion.
2.5. Postoperative Evaluations
One month after the operation, allowing sufficient time for patients to adapt, all patients were recalled to evaluate the immediate obturator insertion. A subjective evaluation of obturator performance was conducted using the Obturator Functioning Scale (OFS) [3]. This scale consists of 15 items, each assessing the degree of difficulty experienced by the patient in specific functional, speech, esthetic, and psychosocial domains.
Each item was rated on a 5-point Likert scale, where a score of 1 indicated “not at all difficult”, 2 indicated “slightly difficult”, 3 indicated “moderately difficult”, 4 corresponded to “very difficult”, and 5 reflected “extremely difficult”. For analysis, responses were further dichotomized into the following two categories: scores of 1–2 were considered to be indicative of adequate function (no perceived difficulty), while scores of 3–5 were interpreted as reflecting functional impairment (perceived difficulty).
2.6. Statistical Analysis
Data was analyzed using Python (version 3.11) with the SciPy library (version 1.11.1; Virtanen et al., 2020 [16]). Descriptive statistics were calculated for demographic variables and overall functional scores. To assess gender-related differences in patient-reported outcomes, the Mann–Whitney U test was applied to each item of the Obturator Functioning Scale. Due to limited sample sizes in the IIc and IId subgroups, no statistical comparisons were performed across Brown classification categories. A p-value of less than 0.05 was considered as statistically significant.
3. Results
3.1. Demographic Characteristics
A total of 20 patients were enrolled in the study to assess the clinical outcomes of immediate obturator prostheses following partial maxillectomy. Baseline demographic and clinical characteristics are summarized in Table 1. The surgical defects were categorized according to the Brown classification system, which defines maxillary defects based on their vertical extent and horizontal spread [1].

Table 1.
Demographic characteristics for patients.
3.2. Obturator Functioning Scale Outcomes
The mean OFS scores indicated that patients generally experienced mild to moderate difficulties across various functional domains. Specifically, higher difficulty scores were observed in speech-related items, such as “speech is nasal” and “difficulty pronouncing words”, while lower scores were noted in esthetic concerns like “clasps on front teeth are noticeable”. (Table 2).

Table 2.
Patient-reported functional difficulties based on the Obturator Functioning Scale (OFS).
Patients were grouped based on the Brown classification, as follows: IIb (n = 17), IIc (n = 2), and IId (n = 1). Due to the small sample sizes in groups IIc and IId, statistical comparisons were limited; however, descriptive trends suggested greater functional difficulty in patients with more extensive defects.
Furthermore, no statistically significant differences were found between male and female patients across any of the 15 OFS items (all p > 0.05), indicating that gender did not significantly influence patient-reported functional outcomes in this cohort.
4. Discussion
4.1. Digital Protocol
The first objective of this study was to establish a digital workflow for designing immediate obturator prostheses based on preoperative planning. The proposed workflow combines virtual surgical planning using CT scanning, intraoral scanning, CAD design, and the 3D metal printing of both the denture base and retentive copings. By completing the design and fabrication prior to surgery, this protocol enables immediate intraoperative insertion of a transitional prosthesis, eliminating the need for early postoperative impressions and minimizing patient discomfort during the critical initial phase of healing. Previous studies have introduced various digital strategies for fabricating obturators. Zhao et al. in 2024 [17] proposed a technique for designing interim prostheses using postoperative CBCT data in which radiopaque iodoform gauze was used to define the defect shape. Although this approach allows for relatively early delivery of the prosthesis, it does not represent immediate obturation in the strict sense, as both design and fabrication are conducted after resection. In contrast, Hu et al. developed a digitally intensive workflow for definitive obturators, incorporating facebow registration, virtual articulators, esthetic framework contouring, 3D-printed metal substructures, and milled monolithic PMMA bases [15].
Milled PMMA, though superior in surface quality and dimensional stability, is appropriate for definitive prostheses where tissue conditions are stable and high esthetic refinement is required. The current study adopted a different strategy, focusing on transitional obturation during the early postoperative phase, when tissue contours are still evolving. While the underlying framework was produced using 3D metal printing to ensure rigidity and a precise fit, the overlying components were fabricated using heat-cured acrylic resin. This material was chosen over milled PMMA due to its clinical flexibility, and heat-cured acrylic resin is particularly suitable for transitional prostheses, as it allows for intraoperative adjustments, adapts to soft tissue changes during healing, and is easier to repair or modify chairside.
While the digital workflow demonstrated feasibility and clinical benefits in this study, several potential limitations should be acknowledged. The implementation of such workflows requires access to advanced imaging equipment, design software, and metal 3D printing technologies, which may not be readily available in all clinical settings. Additionally, a certain level of technical expertise and training is needed to effectively perform virtual planning and prosthesis design. These factors may limit the generalizability of the workflow, especially in low-resource environments or institutions with limited digital infrastructure.
4.2. Early Functional Outcomes
The second goal of this study was to evaluate the effectiveness of immediate obturator prostheses across three domains, based on self-reported responses from patients. The first domain was masticatory function. Mastication is typically compromised after maxillectomy due to the loss of the palatal vault, dental support, and anchorage for the tongue. The placement of an obturator reestablishes a functional palatal surface, enabling the tongue to exert pressure on the prosthetic palate during chewing. Objective assessments in previous studies have demonstrated significant improvement in chewing efficiency with obturators, with 96% of patients achieving satisfactory mastication [18]. In our study, 75% of patients reported a good masticatory ability. Immediate obturators also help to prevent fluid leakage and nasal regurgitation, enabling patients to resume oral intake earlier. One previous study reported that 50% of patients experienced no or minimal leakage while swallowing [3], while our findings showed a slightly better outcome, with 60% of patients reporting no leakage symptoms. Masticatory performance depends largely on the fitness and stability of the prosthesis. In cases where the obturator is overly heavy or lacks retention, patients may avoid hard foods due to impaired function. In this study, we enhanced retention by using precisely fabricated metal copings on prepared abutment teeth, in combination with custom rests, allowing for accurate repositioning of the tooth-bearing segment and reliable stabilization of the prosthesis.
The second domain involved speech and communication. Speech is often the most noticeably improved function following obturator insertion. Maxillary defects result in hypernasality and unintelligible speech due to oronasal air escape. Obturators restore oral–nasal separation and provide a platform for normal articulation. Dalkiz et al. reported a dramatic improvement in speech intelligibility from approximately 0% pre-obturator to 94% by postoperative day two with an immediate prosthesis [19]. In our study, only 10% of patients reported difficulty in social communication. However, 40% of patients reported noticeable changes in their speech, particularly when speaking on the phone or articulating certain phonemes. This can be attributed to several factors. First, at the one-month postoperative mark, neuromuscular adaptation may still be incomplete. More importantly, in cases where the resection involves the soft palate and uvula—structures that actively elevate and move during speech—rigid obturators cannot replicate their dynamic function. As a result, some degree of speech distortion is inevitable, especially for oral sounds that rely on soft palate mobility to achieve proper resonance and closure.
The third domain was facial esthetics and social reintegration. In addition to functional rehabilitation, obturators play an important role in restoring facial appearance and patient confidence. Maxillary defects may cause midfacial collapse, upper lip retraction, nasal asymmetry, and a visible intraoral void, all of which contribute to social withdrawal. The obturator, particularly when fitted with artificial teeth and a contoured palatal base, helps to restore facial symmetry and soft tissue support. In our study, 90% of patients expressed satisfaction with their facial esthetics. This is consistent with Corsalini et al., who reported 72% satisfaction in their cohort [18]. However, 35% of patients in our study noted upper lip asymmetry, especially in cases where extensive soft tissue or cutaneous resections were required. Nevertheless, most patients achieved a socially acceptable appearance that supported their reintegration into daily life. The majority of patients (80%) indicated successful reintegration into social environments. These findings reflect the critical role of timely and well-adapted prosthetic intervention in supporting psychological recovery.
4.3. Influence of Defect Classification and Gender
In addition to domain-specific findings, this study explored the potential influences of defect severity and patient gender on functional outcomes. Patients were categorized according to the Brown classification system. Although formal statistical comparisons across Brown subgroups were not feasible due to the small number of patients in the IIc and IId categories, descriptive analysis revealed a consistent trend: patients with more extensive defects tended to report higher difficulty scores across multiple domains, including mastication, speech, esthetics, and social reintegration.
Furthermore, statistical analysis using the Mann–Whitney U test showed no significant differences in any Obturator Functioning Scale items between male and female patients (all p > 0.05). However, a descriptive review of the item-wise scores revealed that male patients consistently reported lower difficulty scores than female patients across nearly all functional domains. In contrast to our results, one study noted that female patients reported slightly better quality of life scores than males (65% vs. 64%) [20]. Future studies incorporating qualitative interviews or psychological profiling may help to elucidate these underlying factors.
4.4. Limitations
This study has several limitations. First, the sample size was relatively small, particularly in the Brown IIc and IId subgroups, which limited the ability to perform statistical comparisons across different defect types. The study emphasizes descriptive statistics over inferential conclusions. Trends identified in this study should be interpreted cautiously and used to guide future investigations. Second, the follow-up period was limited to one month postoperatively, which may not fully capture long-term adaptation, functional recovery, or prosthesis-related complications. Third, the study relied solely on patient-reported outcomes using the Obturator Functioning Scale, without incorporating objective functional assessments such as masticatory performance tests or speech intelligibility ratings.
Future studies should aim to include a larger cohort to improve generalizability and provide a more robust dataset, along with extended follow-up periods to evaluate long-term functional outcomes and potential complications. Incorporating objective functional assessments, such as speech intelligibility testing and masticatory efficiency evaluation, would further enhance the understanding of the prosthesis’s clinical impact on patient quality of life. Moreover, future research should explore the integration of artificial intelligence (AI) into the digital workflow for obturator design, as AI has the potential to automate anatomical recognition, optimize prosthesis morphology, and assist in pre-surgical planning, thereby improving fit accuracy, treatment efficiency, and overall rehabilitation outcomes [21,22].
5. Conclusions
Digitally planned immediate obturator prostheses provided effective early rehabilitation following partial maxillectomy, with most patients reporting mild to moderate functional difficulty one month postoperatively. Descriptive trends suggested that patients with larger maxillary defects and female patients may have reported slightly higher levels of perceived difficulty. The digital workflow proved to be feasible, well-tolerated, and beneficial in restoring oral function and supporting psychosocial reintegration.
Author Contributions
Conceptualization, A.T.T., H.T.P., and M.S.T.; methodology, A.T.T., D.T.L., M.T.D., T.T.P., D.M.N., H.T.P., and M.S.T.; validation, A.T.T. and D.M.N.; formal analysis, A.T.T. and D.M.N.; investigation, A.T.T., D.T.L., M.T.D., and T.T.P.; resources, A.T.T. and H.T.P.; data curation, A.T.T. and D.M.N.; writing—original draft preparation, A.T.T. and D.M.N.; writing—review and editing, A.T.T. and D.M.N.; visualization, A.T.T., D.T.L., M.T.D., T.T.P., and D.M.N.; supervision, H.T.P. and M.S.T.; project administration, M.S.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board for Ethics in Biomedical Research at Hanoi Medical University (No. 1557).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Brown, J.S.; Rogers, S.N.; McNally, D.N.; Boyle, M. A modified classification for the maxillectomy defect. Head Neck J. Sci. Spec. Head Neck 2000, 22, 17–26. [Google Scholar] [CrossRef]
- Moreno, M.A.; Skoracki, R.J.; Hanna, E.Y.; Hanasono, M.M. Microvascular free flap reconstruction versus palatal obturation for maxillectomy defects. Head Neck 2010, 32, 860–868. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.M.; Khalifa, N.; Alhajj, M.N. Quality of life and problems associated with obturators of patients with maxillectomies. Head Face Med. 2018, 14, 2. [Google Scholar] [CrossRef] [PubMed]
- Paul, A.; Dhawan, P.; Jain, N. Digital Applications in the Fabrication of Obturators in Maxillectomy Defects: A Systematic Review. Cureus 2024, 16, e70479. [Google Scholar] [CrossRef]
- Chouksey, G.; Gupta, V.; Choure, R.; Pakhare, A.P.; Dev, A.; Kumar, B. Quality of life after prosthodontic rehabilitation in patients with bilateral total maxillectomy due to COVID-19-associated mucormycosis of the maxilla. Arch. Craniofacial Surg. 2024, 25, 285–291. [Google Scholar] [CrossRef]
- Wolfaardt, J.F.; Brecht, L.E.; Taft, R.M.; Grant, G.T. The future of maxillofacial prosthodontics in North America: The role of advanced digital technology and artificial intelligence–A discussion document. J. Prosthet. Dent. 2024, 131, 1253.e1–1253.e34. [Google Scholar] [CrossRef]
- Fernandez, P.K.; Kuscu, E.; Weise, H.; Engel, E.M.; Spintzyk, S. Rapid additive manufacturing of an obturator prosthesis with the use of an intraoral scanner: A dental technique. J. Prosthet. Dent. 2022, 127, 189–193. [Google Scholar] [CrossRef]
- Koyama, S.; Kato, H.; Harata, T.; Sasaki, K. A workflow for fabricating a hollow obturator by using 3D digital technologies. J. Prosthet. Dent. 2020, 123, 648–652. [Google Scholar] [CrossRef]
- Khalaf, K.; Rashad, H.M.A.; Mostafa, T.M.N. Tissue surface adaptation and retention of digital obturator after one year of use. BMC Oral Health 2024, 24, 908. [Google Scholar] [CrossRef]
- Cao, R.; Zhang, S.; Li, L.; Qiu, P.; Xu, H.; Cao, Y. Accuracy of intraoral scanning versus conventional impressions for partial edentulous patients with maxillary defects. Sci. Rep. 2023, 13, 16773. [Google Scholar] [CrossRef]
- Brucoli, M.; Boffano, P.; Pezzana, A.; Corio, C.; Benech, A. The use of optical scanner for the fabrication of maxillary obturator prostheses. Oral Maxillofac. Surg. 2020, 24, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Hattori, M.; Elbashti, M.E.; Sumita, Y.I. Feasibility of Intraoral Scanning for Data Acquisition of Maxillectomy Defects. Int. J. Prosthodont. 2020, 33, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Abdulkarim, L.I.; Alharamlah, F.S.S.; Abubshait, R.M.; Alotaibi, D.A.; Abouonq, A.O. Impact of Digital Workflow Integration on Fixed Prosthodontics: A Review of Advances and Clinical Outcomes. Cureus 2024, 16, e72286. [Google Scholar] [CrossRef] [PubMed]
- Tasopoulos, T.; Chatziemmanouil, D.; Karaiskou, G.; Kouveliotis, G.; Wang, J.; Zoidis, P. Fabrication of a 3D-printed interim obturator prosthesis: A contemporary approach. J. Prosthet. Dent. 2019, 121, 960–963. [Google Scholar] [CrossRef]
- Hu, Y.; Liu, J.; Wu, W.; Wang, Z. Immediate reconstruction of defects after a partial maxillectomy with a digitally planned, prefabricated, 3-dimensionally printed, esthetic obturator prosthesis. J. Prosthet. Dent. 2024, 132, 1330.e1–1330.e7. [Google Scholar] [CrossRef]
- Virtanen, P.; Gommers, R.; Oliphant, T.E.; Haberland, M.; Reddy, T.; Cournapeau, D.; Burovski, E.; Peterson, P.; Weckesser, W.; Bright, J.; et al. SciPy 1.0: Fundamental algorithms for scientific computing in Python. Nat. Methods 2020, 17, 261–272. [Google Scholar] [CrossRef]
- Zhao, R.; Dong, Y.; Liu, N.; Bai, S. A digital workflow for fabricating an interim obturator after partial maxillary resection. J. Prosthet. Dent. 2024, 132, 1070–1074. [Google Scholar] [CrossRef]
- Corsalini, M.; Barile, G.; Catapano, S.; Ciocia, A.; Casorelli, A.; Siciliani, R.; Di Venere, D.; Capodiferro, S. Obturator Prosthesis Rehabilitation after Maxillectomy: Functional and Aesthetical Analysis in 25 Patients. Int. J. Environ. Res. Public Health 2021, 18, 12524. [Google Scholar] [CrossRef]
- Dalkiz, M.; Dalkiz, A.S. The Effect of Immediate Obturator Reconstruction after Radical Maxillary Resections on Speech and other Functions. Dent. J. 2018, 6, 22. [Google Scholar] [CrossRef]
- Depprich, R.; Naujoks, C.; Lind, D.; Ommerborn, M.; Meyer, U.; Kübler, N.R.; Handschel, J. Evaluation of the quality of life of patients with maxillofacial defects after prosthodontic therapy with obturator prostheses. Int. J. Oral Maxillofac. Surg. 2011, 40, 71–79. [Google Scholar] [CrossRef]
- Al Hendi, K.D.; Alyami, M.H.; Alkahtany, M.; Dwivedi, A.; Alsaqour, H.G. Artificial intelligence in prosthodontics. Bioinformation 2024, 20, 238–242. [Google Scholar] [CrossRef]
- Ali, I.E.; Hattori, M.; Sumita, Y.; Wakabayashi, N. Automated design prediction for definitive obturator prostheses: A case-based reasoning study. J. Prosthodont. 2025, 34, 490–499. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).