Abstract
Background/Objectives: The aim of this systematic review was to identify the role of orthodontics in patients undergoing tumor-ablative surgery, in collaboration with maxillofacial prosthodontic rehabilitation in a multidisciplinary fashion. Methods: This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42024582050). The focused question was constructed using the PICO (participant, intervention, comparison, and outcome) approach. A three-stage search was performed in PubMed, Scopus, and Web of Science using Medical Subject Heading (MeSH) terms. To assess the risk of bias, the National Institute of Health (NIH) “Quality Assessment Tool for case series/reports” was used. All data was synthesized qualitatively, according to the Synthesis Without Meta-analysis (SWiM) reporting guideline. Results: The initial search yielded 624 articles, of which 22 met the inclusion criteria after screening and eligibility assessment, with most being single-patient case reports and one case series involving 12 patients. The included studies primarily involved tumors in the mandible (64.5%) and maxilla (32.3%). Orthodontic treatment was initiated at various time points, ranging from one month pre-surgery to 19 years post-surgery, primarily utilizing fixed appliances (77.8%). In some studies, orthodontic appliances were used to enhance the stability of maxillofacial prostheses. The results of this study indicate that orthodontic treatment may facilitate prosthetic rehabilitation by improving conditions prior to prosthetic intervention and increasing the retention of the obturator prosthesis. Conclusions: Orthodontic treatment can enhance maxillofacial prosthetic rehabilitation after tumor-ablative surgery by optimizing jaw growth, improving occlusion, and facilitating prosthetic retention or space creation. Further research is needed to establish treatment guidelines. Orthodontic miniscrews may improve temporary prosthesis retention before final implant placement, when indicated.
1. Introduction
Although head and neck cancer (HNC) mainly occurs in older individuals, a remarkable increase in the number of young patients (<45 diagnosed with head and neck squamous cell carcinoma) has been recently observed worldwide [1,2]. These are predominantly oral and oropharyngeal cancers; their therapeutic approach consists of wide surgical resection and is followed by adjuvant treatment modalities (chemo- and/or radiation therapy).
Tumor-ablative surgery often results in a pronounced intraoral defect that significantly affects function and esthetics, and has a profound effect on quality of life (QOL); therefore, a growing number of younger individuals require multidisciplinary oral rehabilitation to restore facial disfigurement and functional disabilities. Such rehabilitation poses significant challenges due to the destructive nature of many head and neck cancers and the associated resection. Extensive resections often result in a substantial loss of hard and soft intraoral anatomic structures, along with the loss of teeth, leaving large edentulous areas [3]. Additionally, condition-related tooth germ damage during early childhood can lead to the agenesis of one or more teeth [4]. The surgical defects can severely impair speech, swallowing, and mastication, while also causing noticeable differences in appearance [5,6]. Such changes often lead to statistically significantly lower self-esteem, increased risk of clinical depression, and impairment of quality of life [7,8]. Furthermore, if the growing patients have undergone adjuvant radiation therapy, the growth and development of craniofacial structures may be hindered [9].
For the aforementioned reasons, immediate restoration of oral function and esthetic appearance is significantly important. The treatment plan ought to satisfy the patient’s needs, protect the remaining oral structures, and facilitate growth [10]. Achieving these goals often necessitates an interdisciplinary management and team approach that involves an oral and maxillofacial surgeon, a maxillofacial prosthodontist, and an orthodontist [11]. In cases where surgical reconstruction of the defect is not performed, the defect may be restored using a maxillofacial prosthesis supported by the residual teeth, the surrounding oral tissues, and/or, if indicated, dental implants [12,13]. The placement of osseointegrated implants in growing patients should be limited to specific circumstances. Since dental implants behave similarly to ankylosed teeth, their placement is generally deferred until completion of growth [14,15].
Orthodontic treatment in young patients who underwent tumor-ablative surgery may individualize the growth process, establish an improved occlusal relationship, and create the required space for prosthetic rehabilitation [16]. Additionally, orthodontic appliances could assist in the retention of the maxillofacial prostheses, improving their support and stability. In cases where oral tissues provide inadequate support (e.g., partially erupted teeth without engageable undercuts), the prosthesis may lack sufficient retention [17]. This can impair oral function and negatively affect the patient’s psychology during the recovery phase [18].
There are a few case reports examining the contribution of orthodontics toward improving maxillofacial prosthetic rehabilitation in patients undergoing tumor-ablative surgery [11,17,19]. As the average age of these patients decreases, the number of patients requiring such interdisciplinary treatments is rising. However, no systematic review has been conducted on this subject. Hence, the aim of this systematic review is to evaluate the existing literature, identify available studies/reports that refer to the collaboration of orthodontics and maxillofacial prosthodontics in patients with tumor-associated intraoral defects, assess the multidisciplinary treatment outcomes, and attempt to establish treatment guidelines.
2. Materials and Methods
A systematic literature review was performed following the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [20] and was registered in the International Prospective Register of Systematic Reviews (PROSPERO) as CRD42024582050.
2.1. Study Design and Search Strategy
The focused question of this review was constructed according to the PICO (participant, intervention, comparison, and outcome) approach [21] and was the following: “What are the treatment guidelines of combining orthodontics with maxillofacial prosthetic rehabilitation in patients undergoing tumor-ablative surgery?”
P (participants): patients with tumor-associated intraoral defects; I (intervention): oral rehabilitation by means of orthodontic treatment and maxillofacial prosthodontic restoration; C (comparator/control): as this is a review of case reports and case series, no comparator or control was used; O (outcome): (1) Type of orthodontic appliance and timing of orthodontic treatment, relative to the surgical resection and the oncologic therapy; (2) Type of orthodontic appliance and timing of the orthodontic treatment relative to the maxillofacial prosthodontic rehabilitation; (3) Use of orthodontic appliances to accommodate the retention of the maxillofacial prostheses.
A thorough electronic search was performed by two independent reviewers in PubMed, Scopus, and Web of Science databases for articles published up to August 2024. The search strategy with Medical Subject Heading (MeSH) terms used for PubMed is presented in Table 1.

Table 1.
Search Terms used for PubMed.
2.2. Inclusion and Exclusion Criteria
A three-stage screening (titles, abstract, full-text) was executed in duplicate by the two authors (IA and NG) according to the predetermined eligibility criteria. Any disagreement was resolved by discussion and, if necessary, a third reviewer (HV) was consulted. The inclusion criteria concerned patients with tumor-associated oral defects, (1) with or without surgical reconstruction of the defect, (2) who may have undergone other concurrent tumor-related surgical procedures, (3) who may have received adjuvant chemo- or radiation therapy. The exclusion criteria concerned patients with (1) congenital defects, (2) osteonecrosis-related intraoral defects, and (3) orthodontic treatment preceding the surgical resection. Randomized and non-randomized clinical trials, cohort studies, case-control studies, case series, case reports, and reviews published in the English language were included. All other study types were excluded.
2.3. Risk of Bias (Quality) Assessment
The National Institute of Health (NIH) Quality Assessment Tool for case series/reports [22] was employed in duplicate by two calibrated reviewers (IA and NG) independently. This instrument was the most suitable for the type of studies we expect to include, according to the search strategy. The level of agreement between the reviewers for the second and third stages of screening, as well as the quality assessment, was calculated using kappa statistics. All disagreements were solved by reaching a consensus after discussion between the reviewers.
2.4. Data Extraction
The following data was extracted from the full text of the included papers: author name, title, year of publication, type of study, number of patients, patient demographics, medical history, type of surgical resection, adjuvant treatment modalities, type and timing of prosthetic intervention, type and timing of orthodontic intervention, use of orthodontic appliances-means to aid maxillofacial prostheses’ retention, and clinical outcomes. In case of missing data, the authors of the papers were contacted. All data was extracted into prepared electronic tables, in duplicate, and was cross-checked for accuracy.
2.5. Data Synthesis
Due to the heterogeneity of the included studies in terms of study design, time, and duration of the intervention, the reported outcome measures, and the reported methods of outcome evaluation, conducting a meta-analysis of the effect estimates was not considered possible. Therefore, the data was synthesized qualitatively, according to the Synthesis Without Meta-analysis (SWiM) reporting guideline. Hence, the results were synthesized for each expected outcome (type and timing of prosthetic intervention, type and timing of orthodontic intervention, use of orthodontic appliances—means to aid maxillofacial prostheses’ retention) when at least three studies (with different patient samples) reported on them. The data synthesis occurred individually for each expected outcome, and we also tried to account for the time frame. Hence, the summary effect measures could not be determined in advance, but were adapted according to the number of studies reporting on each outcome. The methods of combining individual study data followed the SWiM guideline.
3. Results
3.1. Study Selection
The selection procedure of the studies is demonstrated in Figure 1 as a flow chart. The initial search resulted in 624 articles. After duplicate removal (n = 177), 447 were screened based on title and abstract, and 399 were not relevant for the purpose of this review, so they were rejected. Forty-seven full-text articles were assessed for eligibility. Three studies were excluded because they were focused on congenital defects; 10 studies were excluded due to the absence of orthodontic treatment or tumor-ablative surgeries, and a total of 22 articles were included in this review. All studies except for one [23] were case reports involving a single patient. There was one case series involving 12 patients treated for central giant cell granuloma of the jaws [23]. The selected studies’ quality was evaluated independently and in duplicate utilizing the NIH Quality Assessment Tool for Case Series/Report Studies, and the results are presented in Table 2. Twelve studies (54.5%) were characterized as good, 8 (36.4%) as fair, and only 2 (9.1%) as poor due to incomplete case definitions and results. Detailed information on treatment timing, orthodontic appliances utilized, and the type of prosthetic rehabilitation was often missing.
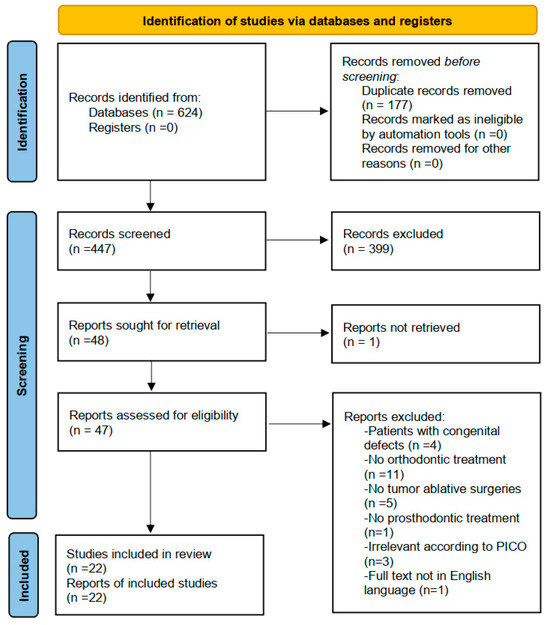
Figure 1.
PRISMA Statement.

Table 2.
Results of the quality evaluation of the included studies using NIH Quality Assessment Tool for Case series/report Studies.
3.2. Study Characteristics
Lesions were located in the maxilla in 10 case reports (32.3%), in the mandible in 20 case reports (64.5%), and only in one case, the defect included the right orbital area (3.2%) [24]. The central giant cell granuloma of the jaws was the most frequently observed tumor, accounting for 13 cases (41.9%). Ameloblastoma was identified in six cases (19.4%), while odontogenic myxoma and melanotic neuroectodermal tumor of infancy (MNTI) were each reported in two studies. A single case was reported for each of the following: mucoepidermoid carcinoma, retinoblastoma, intraosseous venous malformation, Gorlin–Goltz syndrome, peripheral osteoma, fibromatosis tumor, and squamous cell carcinoma. Surgical resection of the tumor was performed in all cases, with adjuvant treatment modalities, such as radio- and chemotherapy, administered in only one case [24]. The key characteristics of each included study are summarized in Table 3.

Table 3.
Key characteristics of the included studies.
3.3. Type and Timing of Orthodontic Treatment Relative to Surgical Resection and Oncologic Therapy
The main features of the orthodontic treatments performed in the included studies are outlined in Table 3. Details regarding the treatment type and timing were reported in 19 reports (86.4%). The timing of the orthodontic treatment varied, ranging from 1 month prior to tumor-ablative surgery to 19 years post-surgery. In two studies [17,27], orthodontic treatment was initiated directly after surgery or following the initial healing phase, to prevent mesial tooth movement and facilitate optimal functional outcome for the obturator prosthesis. Fixed orthodontic appliances were utilized in 14 cases (77.8%), whereas clear aligners were used in only one case [25] (5.6%). Orthognathic surgery was performed in three cases (16.7%) [24,26,31]. Bilateral sagittal split osteotomy was performed in two cases [26,31] to achieve mandibular advancement. In the third case [24], Le Fort I osteotomy and sagittal split ramus osteotomy were performed for maxillary advancement and mandibular setback.
3.4. Type and Timing of Orthodontic Treatment Relative to the Maxillofacial Prosthetic Rehabilitation
The key characteristics of the maxillofacial prosthodontic rehabilitation are provided in Table 3. Eighteen studies (81.8%) offered sufficient information about the type of prosthesis, but the timing was not thoroughly documented. In four cases, prosthetic treatment was initiated prior to orthodontic treatment. Bonitz et al. [26] and Singer et al. [31] used dental implants with a fixed hybrid prosthesis for anchorage, with Singer’s report employing it also as an anterior bite ramp. In the report by Tomita et al. [30], an occlusal splint was utilized in the mandible for three years, leading to an iatrogenic open bite. Kolokitha et al. [19] applied a temporary removable partial denture with posterior bite blocks before starting orthodontic treatment. Additionally, in two cases, dental implants were placed before orthodontic treatment but were not loaded until their completion. Orthodontic treatment coincided with the use of an obturator prosthesis in three cases. In two studies, the prosthesis design was modified to aid orthodontic movement, incorporating a buccal canine retractor in one case and a twin block appliance in the other. In the case of Ruse et al. [17], orthodontic treatment started immediately after healing to enhance the retention of the interim obturator prosthesis. Furthermore, dental implants were utilized in 10 cases (55.6%), whereas conventional tooth-supported prostheses were used in only three cases (16.7%).
3.5. Use of Orthodontic Appliances—Means to Increase the Retention of Maxillofacial Prostheses
Orthodontic appliances were employed to improve the retention of maxillofacial prostheses in three studies. Aponte-Wesson et al. [18] utilized a modified high-pull headgear to stabilize an interim obturator prosthesis. Kocadereli and Atac [33] fabricated a fixed prosthesis resembling a Nance appliance, which was cemented to the maxillary first permanent molars and replaced the missing anterior teeth. Ruse et al. [17] used orthodontic appliances to retain an interim obturator in a patient with mixed dentition and partially erupted teeth that lacked engageable undercuts. The obturator prosthesis clasps were designed according to the position of the orthodontic appliances, incorporating a pigtail loop near the maxillary right lateral incisor and an extended clasp near the maxillary left first molar. This extended clasp provided greater flexibility, ensuring proper seating over the orthodontic band and adequate retention.
4. Discussion
Although case reports on the integration of orthodontics in maxillofacial prosthetic rehabilitation following tumor-ablative surgery have been published, the authors are unaware of any existing systematic reviews. The findings of this systematic review highlight a scarcity of publications in this area, likely due to the perplexity and uniqueness of each case study. Regarding its methodology, the systematic review followed the PRISMA [20] and the SWiM guidelines [35]. All included studies were case reports or case series. The methodological limitations inherent in these reports, such as lack of controls, inconsistent follow-up, and absence of standardized outcome measures (e.g., quality of life), reduce the credibility of the findings. No relevant randomized controlled trials or retrospective studies were found. Another limitation of this systematic review is the absence of a meta-analysis, due to the heterogeneity of the included reports. Significant variations were observed in study design (e.g., patient’s age, tumor type, and site), intervention duration, and reported outcomes. Hence, the results were synthesized qualitatively following the SWiM reporting guideline. We created a flowchart diagram to help clinicians in decision-making regarding the timing of orthodontic treatment (Figure 2).
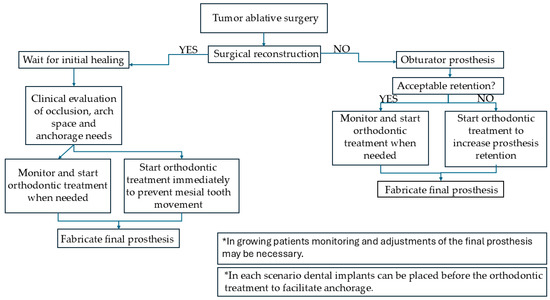
Figure 2.
Flowchart diagram regarding the timing of orthodontic intervention.
For cases involving tumors in the maxilla, orthodontic treatment primarily facilitated maxillofacial prosthetic rehabilitation by optimizing conditions before prosthetic intervention and enhancing obturator prosthesis retention. Saccomanno et al. [25] used myofunctional therapy and clear aligners to reduce an open bite that developed following the surgical resection of an ameloblastoma. Chavis et al. [11] utilized an implant-supported hybrid prosthesis as anchorage to move the anterior maxillary teeth with fixed orthodontic appliances into the preserved lateral alveolus and, therefore, improve the dental–facial midline asymmetry.
Craniofacial growth alterations are observed in 66–100% of children with head and neck cancer. Common findings are maxillary retrusion, tooth agenesis, and delayed tooth eruption [9,36,37]. Rehabilitation of these patients frequently involves the use of an obturator prosthesis, which not only enhances essential functions such as speech and swallowing but also improves esthetics and provides psychological benefits [38,39]. Moreover, the prosthesis is crucial for normal craniofacial growth and for the prevention of secondary deformities, such as overeruption and occlusal plane canting [11].
The optimal retention of the obturator prosthesis is essential for enhancing patients’ quality of life [40]. The edentulous area is typically unilateral and free-end, with a reduced alveolar ridge due to the defect, and an exaggerated vertical distance between the occlusal plane and the basal structures [4]. Additionally, in the mixed dentition, the frequent absence of sufficient undercuts due to partially erupted teeth further complicates retention. In such cases, fixed orthodontic appliances may provide the required retention. Ruse et al. [17] initiated orthodontic treatment simultaneously with the use of the obturator prosthesis, attaching the prosthesis’s clasps to the fixed orthodontic appliances. Another viable approach to improving prosthesis retention is the placement of osseointegrated dental implants [41]. While this method is effective in adults, it is not recommended for individuals with incomplete craniofacial growth, as implants behave similarly to ankylosed teeth [14,15]. Retention of the obturator prosthesis using extraoral devices, such as high-pull headgear, is only a temporary solution and should be limited to specific cases [18].
For patients with tumors located in the mandible, orthodontic treatment improved the conditions prior to maxillofacial prosthetic rehabilitation. Fixed orthodontic appliances were most frequently used. Additionally, in two cases [6,10], transverse discrepancies were corrected using maxillary expansion devices. Kolokitha et al. [19] utilized orthodontic techniques to guide vertical facial growth in a patient who had lost all posterior teeth on the affected side. Posterior acrylic bite blocks were placed bilaterally to enhance the lower facial height. Landes et al. [32] used fixed orthodontic appliances and orthodontic microscrews as skeletal anchorage to retain three wisdom teeth autotransplanted into a free iliac crest graft. One of the transplanted teeth became mobile and was lost within three months. The other two were forced to erupt. As the extrusion was inadequate, a conventional bridge was fabricated for full functional rehabilitation.
5. Conclusions
Orthodontic intervention may provide significant benefits for patients undergoing maxillofacial prosthetic rehabilitation following tumor-ablative surgery. In young patients, orthodontics can aid in optimizing the growth process. In addition, it can improve occlusion and facilitate prosthetic rehabilitation, either by enhancing the retention of removable prostheses or by creating the necessary space for prosthetic placement. Further evaluation of the role of orthodontics in such cases is essential in order to establish treatment guidelines regarding the type and timing of orthodontics in this multidisciplinary treatment plan. This systematic review synthesized the scarce available data qualitatively and attempted to suggest a flowchart diagram regarding orthodontic treatment timing. In addition, the use of orthodontic miniscrews in the anterior palate could provide promising treatment results in adult patients, as they can aid the retention of a temporary prosthesis before the final implant-supported restoration.
Author Contributions
Conceptualization, I.I.A. and H.V.; methodology, I.I.A. and H.V.; formal analysis, N.G.; investigation, N.G. and I.I.A.; data curation, N.G., I.I.A. and H.V.; writing—original draft preparation, N.G.; writing—review and editing, I.I.A. and H.V.; supervision, I.I.A. and H.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Please contact the corresponding author for data requests.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PRISMA | Preferred reporting items for systematic reviews and meta-analyses |
| PROSPERO | International Prospective Register of Systematic Reviews |
| MeSH | Medical Subject Heading |
| NIH | National Institute of Health |
| SWiM | Synthesis without meta-analysis |
| NHC | Head and neck cancer |
| QOL | Quality of life |
| PICO | Participant, intervention, comparison, and outcome |
| MNTI | Melanotic neuroectodermal tumor of infancy |
References
- Llewellyn, C.D.; Johnson, N.W.; Warnakulasuriya, K.A. Risk factors for squamous cell carcinoma of the oral cavity in young people—A comprehensive literature review. Oral Oncol. 2001, 37, 401–418. [Google Scholar] [CrossRef]
- Toner, M.; O’Regan, E.M. Head and neck squamous cell carcinoma in the young: A spectrum or a distinct group? Part 1. Head Neck Pathol. 2009, 3, 246–248. [Google Scholar] [CrossRef]
- Heggie, A.A. Unusual jaw lesions in the paediatric and adolescent patient: A management challenge. Ann. R. Australas. Coll. Dent. Surg. 2000, 15, 185–192. [Google Scholar] [PubMed]
- Kotsiomiti, E.; Kolokitha, O.E.; Lazaridis, N. Interim prosthodontic management of surgery-induced dental agenesis: A clinical report of 8 years of treatment. J. Prosthodont. 2013, 22, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Alhajj, M.N.; Ismail, I.A.; Khalifa, N. Maxillary obturator prosthesis for a hemimaxillectomy patient: A clinical case report. Saudi J. Dent. Res. 2016, 7, 153–159. [Google Scholar] [CrossRef]
- Liao, H.Y.; Chen, M.S.; Yang, Y.F.; Liao, P.B.; Feng, S.W.; Juan, P.K. Multidisciplinary Approach for Full-Mouth Rehabilitation of a Young Adult Patient with Ameloblastoma. Case Rep. Dent. 2021, 2021, 8694775. [Google Scholar] [CrossRef]
- Chigurupati, R.; Aloor, N.; Salas, R.; Schmidt, B.L. Quality of life after maxillectomy and prosthetic obturator rehabilitation. J. Oral Maxillofac. Surg. 2013, 71, 1471–1478. [Google Scholar] [CrossRef]
- Chung, J.O.K.; Li, W.H.C.; Cheung, A.T.; Ho, L.L.K.; Xia, W.; Chan, G.C.F.; Lopez, V. Relationships among resilience, depressive symptoms, self-esteem, and quality of life in children with cancer. Psycho-Oncology 2021, 30, 194–201. [Google Scholar] [CrossRef]
- Gevorgyan, A.; La Scala, G.C.; Neligan, P.C.; Pang, C.Y.; Forrest, C.R. Radiation-induced craniofacial bone growth disturbances. J. Craniofacial Surg. 2007, 18, 1001–1007. [Google Scholar] [CrossRef]
- Nilius, M.; Hölzle, F.; Nilius, M.H.; Lauer, G. Intraosseous venous malformation in an adolescent: Interdisciplinary concept for facial reconstruction after hemimandibulectomy, fibula free flap, and HDPE-chin reconstruction—10 years follow up. Oral Maxillofac. Surg. Cases 2021, 7, 100209. [Google Scholar] [CrossRef]
- Chavis, S.E.; Shrikian, T.M.; Haerian, A.; Edwards, S.P.; Munz, S.M. Coordinated pediatric reconstruction and rehabilitation of maxillary central giant cell granuloma. J. Am. Dent. Assoc. 2018, 149, 1065–1072. [Google Scholar] [CrossRef]
- Moseley, H.C.; Horrocks, E.N.; Welfare, R.R. Use of a modified twin block appliance following partial maxillectomy: Case report. Br. J. Orthod. 1996, 23, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Troulis, M.J.; Williams, W.B.; Kaban, L.B. Staged protocol for resection, skeletal reconstruction, and oral rehabilitation of children with jaw tumors. J. Oral Maxillofac. Surg. 2004, 62, 335–343. [Google Scholar] [CrossRef]
- Bohner, L.; Hanisch, M.; Kleinheinz, J.; Jung, S. Dental implants in growing patients: A systematic review. Br. J. Oral Maxillofac. Surg. 2019, 57, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Elagib, M.F.A.; Alqaysi, M.A.H.; Almushayt, M.O.S.; Nagate, R.R.; Gokhale, S.T.; Chaturvedi, S. Dental implants in growing patients: A systematic review and meta-analysis. Technol. Health Care 2023, 31, 1051–1064. [Google Scholar] [CrossRef] [PubMed]
- Sailer, H.F.; Tarawneh, F.; Fourkas, P.; Antoniades, D.Z.; Athanasiou, A.E. Surgical, orthodontic and prosthodontic rehabilitation of a patient with follicular ameloblastoma: A case report. Eur. J. Dent. 2010, 4, 192–196. [Google Scholar] [CrossRef]
- Ruse, M.K.; Lloren, P.A.; Bigsby, A.J., 3rd; Harper, M.T.; Lee, S.K.Y.; Muller, O.M. Utilizing orthodontic appliances to retain and disguise a pediatric maxillary obturator throughout growth. J. Prosthet. Dent. 2023, in press. [Google Scholar] [CrossRef]
- Aponte-Wesson, R.; Carroll, W.; Waite, P.; Seidenfaden, J.C. Interim obturator retained by an extraoral device: A clinical report. J. Prosthodont. 2008, 17, 582–585. [Google Scholar] [CrossRef]
- Kolokitha, O.E.; Kotsiomiti, E.; Lazaridis, K.; Lazaridis, N. Mandibular Melanotic Neuroectodermal Tumor of Infancy: Interdisciplinary Treatment from 2 Months to 19 Years of Age. J. Maxillofac. Oral Surg. 2022, 21, 105–111. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Faggion, C.M., Jr.; Tu, Y.K. Evidence-based dentistry: A model for clinical practice. J. Dent. Educ. 2007, 71, 825–831. [Google Scholar] [CrossRef] [PubMed]
- NIH. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 30 May 2025).
- Theologie-Lygidakis, N.; Telona, P.; Michail-Strantzia, C.; Iatrou, I. Treatment of central giant-cell granulomas of the jaws in children: Conservative or radical surgical approach? J. Cranio-Maxillofac. Surg. 2011, 39, 639–644. [Google Scholar] [CrossRef]
- Kim, S.H.; Choi, T.H.; Lee, Y.S.; Kim, Y.K.; Jo, D.W.; Kim, B.K.; Choi, H.L.; Lee, N.K. Rehabilitation of severe dentofacial deformity after early radiotherapy of retinoblastoma: A case report. J. Med. Case Rep. 2023, 17, 103. [Google Scholar] [CrossRef] [PubMed]
- Saccomanno, S.; Laganà, D.; Saran, S.; Greco, F.; Capogreco, M.; Pirino, A.; Scoppa, F.; Pirelli, P. Diagnosis, treatment planning and orthodontic treatment in patients with ameloblastoma. J. Biol. Regul. Homeost. Agents 2022, 36, 165–173. [Google Scholar]
- Bonitz, L.; Chhatwani, S.; Hassfeld, S.; Soemmer, C.; Bicsak, A. Complex treatment of huge, massive growing ameloblastoma in teenage, a case report. Oral Maxillofac. Surg. Cases 2021, 7, 100226. [Google Scholar] [CrossRef]
- Nilius, M.; Kohlhase, J.; Lorenzen, J.; Lauer, G.; Schulz, M.C. Multidisciplinary oral rehabilitation of an adolescent suffering from juvenile Gorlin-Goltz syndrome—A case report. Head Face Med. 2019, 15, 5. [Google Scholar] [CrossRef] [PubMed]
- Yuzbasioglu, E.; Alkan, A.; Ozer, M.; Bayram, M. Multidisciplinary approach for the rehabilitation of central giant cell granuloma: A clinical report. Niger. J. Clin. Pract. 2014, 17, 528–533. [Google Scholar] [CrossRef]
- Nojima, K.; Niizuma-Kosaka, F.; Nishii, Y.; Sueishi, K.; Yamakura, D.; Ikumoto, H.; Ohata, H.; Inoue, T. Multidisciplinary treatment of peripheral osteoma arising from mandibular condyle in patient presenting with facial asymmetry. Bull. Tokyo Dent. Coll. 2014, 55, 39–47. [Google Scholar] [CrossRef]
- Tomita, Y.; Kuroda, S.; Takahashi, T.; Ohura, R.; Tanaka, E. Orthodontic occlusal reconstruction after conservative treatment of unicystic ameloblastoma in an adolescent patient: 10-year follow-up. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 466–470. [Google Scholar] [CrossRef]
- Singer, S.L.; Henry, P.J.; Allan, B.P. The interdisciplinary management of a Class II division 1 malocclusion with an associated mandibular defect following surgical excision of fibromatosis: A clinical report. J. Prosthet. Dent. 2009, 102, 279–285. [Google Scholar] [CrossRef]
- Landes, C.A.; Glasl, B.; Ludwig, B.; Rieger, J.; Sader, R. Tooth autotransplantation in a free iliac crest graft for prosthetic reconstruction. J. Craniofacial Surg. 2008, 19, 1281–1286. [Google Scholar] [CrossRef]
- Kocadereli, I.; Atac, A. Orthodontic management of a horizontally positioned maxillary lateral incisor. J. Clin. Pediatr. Dent. 1995, 20, 1–4. [Google Scholar] [PubMed]
- Koumjian, J.H.; Firtell, D.N. An appliance to correct mandibular deviation in a dentulous patient with a discontinuity defect. J. Prosthet. Dent. 1992, 67, 833–834. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef]
- Vissink, A.; Jansma, J.; Spijkervet, F.K.; Burlage, F.R.; Coppes, R.P. Oral sequelae of head and neck radiotherapy. Crit. Rev. Oral Biol. Med. 2003, 14, 199–212. [Google Scholar] [CrossRef]
- Bektaş-Kayhan, K.; Ozbek, C.D.; Yazicioğlu, O.; Karagöz, G.; Altun, M.; Meral, R.; Unür, M. Long-term maxillofacial effects of radiotherapy in young nasopharyngeal carcinoma patients: Report of 3 cases. J. Clin. Pediatr. Dent. 2013, 37, 407–410. [Google Scholar] [CrossRef] [PubMed]
- Manoj, N.; Singaravel Chidambaranathan, A.; Balasubramanium, M.; Rajapandi, G.R. Role of obturator in restoring quality of life and function in maxillary oncological defect cases- A systematic review. Oral Oncol. Rep. 2024, 11, 100636. [Google Scholar] [CrossRef]
- Brandão, T.B.; Vechiato Filho, A.J.; de Souza Batista, V.E.; de Oliveira, M.C.Q.; Santos-Silva, A.R. Obturator prostheses versus free tissue transfers: A systematic review of the optimal approach to improving the quality of life for patients with maxillary defects. J. Prosthet. Dent. 2016, 115, 247–253.e244. [Google Scholar] [CrossRef]
- Andrades, P.; Militsakh, O.; Hanasono, M.M.; Rieger, J.; Rosenthal, E.L. Current strategies in reconstruction of maxillectomy defects. Arch. Otolaryngol. Head Neck Surg. 2011, 137, 806–812. [Google Scholar] [CrossRef]
- Buurman, D.J.M.; Speksnijder, C.M.; Engelen, B.H.B.T.; Kessler, P. Masticatory performance and oral health-related quality of life in edentulous maxillectomy patients: A cross-sectional study to compare implant-supported obturators and conventional obturators. Clin. Oral Implant. Res. 2020, 31, 405–416. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).