Digital Dentistry and Imaging: Comparing the Performance of Smartphone and Professional Cameras for Clinical Use
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol of the Study
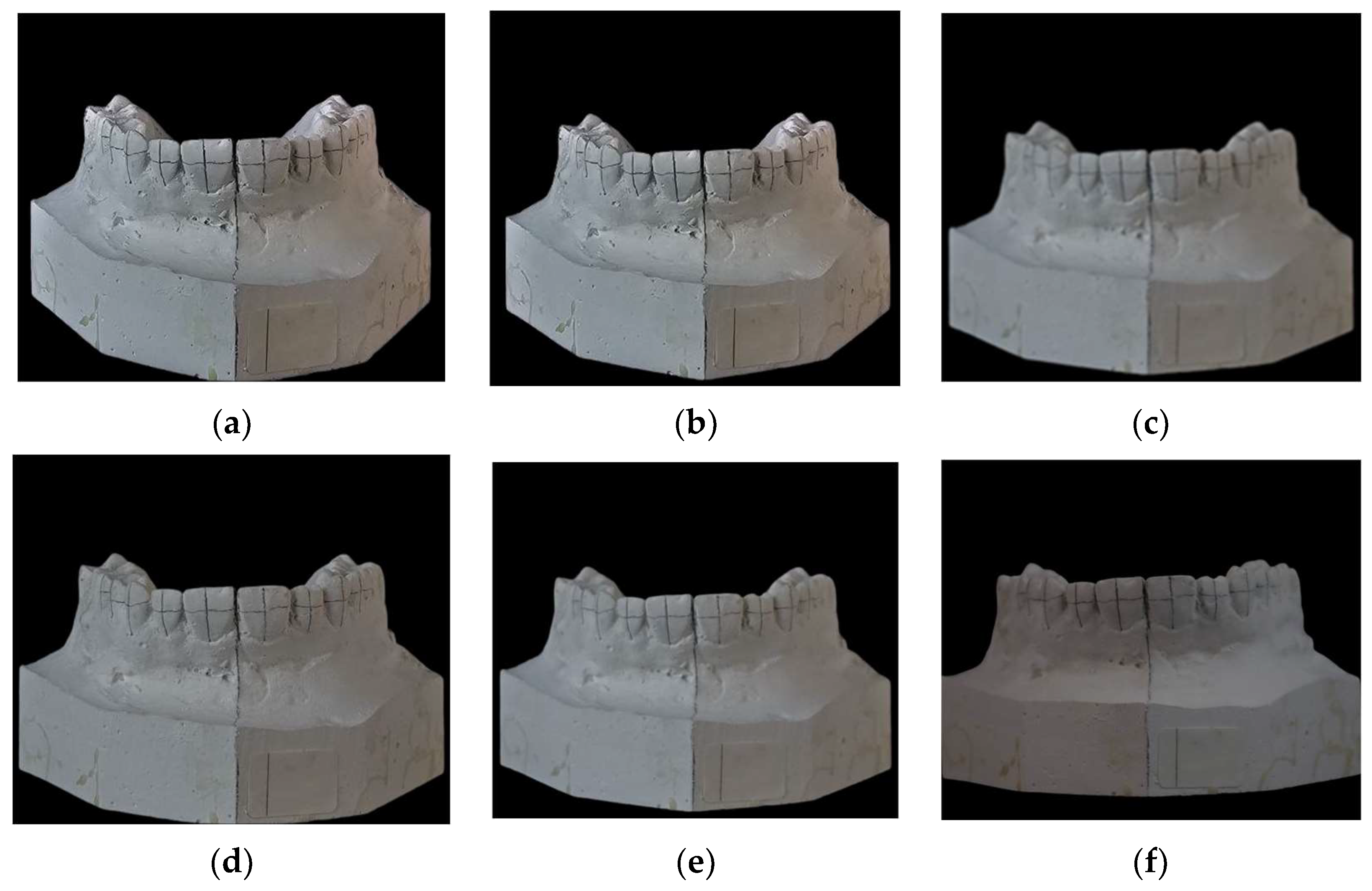
2.2. Model Preparation Before Data Collection
2.3. Model Scanning
2.4. DSLR Photographs
2.5. Smartphone Photographs
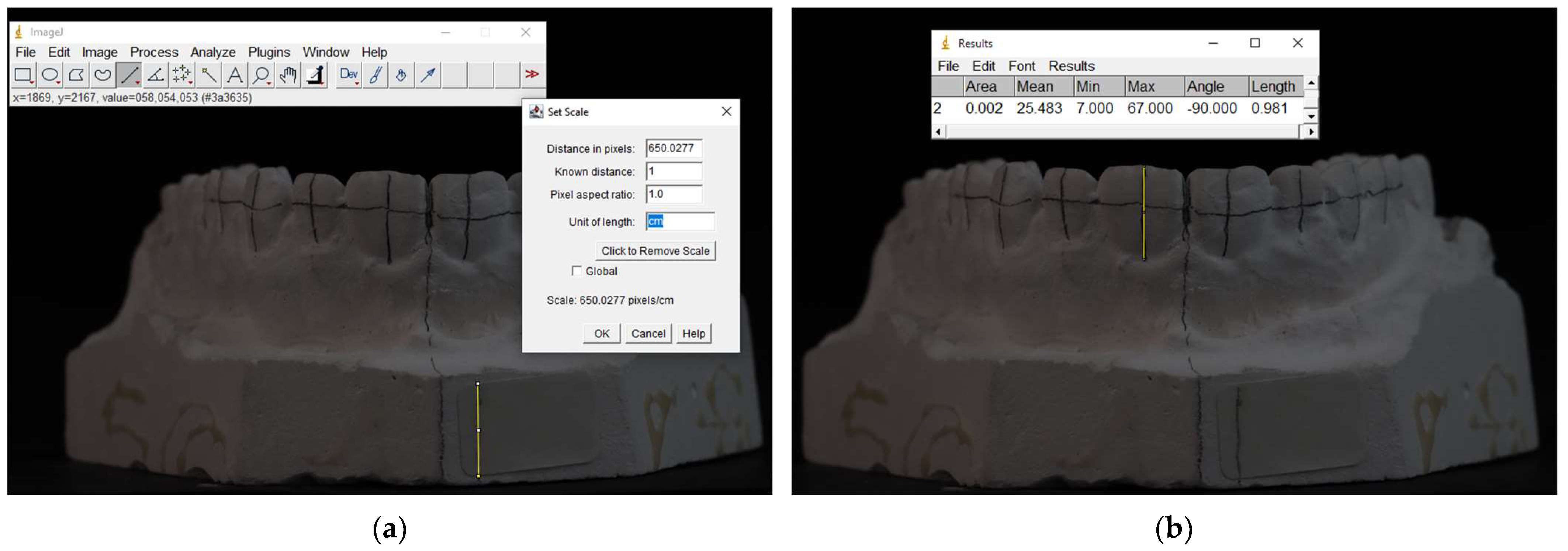
2.6. Collection of Measurements from the Photographs
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Patussi, E.G.; Poltronieri, B.C.G.; Ottoni, R.; Bervian, J.; Lisboa, C.; Corazza, P.H. Comparisons between photographic equipment for dental use: DSLR cameras vs. smartphones. Rev. Fac. Odontol. UPF 2019, 24, 198–203. [Google Scholar] [CrossRef]
- Terry, D.; Snow, S.; McLaren, E. Contemporary dental photography: Selection and application. Compend. Contin. Educ. Dent. 2008, 29, 432. [Google Scholar] [PubMed]
- Chen, J.W.; Hobdell, M.H.; Dunn, K.; Johnson, K.A.; Zhang, J. Teledentistry and its use in dental education. J. Am. Dent. Assoc. 2003, 134, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Kalpana, D.; Rao, S.J.; Joseph, J.K.; Kurapati, S.K.R. Digital dental photography. Indian J. Dent. Res. 2018, 29, 507. [Google Scholar]
- Desai, V.; Bumb, D. Digital dental photography: A contemporary revolution. Int. J. Clin. Pediatr. Dent. 2013, 6, 193–196. [Google Scholar] [CrossRef]
- Hardan, L.; Moussa, C. Mobile dental photography: A simple technique for documentation and communication. Quintessence Int. 2020, 51, 510–518. [Google Scholar]
- Coachman, C.; Calamita, M.; Ricci, A. Digital smile design. In Ronald E. Goldstein’s Esthetics in Dentistry; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2018; pp. 84–111. [Google Scholar]
- Ahmad, I. Digital dental photography. Part 2: Purposes and uses. Br. Dent. J. 2009, 206, 459–464. [Google Scholar] [CrossRef]
- Gonzaga, C.; Garcia, P.; da Costa, R.; Calgaro, M.; Ritter, A.; Correr, G.; da Cunha, L. Digital smile design and mock-up technique for esthetic treatment planning with porcelain laminate veneers. J. Conserv. Dent. 2018, 21, 455–458. [Google Scholar] [CrossRef]
- McLaren, E.A.; Goldstein, R.E. The Photoshop smile design technique. Compend. Contin. Educ. Dent. 2018, 39, e17–e20. [Google Scholar]
- Zhang, C.; Fan, L.; Chai, Z.; Yu, C.; Song, J. Smartphone and medical application use among dentists in China. BMC Med. Inform. Decis. Mak. 2020, 20, 213. [Google Scholar] [CrossRef]
- Hardan, L. Protocols for Mobile Dental Photography with Auxiliary Lighting; Quintessence Publishing: Chicago, IL, USA, 2020. [Google Scholar]
- Majumder, S.; Deen, M.J. Smartphone sensors for health monitoring and diagnosis. Sensors 2019, 19, 2164. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Kim, B.; Lee, J.; Sasian, J. Accurate determination of distortion for smartphone cameras. Appl. Opt. 2014, 53, H1–H6. [Google Scholar] [CrossRef] [PubMed]
- Moussa, C.; Hardan, L.; Kassis, C.; Bourgi, R.; Devoto, W.; Jorquera, G.; Panda, S.; Fadel, R.A.; Cuevas-Suárez, C.E.; Lukomska-Szymanska, M.; et al. Accuracy of dental photography: Professional vs. smartphone cameras. Biomed. Res. Int. 2021, 2021, 3910291. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, L.; Sharland, M. Technique Tips: Mobile Dental Photography (MDP). Dent. Update 2020, 47, 884–885. [Google Scholar] [CrossRef]
- Jorquera, G.J.; Atria, P.J.; Galán, M.; Feureisen, J.; Imbarak, M.; Kernitsky, J.; Cacciuttolo, F.; Hirata, R.; Sampaio, C.S. A Comparison of Ceramic Crown Color Difference Between Different Shade Selection Methods: Visual, Digital Camera, and Smartphone. J. Prosthet. Dent. 2022, 128, 784–792. [Google Scholar] [CrossRef]
- Lazar, R.; Culic, B.; Gasparik, C.; Lazar, C.; Dudea, D. The Accuracy of Dental Shade Matching Using Cross-Polarization Photography. Int. J. Comput. Dent. 2019, 22, 343–351. [Google Scholar]
- Antar, F.; Zebouni, E. Comparative review of DSLR cameras and smartphones in dental photography: Indications and limitations. Int. Arab. J. Dent. 2018, 9, 107–115. [Google Scholar]
- Sampaio, C.S.; Atria, P.J.; Hirata, R.; Jorquera, G. Variability of Color Matching with Different Digital Photography Techniques and a Gray Reference Card. J. Prosthet. Dent. 2019, 121, 333–339. [Google Scholar] [CrossRef]
- Cunha, L.F.D.; Fernandes, A.B.F.; Baechtold, M.S.; Correr, G.M.; Gonzaga, C.C. Cara Smile: Use of Planning Software to Facilitate Esthetic Dental Treatment in a Case. Indian. J. Dent. Res. 2019, 30, 964. [Google Scholar] [CrossRef]
- Jafri, Z.; Ahmad, N.; Sawai, M.; Sultan, N.; Bhardwaj, A. Digital smile design: An innovative tool in aesthetic dentistry. J. Oral. Biol. Craniofac. Res. 2020, 10, 194–198. [Google Scholar] [CrossRef]
- Gorripati, J.P.; Godbole, S.D. Creating smiles with digital workflow and matrix transfer technique in customizing personality-based smile designing. Int. Arab. J. Dent. 2024, 15, 199–206. [Google Scholar] [CrossRef]
- Omar, D.; Duarte, C. The application of parameters for comprehensive smile esthetics by digital smile design programs: A review of literature. Saudi Dent. J. 2018, 30, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Iliev, G.V.; Romeo, G. Harmony of smile design in the facial context. Int. J. Esthet. Dent. 2020, 15, 92–106. [Google Scholar]
- Bourgi, R.; Qaddomi, M.; Hardan, L.; Tohme, H.; Corbani, K.; Abou Isber, S.; Daher, E.A.; Nassar, N.; Kharouf, N.; Haikel, Y. Gingival Contouring and Smile Makeover through Digital Planning and 3D Guidance. J. Clin. Med. Res. 2025, 6, 6208. [Google Scholar] [CrossRef]
- Morris, R.S.; Hoye, L.N.; Elnagar, M.H.; Atsawasuwan, P.; Galang-Boquiren, M.T.; Caplin, J.; Viana, G.C.; Obrez, A.; Kusnoto, B. Accuracy of Dental Monitoring 3D digital dental models using photograph and video mode. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 420–428. [Google Scholar] [CrossRef]
- Sajjadi, S.H.; Khosravanifard, B.; Moazzami, F.; Rakhshan, V.; Esmaeilpour, M. Effects of three types of digital camera sensors on dental specialists’ perception of smile esthetics: A preliminary double-blind clinical trial. J. Prosthodont. 2016, 25, 675–681. [Google Scholar] [CrossRef]
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | iPhone 13 16 cm | iPhone 13 20 cm | iPhone 13 24 cm | iPhone 13 28 cm | iPhone 13 32 cm |
| 15 | 0.61 (0.09) | 0.60 (0.09) | 0.57 (0.08) | 0.56 (0.08) | 0.55 (0.08) | 0.55 (0.07) | 0.53 (0.06) | 0.56 (0.07) |
| 14 | 0.68 (0.09) | 0.66 (0.09) | 0.62 (0.1) | 0.64 (0.11) | 0.63 (0.11) | 0.62 (0.10) | 0.62 (0.11) | 0.63 (0.12) |
| 13 | 0.85 (0.15) | 0.83 (0.12) | 0.79 (0.17) | 0.82 (0.19) | 0.80 (0.17) | 0.79 (0.16) | 0.81 (0.15) | 0.82 (0.18) |
| 12 | 0.77 (0.19) | 0.75 (0.16) | 0.74 (0.19) | 0.74 (0.20) | 0.74 (0.20) | 0.73 (0.19) | 0.73 (0.19) | 0.75 (0.19) |
| 11 | 0.92 (0.12) | 0.90 (0.11) | 0.90 (0.12) | 0.91 (0.14) | 0.90 (0.14) | 0.88 (0.13) | 0.89 (0.12) | 0.92 (0.13) |
| 21 | 0.95 (0.14) | 0.94 (0.12) | 0.91 (0.14) | 0.91 (0.15) | 0.91 (0.15) | 0.87 (0.15) | 0.90 (0.14) | 0.91 (0.15) |
| 22 | 0.80 (0.13) | 0.77 (0.10) | 0.78 (0.12) | 0.76 (0.13) | 0.76 (0.13) | 0.75 (0.13) | 0.76 (0.12) | 0.78 (0.13) |
| 23 | 0.86 (0.16) | 0.85 (0.15) | 0.85 (0.19) | 0.85 (0.20) | 0.84 (0.20) | 0.83 (0.20) | 0.84 (0.20) | 0.86 (0.20) |
| 24 | 0.67 (0.11) | 0.66 (0.09) | 0.64 (0.11) | 0.62 (0.11) | 0.62 (0.10) | 0.61 (0.12) | 0.62 (0.10) | 0.64 (0.10) |
| 25 | 0.59 (0.08) | 0.58 (0.08) | 0.54 (0.07) | 0.53 (0.07) | 0.52 (0.06) | 0.51 (0.06) | 0.53 (0.06) | 0.52 (0.08) |
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | iPhone 15 16 cm | iPhone 15 20 cm | iPhone 15 24 cm | iPhone 15 28 cm | iPhone 15 32 cm |
| 15 | 0.61 (0.09) | 0.60 (0.09) | 0.57 (0.08) | 0.58 (0.06) | 0.55 (0.06) | 0.56 (0.09) | 0.55 (0.10) | 0.56 (0.08) |
| 14 | 0.68 (0.09) | 0.66 (0.09) | 0.62 (0.1) | 0.67 (0.08) | 0.65 (0.10) | 0.64 (0.09) | 0.63 (0.09) | 0.64 (0.06) |
| 13 | 0.85 (0.15) | 0.83 (0.12) | 0.79 (0.17) | 0.84 (0.10) | 0.81 (0.11) | 0.82 (0.10) | 0.81 (0.12) | 0.84 (0.10) |
| 12 | 0.77 (0.19) | 0.75 (0.16) | 0.74 (0.19) | 0.71 (0.20) | 0.75 (0.18) | 0.73 (0.18) | 0.74 (0.16) | 0.91 (0.18) |
| 11 | 0.92 (0.12) | 0.90 (0.11) | 0.90 (0.12) | 0.92 (0.19) | 0.89 (0.14) | 0.89 (0.15) | 0.88 (0.15) | 0.91 (0.14) |
| 21 | 0.95 (0.14) | 0.94 (0.12) | 0.91 (0.14) | 0.91 (0.20) | 0.90 (0.16) | 0.90 (0.16) | 0.88 (0.17) | 0.89 (0.13) |
| 22 | 0.80 (0.13) | 0.77 (0.10) | 0.78 (0.12) | 0.78 (0.19) | 0.76 (0.14) | 0.75 (0.15) | 0.76 (0.14) | 0.77 (0.12) |
| 23 | 0.86 (0.16) | 0.85 (0.15) | 0.85 (0.19) | 0.86 (0.27) | 0.85 (0.22) | 0.84 (0.22) | 0.84 (0.22) | 0.86 (0.19) |
| 24 | 0.67 (0.11) | 0.66 (0.09) | 0.64 (0.11) | 0.66 (0.16) | 0.63 (0.14) | 0.63 (0.12) | 0.63 (0.11) | 0.64 (0.09) |
| 25 | 0.59 (0.08) | 0.58 (0.08) | 0.54 (0.07) | 0.53 (0.08) | 0.55 (0.07) | 0.53 (0.1) | 0.55 (0.11) | 0.54 (0.07) |
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | S22 16 cm | S22 20 cm | S22 24 cm | S22 28 cm | S22 32 cm |
| 15 | 0.61 (0.09) | 0.60 (0.09) | 0.57 (0.08) | 0.54 (0.08) | 0.51 (0.10) | 0.56 (0.09) | 0.57 (0.09) | 0.59 (0.06) |
| 14 | 0.68 (0.09) | 0.66 (0.09) | 0.62 (0.1) | 0.61 (0.08) | 0.60 (0.14) | 0.64 (0.14) | 0.64 (0.12) | 0.68 (0.13) |
| 13 | 0.85 (0.15) | 0.83 (0.12) | 0.79 (0.17) | 0.79 (0.20) | 0.80 (0.22) | 0.84 (0.21) | 0.81 (0.20) | 0.80 (0.18) |
| 12 | 0.77 (0.19) | 0.75 (0.16) | 0.74 (0.19) | 0.74 (0.24) | 0.76 (0.26) | 0.76 (0.23) | 0.77 (0.24) | 0.74 (0.21) |
| 11 | 0.92 (0.12) | 0.90 (0.11) | 0.90 (0.12) | 0.90 (0.16) | 0.89 (0.19) | 0.92 (0.18) | 0.92 (0.15) | 0.93 (0.14) |
| 21 | 0.95 (0.14) | 0.94 (0.12) | 0.91 (0.14) | 0.90 (0.18) | 0.91 (0.22) | 0.92 (0.20) | 0.92 (0.16) | 0.93 (0.17) |
| 22 | 0.80 (0.13) | 0.77 (0.10) | 0.78 (0.12) | 0.76 (0.16) | 0.76 (0.18) | 0.79 (0.17) | 0.78 (0.14) | 0.79 (0.12) |
| 23 | 0.86 (0.16) | 0.85 (0.15) | 0.85 (0.19) | 0.83 (0.23) | 0.84 (0.27) | 0.87 (0.24) | 0.87 (0.23) | 0.85 (0.21) |
| 24 | 0.67 (0.11) | 0.66 (0.09) | 0.64 (0.11) | 0.61 (0.13) | 0.63 (0.15) | 0.64 (0.12) | 0.65 (0.13) | 0.66 (0.1) |
| 25 | 0.59 (0.08) | 0.58 (0.08) | 0.54 (0.07) | 0.52 (0.05) | 0.51 (0.05) | 0.52 (0.07) | 0.54 (0.06) | 0.58 (0.08) |
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | S23 16 cm | S23 20 cm | S23 24 cm | S23 28 cm | S23 32 cm |
| 15 | 0.61 (0.09) | 0.60 (0.09) | 0.57 (0.08) | 0.52 (0.10) | 0.54 (0.09) | 0.54 (0.09) | 0.53 (0.08) | 0.54 (0.08) |
| 14 | 0.68 (0.09) | 0.66 (0.09) | 0.62 (0.1) | 0.62 (0.15) | 0.63 (0.11) | 0.64 (0.13) | 0.63 (0.13) | 0.62 (0.12) |
| 13 | 0.85 (0.15) | 0.83 (0.12) | 0.79 (0.17) | 0.83 (0.22) | 0.79 (0.16) | 0.83 (0.18) | 0.80 (0.17) | 0.79 (0.20) |
| 12 | 0.77 (0.19) | 0.75 (0.16) | 0.74 (0.19) | 0.75 (0.25) | 0.73 (0.21) | 0.74 (0.21) | 0.73 (0.22) | 0.73 (0.21) |
| 11 | 0.92 (0.12) | 0.90 (0.11) | 0.90 (0.12) | 0.88 (0.20) | 0.89 (0.15) | 0.89 (0.16) | 0.89 (0.16) | 0.89 (0.15) |
| 21 | 0.95 (0.14) | 0.94 (0.12) | 0.91 (0.14) | 0.91 (0.19) | 0.90 (0.16) | 0.90 (0.17) | 0.90 (0.16) | 0.90 (0.16) |
| 22 | 0.80 (0.13) | 0.77 (0.10) | 0.78 (0.12) | 0.76 (0.17) | 0.75 (0.13) | 0.77 (0.14) | 0.76 (0.14) | 0.75 (0.13) |
| 23 | 0.86 (0.16) | 0.85 (0.15) | 0.85 (0.19) | 0.83 (0.25) | 0.83 (0.22) | 0.84 (0.22) | 0.82 (0.22) | 0.75 (0.13) |
| 24 | 0.67 (0.11) | 0.66 (0.09) | 0.64 (0.11) | 0.64 (0.13) | 0.61 (0.10) | 0.64 (0.10) | 0.64 (0.11) | 0.62 (0.12) |
| 25 | 0.59 (0.08) | 0.58 (0.08) | 0.54 (0.07) | 0.50 (0.10) | 0.50 (0.06) | 0.52 (0.08) | 0.53 (0.09) | 0.50 (0.09) |
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | S24 16 cm | S24 20 cm | S24 24 cm | S24 28 cm | S24 32 cm |
| 15 | 0.61 (0.09) | 0.60 (0.09) | 0.57 (0.08) | 0.54 (0.09) | 0.58 (0.09) | 0.56 (0.06) | 0.55 (0.08) | 0.55 (0.09) |
| 14 | 0.68 (0.09) | 0.66 (0.09) | 0.62 (0.1) | 0.64 (0.14) | 0.63 (0.14) | 0.67 (0.12) | 0.63 (0.12) | 0.64 (0.14) |
| 13 | 0.85 (0.15) | 0.83 (0.12) | 0.79 (0.17) | 0.80 (0.2) | 0.80 (0.2) | 0.81 (0.17) | 0.80 (0.17) | 0.81 (0.17) |
| 12 | 0.77 (0.19) | 0.75 (0.16) | 0.74 (0.19) | 0.73 (0.25) | 0.74 (0.24) | 0.72 (0.21) | 0.75 (0.24) | 0.72 (0.23) |
| 11 | 0.92 (0.12) | 0.90 (0.11) | 0.90 (0.12) | 0.91 (0.15) | 0.90 (0.16) | 0.91 (0.15) | 0.91 (0.14) | 0.88 (0.16) |
| 21 | 0.95 (0.14) | 0.94 (0.12) | 0.91 (0.14) | 0.91 (0.16) | 0.91 (0.17) | 0.92 (0.16) | 0.91 (0.15) | 0.88 (0.16) |
| 22 | 0.80 (0.13) | 0.77 (0.10) | 0.78 (0.12) | 0.77 (0.14) | 0.76 (0.14) | 0.58 (0.12) | 0.54 (0.08) | 0.53 (0.10) |
| 23 | 0.86 (0.16) | 0.85 (0.15) | 0.85 (0.19) | 0.82 (0.22) | 0.83 (0.22) | 0.84 (0.22) | 0.84 (0.23) | 0.83 (0.21) |
| 24 | 0.67 (0.11) | 0.66 (0.09) | 0.64 (0.11) | 0.63 (0.11) | 0.63 (0.10) | 0.65 (0.11) | 0.64 (0.11) | 0.64 (0.12) |
| 25 | 0.59 (0.08) | 0.58 (0.08) | 0.54 (0.07) | 0.51 (0.04) | 0.52 (0.08) | 0.54 (0.07) | 0.52 (0.08) | 0.54 (0.10) |
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | Vivo 16 cm | Vivo 20 cm | Vivo 24 cm | Vivo 28 cm | Vivo 32 cm |
| 15 | 0.61 (0.09) | 0.60 (0.09) | 0.57 (0.08) | 0.47 (0.14) | 0.51 (0.14) | 0.55 (0.09) | 0.57 (0.08) | 0.55 (0.08) |
| 14 | 0.68 (0.09) | 0.66 (0.09) | 0.62 (0.1) | 0.62 (0.13) | 0.61 (0.07) | 0.63 (0.12) | 0.63 (0.10) | 0.62 (0.12) |
| 13 | 0.85 (0.15) | 0.83 (0.12) | 0.79 (0.17) | 0.80 (0.19) | 0.79 (0.18) | 0.80 (0.19) | 0.81 (0.17) | 0.79 (0.19) |
| 12 | 0.77 (0.19) | 0.75 (0.16) | 0.74 (0.19) | 0.73 (0.20) | 0.73 (0.21) | 0.75 (0.21) | 0.74 (0.19) | 0.72 (0.20) |
| 11 | 0.92 (0.12) | 0.90 (0.11) | 0.90 (0.12) | 0.88 (0.14) | 0.88 (0.14) | 0.90 (0.14) | 0.89 (0.13) | 0.88 (0.14) |
| 21 | 0.95 (0.14) | 0.94 (0.12) | 0.91 (0.14) | 0.89 (0.16) | 0.91 (0.16) | 0.91 (0.14) | 0.90 (0.14) | 0.90 (0.16) |
| 22 | 0.80 (0.13) | 0.77 (0.10) | 0.78 (0.12) | 0.76 (0.14) | 0.77 (0.14) | 0.76 (0.12) | 0.75 (0.12) | 0.75 (0.15) |
| 23 | 0.86 (0.16) | 0.85 (0.15) | 0.85 (0.19) | 0.83 (0.22) | 0.86 (0.21) | 0.86 (0.22) | 0.84 (0.21) | 0.84 (0.20) |
| 24 | 0.67 (0.11) | 0.66 (0.09) | 0.64 (0.11) | 0.62 (0.11) | 0.64 (0.11) | 0.63 (0.10) | 0.63 (0.11) | 0.62 (0.12) |
| 25 | 0.59 (0.08) | 0.58 (0.08) | 0.54 (0.07) | 0.51 (0.06) | 0.54 (0.08) | 0.53 (0.07) | 0.54 (0.09) | 0.52 (0.09) |
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | iPhone 13 16 cm | iPhone 13 20 cm | iPhone 13 24 cm | iPhone 13 28 cm | iPhone 13 32 cm |
| 15 | 0.19 (0.01) | 0.19 (0.01) | 0.23 (0.13) | 0.18 (0.14) | 0.16 (0.13) | 0.49 (0.21) * | 0.12 (0.02) * | 0.12 (0.02) * |
| 14 | 0.29 (0.02) | 0.29 (0.02) | 0.30 (0.13) | 0.22 (0.03) | 0.21 (0.03) | 0.57 (0.21) * | 0.19 (0.02) * | 0.21 (0.03) |
| 13 | 0.46 (0.05) | 0.45 (0.05) | 0.48 (0.15) | 0.41 (0.07) | 0.41 (0.07) | 0.75 (0.24) * | 0.39 (0.07) | 0.40 (0.07) |
| 12 | 0.55 (0.06) | 0.56 (0.06) | 0.54 (0.08) | 0.52 (0.08) | 0.52 (0.08) | 0.72 (0.21) * | 0.51 (0.07) | 0.51 (0.08) |
| 11 | 0.85 (0.1) | 0.84 (0.10) | 0.82 (0.06) | 0.87 (0.10) | 0.87 (0.10) | 0.89 (0.12) | 0.83 (0.09) | 0.85 (0.10) |
| 21 | 0.85 (0.1) | 0.85 (0.11) | 0.83 (0.04) | 0.90 (0.11) | 0.90 (0.11) | 0.89 (0.14) | 0.87 (0.1) | 0.89 (0.1) |
| 22 | 0.53 (0.07) | 0.52 (0.07) | 0.53 (0.08) | 0.54 (0.09) | 0.54 (0.09) | 0.73 (0.15) * | 0.56 (0.1) | 0.54 (0.08) |
| 23 | 0.43 (0.06) | 0.43 (0.06) | 0.48 (0.17) | 0.43 (0.04) | 0.42 (0.04) | 0.82 (0.022) * | 0.43 (0.04) | 0.42 (0.06) |
| 24 | 0.26 (0.05) | 0.26 (0.05) | 0.30 (0.13) | 0.27 (0.05) | 0.26 (0.05) | 0.56 (0.18) * | 0.28 (0.04) | 0.28 (0.05) |
| 25 | 0.17 (0.05) | 0.17 (0.05) | 0.24 (0.12) | 0.18 (0.04) | 0.18 (0.04) | 0.46 (0.16) * | 0.19 (0.05) | 0.20 (0.04) |
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | iPhone 15 16 cm | iPhone 15 20 cm | iPhone 15 24 cm | iPhone 15 28 cm | iPhone 15 32 cm |
| 15 | 0.19 (0.01) | 0.19 (0.01) | 0.23 (0.13) | 0.15 (0.04) | 0.13 (0.03) | 0.14 (0.03) | 0.15 (0.02) | 0.18 (0.03) |
| 14 | 0.29 (0.02) | 0.29 (0.02) | 0.30 (0.13) | 0.23 (0.04) | 0.26 (0.08) | 0.23 (0.04) | 0.24 (0.04) | 0.25 (0.04) |
| 13 | 0.46 (0.05) | 0.45 (0.05) | 0.48 (0.15) | 0.42 (0.09) | 0.41 (0.07) | 0.43 (0.06) | 0.44 (0.07) | 0.46 (0.07) |
| 12 | 0.55 (0.06) | 0.56 (0.06) | 0.54 (0.08) | 0.55 (0.12) | 0.52 (0.09) | 0.52 (0.09) | 0.52 (0.08) | 0.54 (0.08) |
| 11 | 0.85 (0.1) | 0.84 (0.10) | 0.82 (0.06) | 0.89 (0.16) | 0.85 (0.13) | 0.86 (0.12) | 0.85 (0.11) | 0.87 (0.10) |
| 21 | 0.85 (0.1) | 0.85 (0.11) | 0.83 (0.04) | 0.92 (0.17) | 0.89 (0.13) | 0.89 (0.12) | 0.87 (0.12) | 0.90 (0.10) |
| 22 | 0.53 (0.07) | 0.52 (0.07) | 0.53 (0.08) | 0.57 (0.13) | 0.55 (0.10) | 0.55 (0.10) | 0.54 (0.10) | 0.55 (0.09) |
| 23 | 0.43 (0.06) | 0.43 (0.06) | 0.48 (0.17) | 0.44 (0.07) | 0.43 (0.04) | 0.44 (0.05) | 0.42 (0.05) | 0.43 (0.03) |
| 24 | 0.26 (0.05) | 0.26 (0.05) | 0.30 (0.13) | 0.22 (0.04) | 0.23 (0.04) | 0.27 (0.05) | 0.27 (0.05) | 0.27 (0.04) |
| 25 | 0.17 (0.05) | 0.17 (0.05) | 0.24 (0.12) | 0.14 (0.05) | 0.14 (0.04) | 0.19 (0.05) | 0.19 (0.05) | 0.19 (0.04) |
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | S22 16 cm | S22 20 cm | S22 24 cm | S22 28 cm | S22 32 cm |
| 15 | 0.19 (0.01) | 0.19 (0.01) | 0.23 (0.13) | 0.12 (0.02) | 0.13 (0.02) | 0.13 (0.03) | 0.15 (0.02) | 0.12 (0.03) |
| 14 | 0.29 (0.02) | 0.29 (0.02) | 0.30 (0.13) | 0.20 (0.04) | 0.21 (0.03) | 0.23 (0.04) | 0.23 (0.04) | 0.20 (0.04) |
| 13 | 0.46 (0.05) | 0.45 (0.05) | 0.48 (0.15) | 0.40 (0.06) | 0.38 (0.11) | 0.42 (0.08) | 0.42 (0.09) | 0.38 (0.08) |
| 12 | 0.55 (0.06) | 0.56 (0.06) | 0.54 (0.08) | 0.51 (0.10) | 0.51 (0.11) | 0.53 (0.10) | 0.54 (0.09) | 0.53 (0.07) |
| 11 | 0.85 (0.1) | 0.84 (0.10) | 0.82 (0.06) | 0.84 (0.13) | 0.88 (0.26) | 0.86 (0.12) | 0.87 (0.11) | 0.86 (0.10) |
| 21 | 0.85 (0.1) | 0.85 (0.11) | 0.83 (0.04) | 0.88 (0.13) | 0.87 (0.16) | 0.90 (0.12) | 0.89 (0.11) | 0.92 (0.11) |
| 22 | 0.53 (0.07) | 0.52 (0.07) | 0.53 (0.08) | 0.51 (0.12) | 0.51 (0.12) | 0.55 (0.09) | 0.54 (0.09) | 0.59 (0.10) |
| 23 | 0.43 (0.06) | 0.43 (0.06) | 0.48 (0.17) | 0.39 (0.07) | 0.39 (0.06) | 0.42 (0.04) | 0.43 (0.05) | 0.47 (0.05) |
| 24 | 0.26 (0.05) | 0.26 (0.05) | 0.30 (0.13) | 0.21 (0.04) | 0.22 (0.04) | 0.27 (0.05) | 0.29 (0.04) | 0.31 (0.04) |
| 25 | 0.17 (0.05) | 0.17 (0.05) | 0.24 (0.12) | 0.13 (0.04) | 0.14 (0.04) | 0.20 (0.04) | 0.20 (0.04) | 0.23 (0.05) |
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | S23 16 cm | S23 20 cm | S23 24 cm | S23 28 cm | S23 32 cm |
| 15 | 0.19 (0.01) | 0.19 (0.01) | 0.23 (0.13) | 0.17 (0.02) | 0.16 (0.02) | 0.18 (0.04) | 0.17 (0.04) | 0.16 (0.03) |
| 14 | 0.29 (0.02) | 0.29 (0.02) | 0.30 (0.13) | 0.23 (0.04) | 0.23 (0.05) | 0.26 (0.05) | 0.24 (0.04) | 0.29 (0.12) |
| 13 | 0.46 (0.05) | 0.45 (0.05) | 0.48 (0.15) | 0.44 (0.09) | 0.42 (0.07) | 0.46 (0.09) | 0.44 (0.08) | 0.42 (0.08) |
| 12 | 0.55 (0.06) | 0.56 (0.06) | 0.54 (0.08) | 0.57 (0.11) | 0.52 (0.07) | 0.56 (0.11) | 0.55 (0.11) | 0.55 (0.09) |
| 11 | 0.85 (0.1) | 0.84 (0.10) | 0.82 (0.06) | 0.90 (0.15) | 0.86 (0.10) | 0.87 (0.13) | 0.86 (0.12) | 0.85 (0.13) |
| 21 | 0.85 (0.1) | 0.85 (0.11) | 0.83 (0.04) | 0.92 (0.16) | 0.88 (0.11) | 0.87 (0.12) | 0.87 (0.12) | 0.87 (0.12) |
| 22 | 0.53 (0.07) | 0.52 (0.07) | 0.53 (0.08) | 0.55 (0.14) | 0.55 (0.09) | 0.55 (0.10) | 0.53 (0.09) | 0.52 (0.11) |
| 23 | 0.43 (0.06) | 0.43 (0.06) | 0.48 (0.17) | 0.42 (0.07) | 0.42 (0.04) | 0.41 (0.04) | 0.42 (0.04) | 0.41 (0.04) |
| 24 | 0.26 (0.05) | 0.26 (0.05) | 0.30 (0.13) | 0.22 (0.04) | 0.22 (0.04) | 0.26 (0.03) | 0.26 (0.04) | 0.26 (0.05) |
| 25 | 0.17 (0.05) | 0.17 (0.05) | 0.24 (0.12) | 0.13 (0.05) | 0.14 (0.04) | 0.18 (0.04) | 0.18 (0.04) | 0.19 (0.04) |
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | S24 16 cm | S24 20 cm | S24 24 cm | S24 28 cm | S24 32 cm |
| 15 | 0.19 (0.01) | 0.19 (0.01) | 0.23 (0.13) | 0.12 (0.03) | 0.13 (0.04) | 0.12 (0.04) | 0.17 (0.04) | 0.55 (0.10) |
| 14 | 0.29 (0.02) | 0.29 (0.02) | 0.30 (0.13) | 0.22 (0.04) | 0.22 (0.06) | 0.23 (0.04) | 0.26 (0.05) | 0.26 (0.04) |
| 13 | 0.46 (0.05) | 0.45 (0.05) | 0.48 (0.15) | 0.42 (0.06) | 0.41 (0.10) | 0.40 (0.05) | 0.45 (0.10) | 0.44 (0.07) |
| 12 | 0.55 (0.06) | 0.56 (0.06) | 0.54 (0.08) | 0.55 (0.10) | 0.54 (0.11) | 0.53 (0.08) | 0.55 (0.09) | 0.53 (0.09) |
| 11 | 0.85 (0.1) | 0.84 (0.10) | 0.82 (0.06) | 0.88 (0.13) | 0.87 (0.13) | 0.85 (0.13) | 0.87 (0.12) | 0.86 (0.11) |
| 21 | 0.85 (0.1) | 0.85 (0.11) | 0.83 (0.04) | 0.93 (0.15) | 0.92 (0.13) | 0.92 (0.13) | 0.89 (0.11) | 0.87 (0.13) |
| 22 | 0.53 (0.07) | 0.52 (0.07) | 0.53 (0.08) | 0.56 (0.12) | 0.55 (0.11) | 0.58 (0.12) | 0.54 (0.08) | 0.53 (0.10) |
| 23 | 0.43 (0.06) | 0.43 (0.06) | 0.48 (0.17) | 0.44 (0.06) | 0.44 (0.06) | 0.48 (0.08) | 0.42 (0.04) | 0.41 (0.05) |
| 24 | 0.26 (0.05) | 0.26 (0.05) | 0.30 (0.13) | 0.23 (0.04) | 0.23 (0.04) | 0.31 (0.05) | 0.27 (0.04) | 0.27 (0.05) |
| 25 | 0.17 (0.05) | 0.17 (0.05) | 0.24 (0.12) | 0.13 (0.04) | 0.14 (0.04) | 0.22 (0.04) | 0.18 (0.04) | 0.18 (0.05) |
| Device | ||||||||
|---|---|---|---|---|---|---|---|---|
| Teeth | Eighteeth | Desktop | Canon | Vivo 16 cm | Vivo 20 cm | Vivo 24 cm | Vivo 28 cm | Vivo 32 cm |
| 15 | 0.19 (0.01) | 0.19 (0.01) | 0.23 (0.13) | 0.11 (0.02) * | 0.10 (0.02) * | 0.12 (0.02) * | 0.13 (0.03) * | 0.14 (0.04) * |
| 14 | 0.29 (0.02) | 0.29 (0.02) | 0.30 (0.13) | 0.20 (0.04) * | 0.20 (0.03) * | 0.22 (0.04) * | 0.23 (0.04) * | 0.23 (0.04) * |
| 13 | 0.46 (0.05) | 0.45 (0.05) | 0.48 (0.15) | 0.40 (0.08) | 0.39 (0.06) | 0.42 (0.07) | 0.41 (0.06) | 0.42 (0.07) |
| 12 | 0.55 (0.06) | 0.56 (0.06) | 0.54 (0.08) | 0.50 (0.10) | 0.50 (0.09) | 0.51 (0.08) | 0.52 (0.08) | 0.52 (0.08) |
| 11 | 0.85 (0.1) | 0.84 (0.10) | 0.82 (0.06) | 0.85 (0.12) | 0.84 (0.12) | 0.86 (0.10) | 0.85 (0.09) | 0.85 (0.11) |
| 21 | 0.85 (0.1) | 0.85 (0.11) | 0.83 (0.04) | 0.89 (0.11) | 0.92 (0.11) | 0.91 (0.11) | 0.90 (0.10) | 0.85 (0.12) |
| 22 | 0.53 (0.07) | 0.52 (0.07) | 0.53 (0.08) | 0.55 (0.09) | 0.57 (0.09) | 0.56 (0.10) | 0.56 (0.09) | 0.54 (0.09) |
| 23 | 0.43 (0.06) | 0.43 (0.06) | 0.48 (0.17) | 0.43 (0.05) | 0.46 (0.05) | 0.45 (0.04) | 0.43 (0.04) | 0.44 (0.04) |
| 24 | 0.26 (0.05) | 0.26 (0.05) | 0.30 (0.13) | 0.22 (0.04) | 0.22 (0.04) | 0.28 (0.05) | 0.29 (0.03) | 0.28 (0.05) |
| 25 | 0.17 (0.05) | 0.17 (0.05) | 0.24 (0.12) | 0.13 (0.04) | 0.26 (0.27) | 0.21 (0.05) | 0.20 (0.03) | 0.19 (0.04) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hasbini, O.; Bourgi, R.; Kharouf, N.; Cuevas-Suárez, C.E.; Kharma, K.; Moussa, C.; Nassar, N.; Osman, A.; Lukomska-Szymanska, M.; Haikel, Y.; et al. Digital Dentistry and Imaging: Comparing the Performance of Smartphone and Professional Cameras for Clinical Use. Prosthesis 2025, 7, 77. https://doi.org/10.3390/prosthesis7040077
Hasbini O, Bourgi R, Kharouf N, Cuevas-Suárez CE, Kharma K, Moussa C, Nassar N, Osman A, Lukomska-Szymanska M, Haikel Y, et al. Digital Dentistry and Imaging: Comparing the Performance of Smartphone and Professional Cameras for Clinical Use. Prosthesis. 2025; 7(4):77. https://doi.org/10.3390/prosthesis7040077
Chicago/Turabian StyleHasbini, Omar, Rim Bourgi, Naji Kharouf, Carlos Enrique Cuevas-Suárez, Khalil Kharma, Carol Moussa, Nicolas Nassar, Aly Osman, Monika Lukomska-Szymanska, Youssef Haikel, and et al. 2025. "Digital Dentistry and Imaging: Comparing the Performance of Smartphone and Professional Cameras for Clinical Use" Prosthesis 7, no. 4: 77. https://doi.org/10.3390/prosthesis7040077
APA StyleHasbini, O., Bourgi, R., Kharouf, N., Cuevas-Suárez, C. E., Kharma, K., Moussa, C., Nassar, N., Osman, A., Lukomska-Szymanska, M., Haikel, Y., & Hardan, L. (2025). Digital Dentistry and Imaging: Comparing the Performance of Smartphone and Professional Cameras for Clinical Use. Prosthesis, 7(4), 77. https://doi.org/10.3390/prosthesis7040077













