Abstract
Objectives: This systematic review aimed to evaluate the cost, production time, clinical performance, and patient satisfaction of 3D printing workflows in prosthodontics compared to conventional and subtractive methods. Methods: Following PRISMA guidelines, a systematic search of electronic databases was performed to identify studies published between 2015 and 2025 that directly compared digital additive workflows with analogue or subtractive workflows. Studies were eligible if they included prosthodontic treatments such as dentures, crowns, or implant-supported prostheses and reported at least one relevant outcome. The primary outcomes were cost, time efficiency, clinical accuracy (e.g., marginal adaptation, fit), and patient satisfaction. Included studies were methodologically evaluated using MINORS scale and the risk of bias was assessed using ROBINS-I and RoB 2 tools. Results: Seven studies met the inclusion criteria. Overall, 3D printing workflows demonstrated reduced production time and cost in comparison to conventional or subtractive methods. Clinical outcomes were generally comparable or superior, particularly regarding adaptation and fit. Patient satisfaction was favourable in most studies, although reporting varied. Long-term follow-up was limited, which constrains the interpretation of sustained clinical performance. Conclusions: These findings suggest that 3D printing can serve as an efficient and cost-effective alternative in prosthodontic fabrication, with clinical results comparable to those already established. Further research is needed to assess long-term clinical performance and cost-effectiveness in various clinical scenarios.
1. Introduction
Digital dentistry, particularly 3D printing, has emerged as a promising alternative to traditional analogue techniques and subtractive manufacturing methods [1]. While conventional methods rely on manual labour and skilled technicians, digital workflows improve production, minimize manual intervention, and potentially reduce errors [2]. 3D printing offers several advantages over subtractive methods, including less material waste and lower equipment costs [3,4]. However, the decision between digital and analogue methods is deeply intertwined with economic considerations [5]. Digital protocols, despite considerable upfront investments, often promise long-term savings through automation, reduced material waste, and faster turnaround times [6]. The emergence of computer-aided design and computer-aided manufacturing (CAD-CAM) has changed how impressions are captured and prosthetic restorations are designed. This technology has been gradually moving to the mainstream of dentistry over the last twenty-five years. Implementation of digital systems utilizing in-house, chairside CAD/CAM technology may create cost savings for clinical programmes in dental settings [7,8]. Recent advancements have enabled the introduction of 3D printers for producing chairside definitive fixed restorations in new materials, such as new-generation hybrid composites filled with ceramics [9,10]. However, the literature on chairside additive technology and new 3D-printed hybrid composites is relatively scarce due to their recent introduction. In the field of removable prosthetics, digital denture technology has been refined and accepted by most dentists, making milled and printed complete dentures not only possible but potentially reducing the overall costs [11]. Both milled and 3D-printed complete removable dental prostheses (CRDPs) are now considered valid treatment modalities for edentulous patients [12,13]. Economic analyses of these digital workflows are important for dental practices striving to balance high-quality care with cost containment. Understanding the cost-effectiveness and profitability of implementing digital technologies for removable complete dentures is vital for clinical decision-making. For example, recent studies found that digital workflows utilizing resin not only reduced production time but also significantly lowered material wastage, leading to overall cost savings in high-volume practices [7,11,14]. Several studies [12,15] illustrated that digital manufacturing techniques deliver enhanced precision and reproducibility, which correlates with lower rates of prosthesis failure and fewer costly remakes. Additional papers, including those by Fouda et al. (2024) and Jafarpour et al. (2024), have emphasized that digital protocols streamline workflows and reduce labour-related costs, reinforcing their potential for long-term economic benefit [10,16]. Evaluating the cost-effectiveness of 3D printing protocols in dental prosthodontics involves assessing multiple factors such as production efficiency, material costs, laboratory expenses, and waste reduction. For example, a paper published in 2024 illustrated that while digital protocols require significant initial investment, their operational efficiency (such as reduced turnaround times and lower error rate) can lead to substantial long-term savings [9]. However, the reliability of analogue methods continues to make them a viable option in scenarios where digital infrastructure is either unavailable or impractical [1,2,12,16,17,18]. The practical implications of these findings extend well beyond academic debate. In an era of increasing financial pressures on dental practices, it is very important to determine the most cost-effective manufacturing protocol. The decision to invest in digital technology must balance the promise of enhanced precision and reduced material waste with the overall financial sustainability of the practice [16,19,20]. At the same time, the continued relevance of analogue methods in certain contexts suggests that, in some cases, a hybrid approach might offer the optimal balance between innovation and tradition [10,21]. Digital workflows have made it possible to fabricate a variety of prosthodontic structures, such as crowns, removable full dentures, provisional restorations, and implant-supported overdentures. These advancements have the potential to improve accuracy, reduce production time, and streamline dental care. Therefore, this review was conducted to evaluate and compare the cost, production time, clinical outcomes, and patient satisfaction associated with 3D printing workflows versus conventional and subtractive manufacturing methods in fixed and removable prosthodontics.
2. Materials and Methods
This systematic review was conducted in accordance with the PRISMA 2020 guidelines [22] and the completed PRISMA checklist is provided in the Supplementary Materials. The selection of studies was conducted using the following electronic databases, PubMed-Medline, Scopus, and Google Scholar, to identify articles published from January 2015 to February 2025. The research question was the following: “In dental prosthodontic manufacturing, how do digital protocols for resin and metal 3D printing compare to analogue protocols in terms of cost-effectiveness?” The PICO process is presented in Table 1. The keywords used for the search query were as follows: (Digital OR Computerized OR CAD CAM) AND (Dentistry OR Prosthodontics OR Implantology) AND (Cost OR Time OR Efficiency). Additionally, the reference lists of all included articles were screened manually. No new eligible studies were found. The papers were screened using the following criteria: dental application, protocol comparison, and 3D printing materials (Table 2). Inclusion criteria were articles written in English, published from January 2015 to February 2025, that compared the analogue protocol with the digital one with regard to, primarily, the cost efficiency and, secondly, time efficiency. Studies that were limited to in vitro experiments, technical notes, or descriptions of workflow feasibility without patient-level data were not considered. Additionally, case reports, conference abstracts, narrative reviews, and editorials were also excluded as they typically do not provide structured comparisons or measurable outcomes necessary for synthesis. Studies were only eligible if they included clinically relevant data and addressed at least one of the predefined outcome categories. To evaluate the methodological quality of the selected studies, the MINORS (Methodological Index for Non-Randomized Studies) tool was applied. This validated instrument is widely used for assessing the quality of non-randomized and comparative clinical studies. The tool comprises 12 criteria—8 core items for all studies and 4 additional items for comparative studies. Each item was scored as 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate), with a maximum total score of 24 points for comparative studies [17]. While the MINORS tool was used to assess methodological quality across all included studies for consistency, it should be noted that this instrument was originally validated for non-randomized studies only [17]. Therefore, results for randomized studies should be interpreted with caution, and the RoB 2 tool was additionally applied for rigorous bias assessment in randomized trials. To evaluate the methodological rigour and potential for bias in the included studies, two validated instruments developed by the Cochrane Collaboration were used: the RoB 2 tool for randomized controlled trials (RCTs) [23] and the ROBINS-I (Risk Of Bias In Non-randomized Studies of Interventions) tool for non-randomized studies [24]. The RoB 2 tool assesses bias across the following five domains: the randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Each domain is rated as low risk, some concerns, or high risk, culminating in an overall risk of bias judgement. For non-randomized studies, the ROBINS-I tool was applied to examine the following seven domains: bias due to confounding, participant selection, classification of interventions, deviations from intended interventions, missing data, outcome measurement, and selection of reported results. These tools were selected to ensure transparent and domain-specific risk assessment, allowing appropriate interpretation of the internal validity of both randomized and observational evidence. The extracted variables were defined as follows: (1) cost referred to direct manufacturing expenses, including material, labour, and equipment use; (2) production time described the duration from initial impression or scan to final delivery; (3) clinical outcomes included measures such as marginal fit, adaptation, and clinical success; and (4) patient satisfaction reflected the subjective perception of comfort, aesthetics, and functional quality reported by participants. The present review was conducted by four reviewers, following the PRISMA and strengthening the reporting of observational studies in epidemiology (STROBE) guidelines. The searches were conducted electronically and manually, being verified by three individuals, and EndNote X9 (Clarivate, Philadelphia, PA, USA) software was used for the organization of references and the elimination of duplicates. During the preparation of this work the authors used ChatGPT 4.0 (OpenAI, San Francisco, CA, USA) and Elicit Pro (Elicit, Oakland, CA, USA), accessed on 27 April 2025, in order to generate figures, improve the readability of the text, and refine the data extracted. After using these tools, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication. All monetary values reported in EUR and CHF were converted to USD using 2025 average exchange rates of EUR 1 = USD 1.15 and CHF 1 = USD 1.23. These rates were based on publicly available forex data as of June 2025.

Table 1.
PICO framework.

Table 2.
Inclusion criteria.
3. Results
3.1. Selection of the Studies
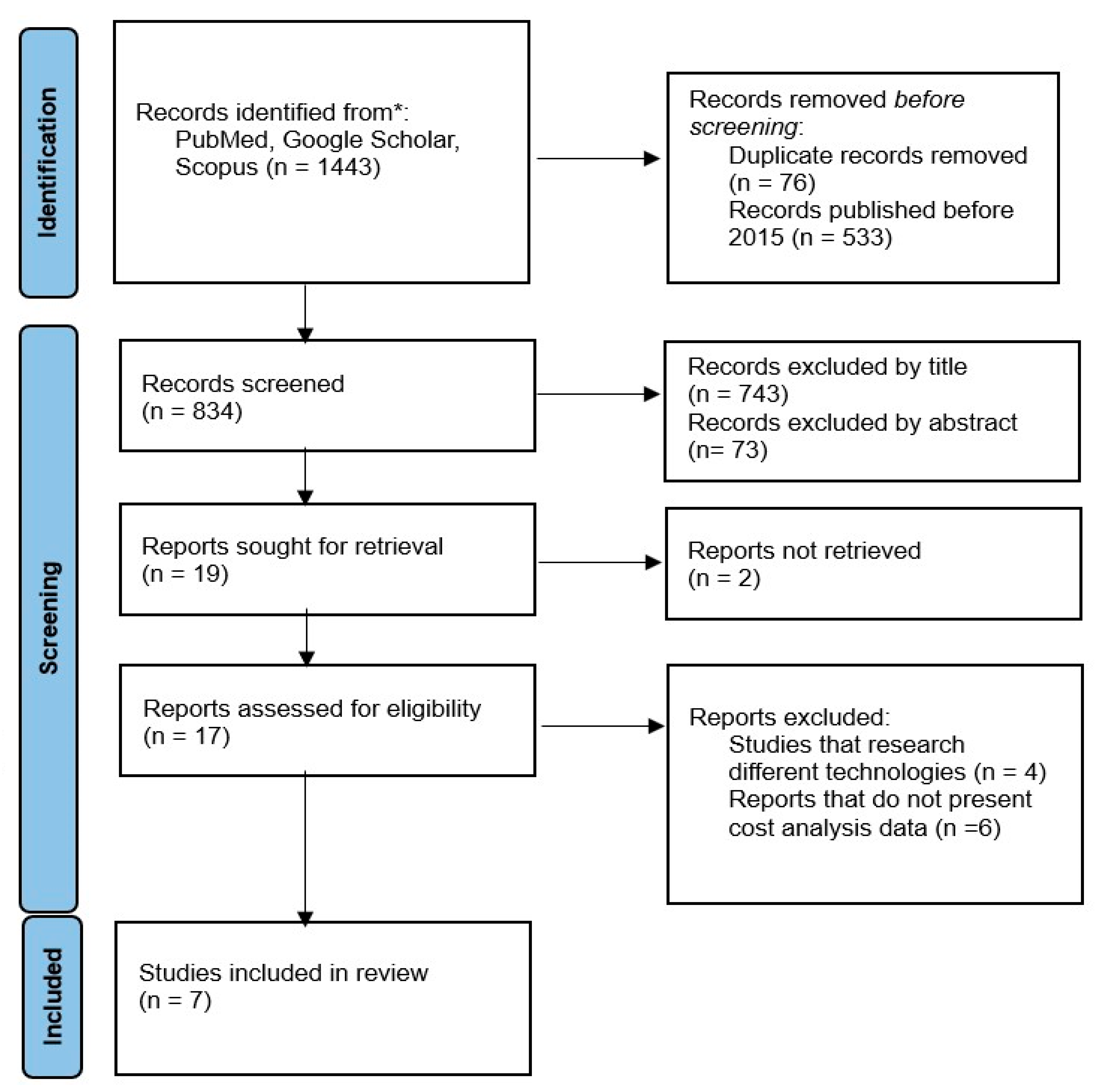
The initial search resulted in the identification of 1443 studies, with 910 of them published after January 2015. After the removal of the duplicates, 834 records remained. Following the screening by titles, 743 studies were eliminated. Out of the remaining 91 studies, 73 were excluded after reading the abstract and 10 more after reading the full text. Two papers could not be retrieved. Discrepancies between the authors of the present review were managed through discussions and consultation, the agreement between the authors being materialized by a kappa coefficient (Cohen) of 0.96, which indicates a high degree of consensus between them. Finally, seven studies were included in this review (Figure 1). The seven included studies differed in their design and the types of prostheses they examined. Most focused on removable complete dentures or implant-supported overdentures, comparing 3D-printed workflows with conventional or subtractive digital protocols.
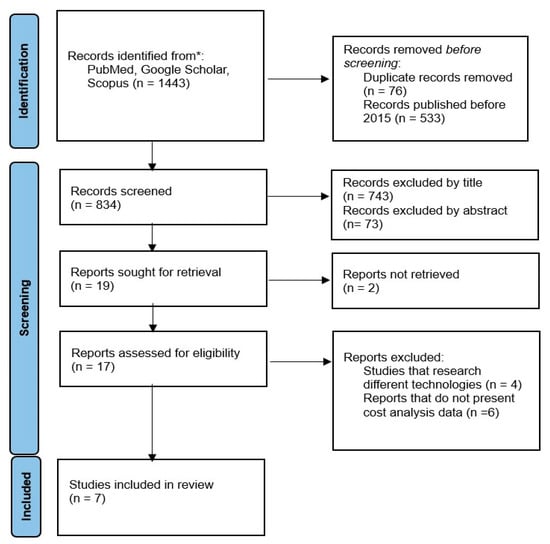
Figure 1.
PRISMA process diagram. * Records were retrieved from PubMed, Google Scholar, and Scopus. Searches were limited to studies published from January 2015 onward. Reference lists of eligible studies were manually screened to identify additional relevant records.
3.2. Evaluation of the Included Studies
The methodological quality of the included studies was evaluated using the MINORS tool. Table 3 summarizes the individual scoring of seven included studies across all MINORS criteria. All seven studies were comparative in nature and therefore assessed using the full 12-item MINORS criteria, with a maximum score of 24. Overall, the studies demonstrated moderate to high methodological quality, with total scores ranging from 20 to 22 out of 24. The highest score was achieved by Srinivasan et al. (23/24) [13], followed by Daher et al. [9] and Van der Winkel et al. (22/24) [25]. The studies generally exhibited strong methodological rigour, particularly in areas such as prospective data collection, appropriate endpoint selection, and group comparability. Most studies effectively controlled for confounding factors through well-defined comparative designs, ensuring baseline equivalence between intervention and control groups. Additionally, the use of contemporary patient cohorts and appropriate statistical analyses enhanced the reliability of the reported findings. Most studies scored well in criteria such as clearly stated aims, prospective data collection, adequate control groups, and baseline equivalence of groups. However, two recurring limitations observed across the included studies warrant consideration. First, the lack of prospective sample size calculation raises questions about the statistical power of some findings, particularly in studies assessing cost-effectiveness outcomes where variability in cost inputs can be substantial. Second, inadequate reporting of blinding procedures in endpoint assessment introduces the possibility of detection bias, especially for subjective measures like satisfaction or perceived efficiency. Furthermore, the six non-randomized studies were assessed with ROBINS-I across seven bias domains. Most studies demonstrated a moderate overall risk of bias, primarily due to potential confounding factors and a lack of blinding during outcome assessment. Notably, the in vitro studies (Mangano et al., 2024 [26]; Daher et al., 2022 [9]; No-Cortes et al., 2021 [27]) displayed low to moderate risk, reflecting the advantages of highly controlled experimental conditions. In addition, the randomized controlled trials by Van de Winkel et al. (2025) [25] and Srinivasan et al. (2021) [13] were assessed separately using the RoB 2 tool, showing an overall low risk of bias, with minor concerns noted regarding the blinding of outcome assessment. Table 3 and Table 4 summarize the ROBINS-I bias judgments and MINORS quality scores for the non-randomized studies, and Table 5 presents the RoB 2 assessment of the randomized trials. Following this detailed methodological appraisal, synthesis of study outcomes was performed with consideration of the observed strengths and potential limitations identified during the risk of bias assessment. The high methodological rigour observed across most of the included studies provides a solid foundation for interpreting the clinical and economic findings reported in the subsequent sections.

Table 3.
MINORS scale study quality assessment. Each criterion is scored either 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate), with a maximum score of 24.

Table 4.
ROBINS-I risk of bias assessment.

Table 5.
RoB 2 assessment for RCTs.
3.3. Methodological Framework and Study Characteristics
The systematic review identified seven studies comparing only 3D printing manufacturing or different types of workflows including 3D printing with analogue and/or digital subtractive protocols. The methodological framework of the reviewed studies encompassed diverse study designs, including two economic modelling studies, two randomized controlled trials, and three laboratory-based comparative in vitro studies. The studies primarily investigated digital technologies, including 3D printing, milling, and general digital procedures, compared against conventional or analogue methods. Sample sizes varied considerably, ranging from 15 to 50 patients in the clinical studies, while follow-up periods spanned from 6 weeks to 1 year. Three studies focused on economic modelling and laboratory analysis did not require follow-up periods, while one study did not provide follow-up information in the available data (Table 6). Among the included studies, various 3D printing methods were utilized, primarily stereolithography (SLA), digital light processing (DLP), and selective laser sintering (SLS). To aid the interpretation of reported economic outcomes, Appendix A provides a comparative overview of their approximate costs, clinical applications, and workflow characteristics based on synthesis of the included studies.

Table 6.
Characteristics of included studies.
3.4. Economic Outcomes
3D printing technology has demonstrated significant economic advantages in dental prosthetics (Table 7). For complete dentures, Lo Russo et al. [21] found that fully digital workflows, including 3D printing, provided an additional USD 34 reduction in costs compared to mixed digital–analogue workflows. In a dental school setting, transitioning to digital denture fabrication, which includes 3D printing options, could save USD 119,332 to USD 179,588 over a 10-year period with a volume of 400 dentures/year. [28]. Srinivasan et al. reported that the total costs for a digital denture protocol, which incorporated 3D printing, were significantly lower than for the conventional protocol (EUR 4030.61 (≈USD 4635.2) vs. EUR 4700.33 (≈USD 5405.38) p < 0.001) [11]. For single crowns, Mangano et al. found that additive chairside methods, which utilize 3D printing, had the lowest cost at EUR 8 (≈USD 9.2) per crown, compared to EUR 29 (≈USD 33.35) for subtractive chairside and EUR 8.1 (≈USD 9.4), for lab-based subtractive methods [26]. Daher et al. provided even more striking evidence, reporting that 3D printing was 5.5, 8.7, and 10.2 times less expensive than PMMA, milled composite, and lithium disilicate, respectively [9]. Initial equipment investments for 3D printing systems were generally lower than other digital methods. Lo Russo et al. found that fully digital workflows, which include 3D printing options, required initial investments ranging from USD 14,950 to 67,275, while mixed workflows ranged from USD 28,750 to 81,075, with the break-even analysis revealing that fully digital workflows, including 3D printing, required fewer cases to recoup initial investments. They calculated that 73–534 dentures were needed for fully digital workflows, compared to 170–933 dentures for mixed digital workflows [21]. Mangano et al. found that additive methods required only 90 min to produce 10 crowns, compared to 450 min for subtractive methods and 930 min for conventional production; meanwhile, Daher et al. noted that this efficiency advantage becomes apparent when producing more than eight restorations at a time [9,22]. Regarding material costs and efficiency, Daher et al. found that the waste factor for 3D printing (73%) was not considerably less than for milled restorations (90%), contradicting previous assumptions about material efficiency in additive manufacturing. However, the overall cost savings still favoured 3D printing due to lower material costs and increased production efficiency [27]. In terms of maintenance and adjustments, Srinivasan et al. reported that 3D-printed CRDPs required more maintenance visits and adjustment time (p = 0.0003), with higher adjustment costs (p = 0.021) compared to milled CRDPs [11]. However, for implant-supported overdentures, Van der Winkel et al. found no significant differences in repair time or costs between milled and 3D-printed prostheses [25]. Patient willingness to pay for 3D-printed prostheses was slightly lower than for milled prostheses, but still higher than conventional methods [23]. Srinivasan et al. found that patients were willing to pay CHF 2593.33 ± 773.18 (USD 2000–USD 4000) for 3D-printed CRDPs, compared to CHF 3200.00 ± 1211.85 (USD 2000–USD 7000) for milled CRDPs [11]. On a broader economic scale, Van der Winkel et al. estimated that implementing 3D-printed implant-supported overdentures could save approximately EUR 48,285,973 (USD 55,648,234) annually in the Dutch healthcare system. They also calculated that the productivity loss caused by treatment sessions and travel time was substantially lower for 3D-printed implant-supported overdentures (EUR 383.47 (≈USD 440.99)) compared to conventional methods (EUR 991.89 (≈USD 1140.67)) [25].

Table 7.
Direct manufacturing costs.
3.5. Clinical Outcomes and Quality Metrics
Clinical success rates were comparable between digital and conventional methods, with studies reporting 92% success rates for both approaches and 100% survival rates in long-term follow-up [9,13,25,27]. Manufacturing accuracy measurements demonstrated high precision across different digital methods, with additive manufacturing achieving 16.80 μm (±2.42) accuracy, subtractive methods showing 29.56 μm (±4.16), and lab-based processes achieving 14.81 μm (±2.27) [26,27]. In a clinical evaluation, marginal closure, interproximal contact, and occlusal contact did not differ significantly between additive chairside, subtractive chairside, and laboratory-based subtractive manufacturing workflows. Patient satisfaction with digital dentures was consistently high. In another paper, a mean marginal trueness of 26.05 μm (±2.70), 46.80 μm (±6.39), and 21.57 μm (±2.57) was found for crowns manufactured using additive chairside, subtractive chairside, and subtractive lab-based technology, respectively [9].
3.6. Time Efficiency and Workflow Analysis
Digital protocols demonstrated significant time savings across all procedural steps (Table 8). Mangano et al. found that digital impression-taking required 20 ± 5 min versus 50 ± 7 min for conventional methods, while provisional restoration fabrication reduced from 340 ± 37 min to 70 ± 15 min [26]. Manufacturing efficiency for multiple units showed marked improvements, with additive digital methods requiring 90 min and subtractive methods 450 min for ten crowns, compared to 930 min for conventional production. Total clinical time requirements decreased substantially, with reductions from 10.73 to 6.85 h and from 309 to 182 min reported in different studies [23,24]. Visit requirements were consistently lower with digital protocols, reducing from 5–6 conventional visits to 2–4 digital visits. One study documented a reduction from five visits requiring 8 h to four visits requiring 7 h, while another achieved a reduction to just two visits with the digital protocol [28]. For complete dentures, Lo Russo et al. reported that digital workflows significantly reduced manufacturing time by 5.90 to 7.35 h per denture, decreasing opportunity costs [21]. Srinivasan et al. found that the total costs for a digital denture protocol were significantly lower than for the conventional protocol (EUR 4030.61 (≈USD 4635.2) vs. EUR 4700.33 (≈USD 5405.38) p < 0.001 [11]).

Table 8.
Time efficiency metrics.
3.7. Patient-Centred Outcomes
Patient satisfaction metrics showed favourable results for digital protocols. Comfort during impression-taking was notably higher with digital methods, though one study found no significant difference in overall quality of life measures [25]. Patient satisfaction was consistently high across digital protocols, suggesting good acceptability of these new technologies [13,21]. The reduced number of visits and shorter treatment times contributed to positive patient experiences, though specific satisfaction metrics varied across studies. One study revealed that digital workflows for fabricating complete removable dental prostheses (removable dental prostheses) were consistently more cost-effective and efficient than conventional analogue methods. Workflow M (mixed analogue–digital) allowed variable cost savings between USD 81 and 169 per denture compared to conventional methods, while workflow D (fully digital) allowed for an additional saving of USD 34 [21].
4. Discussion
This review found that digital workflows, especially those using 3D printing, are generally more cost-effective and time-efficient than traditional or subtractive methods in prosthodontics. This synthesis is further supported by the cost and workflow differences between the major 3D printing technologies used, which are detailed in Appendix A. These differences help explain the variations in reported economic outcomes across the included studies. Across the included studies, 3D printing showed clear advantages in reducing production time, lowering material costs, and minimizing the number of patient visits. However, it is important to look deeper into these findings to understand what they really mean for dental professionals. One major point is that not all digital technologies work the same. SLA (stereolithography), DLP (digital light processing), and SLS (selective laser sintering) each have different strengths, costs, and learning curves. For example, DLP systems are often faster and easier to maintain, which makes them useful for clinics needing quick turnarounds [1,29]. SLA systems, while generally slower, offer better surface detail, which can be helpful in crown and bridge work [2,30]. SLS machines are more expensive and usually better suited for complex frameworks or larger-scale labs [8]. These differences are not clearly separated in some studies, which can make it hard to compare outcomes directly. It would help if future research specified exactly which technology was used, along with the costs and limitations. The cost data included in the studies shows that 3D printing can save money, but the savings depend heavily on volume. Practices that produce a high number of dentures or crowns benefit the most because the equipment and software costs are spread across many cases. For smaller practices, the initial investment in printers, design software, and training may take longer to pay off. These numbers highlight that while digital tools can offer savings, they are best suited to clinics or labs that handle a steady patient load. Some studies also did not account for hidden costs like machine maintenance, technician training, software upgrades, and reprints due to print failures [9,25]. These issues are part of daily clinical work and can affect the overall cost and efficiency of a system. For example, SLA systems often require careful post-processing, including washing, curing, and removing supports, which takes time and increases labour [31]. Subtractive methods create more waste but may be more reliable for single-unit production. From a clinical standpoint, the review showed that digital and conventional prostheses perform similarly in terms of fit, success rate, and patient satisfaction. Most patients reported high comfort and fewer visits with digital workflows. However, one study did find that 3D-printed dentures needed more maintenance and adjustments than milled ones, especially over time. These findings suggest that while digital workflows are generally effective, the final quality may also depend on technician skill, equipment calibration, and quality control practices. Many of the included studies had short follow-up periods, often less than one year. That makes it hard to judge long-term durability or complication rates. Also, only a few studies looked at full-arch restorations, implant-supported dentures, or complex cases. Most of the data is based on single crowns or removable dentures, which means that the results may not apply to all treatment types.
The findings of this systematic review are largely consistent with and complementary to those reported in other recent systematic reviews on the topic. This is, however, the first systematic review that uses cost as the primary variable taken into account. The emergence of 3D printing as a particularly cost-effective and efficient option for denture fabrication is a significant development. The ability to print multiple restorations simultaneously offers a level of scalability that could be particularly beneficial for high-volume practices or dental laboratories. One systematic review on time efficiency and cost of fabricating removable complete dentures using digital, hybrid, and conventional workflows provides additional support for the advantages of digital methods. This review together with Bessadet et al. and Tew et al. found that digital workflows consistently reduced clinical times and costs compared to conventional methods [5,19]. This is consistent with the time savings for impression-taking reported in our review, further emphasizing the efficiency gains of digital workflows in the initial stages of prosthodontic treatment. However, they also noted that for complete arch scans, some studies found digital methods to be more time-consuming than conventional impressions. Regarding laboratory procedures, the literature corroborates our findings of significant time savings with digital methods [19,32]. They reported that the total working time for dental technicians was considerably shorter for digital workflows compared to conventional ones, regardless of the specific CAD-CAM system used. This reinforces the potential for digital workflows to improve laboratory efficiency and reduce production costs. In terms of clinical evaluation and chairside adjustments, El Osta et al. found mixed results, with some studies reporting no significant difference in treatment times between digital and conventional workflows. This contrasts somewhat with our findings of consistent time savings in clinical procedures with digital methods. This discrepancy may be due to differences in the specific technologies and protocols used in the studies included in each review, highlighting the need for standardized research methodologies in this field. Three systematic reviews on time efficiency and cost analysis between digital and conventional workflows for fixed dental prostheses provides further context for our findings [2,5,19]. This consistency across multiple systematic reviews strengthens the overall evidence supporting the efficiency and cost-effectiveness of digital prosthodontic workflows. This cost advantage is particularly important given the rising healthcare costs and the need for more affordable dental care options. The significant reduction in manufacturing time and clinical visits is another crucial advantage of digital workflows. This increased efficiency could allow dental practices to treat more patients, potentially reducing wait times and improving access to care [33,34,35,36,37]. The comparison between milled and 3D-printed removable dental prostheses revealed interesting insights. The comparable or superior marginal adaptation of 3D printed restorations to milled alternatives is a finding that addresses potential concerns about the quality of digitally fabricated prostheses [9,27]. The high levels of patient satisfaction reported with digital dentures are encouraging and suggest that these new technologies can meet or exceed patient expectations [36,38,39,40]. The preference for digital impressions over conventional ones, with patients reporting less discomfort and a lower likelihood of experiencing gag reflex, indicates that digital workflows can contribute to a more positive patient experience. While this review did not provide specific data on training times, it acknowledged that additional time and resources may be required for staff to become proficient with new technologies. This systematic review has several limitations that should be considered when interpreting its findings. Some included studies had methodological limitations, particularly in blinding procedures and sample size calculations, which may affect the robustness of their results. The review primarily focused on data from small dental practices and laboratories, potentially limiting generalizability to larger-scale operations. The rapid evolution of digital technologies in dentistry means that some findings may become outdated quickly, necessitating ongoing research and updates. Heterogeneity in study designs, specific digital technologies used, and outcome measures across the included studies presented challenges in directly comparing results. The economic analyses were based on specific geographic locations and healthcare systems, primarily in Europe and North America, which may limit applicability to other regions with different economic contexts. While the findings of this review support the cost and time advantages of 3D printing in prosthodontics, the relatively small number of included studies and the alignment with expected trends highlight the need for further longitudinal research to strengthen and diversify the evidence. The review lacked comprehensive long-term clinical data on the performance and durability of digitally manufactured prostheses over extended periods. Additionally, the inclusion of studies using various digital systems and workflows, each with potentially different learning curves, efficiencies, and cost structures, may have introduced variability in the reported outcomes. The absence of standardized research methodologies and outcome measures across studies in this field made direct comparisons challenging. These limitations highlight the need for further research with standardized protocols, longer follow-up periods, and broader geographic representations to strengthen the evidence base for digital workflows in prosthodontics.
5. Conclusions
This systematic review provides strong evidence supporting the cost-effectiveness and time efficiency of digital workflows in dental prosthodontic manufacturing. Digital protocols consistently demonstrated lower direct costs, shorter production times, and fewer patient visits compared to traditional analogue methods. Clinical outcomes and patient satisfaction were comparable or favoured digital approaches. The adoption of digital workflows, particularly those incorporating 3D printing, represents a promising opportunity to enhance the accessibility and affordability of prosthodontic treatments. However, the significant initial investment required for digital equipment necessitates careful consideration of practice volume and long-term cost savings. As digital technologies continue to advance, their integration into dental education and practice will likely become increasingly important for delivering efficient, high-quality prosthodontic care.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/prosthesis7040078/s1. PRISMA 2020 Checklist.
Author Contributions
Conceptualization, M.P., V.S.P. and A.V.; methodology, M.B.; software, A.B.; validation, D.-C.P., M.A.M. and R.C.C.; formal analysis, R.M.C.; investigation, A.V.; resources, A.A.Ș.; data curation, M.A.Ș. and A.C.D.; writing—original draft preparation, M.P.; writing—review and editing, M.B., L.B. and A.C.D.; visualization, M.A.M.; supervision, V.S.P. and L.B.; project administration, M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding authors.
Acknowledgments
During the preparation of this work the authors used ChatGPT (OpenAI, San Francisco, CA, USA) and Elicit (Elicit, Oakland, CA, USA) in order to generate figures, improve the readability of the text, and refine the data extracted. After using these tools, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Comparative overview of 3D printing technologies.
Table A1.
Comparative overview of 3D printing technologies.
| Technology | Printer Cost (USD) | Material Cost per Unit | Print Speed | Clinical Use Case | Key Advantages | Main Limitations |
|---|---|---|---|---|---|---|
| SLA (Stereolithography) | USD 2000–15,000 | USD 3–6 | Moderate (45–90 min/unit) | Crowns, bridges, and precision parts | High accuracy and fine detail | Requires post-processing (curing and cleaning) and is slower for volume |
| DLP (Digital Light Processing) | USD 3000–20,000 | USD 2.50–5 | Fast (30–60 min/unit) | Chairside applications and dentures | Fast printing and good detail | Surface quality may be slightly lower than SLA |
| SLS (Selective Laser Sintering) | USD 10,000–100,000+ | USD 8–15 | Moderate–fast | Frameworks, splints and RPDs | No support needed and strong parts | High cost, complex maintenance and not widely used chairside |
Data compiled from literature sources and 2025 manufacturer pricing estimates [6,29,30,41].
References
- Alyami, M.H. The applications of 3D-printing technology in prosthodontics: A review of the current literature. Cureus 2024, 16, e68501. [Google Scholar] [CrossRef] [PubMed]
- Anadioti, E.; Musharbash, L.; Blatz, M.B.; Papavasiliou, G. 3D printed complete removable dental prostheses: A narrative review. BMC Oral Health 2020, 20, 343. [Google Scholar] [CrossRef]
- Joda, T.; Brägger, U. Time-Efficiency Analysis Comparing Digital and Conventional Workflows for Implant Crowns: A Prospective Clinical Crossover Trial. Int. J. Oral Maxillofac. Implant. 2015, 30, 1047–1053. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A.; Singh, R.P.; Suman, R.; Rab, S. Role of additive manufacturing applications towards environmental sustainability. Adv. Ind. Eng. Polym. Res. 2021, 4, 312–322. [Google Scholar] [CrossRef]
- Bessadet, M.; Drancourt, N.; El Osta, N. Time efficiency and cost analysis between digital and conventional workflows for the fabrication of fixed dental prostheses: A systematic review. J. Prosthet. Dent. 2025, 133, 71–84. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Gandolfi, A.; Luongo, G.; Logozzo, S.; Mangano, C. Intraoral scanners in dentistry: A review of the current literature. BMC Oral Health 2020, 17, 149. [Google Scholar] [CrossRef]
- El Osta, N.; Bessadet, M.; Drancourt, N. Time efficiency and cost of fabricating removable complete dentures using digital, hybrid, and conventional workflows: A systematic review. J. Prosthet. Dent. 2025, 133, 1194–1208. [Google Scholar] [CrossRef] [PubMed]
- Barbin, T.; Velôso, D.V.; Del Rio Silva, L.; Borges, G.A.; Presotto, A.G.C.; Barão, V.A.R.; Mesquita, M.F. 3D metal printing in dentistry: An in vitro biomechanical comparative study of two additive manufacturing technologies for full-arch implant-supported prostheses. J. Mech. Behav. Biomed. Mater. 2020, 108, 103821. [Google Scholar] [CrossRef]
- Daher, R.; Ardu, S.; di Bella, E.; Krejci, I.; Duc, O. Efficiency of 3D printed composite resin restorations compared with subtractive materials: Evaluation of fatigue behavior, cost, and time of production. J. Prosthet. Dent. 2024, 131, 943–950. [Google Scholar] [CrossRef]
- Fouda, A.; Tonogai, J.; McDermott, P. A systematic review on patient perceptions and clinician-reported outcomes when comparing digital and analog workflows for complete dentures. J. Prosthodont. 2024, 1–20. [Google Scholar] [CrossRef]
- Srinivasan, M.; Schimmel, M.; Naharro, M.; Neill, C.O.; McKenna, G.; Müller, F. CAD/CAM milled removable complete dentures: Time and cost estimation study. J. Dent. 2019, 80, 75–79. [Google Scholar] [CrossRef]
- Alotaibi, H.N. Patient Satisfaction with CAD/CAM 3D-Printed Complete Dentures: A Systematic Analysis of the Clinical Studies. Healthcare 2025, 13, 388. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Kalberer, N.; Fankhauser, N.; Naharro, M.; Maniewicz, S.; Müller, F. CAD-CAM complete removable dental prostheses: A double-blind, randomized, crossover clinical trial evaluating milled and 3D-printed dentures. J. Dent. 2021, 115, 103842. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, I.; Al-Haj Husain, N.; Srinivasan, M.; Maniewicz, S.; Abou-Ayash, S.; Schimmel, M. Clinical outcomes and costs of conventional and digital complete dentures in a university clinic: A retrospective study. J. Prosthet. Dent. 2022, 128, 390–395. [Google Scholar] [CrossRef]
- Joda, T.; Gintaute, A.; Brägger, U.; Ferrari, M.; Weber, K.; Zitzmann, N.U. Time-efficiency and cost-analysis comparing three digital workflows for treatment with monolithic zirconia implant fixed dental prostheses: A double-blinded RCT. J. Dent. 2021, 113, 103779. [Google Scholar] [CrossRef]
- Jafarpour, D.; Haricharan, P.B.; de Souza, R.F. CAD/CAM versus traditional complete dentures: A systematic review and meta-analysis of patient- and clinician-reported outcomes and costs. J. Oral Rehabil. 2024, 51, 1911–1924. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Marcov, E.C.; Burlibașa, M.; Marcov, N.; Căminișteanu, F.; Ștețiu, A.A.; Popescu, M.; Costea, R.C.; Costea, R.M.; Burlibașa, L.; Drăguș, A.C.; et al. The Evaluation of Restored Proximal Contact Areas with Four Direct Adherent Biomaterials: An In Vitro Study. J. Funct. Biomater. 2025, 16, 128. [Google Scholar] [CrossRef] [PubMed]
- Tew, I.M.; Soo, S.Y.; Pow, E.H.N. Digitally versus conventionally fabricated complete dentures: A systematic review on cost-efficiency analysis and patient-reported outcome measures (PROMs). J. Prosthet. Dent. 2025, 133, 998–1007. [Google Scholar] [CrossRef]
- Alghauli, M.A.; Alqutaibi, A.Y. 3D-printed intracoronal restorations, occlusal and laminate veneers: Clinical relevance, properties, and behavior compared to milled restorations; a systematic review and meta-analysis. J. Esthet. Restor. Dent. 2024, 36, 1153–1170. [Google Scholar] [CrossRef]
- Lo Russo, L.; Zhurakivska, K.; Guida, L.; Chochlidakis, K.; Troiano, G.; Ercoli, C. Comparative cost-analysis for removable complete dentures fabricated with conventional, partial, and complete digital workflows. J. Prosthet. Dent. 2024, 131, 689–696. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Van de Winkel, T.; Delfos, F.; van Oirschot, B.; Maal, T.; Adang, E.; Meijer, G. Budget Impact Analysis: Digital Workflow Significantly Reduces Costs of Implant Supported Overdentures (IODs). Clin. Implant Dent. Relat. Res. 2025, 27, e13413. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.G.; Cianci, D.; Pranno, N.; Lerner, H.; Zarone, F.; Admakin, O. Trueness, precision, time-efficiency and cost analysis of chairside additive and subtractive versus lab-based workflows for manufacturing single crowns: An in vitro study. J. Dent. 2024, 141, 104792. [Google Scholar] [CrossRef]
- No-Cortes, J.; Ayres, A.P.; Lima, J.F.; Markarian, R.A.; Attard, N.J.; Cortes, A.R.G. Trueness, 3D Deviation, Time and Cost Comparisons Between Milled and 3D-Printed Resin Single Crowns. Eur. J. Prosthodont. Restor. Dent. 2022, 30, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.B.; Perry, J.; Elza, W. Economic and Clinical Impact of Digitally Produced Dentures. J. Prosthodont. 2021, 30, 108–112. [Google Scholar] [CrossRef]
- Asiga. DLP 3D Printer Product Sheet. Available online: https://asiga.com (accessed on 12 June 2025).
- Formlabs. SLA 3D Printer Specifications and Pricing. Available online: https://formlabs.com (accessed on 12 June 2025).
- Dimitrova, M.; Vlahova, A.; Kalachev, Y.; Zlatev, S. Recent advances in 3D printing of polymers for application in prosthodontics. Polymers 2023, 15, 4525. [Google Scholar] [CrossRef]
- Corsalini, M.; Barile, G.; Ranieri, F.; Morea, E.; Corsalini, T.; Capodiferro, S.; Palumbo, R.R. Comparison between Conventional and Digital Workflow in Implant Prosthetic Rehabilitation: A Randomized Controlled Trial. J. Funct. Biomater. 2024, 15, 149. [Google Scholar] [CrossRef]
- Pan, S.; Guo, D.; Zhou, Y.; Jung, R.E.; Hämmerle, C.H.F.; Mühlemann, S. Time efficiency and quality of outcomes in a model-free digital workflow using digital impression immediately after implant placement: A double-blind self-controlled clinical trial. Clin. Oral Implant. Res. 2019, 30, 617–626. [Google Scholar] [CrossRef] [PubMed]
- Ren, S.; Jiang, X.; Lin, Y.; Di, P. Crown Accuracy and Time Efficiency of Cement-Retained Implant-Supported Restorations in a Complete Digital Workflow: A Randomized Control Trial. J. Prosthodont. 2022, 31, 405–411. [Google Scholar] [CrossRef]
- Pullisaar, H.; Cattaneo, P.M.; Gera, A.; Sankiewicz, M.; Bilińska, M.; Vandevska-Radunovic, V.; Cornelis, M.A. Stability, survival, patient satisfaction, and cost-minimization of CAD/CAM versus conventional multistranded fixed retainers in orthodontic patients: A 2-year follow-up of a two-centre randomized controlled trial. Eur. J. Orthod. 2024, 46, cjae006. [Google Scholar] [CrossRef] [PubMed]
- Kharat, S.; Dudhani, S.I.; Kouser, A.; Subramanian, P.; Bhattacharjee, D.; Jhamb, V. Exploring the Impact of 3D Printing Technology on Patient-Specific Prosthodontic Rehabilitation: A Comparative Study. J. Pharm. Bioallied Sci. 2024, 16 (Suppl. 1), S423–S426. [Google Scholar] [CrossRef] [PubMed]
- Deng, K.; Wang, Y.; Zhou, Y.; Sun, Y. Comparison of treatment outcomes and time efficiency between a digital complete denture and conventional complete denture: A pilot study. J. Am. Dent. Assoc. 2023, 154, 32–42. [Google Scholar] [CrossRef]
- Park, J.-Y.; Kim, H.-Y.; Kim, J.-H.; Kim, J.-H.; Kim, W.-C. Comparison of prosthetic models produced by traditional and additive manufacturing methods. J. Adv. Prosthodont. 2015, 7, 294–302. [Google Scholar] [CrossRef]
- Otake, R.; Kanazawa, M.; Iwaki, M.; Soeda, Y.; Hada, T.; Katheng, A.; Komagamine, Y.; Minakuchi, S. Patient-reported outcome and cost-effectiveness analysis of milled and conventionally fabricated complete dentures in a university clinic: A retrospective study. J. Prosthet. Dent. 2024, 131, 227–232. [Google Scholar] [CrossRef]
- Ahlholm, P. Digital Techniques in Restorative Dentistry: Attitudes Among Dentists, Benefits of Digital Impression, and Applicability of 3D Printing; University of Eastern Finland: Eastern Finland, Finland, 2022. [Google Scholar]
- 3DSystems. SLS Dental Solutions Overview. Available online: https://3dsystems.com/dental (accessed on 12 June 2025).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).