Effectiveness of Surface Treatments on the Bond Strength to 3D-Printed Resins: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Literature Search
2.3. Study Selection
2.4. Data Extraction
2.5. Quality Assessment
2.6. Data Synthesis and Statistical Analysis
3. Results
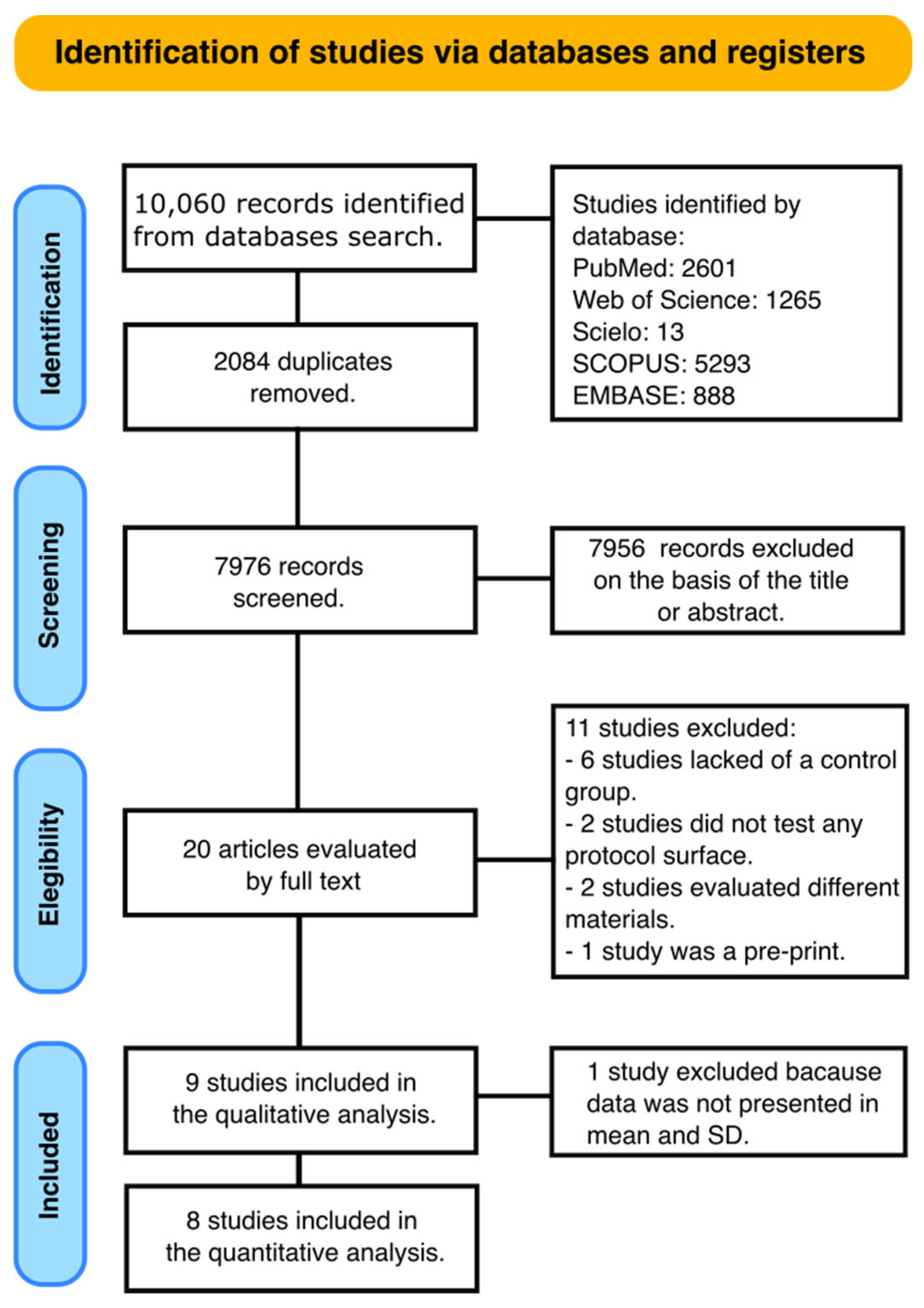
3.1. Search Strategy
3.2. Main Findings
3.3. Quality Assessment and Risk of Bias
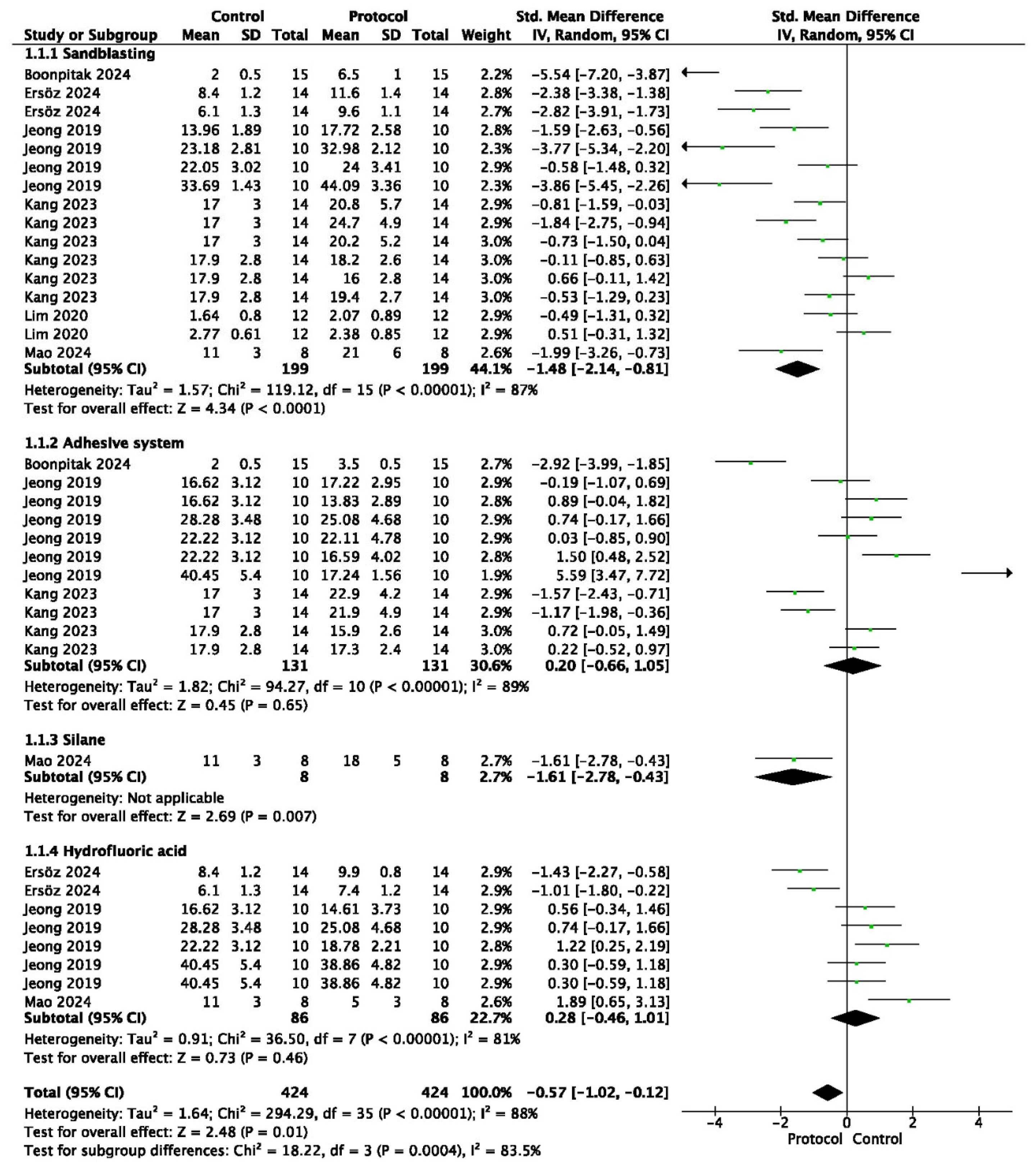
3.4. Meta-Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mao, Z.; Schmidt, F.; Beuer, F.; Yassine, J.; Hey, J.; Prause, E. Effect of surface treatment strategies on bond strength of additively and subtractively manufactured hybrid materials for permanent crowns. Clin. Oral Investig. 2024, 28, 371. [Google Scholar] [CrossRef] [PubMed]
- Mayer, J.; Stawarczyk, B.; Vogt, K.; Hickel, R.; Edelhoff, D.; Reymus, M. Influence of cleaning methods after 3D printing on two-body wear and fracture load of resin-based temporary crown and bridge material. Clin. Oral Investig. 2021, 25, 5987–5996. [Google Scholar] [CrossRef]
- ISO/ASTM 52900:2015 (ASTM F2792); Additive Manufacturing–General Principles—Terminology. ISO International Organization for Standardization: Geneva, Switzerland; ASTM American Society for Testing and Materials: West Conshohocken, PA, USA, 2015.
- Balestra, D.; Lowther, M.; Goracci, C.; Mandurino, M.; Cortili, S.; Paolone, G.; Louca, C.; Vichi, A. 3D Printed Materials for Permanent Restorations in Indirect Restorative and Prosthetic Dentistry: A Critical Review of the Literature. Materials 2024, 17, 1380. [Google Scholar] [CrossRef]
- Alsandi, Q.; Ikeda, M.; Arisaka, Y.; Nikaido, T.; Tsuchida, Y.; Sadr, A.; Yui, N.; Tagami, J. Evaluation of mechanical and physical properties of light and heat polymerized UDMA for DLP 3D printer. Sensors 2021, 21, 3331. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D printing in dentistry-state of the art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef]
- Kim, M.; Lee, J.; Park, C.; Jo, D.; Yu, B.; Khalifah, S.A.; Hayashi, M.; Kim, R.H. Evaluation of shear bond strengths of 3D printed materials for permanent restorations with different surface treatments. Polymers 2024, 16, 1838. [Google Scholar] [CrossRef]
- Elsaka, S.E. Bond strength of novel CAD/CAM restorative mate rials to self-adhesive resin cement: The effect of surface treatments. J. Adhes. Dent. 2014, 16, 531–540. [Google Scholar] [CrossRef]
- Khan, A.A.; Al Kheraif, A.A.; Jamaluddin, S.; Elsharawy, M.; Divakar, D.D. Recent Trends in Surface Treatment Methods for Bonding Composite Cement to Zirconia: A Review. J. Adhes. Dent. 2017, 19, 7–19. [Google Scholar] [CrossRef]
- Cobb, D.S.; Vargas, M.A.; Fridrich, T.A.; Bouschlicher, M.R. Metal surface treatment: Characterization and effect on composite-to-metal bond strength. Oper. Dent. 2000, 25, 427–433. [Google Scholar]
- Campos, F.; Almeida, C.S.; Rippe, M.P.; De Melo, R.M.; Valandro, L.F.; Bottino, M.A. Resin bonding to a hybrid ceramic: Effects of surface treatments and aging. Oper. Dent. 2016, 41, 171–178. [Google Scholar] [CrossRef]
- Berghaus, E.; Klocke, T.; Maletz, R.; Petersen, S. Degree of conversion and residual monomer elution of 3D-printed, milled and self-cured resin-based composite materials for temporary dental crowns and bridges. J. Mater. Sci. Mater. Med. 2023, 34, 23. [Google Scholar] [CrossRef] [PubMed]
- Reymus, M.; Roos, M.; Eichberger, M.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Bonding to new CAD/CAM resin composites: Influence of air abrasion and conditioning agents as pretreatment strategy. Clin. Oral Investig. 2019, 23, 529–538. [Google Scholar] [CrossRef]
- Borella, P.S.; Alvares, L.A.; Ribeiro, M.T.; Moura, G.F.; Soares, C.J.; Zancopé, K.; Mendonça, G.; Rodrigues, F.P.; Neves, F.D.D. Physical and mechanical properties of four 3D-printed resins at two different thick layers: An in vitro comparative study. Dent. Mater. 2023, 39, 686–692. [Google Scholar] [CrossRef]
- Sürer, E.; Ünal, M.; Aygün, E.B.; Ucar, Y. Evaluating the conversion degree of interim restorative materials produced by different 3-dimensional printer technologies. J. Prosthet. Dent. 2023, 130, 654.e1–654.e6. [Google Scholar] [CrossRef]
- Bora, P.V.; Sayed Ahmed, A.; Alford, A.; Pitttman, K.; Thomas, V.; Lawson, N.C. Characterization of materials used for 3D printing dental crowns and hybrid prostheses. J. Esthet. Restor. Dent. 2024, 36, 220–230. [Google Scholar] [CrossRef]
- Hammamy, M.; Rueda, S.R.; Pio, A.; Rizzante, F.A.; Lawson, N.C. Effect of Air Particle Abrasion and Primers on Bond Strength to 3D-Printed Crown Materials. Materials 2025, 18, 265. [Google Scholar] [CrossRef]
- Ersöz, B.; Aydın, N.; Ezmek, B.; Karaoğlanoğlu, S.; Çal, İ.K. Effect of Surface Treatments Applied to 3D Printed Permanent Resins on Shear Bond Strength. J. Clin. Exp. Dent. 2024, 16, e1059–e1066. [Google Scholar] [CrossRef]
- Lankes, V.; Reymus, M.; Liebermann, A.; Stawarczyk, B. Bond strength between temporary 3D printable resin and conventional resin composite: Influence of cleaning methods and air-abrasion parameters. Clin. Oral Investig. 2023, 27, 31–43. [Google Scholar] [CrossRef]
- Graf, T.; Erdelt, K.J.; Güth, J.F.; Edelhoff, D.; Schubert, O.; Schweiger, J. Influence of pre-treatment and artificial aging on the retention of 3D-printed permanent composite crowns. Biomedicines 2022, 10, 2186. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Moher, D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Delgado, A.H.; Sauro, S.; Lima, A.F.; Loguercio, A.D.; Della Bona, A.; Mazzoni, A.; Collares, F.M.; Staxrud, F.; Ferracane, J.; Tsoi, J.; et al. RoBDEMAT: A risk of bias tool and guideline to support reporting of pre-clinical dental materials research and assessment of systematic reviews. J. Dent. 2022, 127, 104350. [Google Scholar] [CrossRef] [PubMed]
- Sutuven, E.O.; Yildirim, N.C. Bond strength of self-adhesive resin cement to definitive resin crown materials manufactured by additive and subtractive methods. Dent. Mater. J. 2025, 44, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Aldosari, M.A.; Anany, N.M.; Alaqeely, R.; Alsenaidi, J.; Sufyan, A.; Talaat, S.; Bourauel, C.; Elshazly, T.M.; Alhotan, A. Comparative Analysis of Shear Bond Strength in Orthodontic Brackets Between Milled and 3D-Printed Definitive CAD/CAM Restorations. Appl. Sci. 2024, 14, 9530. [Google Scholar] [CrossRef]
- Boonpitak, K.; Chailark, P.; Wisitset, W.; Prawatvatchara, W.; Panpisut, P.; Wongkamhaeng, K. Assessing shear bond strength of various surface treatments of 3D-printed provisional material with bis-acryl relining material. BMC Oral Health 2024, 24, 1496. [Google Scholar] [CrossRef]
- Soto-Montero, J.; Romano, B.D.; Noronha, M.D.; André, C.B.; Giannini, M. Microtensile bond strength of resin cements to 3-D printed and milled temporary restorative resins. Odovtos Int. J. Dent. Sci. 2023, 25, 82–98. [Google Scholar] [CrossRef]
- Kang, Y.J.; Park, Y.; Shin, Y.; Kim, J.H. Effect of adhesion conditions on the shear bond strength of 3D printing resins after thermocycling used for definitive prosthesis. Polymers 2023, 15, 1390. [Google Scholar] [CrossRef]
- Lim, N.K.; Shin, S.Y. Bonding of conventional provisional resin to 3D printed resin: The role of surface treatments and type of repair resins. J. Adv. Prosthodont. 2020, 12, 322. [Google Scholar] [CrossRef]
- Jeong, K.W.; Kim, S.H. Influence of surface treatments and repair materials on the shear bond strength of CAD/CAM provisional restorations. J. Adv. Prosthodont. 2019, 11, 95–104. [Google Scholar] [CrossRef]
- Alijani, S.; Fotovat, F.; Soufi, L.R.; Alafchi, B.; Mohammadkhani, M.H. Shear bond strength of orthodontic brackets to specimens fabricated from temporary restorative materials by 3D-printing, CAD/CAM technology, and the conventional technique after surface treatment by sandblasting and laser. Int. Orthod. 2023, 21, 100790. [Google Scholar] [CrossRef]
- Spitznagel, F.A.; Horvath, S.D.; Guess, P.C.; Blatz, M.B. Resin bond to indirect composite and new ceramic/polymer materials: A review of the literature. J. Esthet. Restor. Dent. 2014, 26, 382–393. [Google Scholar] [CrossRef]
- Strasser, T.; Preis, V.; Behr, M.; Rosentritt, M. Roughness, surface energy, and superficial damages of CAD/CAM materials after surface treatment. Clin. Oral Investig. 2018, 22, 2787–2797. [Google Scholar] [CrossRef] [PubMed]
- Ozcan, M.; Vallittu, P.K. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent. Mater. 2003, 19, 725–731. [Google Scholar] [CrossRef]
- Amaral, R.; Ozcan, M.; Valandro, L.F.; Balducci, I.; Bottino, M.A. Effect of conditioning methods on the microtensile bond strength of phosphate monomer-based cement on zirconia ceramic in dry and aged conditions. J. Biomed. Mater. Res. Part B Appl. Biomater. 2008, 85, 1–9. [Google Scholar] [CrossRef]
- Blatz, M.B.; Chiche, G.; Holst, S.; Sadan, A. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int. 2007, 38, 745–753. [Google Scholar]
- Wolfart, M.; Lehmann, F.; Wolfart, S.; Kern, M. Durability of the resin bond strength to zirconia ceramic after using different surface conditioning methods. Dent. Mater. 2007, 23, 45–50. [Google Scholar] [CrossRef]
- Wiegand, A.; Stucki, L.; Hoffmann, R.; Attin, T.; Stawarczyk, B. Repairability of CAD/CAM high-density PMMA- and composite-based polymers. Clin. Oral Investig. 2015, 19, 2007–2013. [Google Scholar] [CrossRef]
- Altan, B.; Cinar, S.; Tuncelli, B. Evaluation of shear bond strength of zirconia- based monolithic CAD-CAM materials to resin cement after different surface treatments. Niger. J. Clin. Pract. 2019, 22, 1475–1482. [Google Scholar] [CrossRef]
- Park, J.H.; Choi, Y.S. Microtensile bond strength and micro- morphologic analysis of surface-treated resin nanoceramics. J. Adv. Prosthodont. 2016, 8, 275–284. [Google Scholar] [CrossRef]
- Ozcan, M.; Alander, P.; Vallittu, P.K.; Huysmans, M.C.; Kalk, W. Effect of three surface conditioning methods to improve bond strength of particulate filler resin composites. J. Mater. Sci. Mater. Med. 2005, 16, 21–27. [Google Scholar] [CrossRef]
- Ozcan, M. Evaluation of alternative intra-oral repair techniques for fractured ceramic-fused-to-metal restorations. J. Oral Rehabil. 2003, 30, 194–203. [Google Scholar] [CrossRef]
- Swift, E.J., Jr.; LeValley, B.D.; Boyer, D.B. Evaluation of new methods for composite repair. Dent. Mater. 1992, 8, 362–365. [Google Scholar] [CrossRef] [PubMed]
- ISO/TS 11405:2015; Dental Materials—Testing of Adhesion to Tooth Structure. ISO International Organization for Standardization: Geneva, Switzerland, 2015.
- Yuasa, T.; Iijima, M.; Ito, S.; Muguruma, T.; Saito, T.; Mizoguchi, I. Effects of long-term storage and thermocycling on bond strength of two self-etching primer adhesive systems. Eur. J. Orthod. 2009, 32, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Al Jabbari, Y.S.; Al Taweel, S.M.; Al Rifaiy, M.; Alqahtani, M.Q.; Koutsoukis, T.; Zinelis, S. Effects of surface treatment and artificial aging on the shear bond strength of orthodontic brackets bonded to four different provisional restorations. Angle Orthod. 2014, 84, 649–655. [Google Scholar] [CrossRef]
- Gale, M.S.; Darvell, B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Emsermann, I.; Eggmann, F.; Krastl, G.; Weiger, R.; Amato, J. Influence of Pretreatment Methods on the Adhesion of Composite and Polymer Infiltrated Ceramic CAD-CAM Blocks. J. Adhes. Dent. 2019, 21, 433–443. [Google Scholar] [CrossRef]
- Peumans, M.; Valjakova, E.B.; De Munck, J.; Mishevska, C.B.; Van Meerbeek, B. Bonding effectiveness of luting composites to different CAD/CAM materials. J. Adhes. Dent. 2016, 18, 289–302. [Google Scholar] [CrossRef]
- Yen, T.W.; Blackman, R.B.; Baez, R.J. Effect of acid etching on the flexural strength of a feldspathic porcelain and a castable glass ceramic. J. Prosthet. Dent. 1993, 70, 224–233. [Google Scholar] [CrossRef]
- Ozcan, M.; Allahbeickaraghi, A.; Dündar, M. Possible hazardous effects of hydrofluoric acid and recommendations for treatment approach: A review. Clin. Oral Investig. 2012, 16, 15–23. [Google Scholar] [CrossRef]
- Peumans, M.; Van Meerbeek, B.; Yoshida, Y.; Lambrechts, P.; Vanherle, G. Porcelain veneers bonded to tooth structure: An ultra-morphological FE-SEM examination of the adhesive interface. Dent. Mater. 1999, 15, 105–119. [Google Scholar] [CrossRef]
- Özcan, M.; Valandro, L.F.; Amaral, R.; Leite, F.; Bottino, M.A. Bond strength durability of a resin composite on a reinforced ceramic using various repair systems. Dent. Mater. 2009, 25, 1477–1483. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Basler, T.; Ender, A.; Roos, M.; Özcan, M.; Hämmerle, C. Effect of surface conditioning with airborne-particle abrasion on the tensile strength of polymeric cad/cam crowns luted with self-adhesive and conventional resin cements. J. Prosthet. Dent. 2012, 107, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.E.; Kim, S.H.; Lee, J.B.; Han, J.S.; Yeo, I.S.; Ha, S.R. Effects of airborne-particle abrasion protocol choice on the surface characteristics of monolithic zirconia materials and the shear bond strength of resin cement. Ceram. Int. 2016, 42, 1552–1562. [Google Scholar] [CrossRef]
- Kömürcüoğlu, M.B.; Sağırkaya, E.; Tulga, A. Influence of different surface treatments on bond strength of novel cad/cam restorative materials to resin cement. J. Adv. Prosthodont. 2017, 9, 439–446. [Google Scholar] [CrossRef]
- Keul, C.; Liebermann, A.; Roos, M.; Uhrenbacher, J.; Stawarczyk, B. The effect of ceramic primer on shear bond strength of resin composite cement to zirconia: A function of water storage and thermal cycling. J. Am. Dent. Assoc. 2013, 144, 1261–1271. [Google Scholar] [CrossRef]
- Román-Rodríguez, J.L.; Fons-Font, A.; Amigó-Borrás, V.; Granell-Ruiz, M.; Busquets-Mataix, D.; Panadero, R.A.; Solá-Ruiz, M.F. Bond strength of selected composite resin-cements to zirconium-oxide ceramic. Med. Oral Patol. Oral Y Cir. Bucal 2013, 18, e115–e123. [Google Scholar] [CrossRef]

| Search | Terms |
|---|---|
| #1 (Bonding Treatments) | Universal adhesives OR Universal simplified adhesive systems OR Universal Dental Adhesives OR Multipurpose adhesives OR multi-purpose adhesives OR multimode adhesives OR multi-mode adhesives OR universal bonding agent OR silane OR surface treatment OR sandblasting |
| #2 (Bond Strength) | Bond OR Bonding OR Dental bonding OR Bondng efficacy OR bond strength OR Bonding performance OR bonding effectiveness OR Bond performance OR adhesive properties OR microtensile strength OR Micro-tensile strength OR bonding properties OR Microtensile bond strength OR shear bond strength OR microshear bond strength |
| #3 (3D-Printed Materials) | 3D printing OR 3D printing manufacturing OR 3D printing resin OR 3D print resin OR additive manufacturing OR 3D-printed materials |
| # 4 | #1 AND #2 AND #3 |
| Study and Year | 3D-Printed Resin Tested and Manufacturer | 3D Printer | Surface Treatments Applied | Bond Strength Test | Storage | Main Results |
|---|---|---|---|---|---|---|
| Sutuven EO and Yildirim NC, 2025 [23] | VarseoSmile Crown Plus (BEGO, Bremen, Germany) | Digital Light Processing (DLP) printer Varseo XS (BEGO, Bremen, Germany) | Sandblasting (SB) Hydrofluoric (HF) acid etching Multi-primer (MP) SB + HF SB + MP SB + HF + MP | Shear | 24 h water storage + 5000 thermal cycles (5–55 °C) | SB-HF-MP, SB-MP, and HF groups have revealed the highest bond strength values. |
| Aldosari, 2024 [24] | Crowntec™ (Saremco Dental AG, Rebstein, Switzerland) C&B Per- manent™ (ODS, Seoul, Republic of Korea) | Liquid Crystal Display (LCD) printer Sonic Mighty 4K (Phrozen Tech. Co., Ltd., Hsinchu, Taiwan) | HF acid Diamond bur SB | Shear | Distilled water at 37 °C for 24 h | HF etching and SB improve bond strength. |
| Boonpitak, 2024 [25] | P Pro crown and bridge (Straumann, Basel, Switzerland) | DLP printer P30 Rapid- Shape (Straumann, Basel, Switzerland) | 95% ethanol Universal adhesive SB | Shear | Stored in dry for 24 h at room temperature | Highest bond strength was achieved with the combined application of SB and an adhesive system. |
| Ersöz B, 2024 [18] | Crowntec (Saremco Dental AG, Zwitserland), Permanent Crown (Formlabs, MA, USA) | Stereolithography (SLA) printer (Formlabs 3B+, Formlabs, MA, USA), DLP printer (Asiga MAX UV, Asiga, Sydney, Australia) | SB HF acid | Shear | 37 °C distilled water for 24 h | SB resulted in higher bond strength values. |
| Mao, 2024 [1] | VarseoSmile Crown plus (BEGO, Bremen, Germany) | DLP printer Varseo XS (BEGO, Bremen, Germany). | Silane SB SB + silane HF acid HF + silane | Shear | 37 °C distilled water for 24 h and 5000 thermal cycles in 5 and 55 °C | Etching showed the lowest mean bond strength values. Sandblasting and silane resulted in higher values. |
| Soto-Montero, 2023 [26] | Cosmos Temp 3D (Yller, Pelotas, RS, Brazil), Smart Print Bio Temp (MM Tech, São Carlos, SP, Brazil), Resilab 3D Temp (Wilcos, Petrópolis, RJ, Brazil) | Photon, Anycubic Technology Co., Shenzen, China (DLP technology) | SB | Microtensile | 24 h at 37 °C in distilled water, followed by thermal cycling (5000 cycles, 5 °C to 55 °C) | Airborne-particle abrasion did not improve the bond strength of 3D-printed resins. |
| Kang, 2023 [27] | TeraHarz TC-80 (Graphy, Seoul, Republic of Korea), Permanent Crown Resin (Formlabs, Somerville, MA, USA) | DLP printer Sprint Ray Pro 95 (Sprint Ray, Los Angeles, CA, USA), SLA printer Form 3 (Formlabs, Somerville, MA, USA) | SB Single bond universal adhesive (SBU) | Shear | 24 h in distilled water at 37 °C, followed by 10,000 thermocycles between 5–55 °C (70 s per cycle). | Combining SB and adhesive resulted in higher bond strength. |
| Lim, 2020 [28] | Nextdent C&B (Vertex-Dental B. V., Soesterberg, Netherlands) | DLP printer cara Print 4.0 (Kulzer, Hanau, Germany) | SB Primer | Shear | Distilled water at 37 °C for 24 h | Adhesion without additional surface treatment is recommended. |
| Jeong, 2019 [29] | Nextdent C&B ZMD-1000B Temporary (Vertex-Dental B. V., Soesterberg, The Netherlands) | DLP printer W11, Bio3D, Seoul, Korea Zenith U, Dentis, Daegu, Korea | Silicon Carbide (SiC) paper SiC paper+ sandblasting SiC paper+ HF acid SiC paper+ adhesive (Adper Scotchbond Multi-Purpose) SiC paper+ Single bond universal adhesive | Shear | Distilled water at 37 °C for 24 h | SiC paper and SB achieved the highest bond strength values. |
| Study | D1. Bias in Planning and Allocation | D2. Bias in Sample/Specimen Preparation | D3. Bias in Outcome Assessment | D4. Bias in Data Treatment and Outcome Reporting | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1.1 | 1.2 | 1.3 | 2.1 | 2.2 | 3.1 | 3.2 | 4.1 | 4.2 | |
| Sutuven EO and Yildirim NC, 2025 [23] | R | R | IR | R | R | R | NR | R | R |
| Aldosari 2024 [24] | R | R | R | R | R | R | NR | R | R |
| Boonpitak 2024 [25] | R | IR | R | R | R | R | NR | R | R |
| Ersöz, 2024 [18] | R | NR | IR | R | R | R | NR | R | R |
| Mao, 2024 [1] | R | R | NR | R | R | R | NR | R | R |
| Soto-Montero, 2023 [26] | R | R | NR | R | R | R | R | R | R |
| Kang, 2023 [27] | R | NR | NR | R | R | R | NR | R | R |
| Lim, 2020 [28] | R | R | IR | R | R | R | NR | R | R |
| Jeong, 2019 [29] | R | NR | NR | R | R | IR | NR | R | IR |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bourgi, R.; Etienne, O.; Holiel, A.A.; Cuevas-Suárez, C.E.; Hardan, L.; Roman, T.; Flores-Ledesma, A.; Qaddomi, M.; Haikel, Y.; Kharouf, N. Effectiveness of Surface Treatments on the Bond Strength to 3D-Printed Resins: A Systematic Review and Meta-Analysis. Prosthesis 2025, 7, 56. https://doi.org/10.3390/prosthesis7030056
Bourgi R, Etienne O, Holiel AA, Cuevas-Suárez CE, Hardan L, Roman T, Flores-Ledesma A, Qaddomi M, Haikel Y, Kharouf N. Effectiveness of Surface Treatments on the Bond Strength to 3D-Printed Resins: A Systematic Review and Meta-Analysis. Prosthesis. 2025; 7(3):56. https://doi.org/10.3390/prosthesis7030056
Chicago/Turabian StyleBourgi, Rim, Olivier Etienne, Ahmed A. Holiel, Carlos Enrique Cuevas-Suárez, Louis Hardan, Tatiana Roman, Abigailt Flores-Ledesma, Mohammad Qaddomi, Youssef Haikel, and Naji Kharouf. 2025. "Effectiveness of Surface Treatments on the Bond Strength to 3D-Printed Resins: A Systematic Review and Meta-Analysis" Prosthesis 7, no. 3: 56. https://doi.org/10.3390/prosthesis7030056
APA StyleBourgi, R., Etienne, O., Holiel, A. A., Cuevas-Suárez, C. E., Hardan, L., Roman, T., Flores-Ledesma, A., Qaddomi, M., Haikel, Y., & Kharouf, N. (2025). Effectiveness of Surface Treatments on the Bond Strength to 3D-Printed Resins: A Systematic Review and Meta-Analysis. Prosthesis, 7(3), 56. https://doi.org/10.3390/prosthesis7030056











