Experience Using a New High-Density Polyethylene-Based Porous Orbital Implant: Explorative 1-Year Performance and Safety Results
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Surgical Technique
2.3. Orbital Implants
2.4. Clinical Evaluation
2.5. Statistical Analysis
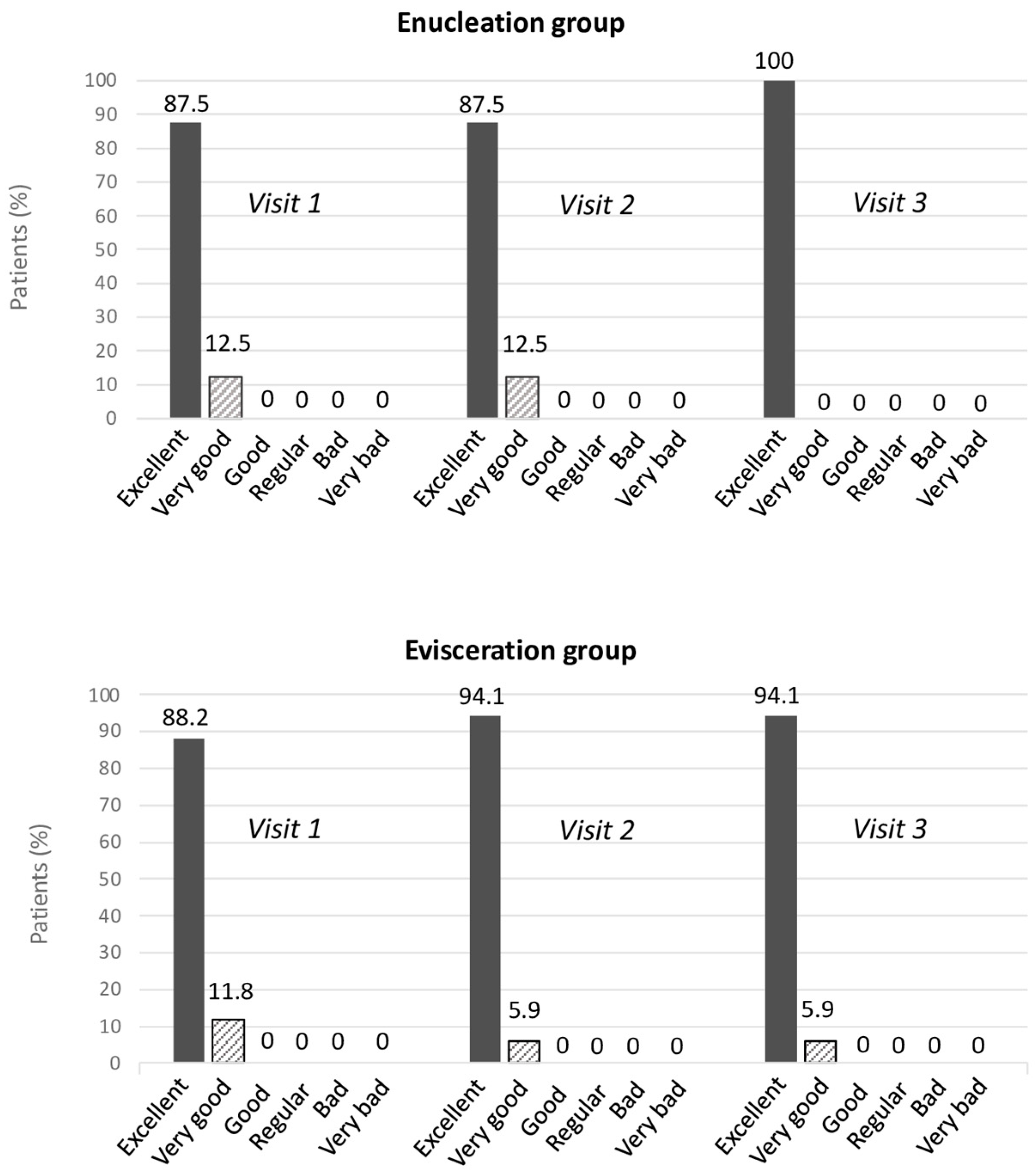
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Custer, P.L.; Kennedy, R.H.; Woog, J.J.; Kaltreider, S.A.; Meyer, D.R. Orbital implants in enucleation surgery: A report by the American Academy of Ophthalmology. Ophthalmology 2003, 110, 2054–2061. [Google Scholar] [CrossRef] [PubMed]
- Wladis, E.J.; Aakalu, V.K.; Sobel, R.K.; Yen, M.T.; Bilyk, J.R.; Mawn, L.A. Orbital Implants in Enucleation Surgery: A Report by the American Academy of Ophthalmology. Ophthalmology 2018, 125, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Moshfeghi, D.M.; Moshfeghi, A.A.; Finger, P.T. Enucleation. Surv. Ophthalmol. 2000, 44, 277–301. [Google Scholar] [CrossRef]
- Shah, S.U.; Shields, C.L.; Lally, S.E.; Shields, J.A. Hydroxyapatite orbital implant in children following enucleation: Analysis of 531 sockets. Ophthal. Plast. Reconstr. Surg. 2015, 31, 108–114. [Google Scholar] [CrossRef]
- Hornblass, A.; Biesman, B.S.; Eviatar, J.A. Current techniques of enucleation: A survey of 5,439 intraorbital implants and a review of the literature. Ophthal. Plast. Reconstr. Surg. 1995, 11, 77–78. [Google Scholar] [CrossRef]
- Jordan, D.R. Porous versus Nonporous Orbital Implants: A 25-Year Retrospective. Ophthalmology 2018, 125, 1317–1319. [Google Scholar] [CrossRef]
- Soares, I.P.; França, V.P. Evisceration and enucleation. Semin. Ophthalmol. 2010, 25, 94–97. [Google Scholar] [CrossRef]
- Alwitry, A.; West, S.; King, J.; Foss, A.J.; Abercrombie, L.C. Long-term follow-up of porous polyethylene spherical implants after enucleation and evisceration. Ophthal. Plast. Reconstr. Surg. 2007, 23, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Schellini, S.A.; El Dib, R.; Limongi, R.M.; Mörschbächer, R. Anophthalmic socket: Choice of orbital implants for reconstruction. Arq. Bras. Oftalmol. 2015, 78, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Bueno, I.; Di Lauro, S.; Alvarez, I.; Lopez, J.C.; Garcia-Gutierrez, M.T.; Fernandez, I.; Larra, E.; Pastor, J.C. Safety and Biocompatibility of a New High-Density Polyethylene-Based Spherical Integrated Porous Orbital Implant: An Experimental Study in Rabbits. J. Ophthalmol. 2015, 2015, 904096. [Google Scholar] [CrossRef] [PubMed]
- Garrido-Hermosilla, A.; Martínez-Alberquilla, I.; Díaz-Ruiz, M.C.; Monge-Carmona, R.; Méndez-Muros, M.; López-Díaz, Á.; Sánchez-Margalet, V.; Gutiérrez-Sánchez, E.; Relimpio-López, M.I.; Rodríguez-de-la-Rúa-Freanch, E. Long-Term Mental Health after High-Density Polyethylene-Based Porous Orbital Implant in Enucleated and Eviscerated Patients. Prosthesis 2024, 6, 979–988. [Google Scholar] [CrossRef]
- Sales-Sanz, M.; Sanz-Lopez, A. Four-petal evisceration: A new technique. Ophthal. Plast. Reconstr. Surg. 2007, 23, 389–392. [Google Scholar] [CrossRef] [PubMed]
- Goiato, M.C.; Haddad, M.F.; dos Santos, D.M.; Pesqueira, A.A.; Ribeiro, P.d.P.; Moreno, A. Orbital implants insertion to improve ocular prostheses motility. J. Craniofac. Surg. 2010, 21, 870–875. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.M.; Lee, S.Y.; Yoon, J.S. Health-related quality of life and emotional status of anophthalmic patients in Korea. Am. J. Ophthalmol. 2010, 149, 1005–1011.e1. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, M.L.R.; Ekholm, O.; Prause, J.U.; Toft, P.B. Quality of life of eye amputated patients. Acta Ophthalmol. 2012, 90, 435–440. [Google Scholar] [CrossRef] [PubMed]
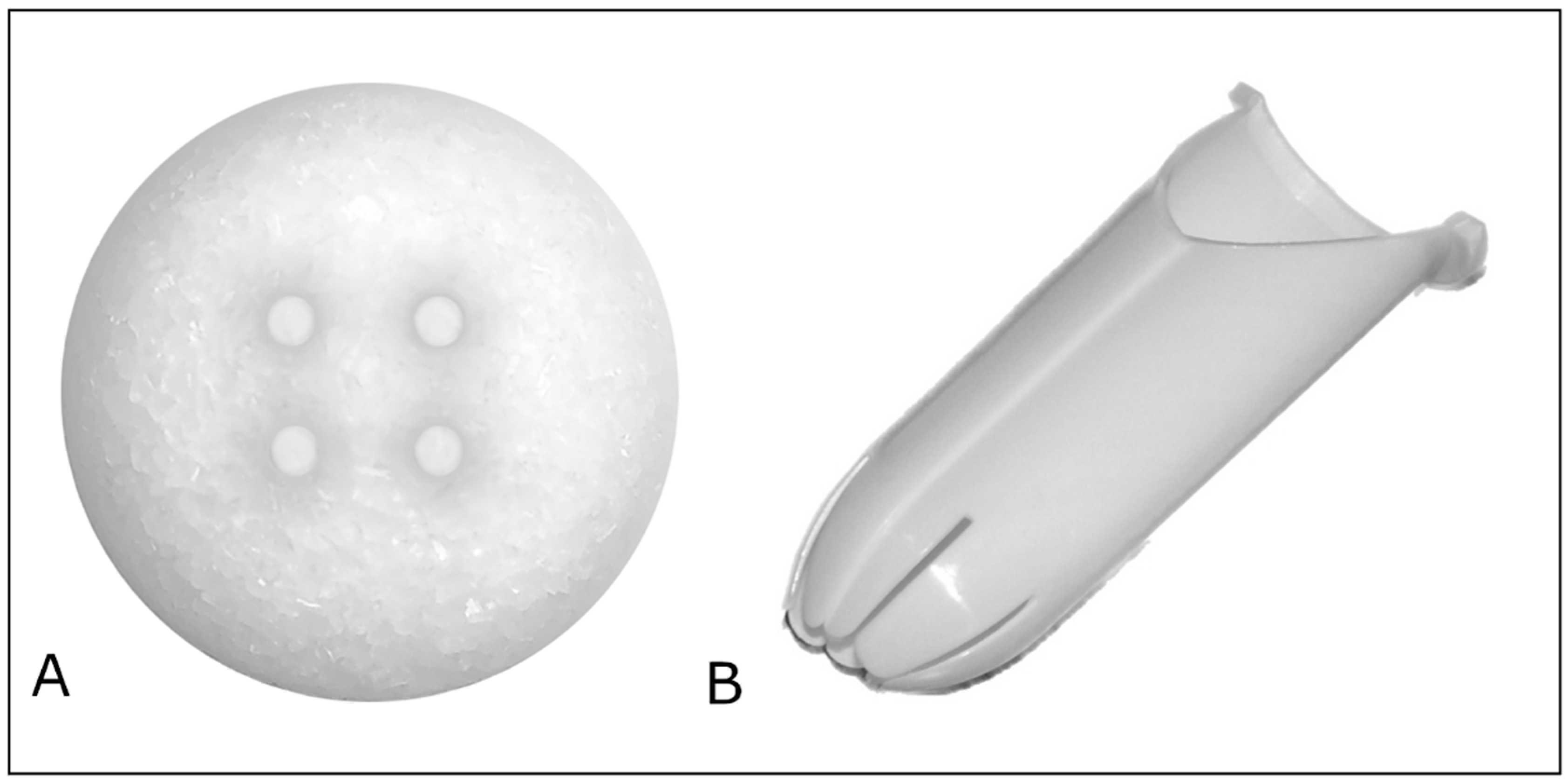
| OCULFIT ORBITAL IMPLANT | |
|---|---|
| Sphere diameter | 14/16/18–23 mm |
| Material | High-density porous polyethylene |
| Porosity | 45% |
| Pore size | >100 µm |
| Granules used | <400 µm in the previous part 700–100 µm at the rear |
| Suture channels | 4 interconnected |
| Sterilization | Ethylene Oxide |
| Expiration | 5 years |
| Visit 1 | Visit 2 | Visit 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| AESTHETIC APPEARANCE (WITH EXTERNAL PROSTHESIS) [n (%)] | |||||||||
| Good | Poor | Bad | Good | Poor | Bad | Good | Poor | Bad | |
| Enucleation | - | - | - | 13 (81.3) | 3 (18.7) | 0 (0) | 14 (87.5) | 2 (12.5) | 0 (0) |
| Evisceration | - | - | - | 13 (76.5) | 4 (23.5) | 0 (0) | 17(100) | 0 (0) | 0 (0) |
| p-value | - | 0.74 | 0.13 | ||||||
| PALPEBRAL FISSURE(WITH EXTERNAL PROSTHESIS) [n (%)] | |||||||||
| Symmetric | Asymmetric | Symmetric | Asymmetric | Symmetric | Asymmetric | ||||
| Enucleation | - | - | 14 (87.5) | 2 (12.5) | 15 (93.8) | 1 (6.3) | |||
| Evisceration | - | - | 12 (70.6) | 5 (29.4) | 15 (88.2) | 2 (11.8) | |||
| p-value | - | 0.24 | 0.58 | ||||||
| FORNIX CONDITION [n (%)] | |||||||||
| Wide | Shortened | Wide | Shortened | Wide | Shortened | ||||
| Enucleation | 16 (100) | 0 (0) | 16 (100) | 0 (0) | 16 (100) | 0 (0) | |||
| Evisceration | 17 (100) | 0 (0) | 17 (100) | 0 (0) | 17 (100) | 0 (0) | |||
| p-value | - a | - a | - a | ||||||
| LOWER EYELID LAXITY [n (%)] | |||||||||
| Symmetric | Asymmetric | Symmetric | Asymmetric | Symmetric | Asymmetric | ||||
| Enucleation | 15 (93.8) | 1 (6.3) | 15 (93.8) | 1 (6.3) | 16 (100) | 0 (0) | |||
| Evisceration | 16 (94.1) | 1 (5.9) | 16 (94.1) | 1 (5.9) | 16 (94.1) | 1 (5.9) | |||
| p-value | 0.97 | 0.97 | 0.33 | ||||||
| EXTERNAL PROSTHESIS MOTILITY [n (%)] | |||||||||
| Good | Limited | Null | Good | Limited | Null | Good | Limited | Null | |
| Enucleation | - | - | - | 11 (68.8) | 5 (31.2) | 0 (0) | 11 (68.8) | 5 (31.2) | 0 (0) |
| Evisceration | - | - | - | 15 (88.2) | 2 (11.8) | 0 (0) | 16 (94.1) | 1 (5.9) | 0 (0) |
| p-value | - | 0.17 | 0.06 | ||||||
| OCULAR PROTRUSION (WITH EXTERNAL PROSTHESIS) (mm) | |||||||||
| Operated eye | Contralateral eye | Operated eye | Contralateral eye | Difference between eyes | Operated eye | Contralateral eye | Difference between eyes | ||
| Enucleation | - | - | 14.59 ± 2.73 | 15.81 ± 2.50 | 1.22 ± 0.93 | 15.00 ± 2.37 | 15.63 ± 2.31 | 0.63 ± 0.67 | |
| Evisceration | - | - | 14.94 ± 2.53 | 15.19 ± 3.03 | 0.29 ± 1.80 | 15.24 ± 2.48 | 15.76 ± 2.76 | 0.53 ± 1.07 | |
| p-value | - | 0.08 b | 0.76 b | ||||||
| SUPERIOR PALPEBRAL SULCUS DEPRESSION (WITH EXTERNAL PROSTHESIS) [n (%)] | |||||||||
| Mild | Moderate | Severe | Mild | Moderate | Severe | Mild | Moderate | Severe | |
| Enucleation | - | - | - | 12 (75.0) | 2 (12.5) | 2 (12.5) | 12 (75.0) | 3 (18.8) | 1 (6.2) |
| Evisceration | - | - | - | 15 (88.2) | 1 (5.9) | 1 (5.9) | 15 (88.2) | 1 (5.9) | 1 (5.9) |
| p-value | - | 0.62 | 0.52 | ||||||
| UPPER EYELID ELEVATOR MUSCLE FUNCTION (WITH EXTERNAL PROSTHESIS) [n (%)] | |||||||||
| Worse than contralateral eye | Same as contralateral eye | Worse than contralateral eye | Same as contralateral eye | Worse than contralateral eye | Same as contralateral eye | ||||
| Enucleation | - | - | 11 (68.8) | 5 (31.2) | 11 (68.8) | 5 (31.2) | |||
| Evisceration | - | - | 6 (35.3) | 11 (64.7) | 7 (41.2) | 10 (58.8) | |||
| p-value | - | 0.06 | 0.11 | ||||||
| ORBITAL VOLUME (WITH EXTERNAL PROSTHESIS) [n (%)] | |||||||||
| Symmetric | Asymmetric | Symmetric | Asymmetric | Symmetric | Asymmetric | ||||
| Enucleation | - | - | 14 (87.5) | 2 (12.5) | 16 (100) | 0 (0) | |||
| Evisceration | - | - | 15 (88.2) | 2 (11.8) | 17 (100) | 0 (0) | |||
| p-value | - | 0.95 | - a | ||||||
| ORBITAL IMPLANT MOTILITY (WITHOUT EXTERNAL PROSTHESIS) [n (%)] | |||||||||
| Good | Limited | Null | Good | Limited | Null | Good | Limited | Null | |
| Enucleation | 15 (93.8) | 1 (6.3) | 0 (0) | 15 (93.8) | 1 (6.3) | 0 (0) | 15 (93.8) | 1 (6.3) | 0 (0) |
| Evisceration | 17 (100) | 0 (0) | 0 (0) | 17 (100) | 0 (0) | 0 (0) | 17 (100) | 0 (0) | 0 (0) |
| p-value | 0.30 | 0.30 | 0.30 | ||||||
| Variable | ANATOMICAL SUCCESS | FUNCTIONAL SUCCESS | |||||
| Success (n = 26) | Failure (n = 7) | p-Value | Success (n = 27) | Failure (n = 6) | p-Value | ||
| Conjunctiva-Tenon status [n, (%)] |
| 11 (42.3) | 2 (28.6) | 0.51 | 10 (37.0) | 3 (50) | 0.56 |
| 15 (57.7) | 5 (71.4) | 17 (63.0) | 3 (50) | |||
| Previous surgeries [n, (%)] |
| 16 (61.5) | 5 (71.4) | 0.63 | 19 (70.4) | 2 (33.3) | 0.09 |
| 10 (38.5) | 2 (28.6) | 8 (29.6) | 4 (66.7) | |||
| Gender [n, (%)] |
| 12 (46.2) | 2 (28.6) | 0.40 | 10 (37.0) | 4 (66.7) | 0.18 |
| 14 (53.8) | 5 (71.4) | 17 (63.0) | 2 (33.3) | |||
| Abdominal dermal fat grafting [n, (%)] |
| 10 (38.5) | 4 (57.1) | 0.38 | 11 (40.7) | 3 (50) | 0.68 |
| 16 (61.5) | 3 (42.9) | 16 (59.3) | 3 (50) | |||
| Main cause of eye removal [n, (%)] |
| 9 (34.6) | 2 (28.6) | 0.39 | 10 (37.0) | 1 (16.7) | 0.44 |
| 3 (11.5) | 1 (14.3) | 4 (14.8) | 0 (0.0) | |||
| 1 (3.9) | 0 (0.0) | 1 (3.7) | 0 (0.0) | |||
| 13 (50.0) | 3 (42.9) | 11 (40.7) | 5 (83.3) | |||
| 0 (0.0) | 1 (14.3) | 1 (3.7) | 0 (0.0) | |||
| Type of intervention [n, (%)] |
| 13 (50.0) | 3 (42.9) | 0.74 | 11 (40.7) | 5 (83.3) | 0.06 |
| 13 (50.0) | 4 (57.1) | 16 (59.3) | 1 (16.7) | |||
| Age (mean ± SD) | 63.2 ± 14.2 | 74.4 ± 9.8 | 0.06 | 65.7 ± 15.0 | 65.2 ± 9.5 | 0.94 | |
| Diameter of implants (mean ± SD) | 20.3 ± 1.1 | 20.1 ± 1.2 | 0.66 | 20.4 ± 1.0 | 19.8 ± 1.2 | 0.24 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garrido-Hermosilla, A.M.; Martínez-Alberquilla, I.; Díaz-Ruiz, M.C.; Monge-Carmona, R.; Méndez-Muros, M.; Sánchez-Margalet, V.; Gutiérrez-Sánchez, E.; Relimpio-López, M.I.; Rodríguez-de-la-Rúa-Franch, E. Experience Using a New High-Density Polyethylene-Based Porous Orbital Implant: Explorative 1-Year Performance and Safety Results. Prosthesis 2024, 6, 1400-1409. https://doi.org/10.3390/prosthesis6060101
Garrido-Hermosilla AM, Martínez-Alberquilla I, Díaz-Ruiz MC, Monge-Carmona R, Méndez-Muros M, Sánchez-Margalet V, Gutiérrez-Sánchez E, Relimpio-López MI, Rodríguez-de-la-Rúa-Franch E. Experience Using a New High-Density Polyethylene-Based Porous Orbital Implant: Explorative 1-Year Performance and Safety Results. Prosthesis. 2024; 6(6):1400-1409. https://doi.org/10.3390/prosthesis6060101
Chicago/Turabian StyleGarrido-Hermosilla, Antonio Manuel, Irene Martínez-Alberquilla, María Concepción Díaz-Ruiz, Raquel Monge-Carmona, Mariola Méndez-Muros, Víctor Sánchez-Margalet, Estanislao Gutiérrez-Sánchez, María Isabel Relimpio-López, and Enrique Rodríguez-de-la-Rúa-Franch. 2024. "Experience Using a New High-Density Polyethylene-Based Porous Orbital Implant: Explorative 1-Year Performance and Safety Results" Prosthesis 6, no. 6: 1400-1409. https://doi.org/10.3390/prosthesis6060101
APA StyleGarrido-Hermosilla, A. M., Martínez-Alberquilla, I., Díaz-Ruiz, M. C., Monge-Carmona, R., Méndez-Muros, M., Sánchez-Margalet, V., Gutiérrez-Sánchez, E., Relimpio-López, M. I., & Rodríguez-de-la-Rúa-Franch, E. (2024). Experience Using a New High-Density Polyethylene-Based Porous Orbital Implant: Explorative 1-Year Performance and Safety Results. Prosthesis, 6(6), 1400-1409. https://doi.org/10.3390/prosthesis6060101








