Micro-CT Structure Analysis on Dental Implants: Preliminary In Vitro Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Approach and Criteria
2.2. Sources and Search Parameters
2.3. Data Extraction and Analysis
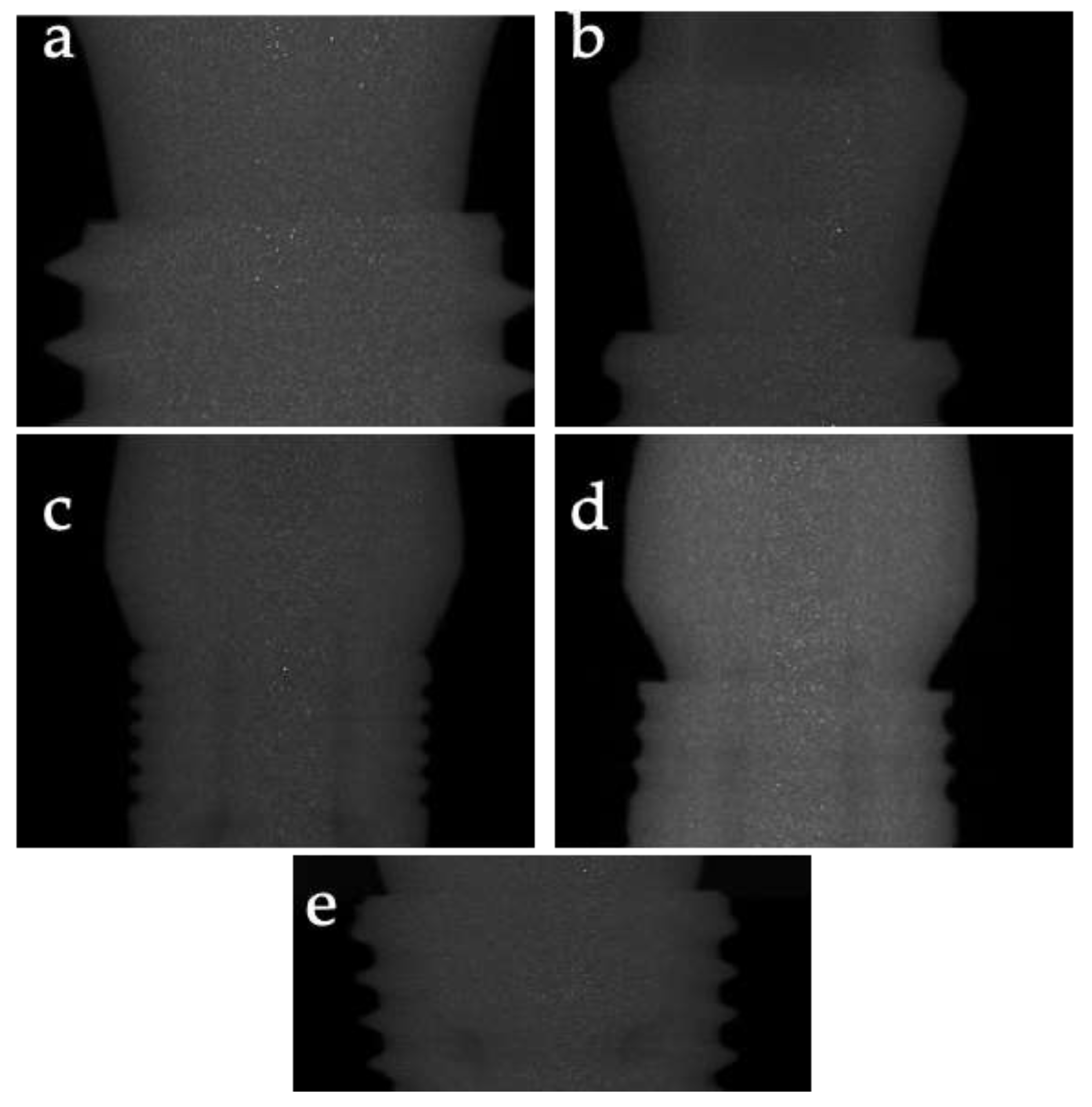
2.4. Micro-CT Imaging in the Present Study
2.4.1. Sample
- OsstemImplant (Seoul, Republic of Korea); TSIII, Regular connection;
- Megagen Implant Co., Ltd. (Seoul, Republic of Korea); AnyOne, Regular connection;
- Schütz Dental GmbH (Rosbach, Germany); Diagram, Regular connection;
- FDS76 (Reggio Calabria, Italy); K2 Regular connection;
- FDS76 (Reggio Calabria, Italy); V4 Regular connection.
2.4.2. Micro-CT
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias in Studies
3.4. Results of Individual Studies
- Yu et al. [11] found that fluoride exposure significantly reduced bone mineral density (BMD) and BIC ratios in rabbits;
- Min et al. [12] reported that metal artifacts in CBCT images could be effectively quantified using micro-CT as a reference;
- González-García et al. [13] demonstrated a strong correlation between radiographic bone density from CBCT and bone volumetric fraction from micro-CT;
- Neldam et al. [14] showed that synchrotron micro-CT provides high-resolution images that accurately depict bone microarchitecture;
- Kapishnikov et al. [15] observed that static compressive loads significantly increased the microgap size at the implant–sleeve connection;
- Hsu et al. [16] found a positive correlation between bone stiffness, BIC, and initial implant stability;
- Parsa et al. [17] reported strong correlations between bone volume fraction and bone density;
3.5. Results of Syntheses
3.6. Certainty of Evidence
3.7. Additional Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hipsley, C.A.; Aguilar, R.; Black, J.R.; Hocknull, S.A. High-throughput microCT scanning of small specimens: Preparation, packing, parameters and post-processing. Sci. Rep. 2020, 10, 13863. [Google Scholar] [CrossRef]
- Batista, R.; Moreira, A.; Oliveira, S.J.; Mesquita, P.; Sampaio-Fernandes, J.; Figueiral, M.H. Deformation of implant retaining screws-Study with stereoscopic microscopy and microCT. J. Esthet. Restor. Dent. 2022, 34, 1147–1155. [Google Scholar] [CrossRef] [PubMed]
- Roatesi, I.; Roatesi, S. Modeling of Dental Implant Osseointegration Progress by Three-Dimensional Finite Element Method. Appl. Sci. 2020, 10, 5561. [Google Scholar] [CrossRef]
- Brånemark, P.I. Osseointegration and its experimental background. J. Prosthet. Dent. 1983, 50, 399–410. [Google Scholar] [CrossRef]
- Romanos, G.E.; Schesni, A.; Nentwig, G.-H.; Winter, A.; Sader, R.; Brandt, S. Impact of Implant Diameter on Success and Survival of Dental Implants: An Observational Cohort Study. Prosthesis 2023, 5, 888–897. [Google Scholar] [CrossRef]
- Shopova, D.; Mihaylova, A.; Yaneva, A.; Bakova, D.; Dimova-Gabrovska, M. Biofabrication Approaches for Peri-Implantitis Tissue Regeneration: A Focus on Bioprinting Methods. Prosthesis 2024, 6, 372–392. [Google Scholar] [CrossRef]
- Mannino, F.; D’Angelo, T.; Pallio, G.; Ieni, A.; Pirrotta, I.; Giorgi, D.A.; Scarfone, A.; Mazziotti, S.; Booz, C.; Bitto, A.; et al. The Nutraceutical Genistein-Lycopene Combination Improves Bone Damage Induced by Glucocorticoids by Stimulating the Osteoblast Formation Process. Nutrients 2022, 14, 4296. [Google Scholar] [CrossRef]
- Matos, J.D.M.d.; Queiroz, D.A.; Nakano, L.J.N.; Andrade, V.C.; Ribeiro, N.d.C.R.; Borges, A.L.S.; Bottino, M.A.; Lopes, G.d.R.S. Bioengineering Tools Applied to Dentistry: Validation Methods for In Vitro and In Silico Analysis. Dent. J. 2022, 10, 145. [Google Scholar] [CrossRef]
- Zangooei, M.H.; Margolis, R.; Hoyt, K. Multiscale computational modeling of cancer growth using features derived from microCT images. Sci. Rep. 2021, 11, 18524. [Google Scholar] [CrossRef]
- Ghavami-Lahiji, M.; Davalloo, R.T.; Tajziehchi, G.; Shams, P. Micro-computed tomography in preventive and restorative dental research: A review. Imaging Sci. Dent. 2021, 51, 341–350. [Google Scholar] [CrossRef]
- Yu, Y.J.; Zhu, W.Q.; Xu, L.N.; Ming, P.P.; Shao, S.Y.; Qiu, J. Osseointegration of titanium dental implant under fluoride exposure in rabbits: Micro-CT and histomorphometry study. Clin. Oral Implant. Res. 2019, 30, 1038–1048. [Google Scholar] [CrossRef] [PubMed]
- Min, C.K.; Kim, K.A. Quantitative analysis of metal artefacts of dental implant in CBCT image by correlation analysis to micro-CT: A microstructural study. Dentomaxillofacial Radiol. 2021, 50, 20200365. [Google Scholar] [CrossRef] [PubMed]
- González-García, R.; Monje, F. The reliability of cone-beam computed tomography to assess bone density at dental implant recipient sites: A histomorphometric analysis by micro-CT. Clin. Oral Implant. Res. 2012, 24, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Neldam, C.A.; Lauridsen, T.; Rack, A.; Lefolii, T.T.; Jørgensen, N.R.; Feidenhans’l, R.; Pinholt, E.M. Application of high resolution synchrotron micro-CT radiation in dental implant osseointegration. J. Cranio-Maxillofac. Surg. 2015, 43, 682–687. [Google Scholar] [CrossRef] [PubMed]
- Kapishnikov, S.; Gadyukov, A.; Chaushu, G.; Chaushu, L. Micro-CT Analysis of Microgap at a Novel Two-Piece Dental Implant Comprising a Replaceable Sleeve In Vitro. Int. J. Oral Maxillofac. Implant. 2021, 36, 451–459. [Google Scholar] [CrossRef]
- Hsu, J.T.; Huang, H.L.; Tsai, M.T.; Wu, A.Y.; Tu, M.G.; Fuh, L.J. Effects of the 3D bone-to-implant contact and bone stiffness on the initial stability of a dental implant: Micro-CT and resonance frequency analyses. Int. J. Oral Maxillofac. Surg. 2013, 42, 276–280. [Google Scholar] [CrossRef]
- Parsa, A.; Ibrahim, N.; Hassan, B.; van der Stelt, P.; Wismeijer, D. Bone quality evaluation at dental implant site using multislice CT, micro-CT, and cone beam CT. Clin. Oral Implant. Res. 2015, 26, e1–e7. [Google Scholar] [CrossRef]
- Bissinger, O.; Probst, F.A.; Wolff, K.D.; Jeschke, A.; Weitz, J.; Deppe, H.; Kolk, A. Comparative 3D micro-CT and 2D histomorphometry analysis of dental implant osseointegration in the maxilla of minipigs. J. Clin. Periodontol. 2017, 44, 418–427. [Google Scholar] [CrossRef]
- Vinhas, A.S.; Salazar, F.; Mendes, J.M.; Silva, A.S.; Ríos-Carrasco, B.; Ríos-Santos, J.V.; Gil, J.; Herrero-Climent, M.; Aroso, C. SEM Analysis and Micro-CT Evaluation of Four Dental Implants after Three Different Mechanical Requests—In Vitro Study. Materials 2024, 17, 434. [Google Scholar] [CrossRef]
- Kowalski, J.; Puszkarz, A.K.; Radwanski, M.; Sokolowski, J.; Cichomski, M.; Bourgi, R.; Hardan, L.; Sauro, S.; Lukomska-Szymanska, M. Micro-CT Evaluation of Microgaps at Implant-Abutment Connection. Materials 2023, 16, 4491. [Google Scholar] [CrossRef]
- Takechi, M.; Ishioka, Y.; Ninomiya, Y.; Ono, S.; Tada, M.; Nakagawa, T.; Sasaki, K.; Murodumi, H.; Shigeishi, H.; Ohta, K. Morphological Evaluation of Bone by CT to Determine Primary Stability—Clinical Study. Materials 2020, 13, 2605. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L.; D’Amico, C.; Ronsivalle, V.; Cicciù, M.; Cervino, G. Single Dental Implant Restoration: Cemented or Screw-Retained? A Systematic Review of Multi-Factor Randomized Clinical Trials. Prosthesis 2024, 6, 871–886. [Google Scholar] [CrossRef]
- Capparé, P.; Vinci, R.; Di Stefano, D.A.; Traini, T.; Pantaleo, G.; Gherlone, E.F.; Gastaldi, G. Correlation between Initial BIC and the Insertion Torque/Depth Integral Recorded with an Instantaneous Torque-Measuring Implant Motor: An in vivo Study. Clin. Implant. Dent. Relat. Res. 2015, 17, e613–e620. [Google Scholar] [CrossRef] [PubMed]
- Berberi, A.; Dagher, M.; Kanj, W.; Amine, E.; Aramouni, P. Micromovement Evaluation of Original and Compatible Abutments at the Implant–abutment Interface. J. Contemp. Dent. Pract. 2016, 17, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Camps-Font, O.; Rubianes-Porta, L.; Valmaseda-Castellón, E.; Jung, R.E.; Gay-Escoda, C.; Figueiredo, R. Comparison of external, internal flat-to-flat, and conical implant abutment connections for implant-supported prostheses: A systematic review and network meta-analysis of randomized clinical trials. J. Prosthet. Dent. 2023, 130, 327–340. [Google Scholar] [CrossRef]
- Cicciù, M.; Bramanti, E.; Cecchetti, F.; Scappaticci, L.; Guglielmino, E.; Risitano, G. FEM and Von Mises analyses of different dental implant shapes for masticatory loading distribution. Oral Implantol. 2014, 7, 1–10. [Google Scholar]
- Lo Russo, L.; Guida, L.; Mariani, P.; Ronsivalle, V.; Gallo, C.; Cicciù, M.; Laino, L. Effect of Fabrication Technology on the Accuracy of Surgical Guides for Dental-Implant Surgery. Bioengineering 2023, 10, 875. [Google Scholar] [CrossRef]
| Stage | Description |
|---|---|
| Identification | Records identified through database searching (n = 256) |
| Screening | Records after duplicates removed (n = 200) |
| Eligibility | Full-text articles assessed for eligibility (n = 45) |
| Eligibility | Full-text articles excluded (n = 37) |
| Included | Studies included in qualitative synthesis (n = 8) |
| Study | Random Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Other Bias |
|---|---|---|---|---|---|---|---|
| Yu YJ et al. (2019) [11] | Low | Low | Unclear | Unclear | Low | Low | Low |
| Min CK et al. (2021) [12] | Unclear | Unclear | Unclear | Low | Low | Low | Low |
| González-García R et al. (2013) [13] | Low | Low | Unclear | Unclear | Low | Low | Low |
| Neldam CA et al. (2015) [14] | Low | Low | Low | Low | Low | Low | Low |
| Kapishnikov S et al. (2021) [15] | Low | Low | Low | Low | Low | Low | Low |
| Hsu JT et al. (2013) [16] | Unclear | Unclear | Unclear | Unclear | Low | Low | Low |
| Parsa et al. (2013) [17] | Low | Low | Low | Low | Low | Low | Low |
| Bissinger O et al. (2017) [18] | Low | Low | Low | Low | Low | Low | Low |
| Author and Year | Type of Study | Sample Size and Type | Main Results | Statistical Results |
|---|---|---|---|---|
| Yu YJ et al. (2019) [11] | Animal Study | 24 rabbits | Fluoride exposure significantly reduced BMD and BIC ratios in rabbits. | Bone volume around the implants increased in a time-dependent manner in both groups. |
| Min CK et al. (2021) [12] | Experimental Study | Polyurethane synthetic bone blocks | Metal artifacts in CBCT images quantified effectively using micro-CT. | Spearman correlation coefficients for microstructural parameters varied with alpha angle changes. |
| González-García R et al. (2013) [13] | Observational Study | 39 bone biopsies from 31 patients | Strong correlation between RBD from CBCT and Bone Volume/Total Volume (BV/TV) from micro-CT. | Pearson’s correlation coefficient (r = 0.858, p < 0.001) between RBD and BV/TV. |
| Neldam CA et al. (2015) [14] | Experimental Study | Goat mandible model | High-resolution synchrotron micro-CT accurately depicts bone microarchitecture. | Peri-implant bone volume fraction increased to 50% and leveled out at 80% at 400 μm distance. |
| Kapishnikov S et al. (2021) [15] | Experimental Study | In vitro | Static compressive loads significantly increased the microgap size at the implant–sleeve connection. | Mean gap difference after cyclic compressive load was 0.3 ± 0.15 μm. |
| Hsu JT et al. (2013) [16] | Experimental Study | Artificial sawbone models | Positive correlation between bone stiffness, BIC, and initial implant stability. | Regression correlation coefficient was 0.96 for correlations of ISQ with elasticity of cancellous bone and 3D BIC%. |
| Parsa A et al. (2013) [17] | Observational Study | 20 human mandibular cadavers | Strong correlations between CBCT and Multislice Computed Tomography (MSCT) density, and CBCT and micro-CT BV/TV measurements. | Excellent correlation observed between MSCT Hounsifield Unit (HU) and micro-CT BV/TV (r = 0.91). |
| Bissinger O et al. (2017) [18] | Animal Study | 54 implants in 14 minipigs | Strong correlations between 3D micro-CT and 2D histomorphometry in evaluating osseointegration. | Strong correlations (p < 0.0001) for BIC, inner ring, and outer ring between micro-CT and histomorphometry. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galletti, F.; D’Angelo, T.; Fiorillo, L.; Lo Giudice, P.; Irrera, N.; Rizzo, G.; Cervino, G. Micro-CT Structure Analysis on Dental Implants: Preliminary In Vitro Trial. Prosthesis 2024, 6, 1437-1447. https://doi.org/10.3390/prosthesis6060104
Galletti F, D’Angelo T, Fiorillo L, Lo Giudice P, Irrera N, Rizzo G, Cervino G. Micro-CT Structure Analysis on Dental Implants: Preliminary In Vitro Trial. Prosthesis. 2024; 6(6):1437-1447. https://doi.org/10.3390/prosthesis6060104
Chicago/Turabian StyleGalletti, Fulvia, Tommaso D’Angelo, Luca Fiorillo, Paola Lo Giudice, Natasha Irrera, Giuseppina Rizzo, and Gabriele Cervino. 2024. "Micro-CT Structure Analysis on Dental Implants: Preliminary In Vitro Trial" Prosthesis 6, no. 6: 1437-1447. https://doi.org/10.3390/prosthesis6060104
APA StyleGalletti, F., D’Angelo, T., Fiorillo, L., Lo Giudice, P., Irrera, N., Rizzo, G., & Cervino, G. (2024). Micro-CT Structure Analysis on Dental Implants: Preliminary In Vitro Trial. Prosthesis, 6(6), 1437-1447. https://doi.org/10.3390/prosthesis6060104








