Flexural Properties of Three Novel 3D-Printed Dental Resins Compared to Other Resin-Based Restorative Materials
Abstract
1. Introduction
2. Materials and Methods
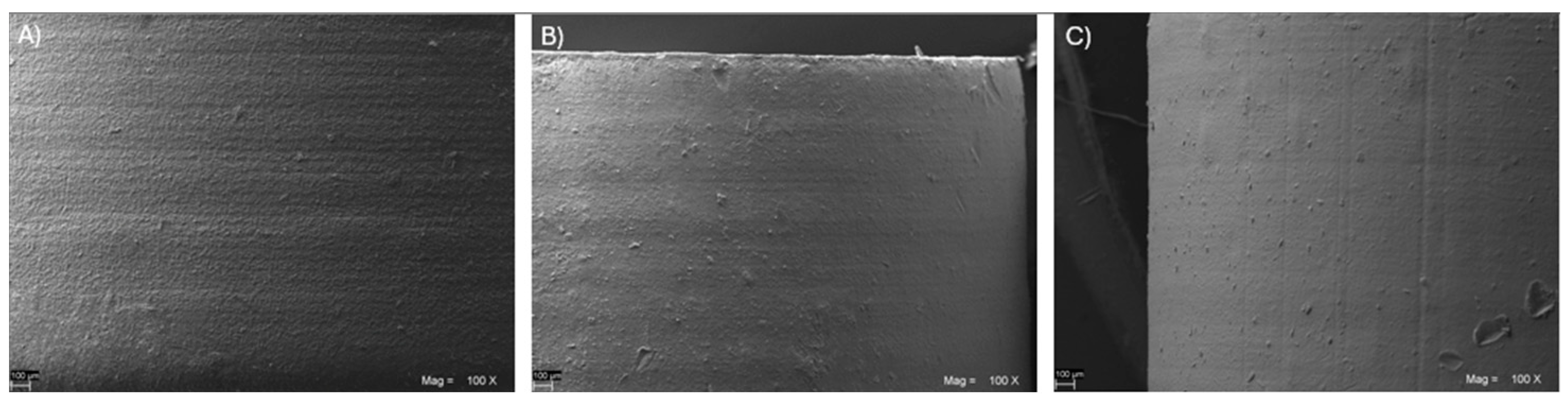
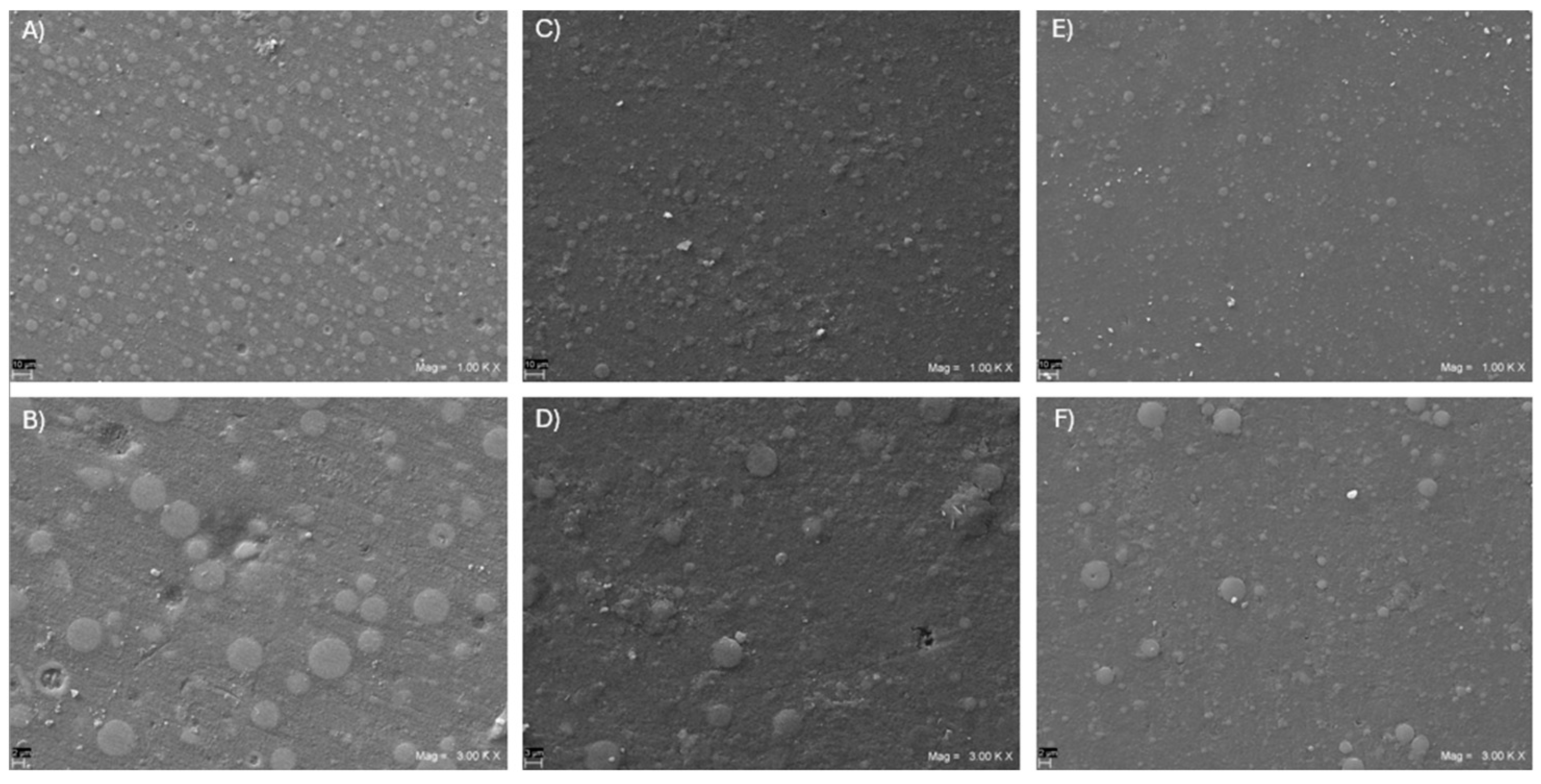
Scanning Electron Microscope (SEM) Analysis
3. Results
4. Discussion
5. Conclusions
- (1)
- CAD/CAM fiber-reinforced epoxy resins seem to show superior flexural strength and the highest flexural modulus of elasticity amongst the resin-based dental materials;
- (2)
- Different 3D-printed resins may show significant differences in flexural properties when compared to one another;
- (3)
- In terms of flexural strength, Irix-Max seems the more promising among the different 3D-printed resins, with a flexural strength that may be even superior to conventional heat-cured BACRs, justifying its safe use as a permanent restorative material;
- (4)
- The other two 3D-printed resins tested, Irix-Plus and Temporis, showed superior flexural strength compared to the conventional S-PMMA (by Sintodent) but reduced performances when compared to G-PMMA and the conventional D-PMMA (by Dentsply-Sirona), so their use as permanent restorative materials should be still considered with some caution.
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Ferracane, J.L. Resin composite—State of the art. Dent. Mater. 2011, 27, 29–38. [Google Scholar] [CrossRef]
- Fasbinder, D.J. Computerized technology for restorative dentistry. Am. J. Dent. 2013, 26, 115–120. [Google Scholar]
- Takeuchi, Y.; Koizumi, H.; Furuchi, M.; Sato, Y.; Ohkubo, C.; Matsumura, H. Use of digital impression systems with intraoral scanners for fabricating restorations and fixed dental prostheses. J. Oral Sci. 2018, 60, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, B.C.; Chen, J.H.; Kontogiorgos, E.D.; Murchison, D.F.; Nagy, W.W. Flexural strength of denture base acrylic resins processed by conventional and cad-cam methods. J. Prosthet. Dent. 2020, 123, 641–646. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J. A comparison of the flexural and impact strengths and flexural modulus of cad/cam and conventional heat-cured polymethyl methacrylate (pmma). J. Prosthodont. 2020, 29, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J.; Özcan, M. A comparison of the surface properties of cad/cam and conventional polymethylmethacrylate (pmma). J. Prosthodont. 2019, 28, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Al-Qarni, F.D.; Goodacre, C.J.; Kattadiyil, M.T.; Baba, N.Z.; Paravina, R.D. Stainability of acrylic resin materials used in cad-cam and conventional complete dentures. J. Prosthet. Dent. 2020, 123, 880–887. [Google Scholar] [CrossRef]
- Gruber, S.; Kamnoedboon, P.; Özcan, M.; Srinivasan, M. Cad/cam complete denture resins: An in vitro evaluation of color stability. J. Prosthodont. 2021, 30, 430–439. [Google Scholar] [CrossRef]
- Alp, G.; Johnston, W.M.; Yilmaz, B. Optical properties and surface roughness of prepolymerized poly(methyl methacrylate) denture base materials. J. Prosthet. Dent. 2019, 121, 347–352. [Google Scholar] [CrossRef]
- Murat, S.; Alp, G.; Alatalı, C.; Uzun, M. In vitro evaluation of adhesion of candida albicans on cad/cam pmma-based polymers. J. Prosthodont. 2019, 28, e873–e879. [Google Scholar] [CrossRef]
- Al-Fouzan, A.F.; Al-Mejrad, L.A.; Albarrag, A.M. Adherence of candida to complete denture surfaces in vitro: A comparison of conventional and cad/cam complete dentures. J. Adv. Prosthodont. 2017, 9, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Ayman, A.D. The residual monomer content and mechanical properties of cad\cam resins used in the fabrication of complete dentures as compared to heat cured resins. Electron. Physician 2017, 9, 4766–4772. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Schimmel, M.; Naharro, M.; O’Neill, C.; McKenna, G.; Müller, F. Cad/cam milled removable complete dentures: Time and cost estimation study. J. Dent. 2019, 80, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Kattadiyil, M.T.; Jekki, R.; Goodacre, C.J.; Baba, N.Z. Comparison of treatment outcomes in digital and conventional complete removable dental prosthesis fabrications in a predoctoral setting. J. Prosthet. Dent. 2015, 114, 818–825. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.Y.; Yang, T.C.; Wang, T.M.; Lin, L.D. Effects of fabrication techniques on denture base adaptation: An in vitro study. J. Prosthet. Dent. 2020, 124, 740–747. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, J.B.; Ramos, V., Jr.; Dickinson, D.P. Comparison of fit of dentures fabricated by traditional techniques versus cad/cam technology. J. Prosthodont. 2019, 28, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Cantin, Y.; Mehl, A.; Gjengedal, H.; Müller, F.; Schimmel, M. Cad/cam milled removable complete dentures: An in vitro evaluation of trueness. Clin. Oral Investig. 2017, 21, 2007–2019. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, B.J.; Goodacre, C.J.; Baba, N.Z.; Kattadiyil, M.T. Comparison of denture base adaptation between cad-cam and conventional fabrication techniques. J. Prosthet. Dent. 2016, 116, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Kalberer, N.; Mehl, A.; Schimmel, M.; Müller, F.; Srinivasan, M. Cad-cam milled versus rapidly prototyped (3d-printed) complete dentures: An in vitro evaluation of trueness. J. Prosthet. Dent. 2019, 121, 637–643. [Google Scholar] [CrossRef]
- Wang, W.; Yu, H.; Liu, Y.; Jiang, X.; Gao, B. Trueness analysis of zirconia crowns fabricated with 3-dimensional printing. J. Prosthet. Dent. 2019, 121, 285–291. [Google Scholar] [CrossRef]
- Shubert, J.; Bell, M.A.L. Photoacoustic imaging of a human vertebra: Implications for guiding spinal fusion surgeries. Phys. Med. Biol. 2018, 63, 144001. [Google Scholar] [CrossRef]
- Best, C.; Strouse, R.; Hor, K.; Pepper, V.; Tipton, A.; Kelly, J.; Shinoka, T.; Breuer, C. Toward a patient-specific tissue engineered vascular graft. J. Tissue Eng. 2018, 9, 2041731418764709. [Google Scholar] [CrossRef] [PubMed]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive technology: Update on current materials and applications in dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Özcan, M. Additive manufacturing technologies used for processing polymers: Current status and potential application in prosthetic dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Kattadiyil, M.T.; AlHelal, A. An update on computer-engineered complete dentures: A systematic review on clinical outcomes. J. Prosthet. Dent. 2017, 117, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.S.; Kim, J.E.; Jeong, S.H.; Choi, Y.J.; Ryu, J.J. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3d-printed resins with various printing orientations. J. Prosthet. Dent. 2020, 124, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Fang, Y.; Liao, Y.; Chen, G.; Gao, C.; Zhu, P. 3d printing and digital processing techniques in dentistry: A review of literature. Adv. Healthc. Mater. 2019, 21, 1801013. [Google Scholar] [CrossRef]
- Alharbi, N.; Alharbi, S.; Cuijpers, V.; Osman, R.B.; Wismeijer, D. Three-dimensional evaluation of marginal and internal fit of 3d-printed interim restorations fabricated on different finish line designs. J. Prosthodont. Res. 2018, 62, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Jang, Y.; Sim, J.Y.; Park, J.K.; Kim, W.C.; Kim, H.Y.; Kim, J.H. Evaluation of the marginal and internal fit of a single crown fabricated based on a three-dimensional printed model. J. Adv. Prosthodont. 2018, 10, 367–373. [Google Scholar] [CrossRef]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.S.; Jiang, H.B. A review of 3d printing in dentistry: Technologies, affecting factors, and applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef]
- Atria, P.J.; Bordin, D.; Marti, F.; Nayak, V.V.; Conejo, J.; Jalkh, E.B.; Witek, L.; Sampaio, C.S. 3d-printed resins for provisional dental restorations: Comparison of mechanical and biological properties. J. Esthet. Restor. Dent. 2022, 34, 804–815. [Google Scholar] [CrossRef] [PubMed]
- Mecholsky, J.J., Jr. Fracture mechanics principles. Dent. Mater. 1995, 11, 111–112. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Ko, K.H.; Huh, Y.H.; Park, C.J.; Cho, L.R. Effects of the thickness ratio of zirconia-lithium disilicate bilayered ceramics on the translucency and flexural strength. J. Prosthodont. 2020, 29, 334–340. [Google Scholar] [CrossRef]
- Aati, S.; Akram, Z.; Ngo, H.; Fawzy, A.S. Development of 3d printed resin reinforced with modified zro(2) nanoparticles for long-term provisional dental restorations. Dent. Mater. 2021, 37, e360–e374. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L. Evaluation of the mechanical properties and degree of conversion of 3d printed splint material. J. Mech. Behav. Biomed. Mater. 2021, 115, 104254. [Google Scholar] [CrossRef]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3d printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef]
- Chung, S.M.; Yap, A.U.; Chandra, S.P.; Lim, C.T. Flexural strength of dental composite restoratives: Comparison of biaxial and three-point bending test. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 71, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Paranhos, M.P.G.; Burnett, L.H., Jr.; Magne, M.; Belser, U.C. Fatigue resistance and failure mode of novel-design anterior single-tooth implant restorations: Influence of material selection for type iii veneers bonded to zirconia abutments. Clin. Oral. Implant. Res. 2011, 22, 195–200. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3d-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- Sulaiman, T.A. Materials in digital dentistry-a review. J. Esthet. Restor. Dent. 2020, 32, 171–181. [Google Scholar] [CrossRef]
- Zimmermann, M.; Ender, A.; Attin, T.; Mehl, A. Fracture load of three-unit full-contour fixed dental prostheses fabricated with subtractive and additive cad/cam technology. Clin. Oral. Investig. 2020, 24, 1035–1042. [Google Scholar] [CrossRef] [PubMed]
- Patnana, A.K.; Vanga, N.R.V.; Vabbalareddy, R.; Chandrabhatla, S.K. Evaluating the fracture resistance of fiber reinforced composite restorations—An in vitro analysis. Indian. J. Dent. Res. 2020, 31, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Tsujimoto, A.; Barkmeier, W.W.; Takamizawa, T.; Latta, M.A.; Miyazaki, M. Mechanical properties, volumetric shrinkage and depth of cure of short fiber-reinforced resin composite. Dent. Mater. J. 2016, 35, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Lassila, L.; Keulemans, F.; Vallittu, P.K.; Garoushi, S. Characterization of restorative short-fiber reinforced dental composites. Dent. Mater. J. 2020, 39, 992–999. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Alshahrani, F.A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Ateeq, I.S.; Helal, M.A.; Al-Harbi, F.A. Strength and surface properties of a 3d-printed denture base polymer. J. Prosthodont. 2022, 31, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Fouda, S.M. Factors affecting flexural strength of 3d-printed resins: A systematic review. J. Prosthodont. 2023, 32, 96–110. [Google Scholar] [CrossRef] [PubMed]
- Borella, P.S.; Alvares, L.A.; Ribeiro, M.T.; Moura, G.F.; Soares, C.J.; Zancopé, K.; Mendonça, G.; Rodrigues, F.P.; das Neves, F.D. Physical and mechanical properties of four 3d-printed resins at two different thick layers: An in vitro comparative study. Dent. Mater. 2023, 39, 686–692. [Google Scholar] [CrossRef]
- Chen, S.; Yang, J.; Jia, Y.G.; Lu, B.; Ren, L. A study of 3d-printable reinforced composite resin: Pmma modified with silver nanoparticles loaded cellulose nanocrystal. Materials 2018, 11, 2444. [Google Scholar] [CrossRef]
- Gad, M.M.; Al-Harbi, F.A.; Akhtar, S.; Fouda, S.M. 3d-printable denture base resin containing sio(2) nanoparticles: An in vitro analysis of mechanical and surface properties. J. Prosthodont. 2022, 31, 784–790. [Google Scholar] [CrossRef]
- Derban, P.; Negrea, R.; Rominu, M.; Marsavina, L. Influence of the printing angle and load direction on flexure strength in 3d printed materials for provisional dental restorations. Materials 2021, 14, 3376. [Google Scholar] [CrossRef]
- Srinivasan, M.; Kalberer, N.; Kamnoedboon, P.; Mekki, M.; Durual, S.; Özcan, M.; Müller, F. Cad-cam complete denture resins: An evaluation of biocompatibility, mechanical properties, and surface characteristics. J. Dent. 2021, 114, 103785. [Google Scholar] [CrossRef] [PubMed]
- Väyrynen, V.O.; Tanner, J.; Vallittu, P.K. The anisotropicity of the flexural properties of an occlusal device material processed by stereolithography. J. Prosthet. Dent. 2016, 116, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Unkovskiy, A.; Bui, P.H.-B.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef] [PubMed]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L.V. 3d-printed vs. Heat-polymerizing and autopolymerizing denture base acrylic resins. Materials 2021, 14, 5781. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Lambart, A.L.; Stawarczyk, B.; Reymus, M.; Spintzyk, S. Postpolymerization of a 3d-printed denture base polymer: Impact of post-curing methods on surface characteristics, flexural strength, and cytotoxicity. J. Dent. 2021, 115, 103856. [Google Scholar] [CrossRef]
- Shin, D.-H.; Rawls, H.R. Degree of conversion and color stability of the light curing resin with new photoinitiator systems. Dent. Mater. 2009, 25, 1030–1038. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, P.P.A.; Moreira, A.D.; Moraes, R.R.; Cavalcante, L.M.; Schneider, L.F.J. Color stability, conversion, water sorption and solubility of dental composites formulated with different photoinitiator systems. J. Dent. 2013, 41, e67–e72. [Google Scholar] [CrossRef] [PubMed]
- Bayarsaikhan, E.; Lim, J.H.; Shin, S.H.; Park, K.H.; Park, Y.B.; Lee, J.H.; Kim, J.E. Effects of postcuring temperature on the mechanical properties and biocompatibility of three-dimensional printed dental resin material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Park, J.M.; Kim, S.K.; Heo, S.J.; Koak, J.Y. Flexural strength of 3d-printing resin materials for provisional fixed dental prostheses. Materials 2020, 13, 3970. [Google Scholar] [CrossRef]
- Valenti, C.; Federici, M.I.; Masciotti, F.; Marinucci, L.; Xhimitiku, I.; Cianetti, S.; Pagano, S. Mechanical properties of 3d-printed prosthetic materials compared with milled and conventional processing: A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2022. [Google Scholar] [CrossRef]
- Duarte, S.; Sartori, N.; Phark, J.-H. Ceramic-reinforced polymers: Cad/cam hybrid restorative materials. Curr. Oral Health Rep. 2016, 3, 198–202. [Google Scholar] [CrossRef]
- Curran, P.; Cattani-Lorente, M.; Wiskott, H.W.A.; Durual, S.; Scherrer, S.S. Grinding damage assessment for cad-cam restorative materials. Dent. Mater. 2017, 33, 294–308. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.; El Shehawy, D.; El-Naggar, G.J.A.S.D.J. Fracture resistance of interim restoration constructed by 3d printing versus cad/cam technique (in vitro study). Egypt. Dent. J. 2020, 23, 13–20. [Google Scholar]
- Corbani, K.; Hardan, L.; Skienhe, H.; Özcan, M.; Alharbi, N.; Salameh, Z. Effect of material thickness on the fracture resistance and failure pattern of 3d-printed composite crowns. Int. J. Comput. Dent. 2020, 23, 225–233. [Google Scholar] [PubMed]
- Taşın, S.; Ismatullaev, A. Comparative evaluation of the effect of thermocycling on the mechanical properties of conventionally polymerized, cad-cam milled, and 3d-printed interim materials. J. Prosthet. Dent. 2022, 127, 173.e1–173.e8. [Google Scholar] [CrossRef] [PubMed]
- Digholkar, S.; Madhav, V.N.; Palaskar, J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J. Indian. Prosthodont. Soc. 2016, 16, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Pantea, M.; Ciocoiu, R.C.; Greabu, M.; Totan, A.R.; Imre, M.; Țâncu, A.M.C.; Sfeatcu, R.; Spînu, T.C.; Ilinca, R.; Petre, A.E. Compressive and flexural strength of 3d-printed and conventional resins designated for interim fixed dental prostheses: An in vitro comparison. Materials 2022, 15, 3075. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Meyers, M.J.; Zandinejad, A.; Özcan, M. A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J. Esthet. Restor. Dent. 2019, 31, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Dai, Z.; Liu, L.; Hu, H.; Dai, Q.; Zhang, Z. Tuning the interfacial mechanical behaviors of monolayer graphene/pmma nanocomposites. ACS Appl. Mater. Interfaces 2016, 8, 22554–22562. [Google Scholar] [CrossRef]
- Hu, X.; Su, E.; Zhu, B.; Jia, J.; Yao, P.; Bai, Y. Preparation of silanized graphene/poly (methyl methacrylate) nanocomposites in situ copolymerization and its mechanical properties. Compos. Sci. Technol. 2014, 97, 6–11. [Google Scholar] [CrossRef]
- Vallés, C.; Kinloch, I.A.; Young, R.J.; Wilson, N.R.; Rourke, J.P. Graphene oxide and base-washed graphene oxide as reinforcements in pmma nanocomposites. Compos. Sci. Technol. 2013, 88, 158–164. [Google Scholar] [CrossRef]
- Bacali, C.; Badea, M.; Moldovan, M.; Sarosi, C.; Nastase, V.; Baldea, I.; Chiorean, R.S.; Constantiniuc, M. The influence of graphene in improvement of physico-mechanical properties in pmma denture base resins. Materials 2019, 12, 2335. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, F.; Vadini, M.; Buonvivere, M.; Valerio, A.; Di Cosola, M.; Piattelli, A.; Biferi, V.; D’Arcangelo, C. In vitro mechanical properties of a novel graphene-reinforced pmma-based dental restorative material. Polymers 2023, 15, 622. [Google Scholar] [CrossRef] [PubMed]
| Experimental Group | Type of Material | Manufacturing Process | Batch Number | Manufacturer | Material Trade Name |
|---|---|---|---|---|---|
| Fiber-reinforced Epoxy | CAD/CAM Fiber-reinforced Epoxy Resin | CAD/CAM milling | 2208 | Bioloren, Varese, Italy | Trilor |
| G-PMMA | CAD/CAM Graphene-reinforced Polymethylmethacrylate | CAD/CAM milling | L18101120161 | Andromeda Nanotech, Lesignano de’ Bagni, Italy | G-Cam |
| Conventional D-PMMA | CAD/CAM Polymethylmethacrylate | CAD/CAM milling | 85196 | Dentsply Sirona, Charlotte, NC, USA | Multilayer PMMA |
| Conventional S-PMMA | CAD/CAM Polymethylmethacrylate | CAD/CAM milling | 2247220 | Sintodent, Roma, Italy | Cad-Cam shaded disc for provisional prosthesis |
| Irix-Max | Photosensitive ceramic filled hybrid composite | CAD/CAM 3D-printing | 2314941 | DWS S.r.l, Thiene, Italy | Irix Max |
| Irix-Plus | Photosensitive hyrid composite | CAD/CAM 3D-printing | 2310941 | DWS S.r.l, Thiene, Italy | Irix Plus |
| Temporis | Photosensitive composite | CAD/CAM 3D-printing | 2301271 | DWS S.r.l, Thiene, Italy | Temporis |
| BACR | Light and heat cured Bis-acrylate based composite resins | Conventional layering technique | 2022006932 | Micerium S.p.A., Avegno, Genova, Italy | Enamel Plus Biofunction |
| Experimental Group | Flexural Strength (MPa) | Flexural Modulus (MPa) |
|---|---|---|
| Fiber-reinforced Epoxy | 418.0 a (51.0) | 14,672.2 a (1296.5) |
| Irix-Max | 135.0 b (2.3) | 4429.1 c (570.6) |
| BACR | 127.9 c (17.6) | 10,010.1 b (720.6) |
| G-PMMA | 120.1 d (9.7) | 2700.2 d (180.8) |
| Conventional D-PMMA | 113.3 e (13.7) | 2506.8 e (485.4) |
| Irix-Plus | 103.9 f (3.8) | 2750.2 d (260.9) |
| Temporis | 101.3 f (6.4) | 2824.2 d (219.7) |
| Conventional S-PMMA | 88.9 g (6.7) | 2137.2 f (149.6) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Angelis, F.; D’Amario, M.; Jahjah, A.; Frascaria, M.; Vadini, M.; Sorrentino, E.; Biferi, V.; D’Arcangelo, C. Flexural Properties of Three Novel 3D-Printed Dental Resins Compared to Other Resin-Based Restorative Materials. Prosthesis 2024, 6, 619-630. https://doi.org/10.3390/prosthesis6030043
De Angelis F, D’Amario M, Jahjah A, Frascaria M, Vadini M, Sorrentino E, Biferi V, D’Arcangelo C. Flexural Properties of Three Novel 3D-Printed Dental Resins Compared to Other Resin-Based Restorative Materials. Prosthesis. 2024; 6(3):619-630. https://doi.org/10.3390/prosthesis6030043
Chicago/Turabian StyleDe Angelis, Francesco, Maurizio D’Amario, Ali Jahjah, Massimo Frascaria, Mirco Vadini, Edoardo Sorrentino, Virginia Biferi, and Camillo D’Arcangelo. 2024. "Flexural Properties of Three Novel 3D-Printed Dental Resins Compared to Other Resin-Based Restorative Materials" Prosthesis 6, no. 3: 619-630. https://doi.org/10.3390/prosthesis6030043
APA StyleDe Angelis, F., D’Amario, M., Jahjah, A., Frascaria, M., Vadini, M., Sorrentino, E., Biferi, V., & D’Arcangelo, C. (2024). Flexural Properties of Three Novel 3D-Printed Dental Resins Compared to Other Resin-Based Restorative Materials. Prosthesis, 6(3), 619-630. https://doi.org/10.3390/prosthesis6030043











