1. Introduction
According to the World Health Organization, an estimated 1.3 billion people (16% of the world’s population) have a permanent disability [
1], of which at least 10 million are estimated to be people with amputation; of those, 3 million people possess an upper limb amputation condition [
2]. International studies on the causes and prevalence of this level of amputation are limited. The leading cause is trauma, often from work accidents, traffic accidents, and falls [
3,
4,
5]. However, congenital upper limb deficiencies are also present. According to the Centers for Disease Control and Prevention, these malformations occur in approximately 1 out of every 1900 births in the United States [
6]. In cases such as this, specific congenital malformations can lead to limitations in performing tasks, similar to traumatic cases. This is especially true for congenital conditions between the elbow and shoulder.
Individuals with upper limb disabilities often face challenges when performing daily tasks [
7]. The level of difficulty increases with the severity of the amputation. Assistive technologies have been developed to aid individuals with disabilities in performing these tasks. The United Nations global report on assistive technologies states that one in three individuals globally require such devices [
8]. An assistive product helps individuals maintain and improve their functioning and independence, promoting their well-being. This is particularly important for people with upper limb disabilities, who may benefit from prostheses.
Upper limb prostheses can be categorized as active or passive based on their function. An active prosthesis replaces the muscle’s mechanical function by applying force transmission [
9]. In contrast, a passive prosthesis adjusts to a specific movement when an external force is applied [
10]. Passive prostheses are typically used to address aesthetic needs or to compensate for postural balance with the weight of the prosthesis. The internal mechanisms for transmitting movement and force are highly complex in both categories. This is because these prostheses require actuators that do not compromise the weight of the prosthesis while also being compact, light, and aesthetically pleasing. This allows the prosthesis to resemble the human hand in size and weight. However, achieving this purpose is only sometimes possible due to the incompatibility between certain levels of amputation and the desired type of prosthesis. Customization characteristics are crucial in the final adaptation of an upper limb prosthesis [
11]. The prosthetic fit and desired functionality are ultimately defined by factors such as the nature of the accident [
12], the condition of the stump post-surgery, the use given to the stump [
13], and the age, build, and size of the user [
14].
As mentioned above, due to the number of characteristics that need to be considered, numerous reviews have been published on the design and development of upper extremity prostheses. Each has focused on establishing classifications based on use, amputation level, and operating model. Still, other articles, such as that of Brack et al. [
15], also address user satisfaction and device dropout concerning prostheses.
In recent years, there have been works such as “Techniques and Control Systems in Upper-Limb Bionic Prostheses: A Technological Review” that classify 71 articles on bionic prostheses based on the type of control used, including fuzzy logic control systems, PID controllers, and PD controllers [
16]. The authors highlight Technology Readiness Levels (TRL) as a significant classification criterion [
17]. Of all the cited articles, 51 use a superficial electromyographic signal (sEMG). The study published in 2022 focuses on disarticulated-level wrist amputations and transradial amputations. The authors note that 90% of the works studied are within TRL-6. Additionally, they identified that the prostheses presented were designed for individuals between 18 and 54, and more information needed to be presented regarding pediatric prostheses.
Regarding control systems, prominent in the state of the art are invasive modes such as intramuscular electrodes for reading and sensory stimulation [
18]. Additionally, nerve interfaces with activations such as Targeted Muscle Reinnervation (TMR) involve surgically rerouting residual nerves from an amputated limb to intact muscles, enabling the user to control the prosthetic limb by thinking about moving those muscles [
19]. Muscle–Selective Nerve Transfer, akin to TMR, entails transferring nerves to different muscles to enhance control signals. Direct Nerve Interfaces involve placing electrodes directly on or within peripheral nerves to record neural signals for control. It also works to provide sensory feedback [
20,
21].
In the invasive realm, neural implants also stand out in recent years. Neural Implants encompass two main categories: (i) Peripheral Nerve Implants involve surgically implanting micro-electrode arrays or cuffs around peripheral nerves to record neural signals or provide stimulation [
22] and, (ii) at the same time, Neural–Muscular Interfaces entail implanting electrodes at an interface between nerves and muscles to record motor commands or provide feedback [
23]. Tendon-Based Interfaces also stand out. These consist of two key categories: Tendon-Driven Prostheses, which utilize tendons that would typically move the missing limb to control the prosthesis, with sensors on the residual limb detecting tendon movements and translating them into prosthetic actions [
24], and Tendon-Activated Sensory Feedback, where tendons can provide sensory feedback by activating sensors upon stretching or compression [
25].
On the other hand, the review presented in “A Robotic Prosthesis as a Functional Upper-Limb Aid: An Innovative Review” contains a descriptive analysis of 83 reviewed prostheses published in the last five years [
26]. In this paper, the amputation levels that occur in most cases are the transradial level and wrist disarticulation. The authors point out that there is still a lot of work to be completed regarding the cost of the prostheses compared, as well as the improvement of ergonomics for a better adaptation of the users to their prostheses. However, due to the search methodology, this paper needs to show the trend over time in prosthetic development.
This loss of perspective on prosthetic advances over time is a constant in the reviewed works. The main drawback lies in knowing the technological maturity that the same prosthesis, designed and developed in the laboratory, can reach when studied over time. To obtain this relevant information, it is also necessary to carry out a search in commercial repositories as well as in patent databases. Such a search also allows us to extend the search to prosthesis models that are not typically transradial or disarticulated at the wrist.
By analyzing all these aspects, this paper aims to give a comprehensive overview of the current development of upper limb prostheses for adults, classified according to amputation level, according to the year of publication, according to input control, and according to Technology Readiness Levels. Therefore, scientific articles, patents, and commercial products for different levels of upper limb amputation are characterized, analyzing the trend of upper limb prosthesis development in different aspects such as degrees of freedom (DoF), weight, TRL, input control, and their current limitations categorized by the four types of amputation (transmetacarpal, transcarpal, transradial and transhumeral).
This paper is structured as follows:
Section 2: Methodology presents the study method by which the different prosthesis development classified by type of bibliographic resource was obtained.
Section 3: Biomechanics of the Arm presents information on the anatomy of a human hand, including aspects of degrees of freedom and weight by segments.
Section 4: Results presents the different classifications for the developed prostheses.
Section 5: Discussion presents the information divided by each type of amputation. Finally,
Section 6: Conclusion explains and highlights the results.
2. Methodology
We registered our study protocol in PROSPERO on 1 February 2024 (CRD42024504389). We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines in the
Supplementary Materials.
2.1. Data Sources and Search Strategy
In order to initiate the search, a research question was formulated: “What is the trend in the development of upper limb prostheses?” This question allowed us to focus the search for appropriate information. Next, several databases were identified for the search, such as Scopus, IEEE Xplore, Springer, PubMed, Frontiers, and Espacenet. Subsequently, the search terms were determined, incorporating keywords related to the topic, such as “development”, “upper limb prostheses”, “Development of Upper-Limb Prostheses” and “Upper-Limb Prostheses”.
2.2. Inclusion Criteria
The search was focused between 2018 and 2023; furthermore, articles were selected according to the following inclusion criteria:
Articles dealing with advances in the design and implementation of transhumeral, transradial, transcarpal, and transmetacarpal prostheses, with mechanical and dynamic specifications of the results of their implementation.
First or second quartile journals (Q1 and Q2) from university repositories or international congresses.
Complete prosthesis design proposals, mentioning the size characteristics, degree of freedom, material, and whether the prosthesis design had mechanical and kinetic specifications.
Patents with an update within the period from 2018 to 2023.
Commercial prostheses that present a technical data sheet with the mechanical, kinematic, and electrical characteristics of the prosthesis.
2.3. Exclusion Criteria
The systematic search for articles carried out from 2018 to 2023 was performed considering the following exclusion criteria:
Developments of disarticulated shoulder prostheses without adaptations to other amputation levels were not considered.
Articles focused solely on the design of the prosthesis control system.
Pediatric prostheses because these prostheses have mechanical limitations, such as weight and size.
Commercial prostheses that have only descriptive information with no information on technical specifications.
Discontinued commercial prostheses that the company no longer develops.
Commercial prostheses from the same company, with similar functions to other versions, only differ because they can be used for another level of amputation.
2.4. Quality Assessment
The article selection process involved identifying and choosing those pertinent to the research topic. This began with examining the titles and abstracts to ascertain their alignment with the established inclusion criteria. Following this, an in-depth review of each article’s content was conducted. Our search was primarily centered on developments featured in journals and conference proceedings listed in Scimago or Citescore ranking. Initially, we focused on works that fall into the Q1/Q2 quartiles and subsequently broadened our search to include those in the Q3/Q4 quartiles. The credibility of these chosen articles was assessed, prioritizing those published in scientific journals with high trust and regard, specifically, those ranked in the Q1 and Q2 quartiles.
2.5. Data Extraction
The data from the selected articles were synthesized to answer the research question in several aspects; for this purpose, several factors related to the development of upper limb prostheses were analyzed, such as the level of amputation, year of publication, degrees of freedom, weight, prosthesis material, grips, and gestures.
The characteristics delineated above, along with the outcomes, discussions, and conclusions derived from the analyzed articles, constituted input data for the team to stratify the identified prostheses in alignment with their respective stages of Technological Readiness Level (TRL). This categorization considered whether the prosthesis under scrutiny represented a finalized design, development without user testing, or a completed development subjected to user trials in controlled or uncontrolled settings. The comprehensive categorization outcomes are delineated in
Section 4.3.
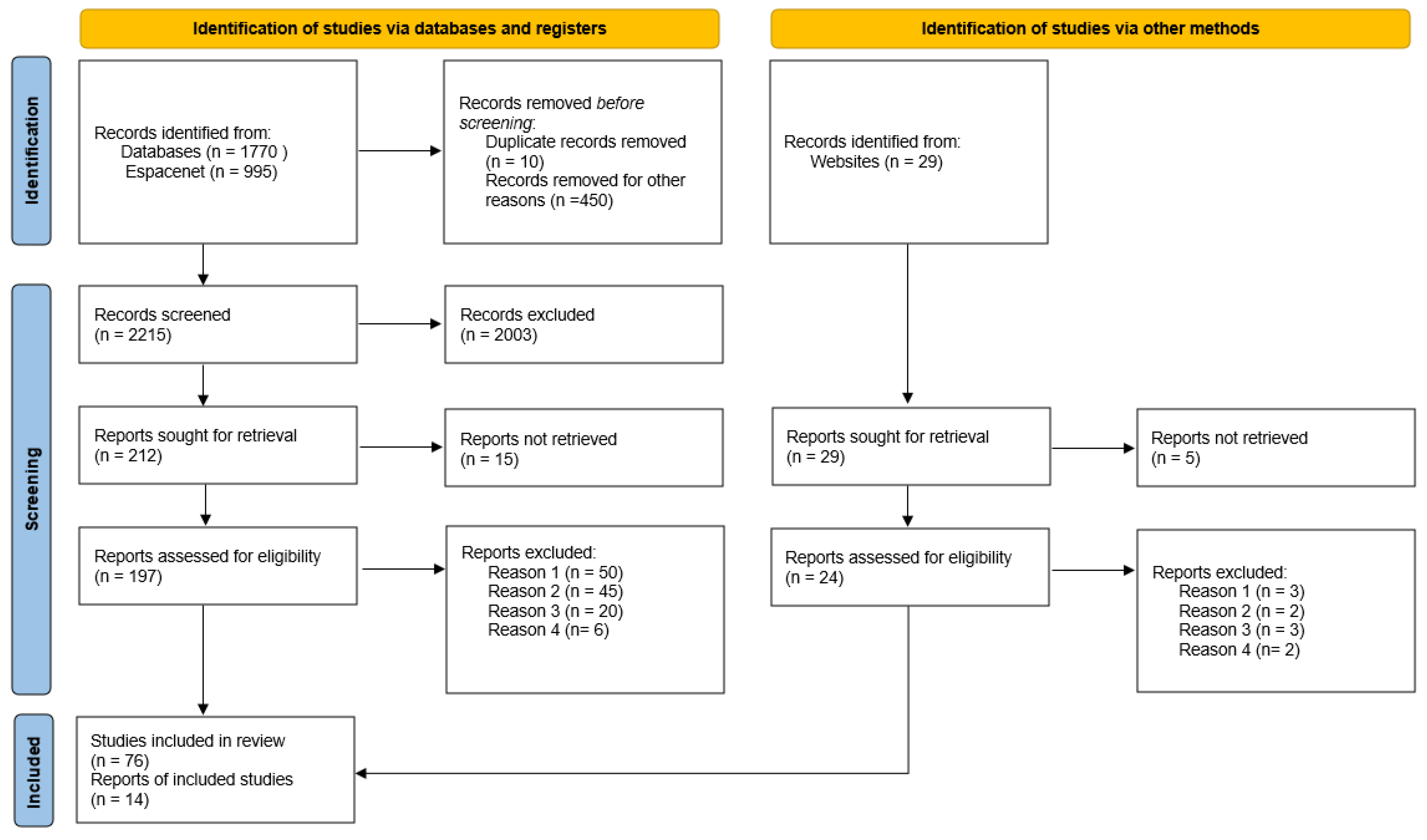
2.6. Search Performance
The final search yielded 2794 articles: Scopus contributed 403, IEEE Xplore 1095, Springer 115, PubMed 1009, Frontiers 172, and Espacenet 995; the website search found 29 commercial prostheses. We eliminated 2003 articles and 5 websites, leaving 2215 articles and 29 websites. After filtering with the exclusion criteria, 197 articles and 24 websites were selected for review, as shown in the PRISMA flow diagram [
27] of
Figure 1. Finally, 90 selected prostheses were analyzed and classified by amputation level: transmetacarpal, transcarpal, transradial, and transhumeral. Essential aspects such as year of publication, TRL, degrees of freedom, weight, material, grips, and gestures were extracted.
3. Biomechanics of the Arm
This section details the joints and muscles of the hand, forearm, and arm to describe the arm’s mobility and an approximation of the weight of the arm segments.
Arm movements are described by considering the person in anatomical position and positioned in space, using the convention of the three planes of movement. A sagittal plane divides the person into two equal parts through an imaginary cut longitudinally, in which a mediolateral axis crosses the plane perpendicularly. The frontal plane divides the person into two equal parts through an imaginary cut longitudinally, which crosses the anteroposterior axis perpendicularly. The last plane, the transverse plane, is a transverse cut at the level of the umbilicus, which divides the person into an upper and lower part, and the axis that crosses perpendicularly is the vertical axis [
28]. Considering this, the description can be refined by examining the anatomical position. Flexion and extension movements occur in the sagittal plane, while abduction and adduction movements occur in the frontal plane. These movements have a different range of motion (ROM) for each joint, according to the European standardized method made by the Association for the Study of Osteosynthesis (AO) in Switzerland, which is described in
Table 1.
The upper limb has 24 joints; in the hand, there are about 20 joints and 23 degrees of freedom, of which the most important are the five metacarpophalangeal (MCP), the four proximal interphalangeal (PIP), the five distal interphalangeal (DIP) [
30], the carpometacarpal, the midcarpal, and the intercarpal joints. The wrist, also called the carpus, is located between the forearm, and the carpal bones allow two movements: flexion/extension and abduction/adduction. At the elbow, there are three joints: the humerocubital trochlearthrosis (allows flexion and extension), the humeroradial, and the radioulnar: the last two joints are the ones that pronate and supinate the forearm. Concerning muscles, there are 19 muscles in the hand [
31], 20 muscles in the forearm [
32], and 5 muscles in the upper arm segment [
33]. This is why the upper limb has excellent mobility and can precisely perform fine movements.
On the other hand, The upper limb represents approximately 5% of a total body weight [
34], which represents the weight range, shown as the lower limit of the ideal weight of a 1.5 m female and the upper limit of the ideal weight of a 1.94 m male. The hand weight range is between 283 g and 565 g, the forearm weight range is from 755 g to 1400 g, and the arm weight range is between 1320 g and 2635 g.
4. Results
Four amputation levels were considered to classify upper limb prostheses. Considerations for limiting each amputation level are considered:
Transmetacarpal: Considered in amputations below the metacarpophalangeal joint, this level has wrist and elbow movement but contains the carpal bones; other authors call this a finger amputation, including interphalangeal amputation. Sometimes, this is the partial loss of some fingers or only the thumb. From the search presented, this is the level of amputation with the most minor prosthetic development.
Transcarpal: Amputation level between the radiocarpal joint and the metacarpophalangeal joint, including partial amputation of the hand, is considered by other authors. This contains wrist and elbow movement as methods of action in the case of mechanical prostheses.
Transradial: Amputation level below the elbow joint includes disarticulated wrist amputation; this does not contain the wrist joint and goes along the radius bone because it is larger distally than the ulna.
Transhumeral: Amputation level below the glenohumeral joint along the humerus. At this level, there is no elbow or wrist joint; in some cases, the method of prosthetic attachment is usually a harness around the shoulder and torso [
35,
36].
Each type of amputation is sub-classified in the type of bibliographic source mentioned in
Section 2 because the information for prostheses presented different characteristics, according to their bibliography.
For transmetacarpal amputation, seven developments were found divided in the following way: two are mentioned in scientific articles [
37,
38], three are mentioned in invention patents [
39,
40,
41], and two in commercial prostheses [
42,
43] were found. For transcarpal amputation, 25 developments were found divided in the following way: 10 are mentioned in scientific articles [
44,
45,
46,
47,
48,
49,
50,
51,
52,
53], 13 are mentioned in invention patents [
54,
55,
56,
57,
58,
59,
60,
61,
62,
63,
64,
65,
66], and 2 in commercial prostheses [
67,
68]. In the transradial amputation, 40 developments were found divided in the following way: 24 are mentioned in scientific articles [
69,
70,
71,
72,
73,
74,
75,
76,
77,
78,
79,
80,
81,
82,
83,
84,
85,
86,
87,
88,
89,
90,
91], 10 are mentioned in invention patents [
92,
93,
94,
95,
96,
97,
98,
99,
100,
101], and 6 in commercial prostheses [
102,
103,
104,
105,
106,
107]. For transhumeral amputation, 18 developments were found divided in the following way: 10 are mentioned in scientific articles [
35,
36,
108,
109,
110,
111,
112,
113,
114], 4 are mentioned in invention patents [
115,
116,
117,
118], and 4 in commercial prostheses [
119,
120,
121,
122].
There was a more significant development of transradial prostheses both at the level of scientific articles and commercial products; this may be because they have an excellent space on which to place the components but do not need an additional fastening, such as a harness. Therefore, they have more possibilities of presenting a development that involves new characteristics at the levels of material, prosthetic control mechanism, etc.
In contrast, the transmetacarpal level can be observed, which presents a mechanical difficulty in operating a prosthesis the size of the fingers. Most design developments focus on this, with nine prostheses found.
Based on the search carried out, other criteria can be used to classify the prostheses:
4.1. According to the Year of Publication
This classification considered information from 2018 to 2023. For forty-six scientific articles: in 2018, seven were found [
50,
53,
78,
88,
108,
110,
111]; in 2019, seven [
38,
48,
51,
76,
82,
86,
109]; in 2020, twelve [
37,
44,
45,
46,
47,
49,
70,
81,
91,
112,
113,
123]; in 2021, nine [
36,
52,
69,
79,
83,
84,
85,
87,
89]; in 2022, eight [
35,
71,
72,
73,
74,
75,
80,
124]; and in 2023, three [
77,
90,
114].
As for thirty invention patents: in 2018, one was found [
95]; in 2019, ten [
41,
54,
56,
61,
63,
66,
94,
96,
97,
99]; in 2020, eight [
57,
58,
59,
64,
92,
93,
101,
118]; in 2021, two [
55,
62]; in 2022, seven [
39,
60,
65,
98,
115,
116,
117]; and in 2023, two [
40,
100].
Finally, for fourteen commercial prostheses: three [
42,
68,
106] were found in 2018, three [
104,
107,
122] in 2019, none in 2020, four [
102,
103,
119,
121] in 2021, three [
43,
105,
120] in 2022, and one [
67] in 2023.
With this, we can see an increasing trend from 2018 to 2019, which stagnates and decreases until 2021. Indeed, in 2020, there has yet to be a record of commercial product launches of upper limb prostheses, most of which were postponed.
4.2. According to Input Control
Currently, there are different types of prostheses; each type has characteristics predisposed to its use depending on the actions the user prioritizes as fundamental and repetitive. The first group is passive prostheses that adjust to a specific movement utilizing springs without active elements; the other focuses on favoring postural balance and are aesthetically similar to the missing limb.
Another group is active prostheses, which have mechanisms that mechanically substitute a muscular function; for this, prosthetic systems such as an energy source, a force transmission system, and a gripping device are needed; classified by their actuation system, they can be as shown in
Table 2.
- (a)
Mechanical prosthesis:
Generally, mechanical upper limb prostheses are driven by wrist or elbow movement, depending on the level of amputation, to transmit through cords to close or open the hand [
43,
53,
56,
65,
96].
- (b)
Pneumatic prosthesis:
Its mechanism is made by air compression, which moves various mechanisms such as large pistons and requires many bulky accessories [
49].
- (c)
Electric prostheses:
They use electric motors to perform the movement; with a battery, usually rechargeable lithium, this increases manufacturing costs and needs to consider the humidity in the prosthesis.
There are different electric prostheses, such as:
Electromyography (EMG): These sensors measure the potential difference due to a contraction of a muscle group; these electrodes can be in direct contact with the muscles (promotes a more stable signal) or be superficial (attached to the skin). Despite taking a long time to develop, it is susceptible to the state of the muscle and the location of the electrodes [
38,
42,
44,
45,
47,
103,
110].
Electroencephalography (EEG): Direct or surface electrodes control it through the brain’s electrical activity. This form of control is the most novel, and there is great potential for further research into this form of control [
72,
86].
Force Myography (FMG): It is a sensor that records the mechanical activity of the muscle during muscle contraction: this sensor captures the force sensors to perceive variations in muscle volume during contraction. It has less electrical interference than EMG [
70].
Near-infrared: Simultaneous monitoring of perfusion level and muscle oxygenation produces a signal with high spatial resolution [
125]. This monitoring method is relatively new, and only scientific articles propose this system [
89,
125,
126].
Synergistic posture mapping: This control is performed using the orientation and contact forces of different parts of the person [
37,
71,
76,
99], an example being detecting the position of the thumb using a gyroscope to move the prosthetic fingers [
37].
Hybrid: This is the mixture of two or more control systems mentioned above; in the literature, the most common is Electromyography–Electroencephalography [
35,
105,
115,
124]. This is intended to improve the accuracy of gesture prediction with AI. However, electromyography can also be complemented with mechanical forces to have a more simplified mechanism of action [
104].
In the reviewed state of the art, it is evident that the predominant control used in electronically activated prostheses is the surface reading of electromyographic signals. However, few studies have used electroencephalographic signal reading for prosthetic control, individually or in combination with electromyography signals. This may be due to three reasons: the low incidence of cases that warrant them (transhumeral amputations where electromyography signals are insufficient) [
35,
109], the cost of electroencephalography reading systems, and the length of the training and calibration process for electroencephalography reading compared to that of electromyography training. However, with recent advances in artificial intelligence [
127,
128,
129,
130], electromyography signals can be made more accessible, offering the possibility of more natural and intuitive control of the prosthesis.
4.3. According to Technology Readiness Levels
TRL is a tool for identifying and characterizing the level of development of an innovation project, with which the proximity of the project to the market can be categorized; to be able to place it in nine levels, specific criteria are taken into account, which have been adapted as follows for the development of upper limb prostheses [
17].
TRL 1: A system or mechanism for the movement of the prosthesis, or an advance close to this, is proposed.
TRL 2: The differentiating component of the prosthesis is demonstrated to be feasible, utilizing a fault theorem or simulation software, and is associated with a specific application.
TRL 3: The prosthesis is developed utilizing a low-fidelity prototype where it may or may not have the movement or be of the desired size.
TRL 4: The prosthesis is developed utilizing a prototype with the materials and weights expected according to a previous simulation.
TRL 5: The prosthesis is validated utilizing attachment tests or validation of all the programmed grips.
TRL 6: At this point, we start with validating the prosthesis in a laboratory environment with fewer participants, i.e., less than five people; we also have results such as the maximum load force and closing speed of the hand, among others.
TRL 7: The prototype is taken to perform the daily actions of the participants in a natural environment.
TRL 8: The point of TRL 7 is carried out but on a larger scale of participants. The certifications or requirements to go to the market are already in place.
TRL 9: The development of the prototype meets all the requirements set out through several large-scale validations. At this stage, it is on the market or months away from launch.
As shown in
Table 3, no prostheses at the TRL8 level have been evaluated in a natural environment but on a large scale of participants. Additionally, certifications or requirements are needed to enter the market. In the development of prostheses, this is a difficult point to overcome, as evidenced in the table.
It should be noted that the patents are in the TRL range from one to two, but this does not indicate that the prostheses of the patents found are at that level of technical maturity because a follow-up search of those patents that could have a scientific article of implementation that could show the current state of the prosthesis was not performed.
5. Discussion
5.1. Development of Input Control, Number of Degrees of Freedom, and Grips on Prostheses According to the Level of Amputation
In limb prosthetics, the challenge intensifies as the level of amputation ascends from transmetacarpal to transcarpal, transradial, and transhumeral. Each level presents unique obstacles and demands specific considerations in the design and functionality of prosthetic limbs. This discussion focuses on prosthetic technology’s evolution and current state, particularly examining the advancements in input control, technology readiness levels, the number of degrees of freedom (DoF), weight, material, and grips (when the prosthesis holds an object) or gestures (when the prosthesis performs a movement without holding anything) achievable, tailored to these specific levels of upper limb amputations.
5.1.1. Transmetacarpal
This level of amputation is where the least amount of prosthetic developments are found.
Table 4 features a range of degrees of freedom (DoF) between 10 and 4. This range is minimal because this level of amputation only requires the mobility of the fingers, particularly finger flexion at the metacarpophalangeal joint, which is the movement with a greater arc length that allows closing of the hand. The thumb, at this level of amputation, is not essential to be able to perform grips [
37,
42]. For this reason, prostheses at this level have a range of 1–8 programmed grips and weigh between 100 and 500 g, which is within the range of an average hand. The range of weights at this level of prostheses depends on the materials, which varies from polymers to metals.
The mechanism of action of the prosthesis control can be mechanical or with EMG. For these cases, the physiological signal is obtained from muscles near the wrist, although there is also a novel prosthesis that does not use any of the above mechanisms of action; rather, it uses a gyroscope located in the thumb to obtain information on the gestures to be used and thus achieves the maximum number of gestures found [
37].
In the Abarca et al. prosthesis [
38], specific mention is made of the DoF of each phalanx and its weight, a grip force of 4.6 N, and a speed for each finger, with non-participant testing. However, the prosthesis needs a palmar space to function; the palmar space is only for storing the components. Unlike the prosthesis in [
37], this one has only one input control component in the thumb, and all the mechanisms of movement are compact in the phalanges with a lower weight but a lesser DoF.
5.1.2. Transcarpal
Prostheses at this level of amputation (see
Table 5) present a much broader range of DoF, from 2 to 22, because they have movement in more phalangeal joints and for all fingers. Therefore, they start to focus on the grip, but there is still not enough space in the prosthesis to obtain grip strength and add motors and the pulley and lever system. That is why they only focus on the form of the grip of the prosthesis, which is expressed in the number of grips they have in a range of 1–14; at this level of amputation, the term self-adaptive grip begins to apply, where it is fed back to receive the location of the position of the prosthesis and thus adjust so that the pressure sensors indicate which phalanges require more or less grip and press evenly so one can hold a wide range of objects. The weights vary from 191 to 556 g, and it is expected that the weights increase as the prosthesis has a higher level of amputation. This weight is within the weight of an average hand, as indicated in
Section 3.
The EMG prosthesis of Dunai et al. [
46] shows comprehensive mobility, with a maximum angle of movement of thumb abduction of 80 degrees and with flexion/extension movements reaching from 0 to 90° in the thumb. Even this range of movements are more significant than the ROM of abduction and flexion/extension of the thumb, as shown in
Section 3. It has a more subtle movement of abduction of the little finger of up to 20° and up to 30° in the index finger. In function tests, obtaining results for the essential grip time in 1.3 s was possible.
Another remarkable thing about this prosthesis is that it uses soft materials, complemented by the fact that the tendons and ligaments are made of rubber. In addition, it is mentioned that it has an adaptive gripping property using force resistors that stop when it exceeds a set threshold using Force-Sensitive Resistors (FSR). The disadvantage of using soft materials is the increased wear; it is mentioned that after six months, the artificial tendons wear out.
The prosthesis was made of soft materials, and wear and tear on the extensor tendon and the artificial adductor muscle was noticeable after six months of use. The commercial prosthesis of Motorica [
68], made of stainless steel, aluminum, and polyamide, is a more rigid prosthesis with performance characteristics of a maximum load on the fingers of 15 kg and a capacity to lift 20 kg.
5.1.3. Transradial
This is the amputation with the highest amount of prosthesis development concerning the other amputation levels (see
Table 6). In this section, we mention both grips and predetermined gestures with a classification system known as the Pattern Recognition Classifier [
78].
Nevertheless, machine learning also plays a role in this context, encompassing a spectrum of grips from 0 to 30. A commercially available prosthesis from Max Bionic [
103] offers an extensive repertoire of 30 predefined gestures, marking a substantial advancement in gesture versatility. Originating from the renowned Max Bionic company, this prosthesis is designed to cater to diverse situations, underscoring its commitment to adaptability in practical usage scenarios. The weight of these prostheses is in a range of 100 g–950 g; this range indicates that they are very light since the lower limit is even less than the ideal weight of the hand and the upper limit of the weight of the prosthesis is almost half the maximum weight of an ideal hand. This, despite being advantageous, presents some difficulties in balancing the weight in the case of unilateral amputations. In these cases, the stability of the person is lost. Curiously, it was found that the [
75,
81] prostheses are lighter than transmetacarpal prostheses.
Transradial prostheses have a very different approach to mobility, which is reflected in the DoF range of 0–20, which is a smaller range than that of transmetacarpal prostheses; this is because they focus on movements with greater arc lengths, and finer movements are more difficult due to the extension of the prosthesis. An important point is that despite losing the mobility of the wrist due to amputation, many prostheses in this segment are rigid and only give mobility to the fingers, despite having space for additional mechanisms in the prosthesis. This limitation significantly impacts the prosthesis’s mobility, particularly in uncontrolled environments, hindering activities. Additionally, there are two aesthetic prostheses [
91] that focus on a design and weight similar to a human arm.
In the Prakash et al. FMG prosthesis [
70], they do not use EMG due to the advantages of FMG over EMG: FMG is cheaper, more accurate, and more consistent over time. With its own single-channel FMG design, it reaches 97% accuracy and 95% accuracy, in identifying the six gestures. They focus more on acquiring the signals from the new sensor rather than on the design of the prosthesis, which is why the mounting and the method of attachment where it connects to the residual limb is not the most suitable or comfortable. Unlike the mechanical prosthesis of Timm [
75], which needs tension in the elbow to work, the fastening in this prosthesis is fundamental. Hence, they use two Velcro straps and a fastening that reaches the elbow.
5.1.4. Transhumeral
This is the amputation (see
Table 7) in which most of the arm is compromised, the DoF range is between 10 and 3, and the maximum degree of freedom is tiny.
There are mechanical limitations that cannot obtain greater mobility due to the attachment or the weight that the prosthesis would have; at this point, the physiological signal is very scarce and attenuated because most of the arm is amputated, and most of the muscles are incomplete, so hybrid mechanisms such as EMG–EEG [
35], vision signals–EMG [
36], EMG–mechanical begin to appear. This difficulty can be observed because they sometimes only focus on a hybrid input control and EMG.
The range of grips is between 0 and 20, and the gestures range from 2 to 12. The weight is between 432 g and 3400 g; these weights should not exceed that of the other hand. However, this range of weights is far from the ideal weight for an arm since it should be in the range from 1320 g to 2635 g. As mentioned in
Section 3, this is three times lower than the ideal weight, which poses a challenge for achieving balance and weight compensation, and, in the case of the upper limit, it is approximately 30% higher, which is seen in the need to have more DoF, sacrificing weight, using a more significant number of actuators. At this level of amputation, prostheses adapt to different types of amputation [
110,
119] or are integrated with commercial subparts or past projects [
108].
In the Kastv et al. EMG prosthesis [
110], they note that the maximum weight it can lift is 3.3 kg in two seconds and that there is a delay of the muscle activity pick-up movement to the arm movement of 20.1 ms. This prosthesis has materials such as AlCu4Mg1, Titan Grade 5, and carbon fiber-reinforced epoxy. The movement of the hand is limited to gripping or gestures; due to the degrees of freedom in the wrist and elbow, the hand is rigid. Unlike the prosthesis of the company BionIT Labs [
120], which has 9 degrees of freedom in hand, this one also has an adaptive grip with a pressure sensor in the thumb to account for sliding and pads for the grip.
5.2. Material Selection in the Development of Prostheses
The materials used for each level of prosthesis will be analyzed for the tendency or benefits achieved by specific materials.
Transmetacarpal amputation: At the transmetacarpal amputation level, where partial hand loss occurs, the materials used for prosthetics are diverse, ranging from various polymers to metals. This variety in materials allows for a balance between durability, weight, and flexibility, essential for the functionality of partial hand prosthetics.
Transcarpal amputation: For transcarpal amputations, the material selection is similar to that of transmetacarpal amputations. However, there is a noticeable shift towards using Polylactic Acid (PLA). This preference is attributed to the need for highly customized prosthetic designs that accurately conform to the user’s residual limb. The advent of 3D printing technology provides a substantial advantage in this regard, facilitating the creation of more precise and personalized prosthetic components.
Transradial Amputation: Moving up to the transradial level, the trend of using polymers, often via 3D printing, continues. Notable instances include a prosthesis referenced in study [
75], which utilized a thermoplastic material combined with Fused Deposition Modeling (FDM) printing. Another innovative approach is seen in the prosthesis in [
81], where acrylic gears were used instead of traditional metal ones, and the entire prosthesis was fabricated from a polymer using 3D printing techniques. These adaptations highlight the focus on balancing strength and weight while maintaining functionality.
Transhumeral Amputation: There is a distinct shift towards using more rigid materials at the transhumeral level. Carbon fiber [
110,
120] is frequently chosen for its high strength-to-weight ratio, making it ideal for prosthetics that need to replace the entire arm’s functionality. Additionally, aluminum and titanium [
110,
117,
119] are also common choices. These materials offer the necessary durability and structural integrity while keeping the prosthetics lightweight, a crucial factor for user comfort and ease of use in full-arm prosthetics.
5.3. Development of Technology Readiness Levels
TRLs are a systematic metric/measurement system that supports the assessment of the maturity level of a particular technology.
Transmetacarpal amputation: The transmetacarpal category, concerning prosthetics for partial hand loss, shows a balanced distribution across various TRL stages, with entries in TRL 1, 2, 5, and 9. This suggests a research pipeline with technologies at both the conceptual stage (TRL 1, 2) and the fully developed stage (TRL 9). The presence of technologies in both the early and late stages of development indicates ongoing innovation and improvement in prosthetics for transmetacarpal amputees.
Transcarpal amputation: The data indicate a significant concentration of development at the lower TRLs (1, 2, 4, 5), with a notable number at TRL 1. This could imply a strong focus on fundamental research and early-stage development for transcarpal prosthetics. At the transcarpal amputation level (TRL 1), there is a necessity for an increased presence of prosthetic options in the market and the development of validation tests, mainly focusing on advancements that propose innovative systems or mechanisms for prosthetic movement. The skew towards lower TRLs suggests either emerging interest in this area or challenges in advancing technologies to higher readiness levels.
Transradial amputation: Transradial prostheses show a more evenly distributed development across the TRL spectrum, with a notable presence in TRL 5 and 6, indicating a focus on prototype development and testing in a relevant environment. This distribution suggests a mature field with ongoing development towards practical, user-friendly prosthetics. We are catering to below-elbow amputations.
Transhumeral amputation: Prosthetics for transhumeral amputations show significant development in the higher TRLs (6 and 9), indicating the presence of more developed and tested technologies. At the transhumeral amputation level, advancements are pretty varied, with a good balance between testing and validating prostheses released to the market. The focus on higher TRLs suggests that significant advancements have been made for above-elbow prosthetics, potentially offering users more sophisticated and functional solutions. However, there needs to be more production of patents and innovative ideas for mechanisms or differentiating forms of attachment.
The notable absence of technologies at Technology Readiness Level (TRL) 8 across all categories, as detailed in
Section 4, is a remarkable observation. This gap suggests a prevalent challenge within the prosthetics field, particularly in transitioning from prototype stages to the final stages of system completion and market deployment. This trend underscores a significant barrier to commercialization, revealing a lack of prosthetic devices ready for large-scale participant validation testing in real-world environments. Furthermore, there needs to be more evidence regarding certifications or approvals from regulatory entities, especially for prosthetics not associated with established brands. This finding indicates a crucial bottleneck in developing and accepting new prosthetic technologies, highlighting the need for focused efforts to bridge this gap in the commercialization process.
5.4. Evolution of Weight over the Years for Different Amputation Levels
The evolution of weight in grams over the years for different amputation levels can be seen in
Table 8. For the Transmetacarpal prosthesis, there has been an improvement in decreasing weight from 2018 to 2022, although there are four weight records for this amputation level. For the Transcarpal amputation level, there is a more significant number of prostheses where the weight could be obtained, and there is a tendency to lose weight in a more considerable way from 2018 to 2021; in 2023, the [
67] prosthesis breaks with this tendency. At both amputation levels, they meet within the weight range of a human hand.
For the Transradial amputation level, it presents 26 records of weights for which it is evident that the effort made by the development of prostheses does not present an improvement in decreasing the weight of a prosthesis but rather in modifying or improving the grips or gestures and including a more significant number of actuators for the approach of the developers so they see it as more necessary than making light prostheses. This can be evidenced to a greater degree for prostheses of a higher amputation level and transhumeral prostheses, where a positive trend in weight increase is evidenced.
5.5. Critical Technological Challenges and Future Prospects in Upper Limb Prostheses
The manuscript shows a precise industry and academic trend in using surface electromyographic signals to control reading. The ability to control prosthetic devices through gestures has significantly improved due to gesture classification algorithms and embedded systems advancements. These advancements have allowed for implementing algorithms with low computational costs that do not excessively drain the batteries of the prosthesis. Although there are other techniques for identifying the user’s intention, such as ultrasound muscle wave identification [
131], these new techniques do not offer an aesthetically pleasing embedding because of the awkwardness of placing the system on the user’s forearm or arm. Therefore, this type of control could be used in the future. However, the geometry has to be reduced.
On the other hand, the advancement of sensory feedback in commercial prostheses aims to create a more natural user experience. As seen in Graczyk et al. [
132], this evolution emphasizes the importance of “A naturalness of experience” for continuous prosthesis use. Users require a prosthesis with intuitive, prehensile, and sensory-rich features to enhance sensation experience, return to normalcy, self-efficacy, and user attitudes in everyday environments.
An ideal prosthesis should provide pressure and hand position feedback, resembling the missing limb segment in appearance and weight. This design allows minimal attention during manipulation, which is essential for practical use and social interactions. Self-efficacy, supported by sensory perception and confidence in grasping, is crucial for user satisfaction. User attitudes, developed over time with the prosthesis, are influenced by the perceived naturalness of the sensory experience. Collaboration between designers and users is necessary for integrating these aspects, fostering a sense of ownership to compensate effectively for the missing limb.
Expanding into prosthesis models working around haptics, commercial models such as Psyonic are implementing haptic feedback systems that can provide the user with the sensation of touch in proportion to the force applied by the fingers of the prosthesis on the object or surface [
102]. Romero and Elias [
133] have designed interfaces that can accommodate different models of prostheses with wireless units for monitoring stages, such as the placement of force and inertial sensors in the prosthetic hand, as well as the actuation stage, which includes a wristband with vibration motors. This design aims to increase the user’s sense of belonging to their prosthesis. In the future, it is expected that prostheses will be able to implement haptic strategies that transfer not only the sensation associated with pressure but also with parameters such as temperature, surface roughness, and imminent sliding of objects.
Our work shows a clear tendency to improve gesture functionality, reduce latency between user decision-making and actuation, and increase the number of possible gestures by adding more actuators. However, we found little research on reducing the weight of prostheses. Although techniques such as 3D printing and carbon fiber socket fabrication allow for lighter sockets, the weight of the units containing the actuators, such as palms, wrists, and forearm sockets, has not been reduced. This is because the actuators are often designed for multiple purposes rather than specifically for prosthetic applications. Therefore, it appears imperative to address the future requirement of reducing the weight of prostheses. A lightweight prosthesis can reduce fatigue in the socket area of the amputated limb during prolonged use. This improves the user’s sense of connection to the device.
Finally, it is essential to note that accessibility is as crucial as the functionality of the prosthesis. According to the global report on assistive technologies, four out of every five people with upper limb amputation live in developing countries [
8]. These countries have similar statistics regarding low minimum living wages, high rates of informality, limited access to private insurance premiums, and minimal local development of assistive technologies. This combination of factors creates the worst scenario for someone who has lost a limb due to working conditions. This is primarily because there are very few quality options that are accessible. In this sense, we reference the most advanced prostheses in our work. Motorica offers finger [
42] and hand prostheses [
68] for transcarpal and transmetacarpal amputations at a cost of up to USD 9600 [
134]. However, transhumeral prostheses, such as the LUKE-arm [
119], can cost up to USD 100,000 [
135], making them unaffordable for many disabled individuals. However, there are efforts being made to lower costs, such as those of Psyonic [
119], which offers transradial prostheses with haptic sensation for USD 3000 [
136]. Importing these to developing countries would increase import costs, resulting in a local cost that could double. In nations such as Peru, where the minimum monthly salary is USD 276, a worker would have to save for about two years without paying for food or housing expenses to afford the prosthesis.
6. Conclusions
With all of this detailed information, we can identify a trend in the development of prostheses at the transradial level where the control mechanism is EMG and based on different modifications that have arisen. Due to the difficulties with extraction of signal quality and the sensitivity of it, these solutions can be a hybrid control mechanism in which another type of biological signal is included.
Transmetacarpal and transcarpal prostheses are very specific for each user who must have a personalized form, so their development is focused on the degrees of freedom of the joints and the force they can withstand.
Building upon the foundation of transradial prostheses, transhumeral prostheses represent a natural progression in upper limb amputation technology. However, at this level of amputation, a key challenge arises: the prosthetic weight falls considerably below the lower threshold of a human arm. This imbalance affects overall stability and leads to a noticeable deviation in the axis of gravity compared to the non-amputated arm. On the other hand, exceeding the upper weight limit reveals another dilemma—the need for additional actuators to enhance torque and increase the number of degrees of freedom (DoF) in the prosthesis. This trade-off between weight and functionality becomes particularly evident in cases of significant amputations. As for their manufacture, they focus on their cutting, which can be used for lower levels of amputations. The movement of the hand is diminished, and the focus is much more on movements with more significant displacement. The integration of this level of the prosthesis is practically the union of commercial parts.
The prosthesis developments at the patent level show a more centralized approach to making more practical mechanisms. Still, without considering the material, because there was not a bibliographic follow-up of the evolution of the prosthesis, it is not possible to detail the evolution or follow-up that this one has. Unlike scientific articles, which look for more updated versions of prostheses with previous investigations, in this type of bibliography, they proposed validation tests for the movements and mechanical tests to quantify the grasp and speed of making gestures or closing the hand. As far as commercial prostheses are concerned, the focus is on increasing the number of gestures and grips and also on having several ways of operating the prosthesis so that its production can be diversified and adapted to different conditions, in an attempt to generalize the users to be able to cover the masses.
All of this mainly affects the naturalness of the experience, which is influenced by the following factors to take into account: “sensation experience”, “return to normalcy”, “self-efficacy”, and “user attitudes”. However, the main factor to consider in the frequency of use of a prosthesis for a patient is the sensation experience; because of this, pressure feedback is developed in some prostheses to provide a tactile sensation in the prosthesis.