Abstract
The removable partial denture, despite new technologies and new materials, continues to play a significant role in clinical dental practice. The purpose of the following study was to evaluate the design of new retention devices in Kennedy class II scenarios. For the study of “lamellar” retentive devices, four prosthetists were chosen. According to inclusion and exclusion criteria, prosthetists selected 16 patients (8 women and 8 men) whose upper arches had to be rehabilitated using a removable partial prosthesis. The results showed that the parameters taken into consideration, such as satisfaction, stability, aesthetics, and retention, had an average score that was higher than 3.30 (range 1–4), with an average standard deviation of 0.6225 in the four parameters, indicative that the data were relatively homogeneous and coherent. In conclusion, we can state that the skeletonized prosthesis with lamellar retentions, designed for Kennedy class II scenarios, has shown high acceptance in selected patients.
1. Introduction
Despite the constant evolution of digital technologies and the extensive development of implant techniques in dentistry, the removable partial denture (RPD) continues to play a significant role in clinical practice. This type of prosthesis, which has deep historical roots in the field of dental prosthetics, remains a valuable and versatile treatment option for patients with partial edentulism or multiple missing teeth. Its usefulness is supported by a series of advantages ranging from the preservation of residual dental tissue to aesthetic and functional customization [1,2,3]. While the dental landscape has witnessed notable advancements in digital technologies and the widespread use of dental implants to restore edentulous spaces, RPDs continue to meet specific clinical needs for patients who may not be adequately rehabilitated by other solutions. Their removable nature allows for the flexible management of ever-changing oral conditions, making corrections and modifications easier when needed. Furthermore, RPDs offer a less invasive alternative to implant procedures, making them particularly appropriate for patients who may not be ideal candidates for dental implants. The versatility of RPDs is also manifested in their ability to be adapted to patients’ individual preferences and needs. Thanks to modern computer-aided design (CAD) and computer-aided manufacturing (CAM) techniques, it is possible to create highly customized and comfortable RPDs that integrate harmoniously with oral morphology and improve the patient’s aesthetics [4,5,6,7,8]. The correct insertion of the skeletonized prosthesis and periodontal health ensure that these prostheses have a long life if carefully maintained; in other cases, the presence of destructive cavities, large reconstructed teeth, and periodontally compromised teeth may lead the patient to undergo dental extractions with a consequent modification of the prosthesis and, in some cases, also the relocation of the hook to another tooth, increasing the blemish even further [9,10,11]. This research has focused attention on a new design that involves the modification of the proximal plate through the addition of two functionally equivalent extensions to the hooks, with the aim of giving greater retention to the proximal plate while also improving the aesthetics of the skeletonized prosthesis [12,13]. This new design was previously used mainly in Kennedy class III patients; in our experimentation, we used this design in Kennedy class II patients to evaluate the efficiency, aesthetics, and retention of the prosthesis.
2. Materials and Methods
For the evaluation of RPDs with lamellar retentions in Kennedy class II scenarios, 4 freelance dentists in the Lombardy hinterland were selected, who gave their availability while respecting anonymity, to mainly carry out the branch of dental prosthetics. Each dentist was asked to conduct the following procedure: (a) select 4 patients (2 men and 2 women); (b) create an RPD in Kennedy class II edentulous cases for the upper arch with the new design where possible; (c) anonymously fill out (respecting privacy) four questionnaires, the first upon the delivery of the prosthesis (Appendix A Questionnaire A1), the second after 1 month, the third at 6 months, and the fourth at 12 months from delivery (Appendix A Questionnaires A2–A4). In total, a sample of 16 patients was selected, aged between 65 and 85 (patients considered elderly),who required rehabilitation in the upper arch with a removable partial prosthesis. All selected patients were not willing to undergo implant-prosthetic rehabilitation or rehabilitation with a fixed prosthesis; all patients chose mobile rehabilitation both for economic and anatomical reasons (lack of bone). All selected patients signed the informed consent form. The choice of only the upper arch for the evaluation of the parameters is mainly due to aesthetic reasons, as the more visible upper arch affects people’s smiles during social relationships [14,15,16,17]. Each dentist selected the patients, comprising 2 men and 2women, according to inclusion and exclusion criteria.
The inclusion criteria were as follows:
- Presence of partial edentulism classifiable as Kennedy class II;
- Absence of tori that could affect the adaptability of the prosthesis;
- Non-inclined residual elements (excessive undercut);
- Absence of para-functions;
- Presence of stable soft tissues not affected by periodontal disease or mucogingival lesions;
- Adequate depth of the roots of the abutment teeth;
- Informed consent of the patient and acceptance of the therapeutic rehabilitation plan with partial removable prosthesis and compliance with the dentist’s instructions.
- Age between 65 and 85 years.
- Patients who met the following exclusion criteria were excluded from the study:
- Poor oral hygiene and lack of patient compliance;
- Smoking habits (>10 cigarettes/day);
- Subjects suffering from oral pathologies;
- Active periodontal disease;
- Anomalies in the anatomy of the labial frenulum (which can interfere with the insertion and adaptability of the removable prosthesis);
- Drug addictions;
- Psychiatric pathologies;
- Subjects disbarred less than 5 years ago;
- Subjects on bisphosphonate therapy;
- Deep bite;
- Failure to consent to prosthetic rehabilitation and to comply with the dentist’s instructions.
The selected patients were numbered from 1 to 16 in order to respect their anonymity and privacy (Table 1).

Table 1.
Sample of selected patients.
All dentists were asked to speak with the dental technician about the design of the retentions and the proximal plate in order to have adequate retention and aesthetics. The dental technician was provided a drawing and wax-up of each project in the study model as a reference for replicating features in are movable partial denture (Figure 1a–d).
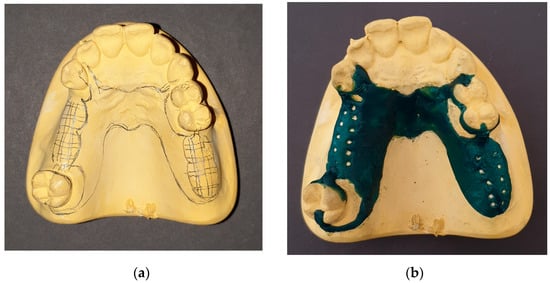
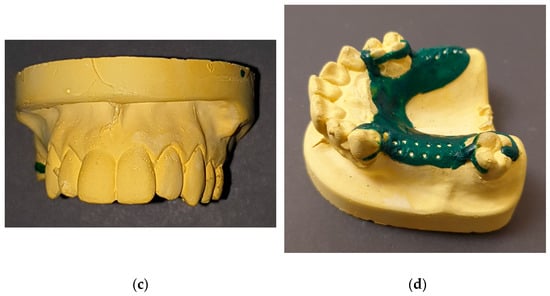
Figure 1.
(a) Drawing on study model—patient n° 14; (b) same study model with the wax applied for greater vision to the dental technician; (c) absence of visible hooks; (d) lamellar retentions on the proximal plate.
3. Results
The results are based on the information obtained from the questionnaires filled out by the patients in the sample at each check-up throughout a follow-up period of 12 months (Figure 2a–c, Figure 3a–c and Figure 4a–d); Table 2 contains the reference values. Some aspects such as satisfaction, stability, retention, and aesthetics were taken into consideration. The results were evaluated by averaging the values to provide a clear summary of any critical issues, while for the last questionnaire, the standard deviation was also calculated to evaluate any differences between the values of each observation and the average after 12 months.
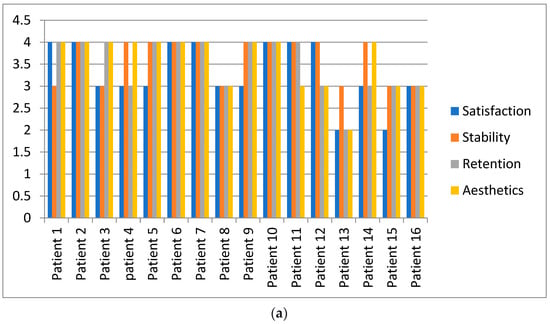
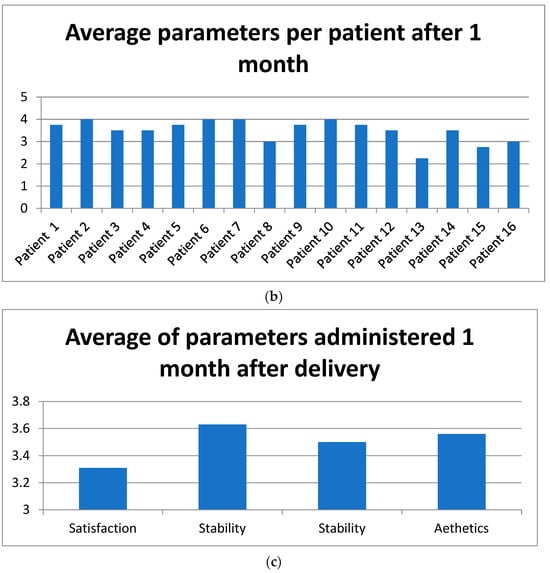
Figure 2.
(a–c): Results of Appendix A Questionnaire A2 administered 1 month after delivery. Evaluation with arithmetic mean of the results.
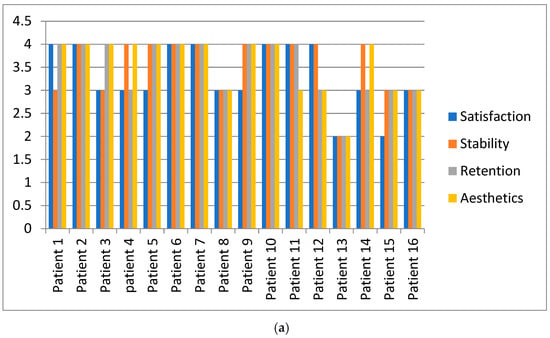
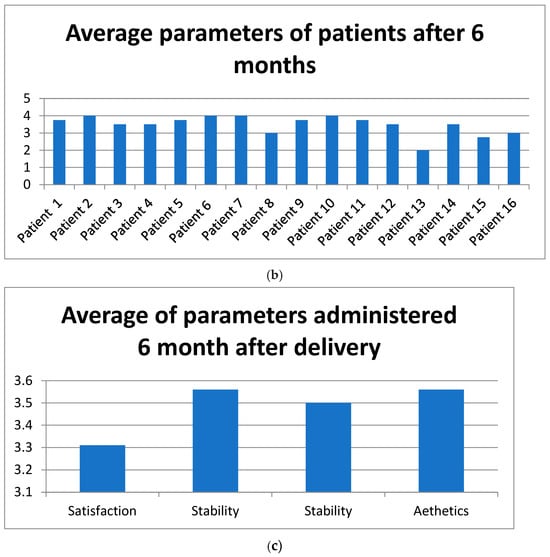
Figure 3.
(a–c): Results of Appendix A Questionnaire A2 administered 6 months after delivery. Evaluation with arithmetic mean of the results.
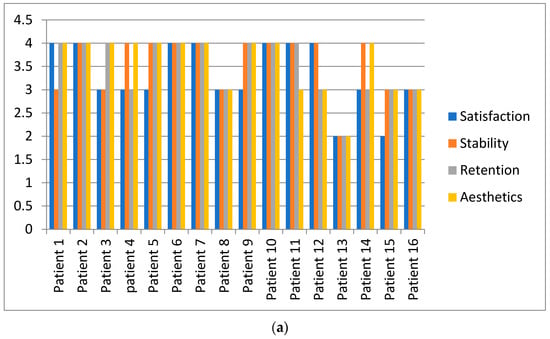
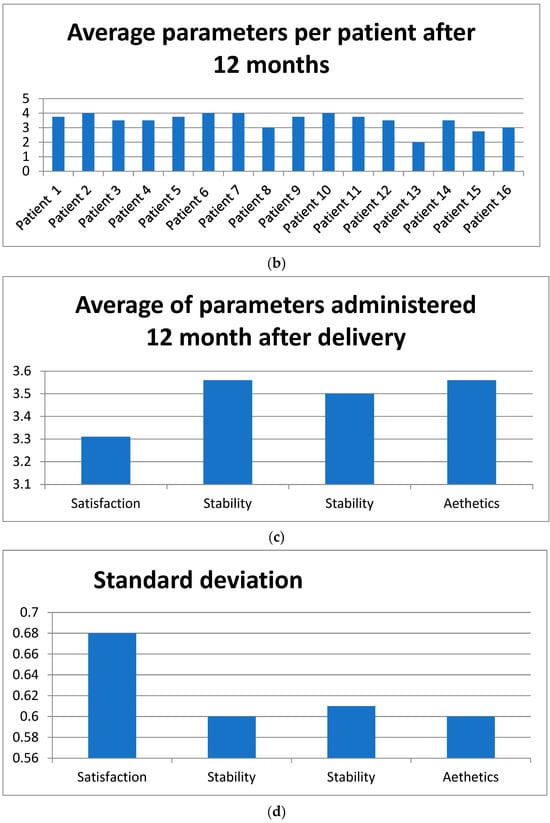
Figure 4.
(a–d): Results of Appendix A Questionnaire A3 administered 12 months after delivery.

Table 2.
Reference values legend.
During the checks, no patient underwent treatment on the abutment teeth and no clinically evident cavities were found in any element. No patient discontinued the use of the skeleton due to a lack of retention or stability. At the first check-up, one month after delivery, the patient identified with number 13 expressed a low score (2 out of 4) for three parameters (retention, aesthetics, and satisfaction), while the patient identified with number 15 expressed a low score for all parameters.
At the six-month check-up, a fracture in the resin element was only found in a single case (Appendix A Questionnaire A2—patient identified with number 8). Once the element was replaced, the patient was satisfied with the result, and at the subsequent check-up, the skeleton was found to be perfectly suitable. The patients identified with numbers 13 and 15 expressed low scores. The last questionnaire, at 12 months, was completed by only 14 patients; the patients identified with numbers 2 and 7 did not show up for the check-up. They were interviewed by telephone on the same day, using the same parameters, and they reported having no problems of any kind and that they were very satisfied. For our investigation, both patients were assigned the maximum value of 4 in all sections. The patient identified with number 13, despite the check-ups and attention, did not feel satisfied because he did not accept the idea of having a mobile prosthesis. The patient identified with number 15, despite the prosthesis being stable and aesthetic, did not feel satisfied.
The two most appreciated parameters among those evaluated in the questionnaires were aesthetics and stability, obtaining a score of 3.56 out of 4. Ten patients (62.5%) expressed a score of 4 out of 4 in the aesthetics and stability boxes. A detail found by the dentists during the checks was that no patient requested the activation of the lamellae retentions to improve retention, and only the two patients identified with numbers 9 and 5 used the adhesive paste for their dentures only on the occasions of social dinners and out off ear that the prosthesis might move. Another important fact is that in no case was it necessary to reline the prosthesis after some time (12 months).
4. Discussion
Edentulism still represents a very important problem to solve for dentists today. Dental caries and periodontal diseases are the main causal factors of tooth loss and, if not treated adequately, lead to edentulism [18,19,20,21]. The aesthetic judgment of patients, often negative regarding the removable partial denture, is very high due to the sight of the clasps and retention. Furthermore, after the delivery of the prosthesis, there are subsequent adjustments or modifications to the prostheses in the following years, and this is also due to periodontal problems [22,23,24]. The progress of different techniques that use new CAD/CAM technologies has allowed operators to use design software and different materials to find increasingly comfortable and aesthetic solutions for the patient [25,26,27,28,29,30,31]. The results of this study highlight how the lamellar retentions in the edentulous areas interspersed in Kennedy class II scenarios provide da high rating for the parameters examined. In these edentulous areas, we tried to exploit the modification of the proximal plate by designing it a few tenths of a millimeter below the undercut of the tooth so as to be more retentive; furthermore; if we consider the forces that acton an inclined plane, we can say that the friction force during the removal of the prosthesis represents the value of the angle between the tooth and the proximal plate. From a practical point of view, the inclined plane is used to move bodies using less effort than that necessary for vertical lifting; in prosthetic terms, the more adherent the proximal plate is, the greater the effort will be when removing the prosthesis. Of the total of sixteen patients selected, seven patients (43.75%) considered themselves very satisfied with the therapeutic choice, seven patients (43.75%) considered themselves satisfied, and only two patients (13.5%) did not consider themselves satisfied. The standard deviation values obtained for the four parameters were 0.68 for satisfaction, 0.60 for stability, 0.61 for retention, and 0.60 for aesthetics. Examining these values, we can say that the data are relatively homogeneous and coherent, with little significant variation between data points. This may indicate some stability or uniformity within the phenomenon or process being sampled.
In practical terms, the low values of standard deviation suggest that the measurements or observations are very similar to each other and that there are few significant fluctuations. However, it is important to consider that the sample size is small. The design of the skeletonized prosthesis with lamellar retentions in Kennedy class III edentulism was introduced in the 2000s. In the first study in 2003, the concept of “lamellae” is described, specifically focusing on the modification of the proximal plate of the skeleton by applying two extensions having the same functions as a hook. In the following year,2004, with the collection of a sample of 31 patients with Kennedy class III partial edentulism, the stability, retention, integrity, hygiene of the prosthesis, and conditions of the elements were checked for teeth that were adjacent to the edentulous area, evaluating the presence of caries and the mobility of the residual elements [12,13]. The search for aesthetics by modifying the hooks to make them increasingly aesthetic has been an objective pursued by researchers [32,33]. The design of the modified retentive devices is very aesthetic as they do not have a supra equatorial portion, and instead, their occlusal and lateral stability is maintained by the large secondary joint and the primary support designed distally (Figure 5). Clearly, the information and indications that the dentist must provide for the technician must be as precise as possible, especially with respect to the health of the periodontium [34,35,36].
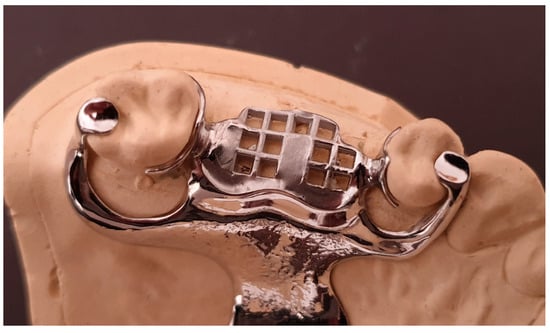
Figure 5.
View of the retentive means.
In light of the results obtained in previous studies and the current study, it is demonstrated that the design of the skeletonized prosthesis with lamellar retentions is not harmful to the periodontal structures of the residual teeth if the level of oral hygiene is maintained well and professional check-ups are consistent.
5. Conclusions
In conclusion, we can state that the lamellar retentions designed for Kennedy class II scenarios have shown high satisfaction in the selected patients. The dialogue between the dentist and dental technician during the design of the prostheses was fundamental for the aspects of retention and aesthetics by not altering the occlusion. In light of the results obtained, we can confirm that even in non-implant-prosthetic cases, the skeletonized partial prosthesis can represent a valid solution for patients, especially if lamellar retentions are designed in the intercalated areas. Across the four parameters observed, an average standard deviation of 0.6225 was found, demonstrating that the data are relatively homogeneous and coherent. The radiographic evaluation of the depth of the roots in teeth with an uncompromised periodontium and an intact crown in the areas of intercalated edentulism allows us to design lamellar retentions. In different cases, such as gingival recessions with bone resorption, this design is not recommended.
It would be desirable for the dentist to always design the RPD project in order to be certain of the adequate positioning of the retentive means and better aesthetics. This study could be continued with a longer follow-up at 2 and 3 years to also evaluate the periodontal appearance and the mobility index of the abutment teeth.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data supporting the reported results of this study are available from sa-verio.ceraulo@unimib.it upon reasonable request.
Conflicts of Interest
The author declares no conflicts of interest.
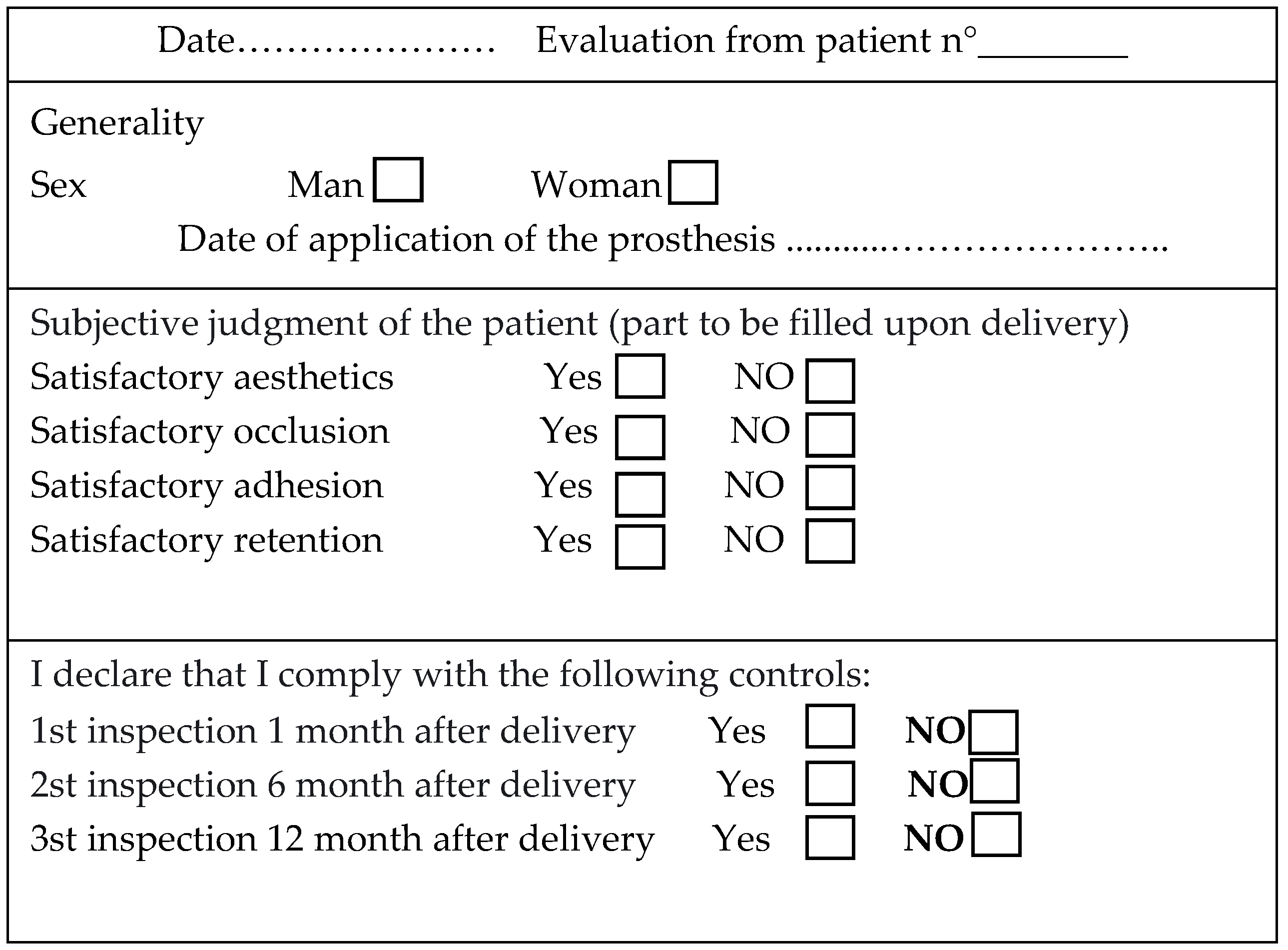
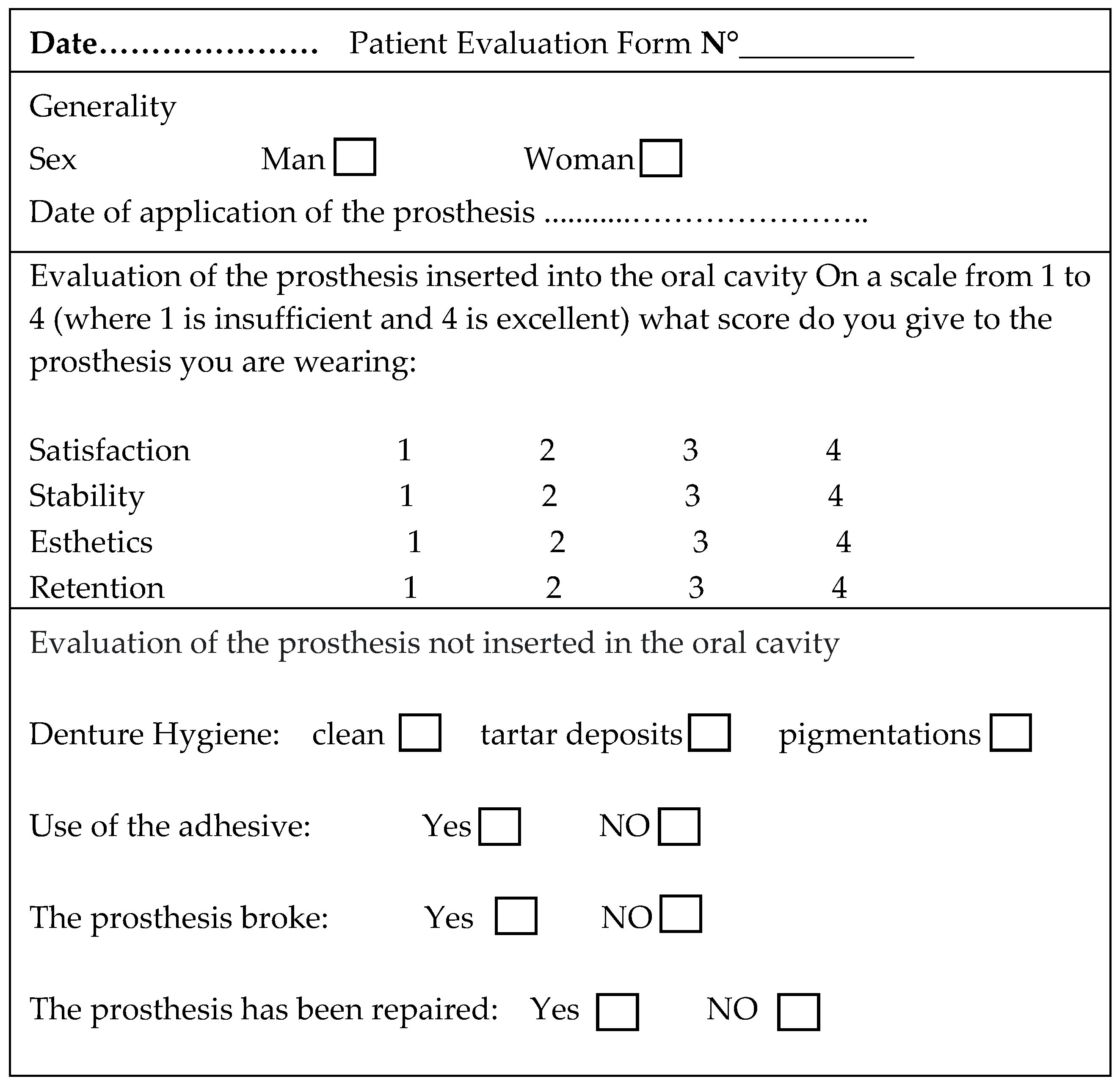
Appendix A
Questionnaire A1 administered to patients upon the delivery of the prosthesis.
Questionnaire A2, A3, and A4 administered to patients 1, 6, and 12 months after the delivery of the prosthesis.
References
- Elfadil, S.; Kahatab, A.; Cronin, E.; O’Mahony, A. Chairside technique for addition of teeth to an acrylic partial denture. A clinical report. Heliyon 2023, 9, e18040. [Google Scholar] [CrossRef]
- Goswami, M.; Chauhan, N. Prosthetic Management with Removable Partial Dentures in Pediatric Dental Care: Case Series. Int. J. Clin. Pediatr. Dent. 2023, 16, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Goguta, L.; Frandes, M.; Candea, A.; Ille, C.; Jivanescu, A. Impact of unilateral removable partial dentures versus removable partial dentures with major connector on oral health-related quality of life of elder patients: A clinical study. BMC Oral Health 2023, 23, 182. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.R.; Xie, R.; Niu, L.N.; Feng, Z.H.; Zhao, Y.M. Novel Digital Mouth Preparation Technique for Fabricating Implant-Retained Removable Partial Dentures with Distal Extension: A Case Report. Chin. J. Dent. Res. 2023, 26, 113–117. [Google Scholar] [CrossRef]
- Jayaraman, S.; Singh, B.P.; Ramanathan, B.; Pazhaniappan Pillai, M.; MacDonald, L.; Kirubakaran, R. Final-impression techniques and materials for making complete and removable partial dentures. Cochrane Database Syst. Rev. 2018, 4, CD012256. [Google Scholar] [CrossRef] [PubMed]
- Kumari, K.S.; Anusha, K.S. An Esthetic Approach for Rehabilitation of Long-Span Edentulous Arch Using Artificial Intelligence. Cureus 2023, 15, e38683. [Google Scholar] [CrossRef]
- Rues, S.; Tasaka, A.; Fleckenstein, I.; Yamashita, S.; Rammelsberg, P.; Boehm, S.; Schwindling, F.S. Fit and Retention of Cobalt-Chromium Removable Partial Denture Frameworks Fabricated with Selective Laser Melting. J. Funct. Biomater. 2023, 14, 416. [Google Scholar] [CrossRef]
- Akinyamoju, C.A.; Ogunrinde, T.J.; Taiwo, J.O.; Dosumu, O.O. Comparison of patient satisfaction with acrylic and flexible partial dentures. Niger. Postgrad. Med. J. 2017, 24, 143–149. [Google Scholar] [CrossRef]
- Campbell, S.D.; Cooper, L.; Craddock, H.; Hyde, T.P.; Nattress, B.; Pavitt, S.H.; Seymour, D.W. Removable partial dentures: The clinical need for innovation. J. Prosthet. Dent. 2017, 118, 273–280. [Google Scholar] [CrossRef]
- Benso, B.; Kovalik, A.C.; Jorge, J.H.; Campanha, N.H. Failures in the rehabilitation treatment with removable partial dentures. Acta Odontol. Scand. 2013, 71, 1351–1355. [Google Scholar] [CrossRef]
- Hatayama, T.; Chiba, A.; Kainose, K.; Nakajima, M.; Hosaka, K.; Wakabayashi, N.; Foxton, R.M.; Tagami, J. Stress distribution in tooth resin core build-ups with different post-end positions in alveolar bone level under two kinds of load directions. Dent. Mater. J. 2018, 37, 474–483. [Google Scholar] [CrossRef]
- Ceraulo, S. Ritenzione a lamella su modifica della placca prossimale. Una nuova progettazione ideata dall’autore della ricerca in riabilitazioni Protesiche parziali rimovibili scheletrate di III classe. Protech 2001, 2, 21–24. [Google Scholar]
- Ceraulo, S. Follow-Up a Due Anni Della PPS Con Ritezioni a Lamelle; Supplemento Doctor OS, Anno XV; Ariesdue (S.R.L.): Milano, Italy, 2004. [Google Scholar]
- Straulino, E.; Scarpazza, C.; Spoto, A.; Betti, S.; Chozas Barrientos, B.; Sartori, L. The Spatiotemporal Dynamics of Facial Movements Reveals the Left Side of a Posed Smile. Biology 2023, 12, 1160. [Google Scholar] [CrossRef]
- Al-Kaisy, N. Measurement of vertical anterior teeth display and lip position at smiling in Kurdish population. Age and gender-based evaluation. Heliyon 2023, 9, e19465. [Google Scholar] [CrossRef]
- Cheng, J.H.; Hsu, Y.C.; Lee, T.Y.; Li, R.W. Factors affecting perception of laypeople and dental professionals toward different smile esthetics. J. Dent. Sci. 2023, 18, 739–746. [Google Scholar] [CrossRef]
- Saffarpour, A.; Ghavam, M.; Saffarpour, A.; Dayani, R.; Fard, M.J. Perception of Laypeopleand Dental Professionals of Smile Esthetics. J. Dent. 2016, 13, 85–91. [Google Scholar]
- Al-Rafee, M.A. The epidemiology of edentulism and the associated factors: A literature Review. J. Fam. Med. Prim. Care 2020, 9, 1841–1843. [Google Scholar] [CrossRef]
- Gabiec, K.; Bagińska, J.; Łaguna, W.; Rodakowska, E.; Kamińska, I.; Stachurska, Z.; Dubatówka, M.; Kondraciuk, M.; Kamiński, K.A. Factors Associated with Tooth Loss in General Population of Bialystok, Poland. Int. J. Environ. Res. Public Health 2022, 19, 2369. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.D.; Badner, V.M. Association between asthma and severe tooth loss in the adult population of the United States. J. Asthma 2022, 59, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, K.; Sakurai, A.; Mizuki, M.; Kurita, H.; Tsukahara, T.; Nomiyama, T. Association between the number of teeth and incident pre-diabetes among middle-aged adults with period ontal disease: A retrospective cohort analysis of Japanese claims data. BMJ Open 2023, 13, e075527. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, N.L.; Hajhamid, B.; Somogyi-Ganss, E. Postinsertion adjustment appointments and their association with cast removable partial denture survival. J. Prosthet. Dent. 2023, 130, e1–e238. [Google Scholar] [CrossRef] [PubMed]
- Cumbo, E.; Messina, P.; Gallina, G.; Scardina, G.A. An Experimental Method to Add New Prosthetic Teeth in the Removable Partial Denture Framework: TIG Cold Welding and Preformed Pins. Prosthesis 2023, 5, 1120–1128. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Taani, D.S.; Naseeb, A.Z.; Al-HajHusain, N.; Özcan, M.; Lynch, E. Evaluation of Clinical Periodontal Parameters of Abutment Teeth Supporting Distal-Extension Base Removable Partial Dentures: A Cross-sectional Study. Eur. J. Prosthodont. Restor. Dent. 2023, 31, 424–431. [Google Scholar] [CrossRef]
- Tregerman, I.; Renne, W.; Kelly, A.; Wilson, D. Evaluation of removable partial denture frameworks fabricated using 3 different techniques. J. Prosthet. Dent. 2019, 122, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Carneiro Pereira, A.L.; Bezerrade Medeiros, A.K.; de Sousa Santos, K.; Oliveirade Almeida, É.; Seabra Barbosa, G.A.; da Fonte Porto Carreiro, A. Accuracy of CAD-CAM systems for removable partial denture framework fabrication: A systematic review. J. Prosthet. Dent. 2021, 125, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Abbasi, M.S.; Haider, S.; Ahmed, N.; Habib, S.R.; Altamash, S.; Zafar, M.S.; Alam, M.K. Fit Accuracy of Removable Partial Denture Frameworks Fabricated with CAD/CAM, Rapid Prototyping, and Conventional Techniques: A Systematic Review. Biomed. Res. Int. 2021, 2021, 3194433. [Google Scholar] [CrossRef] [PubMed]
- Takaichi, A.; Fueki, K.; Murakami, N.; Ueno, T.; Inamochi, Y.; Wada, J.; Arai, Y.; Wakabayashi, N. A systematic review of digital removable partial dentures. Part II: CAD/CAM framework, artificial teeth, and denture base. J. Prosthodont. Res. 2022, 66, 53–67. [Google Scholar] [CrossRef] [PubMed]
- Jafarpour, D.; Feine, J.S.; Morris, M.; Souza, R.F. Patient-reported outcomes and clinical performance of CAD/CAM removable dentures: A scoping review. Int. J. Prosthodont. 2023. [Google Scholar] [CrossRef]
- Ali, I.E.; Tanikawa, C.; Chikai, M.; Ino, S.; Sumita, Y.; Wakabayashi, N. Applications and performance of artificial intelligence models in removable prosthodontics: A literature review. J. Prosthodont. Res. 2023. [Google Scholar] [CrossRef] [PubMed]
- Iannello, G.; Fiorillo, L.; D’Amico, C.; Minervini, G.; Terranova, A.; Cervino, G. Presenting a Protocol for Dental Implant Restorations. Prosthesis 2023, 5, 1153–1170. [Google Scholar] [CrossRef]
- Shen, X.; Zhang, C.; Jia, X.; Li, D.; Liu, T.; Tian, S.; Wei, W.; Sun, Y.; Liao, W. TranSDFNet: Transformer-Based Truncated Signed Distance Fields for the Shape Design of Removable Partial Denture Clasps. IEEE J. Biomed. Health Inform. 2023, 27, 4950–4960. [Google Scholar] [CrossRef] [PubMed]
- Pordeus, M.D.; Gasparetto, G.D.; Machado, L.M.R.; Noritomi, P.Y.; Costa, R.M.B.D.; Chappuis-Chocano, A.P.; Venante, H.S.; Junior, J.F.S.; Porto, V.C. A New Proposal for Calibrated Gauges for Removable Partial Dentures: A Finite Element Analysis. J. Contemp. Dent. Pract. 2022, 23, 1230–1236. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Mao, B.; Dai, Y.; Chen, S.; You, Z.; Zhang, J.; Chen, X.; Dong, H.; Yue, L.; Yu, H. Audit to assess the quality of 916 prosthetic prescriptions of removable partial dentures. Hua Xi Kou Qiang Yi Xue Za Zhi 2023, 41, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Radford, P.J.; Walton, J.; McManus, R. Should dental technicians play a greater role in the education of foundation dentists? Br. Dent. J. 2020, 229, 653–654. [Google Scholar] [CrossRef]
- Juszczyk, A.S.; Clark, R.K.; Radford, D.R. UK dental laboratory technicians’ views on the efficacy and teaching of clinical-laboratory communication. Br. Dent. J. 2009, 206, E21. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).