Abstract
Due to their lack of periodontal ligaments (PLs) and the differences between dental implants and natural teeth, it is necessary to improve and generate a new occlusal scheme to prolong the life of implants and prostheses. The age and the sex of patients must be considered because of their effects on the stomatognathic system’s physiology. Operators must manage all the changes to obtain good sensations during mastication and a better occlusal scheme for implanting fixed partial prostheses. Dentists should try to protect this type of prosthesis using adjacent teeth and the PL. This is why new digital systems were created. The combination of T-Scan® (digital software for occlusal analysis) and electromyography (EMG) could allow doctors to find areas where it is necessary to act and to find suitable solutions for the problems generated by using conventional methods of occlusal analysis (such as articulating paper). In this study, a new method for establishing occlusion on fixed partial implant prostheses has been created, combining digital systems with conventional articulating paper. This method consists of asking the patient to bite down with different forces and situations in an attempt to achieve Implant-Protected Occlusion (IPO). The use of digital systems has been shown to be more effective than using only conventional systems. This new method allows a safer mode of occlusion which protects implants and prostheses, saving all the differences between them and natural teeth, and increasing the satisfaction of patients. This method also helps to overcome the changes in the stomatognathic system as age increases, adjusting the occlusion to changes in PLs with age.
1. Introduction
Currently, implantological treatments are used in cases requiring dental restorations, leading to an improvement in masticatory function and occlusion [1]. However, their use is not exempt from disadvantages and issues that need to be evaluated and addressed to avoid potential treatment failures [2].
Until now, when rehabilitating with partially implant-supported prostheses, the same occlusal scheme used in natural dentition was often adopted, disregarding that they possess certain characteristics that make them susceptible to long-term problems if specific measures are not taken [3].
To study these biological and biomechanical differences, it is essential to understand the divergences between a natural tooth and an implant with regard to the occlusal forces to which they will be subjected. The main difference lies in the presence of a periodontal ligament (PL) that surrounds the root surface of natural teeth, connecting them to the adjacent teeth. Its thickness is approximately 0.2 mm [4]. This area is rich in innervation and contains many mechanoreceptors that capture information to be transmitted to higher enters, thus regulating the muscular activity responsible for mastication. In contrast, a dental implant is encompassed and integrated into the bone (osseointegration) without the presence of PLs [5].
According to Lim, PLs are influenced by the patient’s age, so that with increasing age, the PL space decreases, experiencing a reduction in width due to continuous mineralization of the root cement occupying the PL space [6]. Additionally, the mechanoreceptors it possesses undergo aging and dysfunction [7].
Maintaining proper occlusal alignment is essential for the health of the stomatognathic system [8]. Both natural teeth and placed prostheses must possess a physiological and harmonious occlusion for the stomatognathic system to function correctly, thereby avoiding undesired effects [9].
Due to the anatomical and physiological differences between teeth and implants, it becomes necessary to design a specific occlusal system for partially implant-supported prostheses, providing them with defense mechanisms against potential occlusal abnormalities that may arise [10].
Thus, the concept of Implant-Protective Occlusion (IPO) emerges, which allows Maximum Intercuspation (MI) to be achieved when the natural teeth come into contact while reducing the occlusal load on the implant and prosthetic structures, protecting them [10]. In static occlusion, the objective is to achieve CR (centric relation) along with MI (centric occlusion), with a long centric of approximately 1 to 1.5 mm, which allows for the elimination of interferences [11,12].
The movement of a natural tooth under occlusal load is not linear. It starts with a phase in which the movement occurs due to the compression of the PL, resulting in the lowering of the tooth’s occlusal level. If the load on the tooth continues, it enters the second phase of movement, produced by the elastic deformation of the alveolar bone. The implant only experiences the second phase of movement [9,10,11,12,13]. This necessitates the development of new occlusal schemes that can accommodate the described discrepancy in movements [10].
When the patient performs MI without a conscious effort to clench (without exerting force, only contacting the teeth), there should be contact on the natural teeth but not on the implant-supported prostheses.
Conversely, when the patient performs MI with a conscious biting effort (clenching with force), there should be strong contact on the natural teeth and light contact on the implant-supported pieces. When the patient performs MI without clenching, the PLs of the natural teeth are not compressed, while during forceful MI, the PLs of the natural teeth compress, and at that point, the prosthesis comes into play. If there is contact in the prosthesis without clenching, when a strong clench occurs and the PL contracts, there will be occlusal overload on the prosthesis [10,11,12,13,14]. Michalakis found that, under the same force, a natural tooth intrudes approximately 50 μm while an implant intrudes around 2 μm. If, during light contact, there is the same occlusal force on natural teeth and implant-supported crowns, when there is a conscious biting effort, an occlusal overload will occur on the implant-supported prosthesis [4,5,6,7,8,9,10,11].
The most common way to analyze occlusal contacts is using articulating paper. Subjectively, intense and extensive occlusal marks are usually associated with premature and high-intensity contact, while contact with small surface area and lower intensity is often associated with correct occlusal contact. The presence of numerous contacts with equal intensity and surface area is associated with a balanced occlusion. However, certain studies using digital occlusal analysis devices demonstrate that such correlations are often inaccurate [15,16].
Nowadays, more and more dentists rely on digital methods of occlusal analysis as they are more reliable and provide an added value of objectivity and precision. Articulating paper, in this case, is used solely to locate regions where contact occurs without considering their size or intensity. By combining different computerized systems, the functionality of the masticatory system and prosthetic components can be improved [17].
In 1987, the T-Scan occlusal analysis system was created by Tekscan (Tekscan Inc., South Boston, MA, USA). When the patient bites, an electric current is generated and collected by the software. It is capable of recording the first contact with the MI and faithfully reproducing it to analyze the contact sequence. It evaluates it in intervals of 0.003 s, registering the relative forces of each contact, contact sequence over time, and representing the force of contacts in color-coded bar graphs [18,19].
However, digital occlusal analysis systems still have their limitations. They lack the ability to measure the absolute force of each contact. The sensor has a thickness of 0.1 mm, which, after MI, will compress to 0.06 mm, which is still insufficient and may potentially lead to the appearance of certain interferences during analysis, as well as the possibility of distorting some data. Moreover, they require a relatively steep learning curve and more time in the dental consultation with each patient (pre-practice for occlusal study), making them more time-consuming than conventional methods, and necessitating patients to learn specific movements [14,15].
New research is directed towards the combined use of digital occlusal analysis systems with electromyography (EMG). This symbiosis can reveal dysfunctions of occlusion and the stomatognathic system, allowing control over various parameters such as the center of force, generated balance, time of disocclusion, mandibular position, and occlusal stability [15,16,17,18,19,20].
EMG is another digital system that can be used to monitor occlusal balance in oral rehabilitations. Muscle activity in the temporal and masseter muscles increases when high-intensity contacts are present, supporting the combined use of T-Scan with EMG [21].
The objective of this study is to observe the differences between natural teeth and implants due to the presence of the PL and to assess how patient age affects the PL and patient satisfaction with chewing, in patients with partially implant-supported prostheses. A comparison will be made between the group treated with conventional methods and the group treated with new technologies, following the implementation of Implant Protective Occlusion (IPO).
2. Materials and Methods
The study was conducted in an office equipped with all the technology, instruments, and apparatus necessary for this purpose. The instruments used included an examination kit, coarse-grain button turbine burrs of the Komet® (Lemgo, Germany) brand, ceramic polishing burrs of the Komet® brand, 40 μm articulating paper in blue and red by Bausch®, and Miller forceps. In addition to the mentioned instruments, the T-Scan III occlusal analysis software (TekScan®, South Boston, MA, USA) and the MyoMuscle electromyography software by Noraxon® (Scottsdale, AZ, USA) were used.
The T-Scan III software consists of a handheld device connected to a computer, containing a U-shaped digital sensor that is pressure-sensitive. This sensor, with a thickness of 0.06 mm, is composed of 1500 sensory receptors, which are inserted into the oral cavity.
A total of 120 patients were included in the study. In this study, we chose patients with fixed partial implant prostheses. These prostheses were metal–ceramic. The extension of the prostheses was between 1 crown and a bridge of 3 crowns.
2.1. Methodology of the Project
A randomized double-blind clinical trial was conducted, involving 120 patients who met the inclusion and exclusion criteria.
Inclusion criteria were as follows:
- Patients with partially implant-supported prostheses.
- Patients with Angle Class I occlusion.
- Patients without dental absences, excluding third molars.
- Adult patients.
Exclusion criteria were as follows:
- Patients over 80 years of age.
- Patients with disabilities that hindered proper understanding and execution of the study.
- Patients with temporomandibular joint pathologies.
- Patients without occlusal stability, preventing reliable and repetitive attainment of MI.
- Patients unwilling to participate or desiring to withdraw from the study.
The included patients were educated about the procedure they would undergo and the advantages and potential inconveniences of participating in the project, and they provided informed consent. Upon signing the informed consent form, each patient was randomly assigned to one of the two groups:
- Group 1: 60 patients with partially implant-supported prostheses, where occlusal adjustment and the necessary procedures to establish IPO were performed using conventional methods with articulating paper, along with simultaneous EMG.
- Group 2: 60 patients with partially implant-supported prostheses, where IPO was established using T-Scan III software, along with simultaneous EMG.
2.1.1. Common Methodology for Both Groups
Once the patient was seated in the dental office, their personal data and dental and medical history were collected.
A pre-study survey was conducted, inquiring about the patient’s overall satisfaction with their current prosthesis (their sensation while biting, and any discomfort or issues encountered during MI).
After completing the survey, the electromyographic activity was measured prior to the occlusal analysis. This provides a general overview of the muscular activity before intervening in the stomatognathic system, serving as a baseline for comparison after the implementation of IPO.
The EMG software requires inputting the patient’s age, gender, and weight to calibrate sensitivity. Once the patient was registered, the skin surface corresponding to the masseter region was cleaned with an alcohol solution to remove skin oil and substances like makeup or cream. After cleaning the surface, the patient was asked to clench in MI to palpate the contraction of the masseter muscles and determine the ideal placement of the electrodes. Typically, the electrodes were placed at the mandibular angle, below the zygomatic arch, oriented vertically along the fibers of the masseter muscle. Once the electrodes were positioned (one in each masseter muscle), the information transmitters were connected, sending data to the computer via Bluetooth.
Before recording the electromyographic activity, the patient was instructed on the movements they should perform during the recording. They were trained to perform a clench without a conscious biting effort (contacting the teeth without exerting force) and to perform a clench with the maximum force possible. Once the patient was familiar with the instructed movements, the MI was measured: first without a conscious biting effort and then with maximum force during MI.
To proceed with the T-Scan measurements, the patient’s personal data and dental chart were recorded first. Once completed, the size of the T-Scan III sensor was chosen (according to the patient’s oral cavity size), and the mesio-distal width of the upper right central incisor was measured. This automatically calculated the width of all teeth in both arches to achieve maximum measurement precision. Subsequently, before the measurements, the patient was instructed on the movements they should perform to avoid confusion during the process, ensuring that the movements were performed in MI and with the appropriate force in each situation. Next, the patient was asked to bite without exerting force during MI and to bite with force during MI. In each phase, the action was repeated a minimum of two times to check if it had been performed correctly and to ensure that no different closure acts occurred other than MI. In all patients from both groups and before beginning the measurements and occlusal adjustment, the T-Scan III was calibrated to each patient’s force.
After completing all the EMG and T-Scan measurements, the establishment of IPO was initiated, which was carried out differently depending on the patient’s group. IPO aims to eliminate premature contact points and interferences first, and then prevent implanted-supported prostheses from experiencing contact during a clench without a conscious biting effort, while achieving similar contact to adjacent natural teeth when clenching with force. This step was performed differently depending on the group, with Group 1 using only conventional methods and Group 2 combining conventional and digital methods.
2.1.2. Specific Methodology of Group 1
In Group 1, after performing EMG to monitor the muscular activity of the stomatognathic system, the patients were instructed to bite in MI without consciously exerting force, using only blue articulating paper. In this first phase, premature contacts were eliminated, and the implant-supported prostheses were released from occlusion. Once this first phase was completed, the goal was to achieve light contacts in the prostheses when the patient was asked to clench with force, adjusting the occlusion to achieve stronger contacts in natural teeth and gentle but consistent contacts in the prostheses. Finally, with the red articulating paper, lateral and protrusive movements were performed by the patient to eliminate unwanted contacts and interferences.
After completing the adjustment process, all retouched surfaces were polished with ceramic polishing stones, and the occlusion was checked again using T-Scan III measurements. Lastly, the electromyographic activity was measured again to conclude the study.
2.1.3. Specific Methodology of Group 2
In Group 2, after the initial EMG was performed, all movements described earlier were recorded using T-Scan. Once the T-Scan results were analyzed, and the areas for occlusal adjustment were determined, blue articulating paper was used solely to identify the exact location of the dental contact that needed to be eliminated. In this case, the articulating paper was not used to analyze the patient’s occlusion but only to pinpoint the specific contact identified by T-Scan for removal or smoothing. The occlusal adjustment was performed, and we periodically checked our work with the articulating paper and T-Scan to ensure that the targeted contacts were being appropriately modified. Like the previous group, the goal was to ensure that the prostheses had no contact during MI without consciously exerting force, while in strong clenching MI, there should be balanced contact on all teeth, with the prostheses having slightly lighter contact. After completing the occlusal adjustment for both strong clenching MI and without conscious clenching, red articulating paper was used to eliminate interferences, and the patient was asked to perform lateral and protrusive movements for this purpose. Once the occlusal adjustment was finished, all surfaces were polished using ceramic polishing stones. Subsequently, T-Scan III measurements were performed again to observe the results of the prior work, and the muscular activity of the masseter muscles was re-measured using EMG.
In Group 2, if someone wanted to eliminate the articulating paper, they could use an intraoral scanner. By combining an STL of the dental arch and the information provided by T-Scan, dentists can determine the exact location of occlusal contacts without the necessity of articulating paper. The use of articulating paper is only necessary to identify the positions of occlusal points that T-Scan shows required adjustment.
Table 1 provides an overview of the differences in methodology between Group 1 and Group 2. In both groups, after the final EMG was performed, patients were asked about their perception of chewing during MI. Additionally, they were requested to describe their comfort level compared to their state before the study.

Table 1.
Summary table of methodology in each group.
2.2. Variables
During the clinical trial, the following variables were analyzed:
- Age. Patients were divided intro subgroups based on age intervals: 20 to 49; 50 to 59; 60 to 69; and 70 to 79 years. The aim was to observe if other variables and IPO differed with age.
- Sex. This study aimed to determine if sex influenced other variables and the body’s response to the implementation of IPO.
- Pre-IPO prosthesis contact. The presence of contact between the implant-supported prosthesis and the opposing tooth when the patient was asked to bite without applying conscious force (without exerting force) before the occlusal adjustment for IPO. This variable aimed to determine if the patient had an existing IPO and if this situation could be improved after implementing IPO.
- Post-IPO prosthesis contact. The presence of contact between the prosthesis and the opposing tooth when the patient was asked to perform an MI position without conscious force after the IPO was installed. These data were extracted from T-Scan analysis. This variable aimed to assess the effectiveness of the methodology implemented in establishing IPO and to compare conventional methods with digital systems.
- Time to first contact. The time in seconds (s) it took for the prosthesis to make its first contact with the opposing tooth when the patient performed a forceful MI. These data were extracted from T-Scan analysis and helped to verify theories about the PL space around the teeth, serving as evidence to assess the correct implementation of IPO.
- Post-IPO patient sensation. The patient’s perception of comfort and conformity after the completion of the study, compared to their previous state. This variable aimed to involve the patient and gather their opinion on comfort after the implementation of IPO.
- Electromyographic data. Measured in microvolts (μv), these data represent the muscular activity of the masseter muscles. Values were extracted before and after the implementation of IPO for comparison. These data are useful to assess the reactivity of the stomatognathic system to changes in the dental arch. The goal was to achieve an occlusal balance that also allowed for a balance in muscular electrical activity.
2.3. Statistical Analysis
Quantitative data in this study were represented as X ± SEM (mean ± standard error of the mean). To identify and remove outliers, the Tukey test was applied. The statistical inference for quantitative results (numerical values from independent random samples obtained from the studied populations) was performed using the following methods:
- One-way analysis of variance (ANOVA) with the following statistical tests, depending on the type of distribution and variances:
- a.
- For normally distributed variables with equal variances, the Scheffe test and Tukey–Kramer test were used.
- b.
- For normally distributed variables with unequal variances, stabilizing transformations were applied, followed by the Scheffe test.
- c.
- For variables with any other distribution, either equal or unequal variances, non-parametric methods were used: Kruskal–Wallis Z-value multiple comparison (Dunn’s Test) with Regular Test or Bonferroni Test.
- Two-sample T-test, in which, depending on the type of distribution and variances, the following tests were applied:
- d.
- For normally distributed variables with equal variances, Student’s T-test was used.
- e.
- For normally distributed variables with unequal variances, the Aspin–Welch test was applied.
- f.
- For variables with any other distribution, either equal or unequal variances, the Kolmogorov–Smirnov test was used.
- g.
- For differences between medians, the Mann–Whitney U or Wilcoxon Rank-Sum test was applied.
- Correlation of matrices was determined using the following tests:
- h.
- Pearson correlation
- i.
- Spearman correlation
Qualitative data in this study have been represented as frequency tables. The statistical inference for qualitative results was performed using the Chi-square test and Fisher’s exact test. A significance level of p < 0.05 was accepted for all the above-mentioned studies. The statistical software used for the study was NCSS 2007 and Gess 2006—Version: 07.1.21—Released 1 June 2011 (Dr. Jerry L. Hintze, Utah USA).
3. Results
3.1. Descriptive Statistics
A total of 120 patients were enrolled in the clinical trial, who were divided into two groups of 60 individuals each, randomly. The mean age of Group 1 was 61.18 years with a standard error of 1.29. Regarding the mean age of Group 2, it was lower than Group 1, at 56.53 years with a standard error of 1.54.
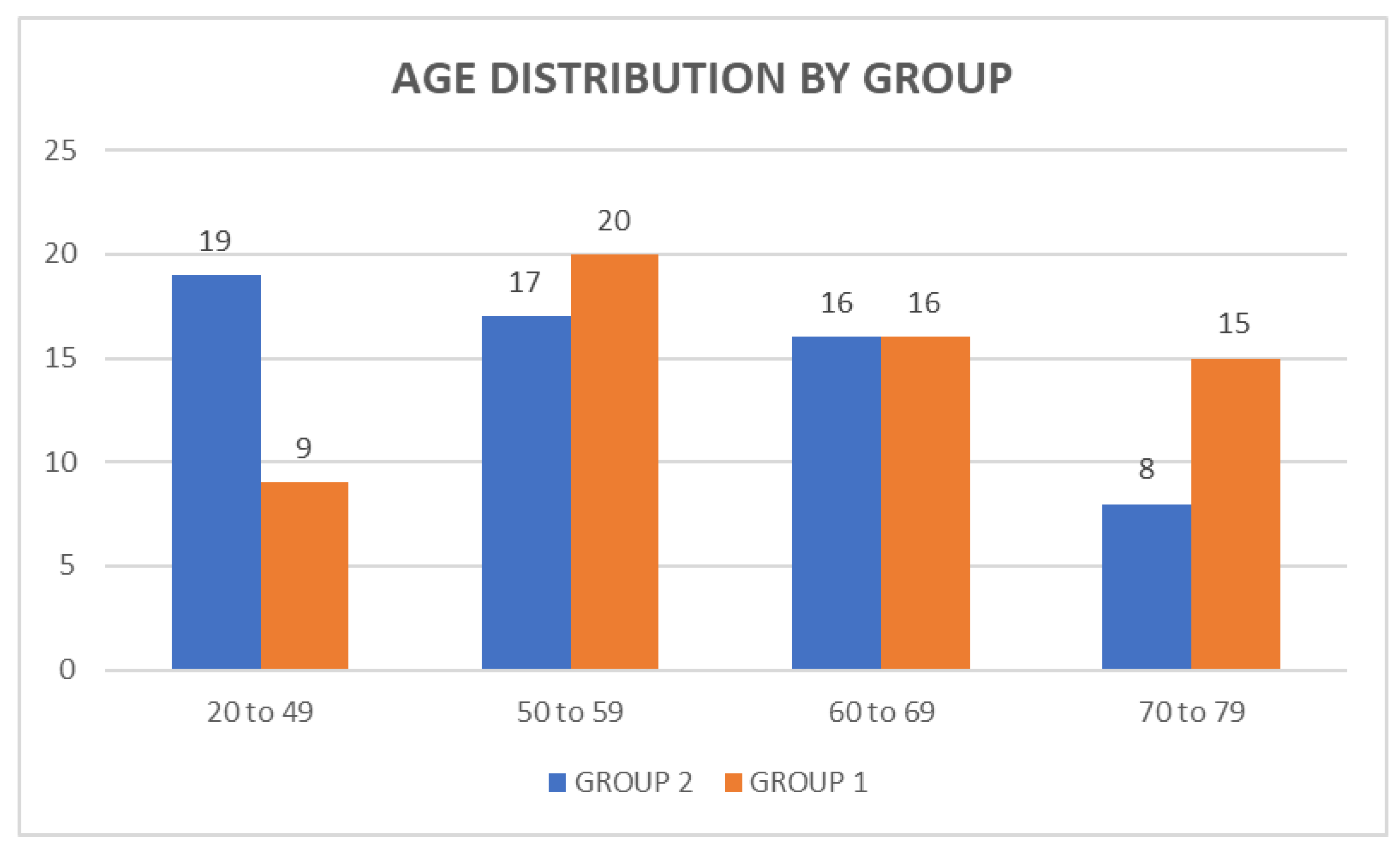
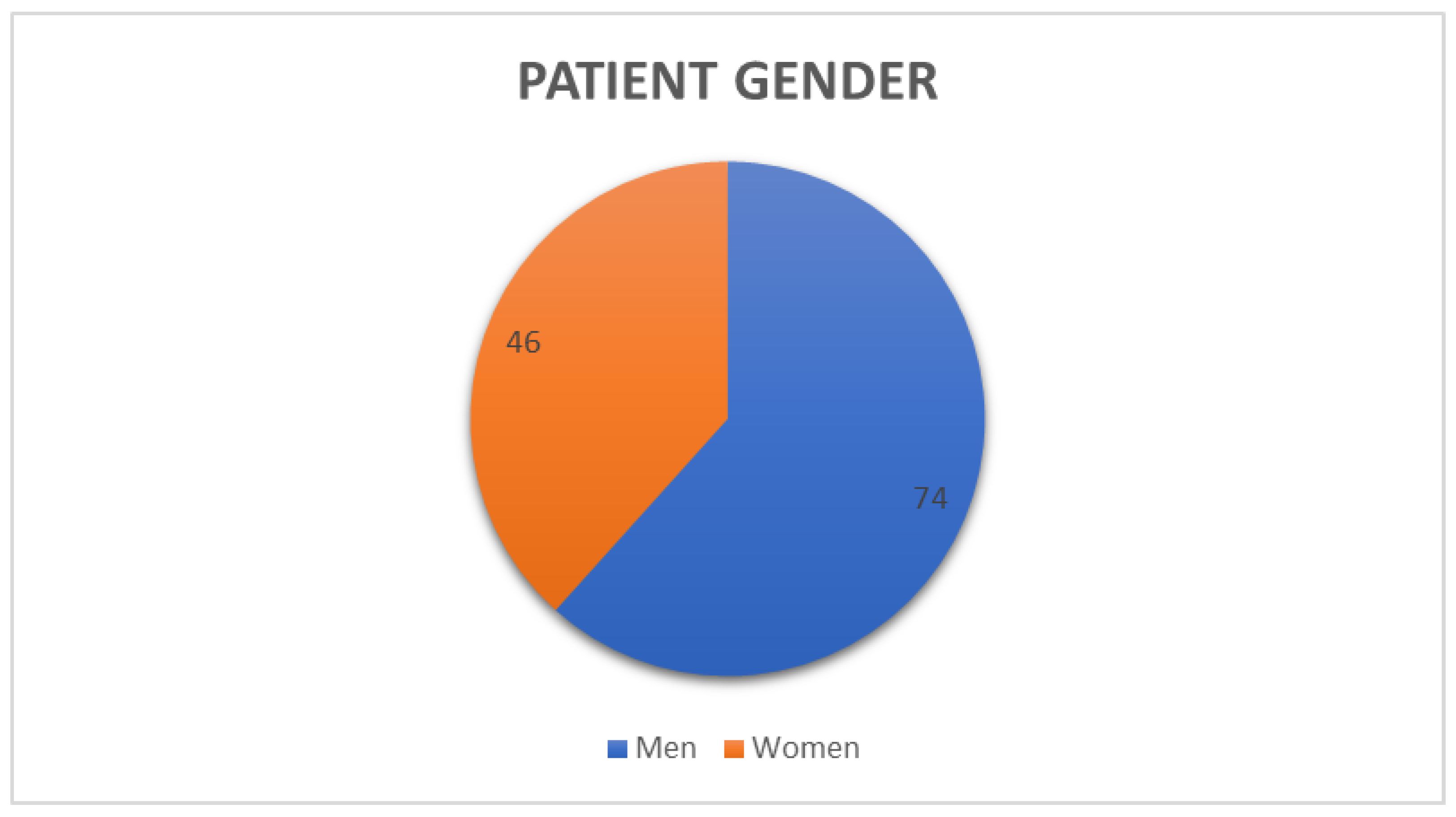
Based on the patients’ ages, four intervals were created and distributed as follows: 20 to 49 years; 50 to 59 years; 60 to 69 years; and 70 to 79 years (Figure 1). Considering the gender distribution of the patients, as shown in Figure 2, a higher number of males participated compared to females, although no significant differences were observed.
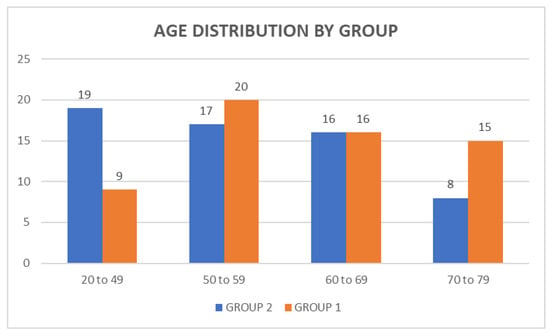
Figure 1.
Distribution of patients by age.
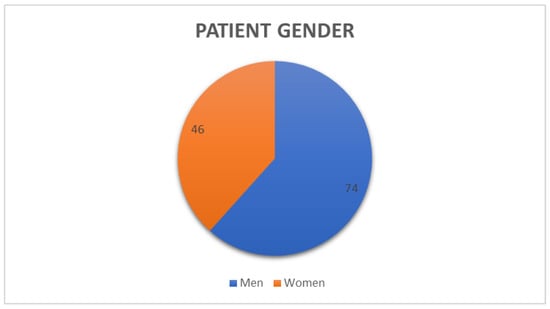
Figure 2.
Gender of the participants in the clinical trial.
3.2. Analysis of Data by Groups
3.2.1. Group 1
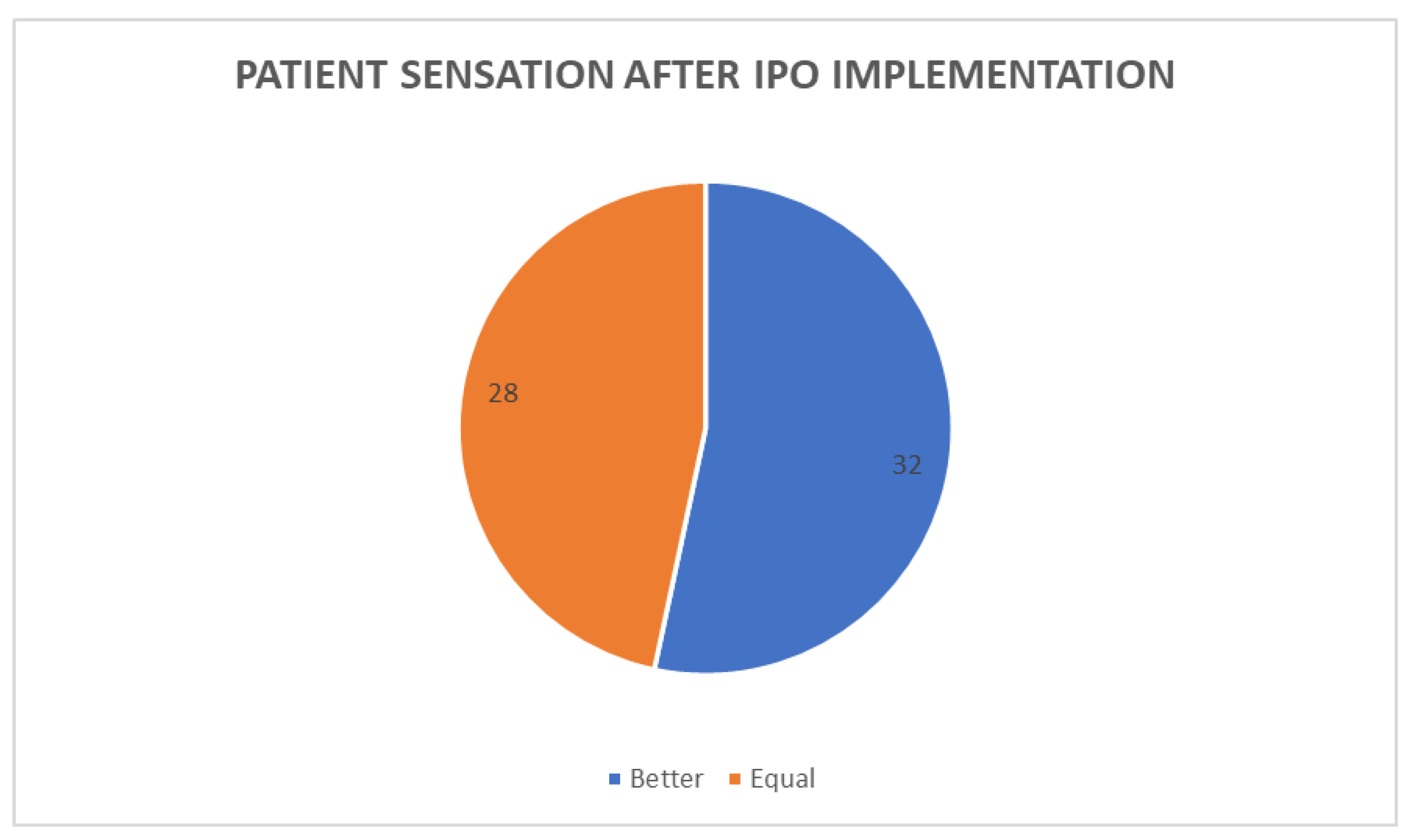
Once the IPO was performed, and after asking the patients to compare their perceived sensation at this moment with how they felt at the beginning of the project, it was revealed that 32 patients had an improved perceived sensation, while 28 subjects did not perceive any change compared to their previous sensation (Figure 3).
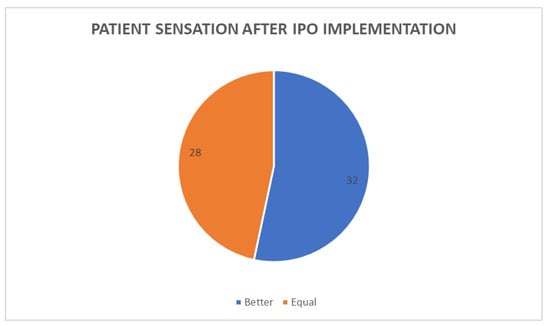
Figure 3.
Distribution of patient sensation after IPO implementation.
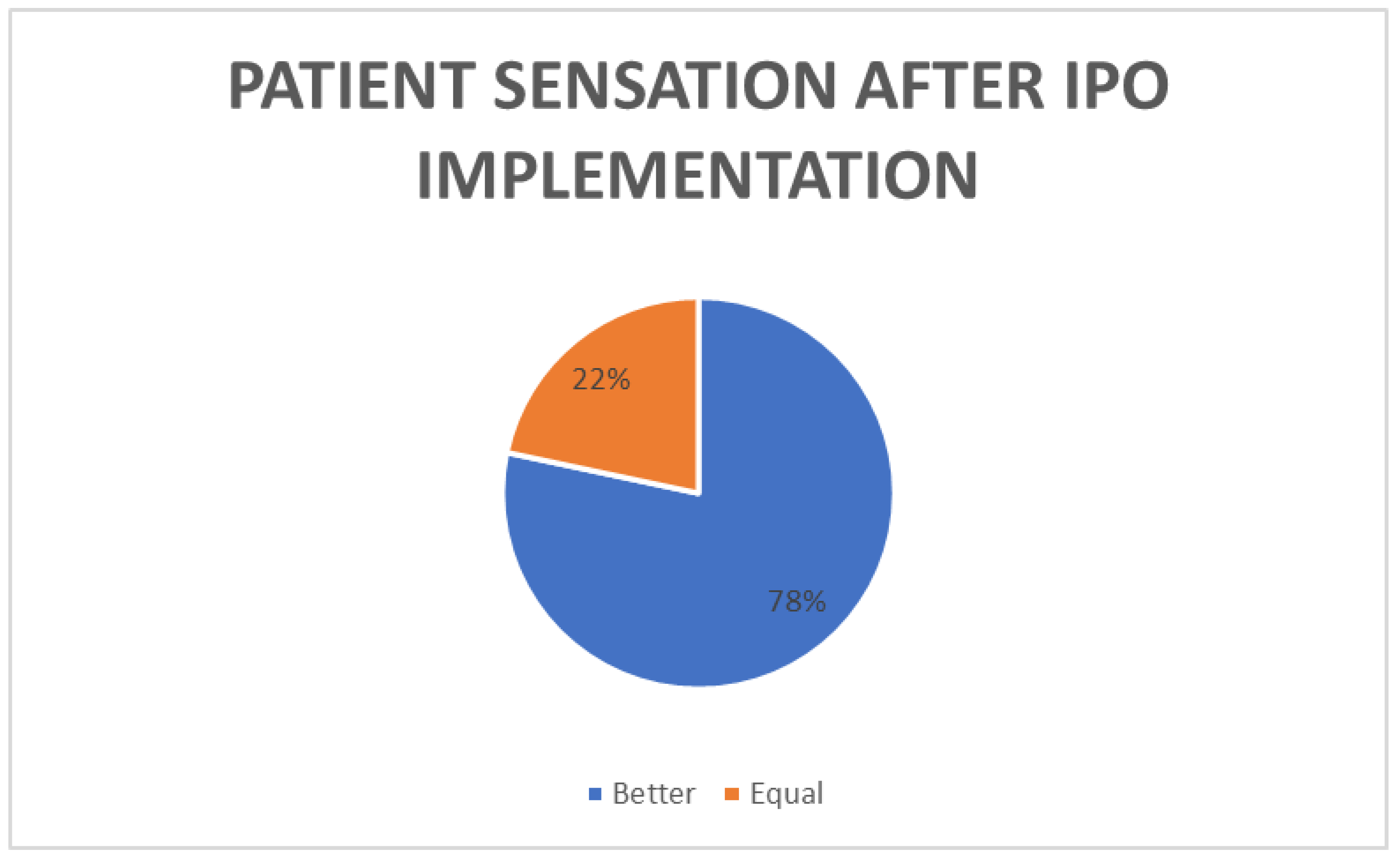
3.2.2. Group 2
After the completion of the project and following inquiries about their subjective sensation compared to their previous state, 60% of the patients (47) reported feeling an improvement in their biting sensation, while 13 individuals stated that they had the same sensation as before their participation in the clinical trial (Figure 4).
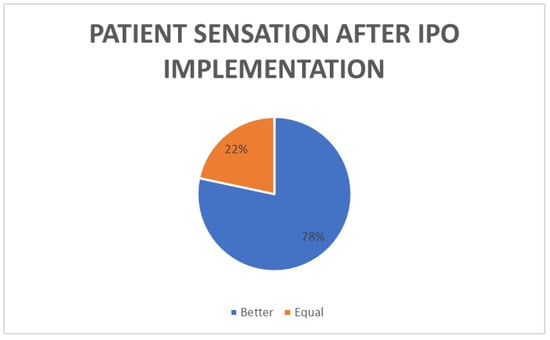
Figure 4.
Percentage of patients with improvement in sensation after IPO implementation.
3.3. Analysis of Data between Groups 1 and 2
Regarding the subjective sensation of patients after IPO implementation, a significant relationship in favor of Group 2 compared to Group 1 was observed (there were more patients with an improved sensation than before IPO implementation) (Table 2). In this comparison, the p-value is 0.004.

Table 2.
Patient sensations after IPO implementation.
In terms of contacts in prosthesis, there was a significant difference between pre and post-IPO contact in the groups. Group 2 showed more improvement between pre-IPO and post-IPO contact than Group 1. The p-value was 0.0025.
The comparison of the time taken for prosthetic contact between the two groups did not show significant results. In both cases, the mean time was similar (Table 3).

Table 3.
Comparison of the time taken for the prosthesis to make its first contact after IPO.
3.4. Analysis of Data via Age Intervals
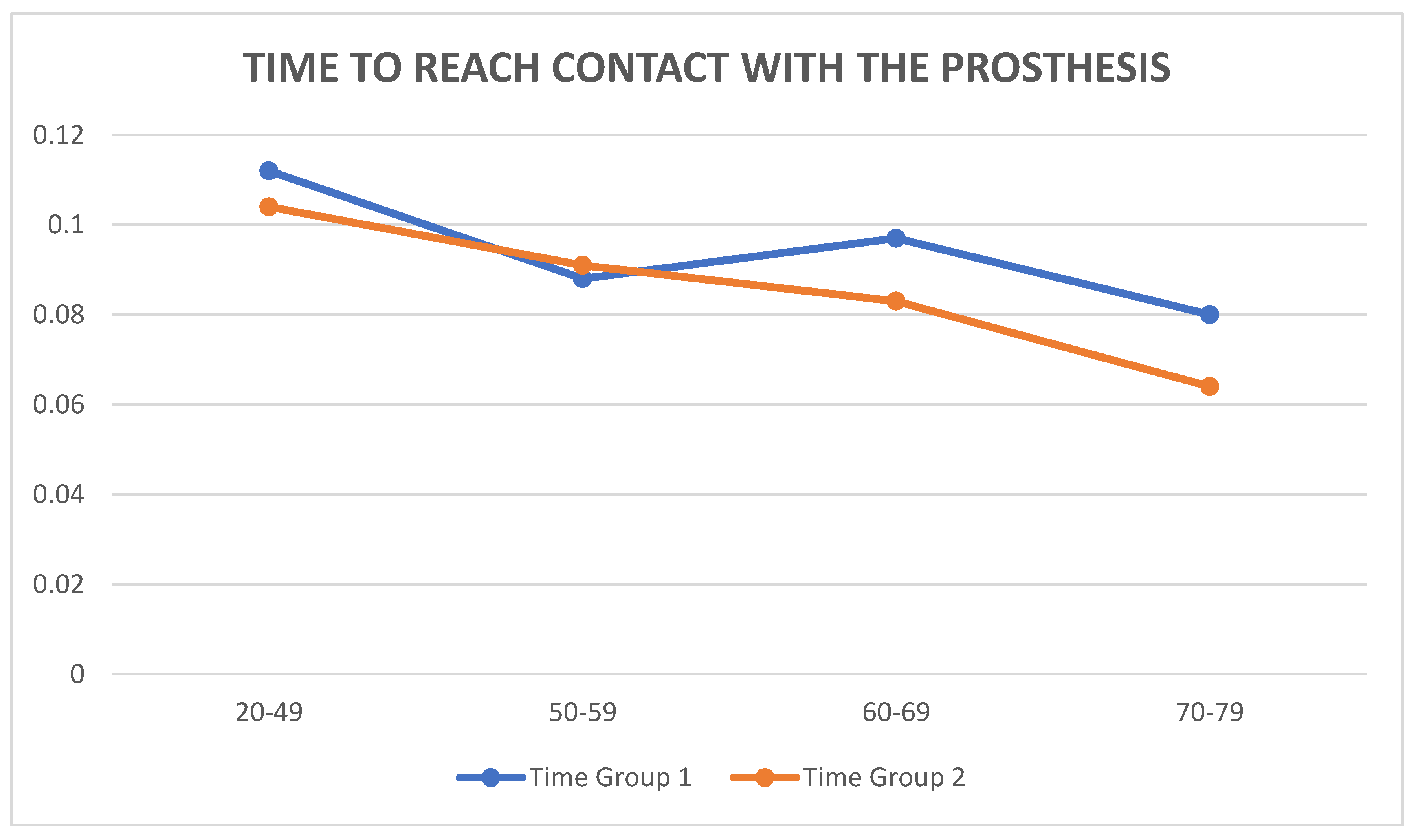
It is important to understand the differences in the time required to achieve contact with the prosthesis depending on the age group (Figure 5).
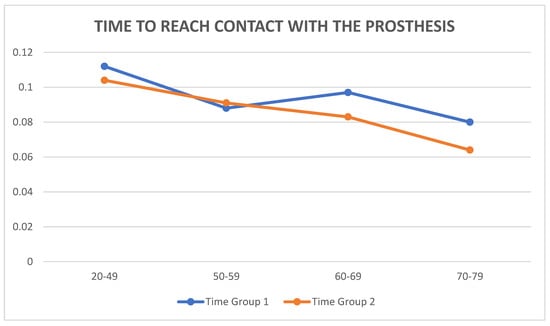
Figure 5.
Time to reach contact with the prosthesis with respect to age.
It is also to know the differences between different age groups regarding overall patient satisfaction after the implementation of IPO. As shown in Table 4, younger patients tended to experience a higher level of satisfaction, having a better subjective sensation compared to the time before IPO was performed. Patients in older age groups had a percentage of “better” responses similar to those patients who described their sensation as “same” as before the study.

Table 4.
Patient perception post-IPO in different age groups.
4. Discussion
This clinical trial aimed to establish an appropriate working methodology for implementing IPO by combining digital systems with conventional methods.
The allocation of patients to the groups was performed randomly, prior to the collection of clinical history and measurements, which added an element of objectivity and scientific rigor to the study. The statistical analysis was conducted without knowing which of the two groups was examined using digital methods, thus eliminating the subjective element that could influence the results. The same variables were extracted and studied in both groups for the purpose of comparison.
The obtained results lead us to believe that digital systems offer an advantage for dentists. The objectives of this study were achieved using an established methodology that can be followed by other dentists, demonstrating that conventional methods should be complemented by digital systems. The subjective assessment by the patients improved before and after the implementation of IPO, suggesting the utility of IPO for patients with implant-supported partial dentures. Additionally, it has been demonstrated that this improvement in patients’ subjective sensation was more pronounced in the group of patients who used digital systems, highlighting the effectiveness of these systems.
Moreover, there is a necessity to increase the number of patients in order to obtain a larger amount of data. This could increase the significance of our statistical analysis and could increase the benefits of our methodology, which is important due to the number of people who use fixed partial implant prostheses. One of our options to increase the number of patients is to perform a multicentric clinical trial. Teaching other dentists and making this occlusal analysis available to more patients would increase the data and would help many more people.
There are various studies advocating against the need for specific occlusal schemes for implant-supported partial dentures, relying on the neuroplasticity of the stomatognathic system to adapt mastication to the new occlusal structures [22]. However, most studies on the subject agree on the necessity of paying greater attention to these situations, emphasizing the need for a specific occlusal system. This is due to the differences in the peri-implant structure, which differs from the periodontal ligaments of natural teeth [23].
The need to differentiate between light contacts and contacts under force becomes evident due to the presence of PLs in natural teeth. This is why this study suggested a differentiation between maximum clenching and light contact during MI. This approach aims to cover and study the peculiarities observed in the introduction, as well as the differences between teeth and implants explained in the first section of this work. Excursive movements, which produce non-axial force vectors, must be eliminated for the same reasons.
Compared to natural teeth, implant-supported prostheses should bear a lower percentage of load, as they lack the periodontal ligament’s ability to withstand generated overloads. By enabling contact in the prosthesis only during forceful clenching in MI, a lower percentage of load is transmitted to the implant-supported tooth compared to the adjacent teeth. Greater load is received by natural teeth with PLs, allowing for a perfect balance across the dental arch [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24].
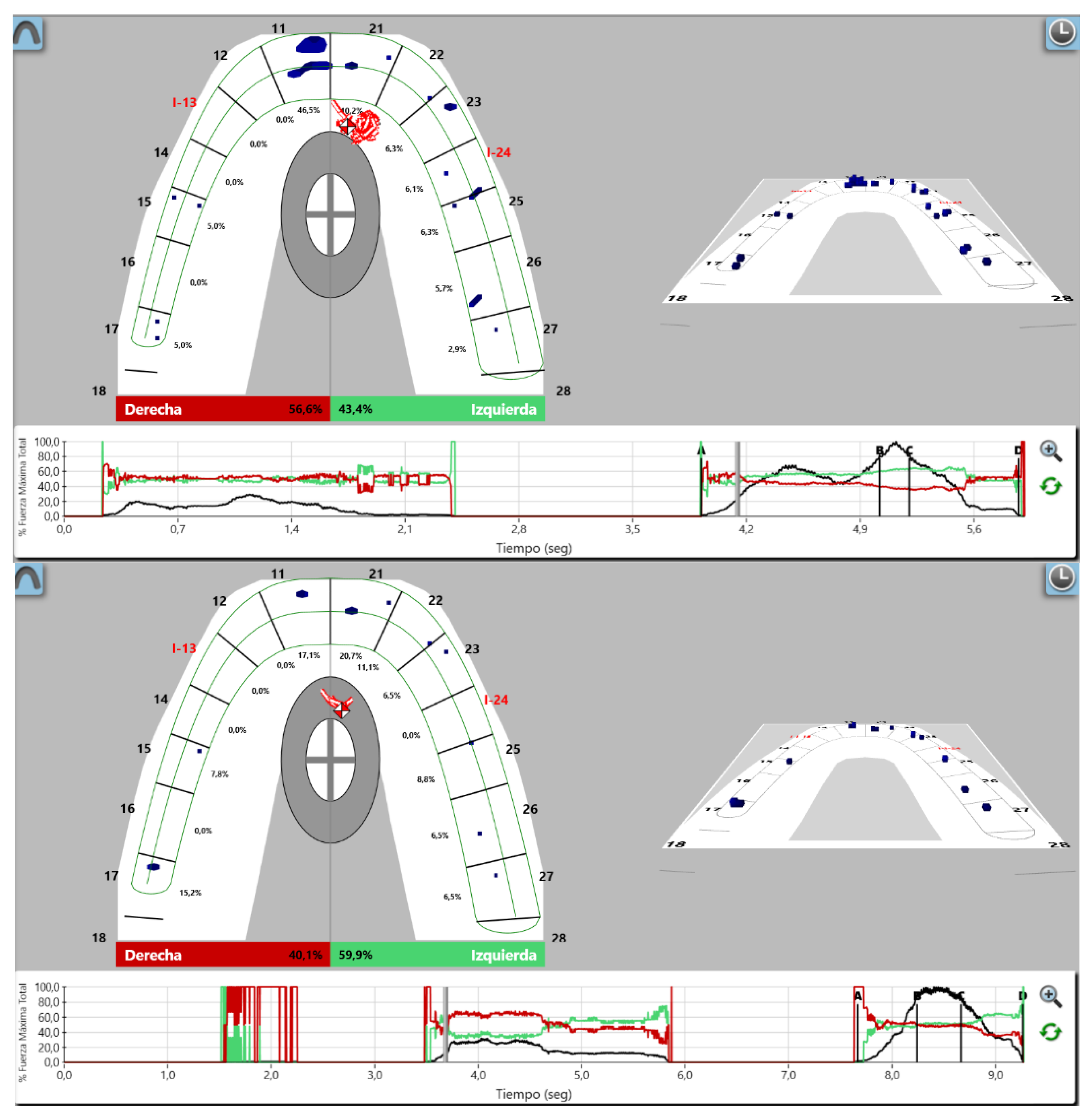
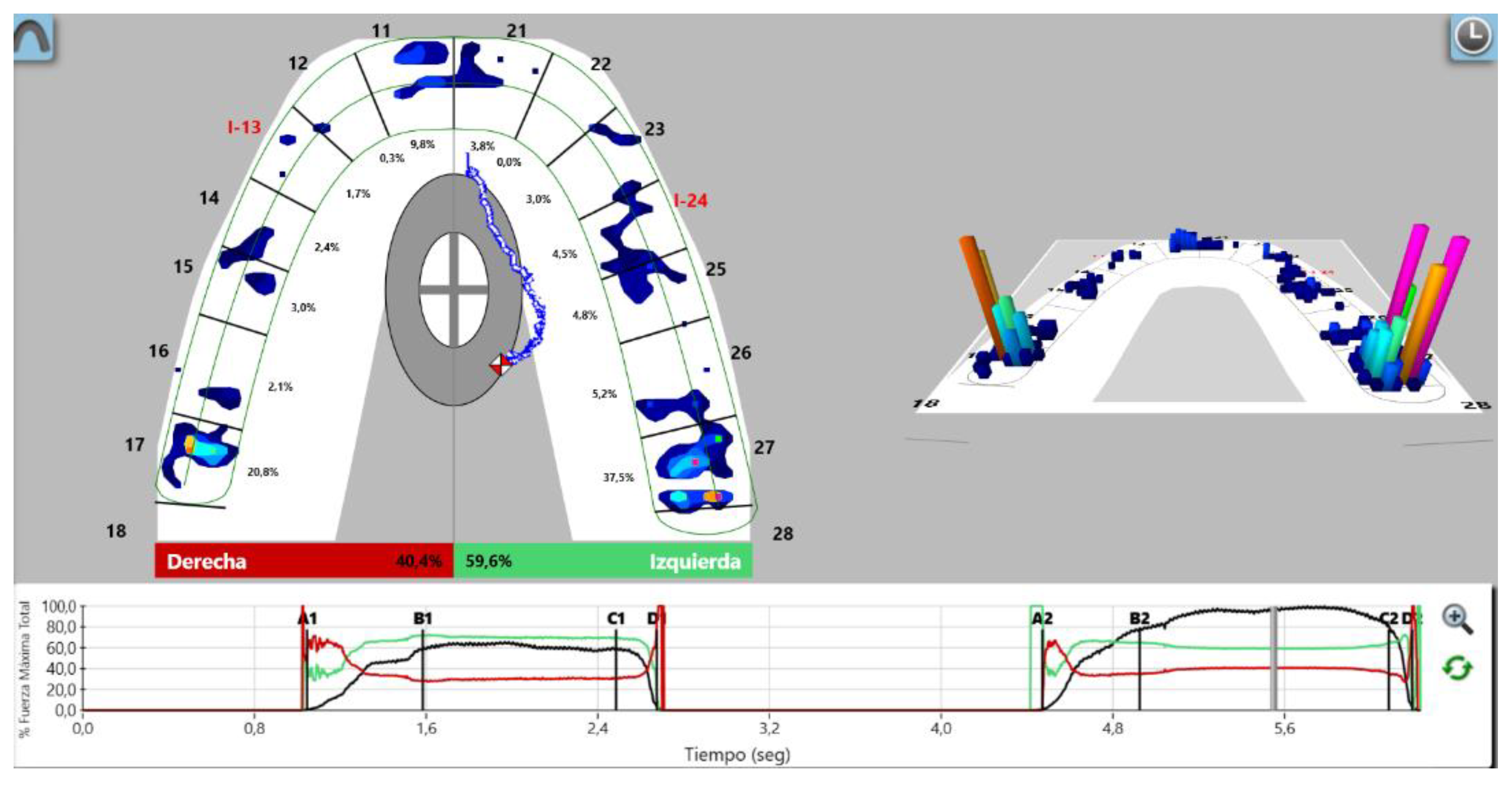
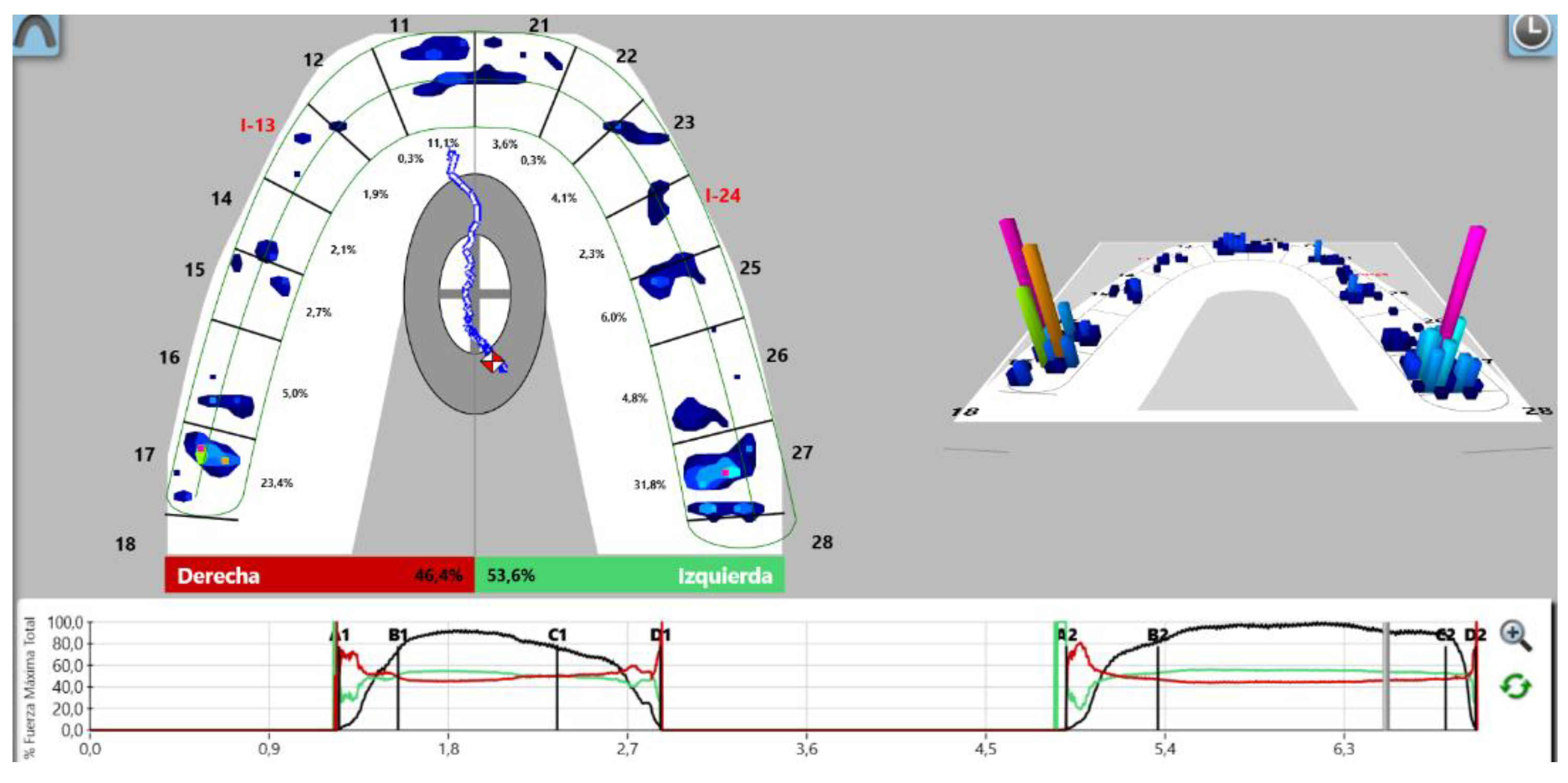
In our study, it can be observed that Group 2, in which occlusal adjustment and IPO implementation were performed using digital methods, achieved better outcomes compared to Group 1. Zhou also emphasizes the neuroplasticity present in the bony surface when an implant-supported prosthesis is perfectly adapted and has a well-established IPO. This feedback mechanism contributes to the optimal functioning of the stomatognathic system. This has a positive impact on overall patient satisfaction, as a well-executed IPO results in an ideal occlusal balance, promoting comfort and minimizing future issues within the stomatognathic system [25,26]. Figure 6 and Figure 7 show how the use of T-Scan can improve occlusal adjustment in order to establish an IPO on fixed partial implant prostheses.
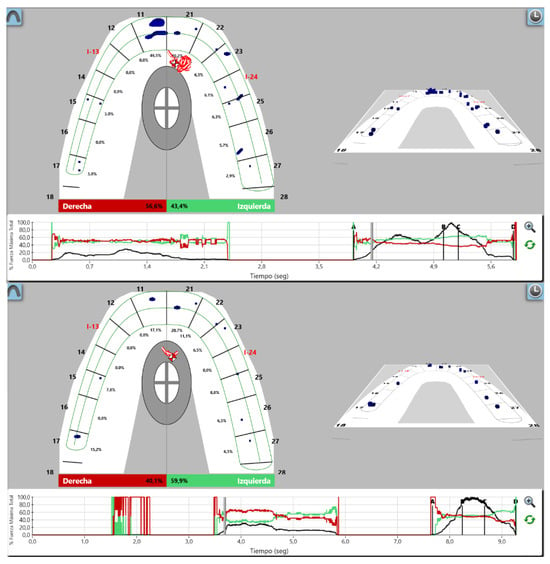
Figure 6.
Occlusal adjustment without exerting force. It can be seen after IPO that implants did not come into contact with their antagonists. Different colors are due to the differences in relative forces into each tooth.
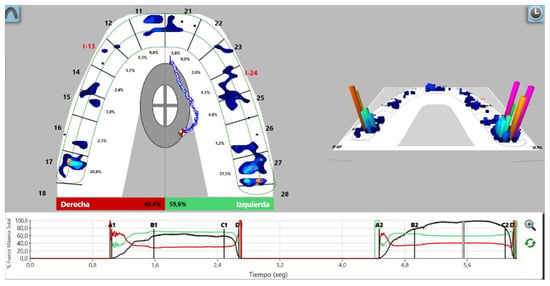
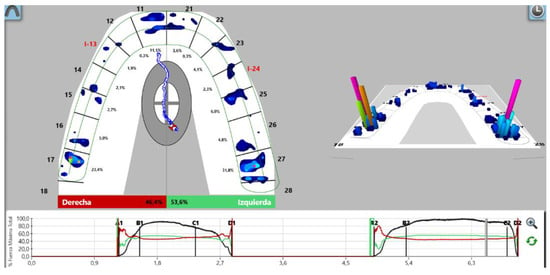
Figure 7.
Occlusal adjustment with exerting force. An improvement in the balance between the left and right hemi-arch can be seen after IPO. Different colors are due to different relative forces on each tooth.
To minimize occlusal loads on implant-supported teeth, Luo confirmed that the ideal approach is to achieve light contacts in MI on these teeth. His technique involved obtaining contacts on prostheses that differed from contacts on natural teeth by fractions of a second, which was also achieved in our study through data analysis. We can observe that, following the implementation of IPO, contacts on implant-supported prostheses occurred fractions of a second after contacts on natural teeth. This highlights the presence of a period of time in which the occlusion is compressed when maximum force is exerted, emphasizing the need to protect implants, which lack the anatomical structure of the PL for protection [25]. The absence of this time gap between contacts in natural teeth and implant-supported prostheses leads to problems in both prostheses and implants [27]. It was observed that patient sensation during chewing was improved in both groups, confirming that the application of IPO allows for greater comfort in the stomatognathic system, thus enhancing patients’ quality of life.
The objective of delayed contact on the prostheses was achieved by observing the number of protheses that did not make contact when the patient was asked to perform an MI without conscious biting demand after the implementation of IPO. As previously discussed, most of the prostheses did not make contact during an MI without conscious biting demand, while in forceful MI, theses prostheses exhibited loading and acted against their antagonist. This demonstrated that the implementation of IPO protects anatomical structures and enhances the physiology of the stomatognathic system [28,29].
In our study, we assessed how gender and age can impact patients’ occlusion and their implications for the health of implant-supported prostheses. Omiri concluded that women exert less occlusal force than men. The reasons cited were lower muscle mass and a smaller PL space. However, this was not reflected in our study, possibly due to an insufficient sample size [30].
Age does indeed influence the force exerted on the masticatory system, especially on implant-supported structures. With increasing age, tactile sensitivity and sensation decrease, particularly in implanted areas. This was confirmed by the data obtained in our study. As observed in Table 3, the subjective sensation of patients improved in many individuals under the age of 50, whereas in patients over 50, that subjective sensation often remained the same after IPO. Kazemi discovered that the older the patients are, the less sensations and sensitivity they have, so the subjective benefits obtained after IPO are not perceived as clearly [31].
Age also influences the behavior of the PL. Studies like those conducted by Benatti suggest that there is a certain involution of the cells involved in maintaining the PL as one ages. This leads to thinning and decreased keratinization, a reduction in cell density within the PL, and a decrease in collagen synthesis and the osteogenic capacity of PL cells. The osteoblastic capacity and osteoblast regeneration also diminish with age [32]. The presented results demonstrate how the time required for the prosthesis to contact with the antagonist decreases with age. This is in line with what Benatti has postulated, as the dysfunction experienced by the PL as one ages causes it to lose width and function. When we instructed patients to bite down in MI with conscious force, the PLs of older patients traveled a shorter distance to compress and were less elastic, resulting in a shorter compression time. Ohi showed that aging leads to hypermethylation of the genes responsible for the metabolism of collagen type I and type III, which are found in the PL [33]. Other studies, like those by Denes, indicated that dysfunction in the remaining teeth and alveolar processes leads to atrophy and dysfunction of PL cells. Consequently, when implants are placed, there are insufficient remaining cells capable of facilitating proper neurointegration [34].
Over the years, it has become evident that dentistry has ceased to be an analog activity and is rapidly entering the digital realm. While this digital world brings numerous advantages, it also comes with its own set of challenges and a steep learning curve to contend with. In our methodology, we aimed to incorporate two of the currently emerging digital systems to harness their full potential and use them to enhance the quality of life for patients. The EMG of the stomatognathic system does not differ significantly between dentate patients and patients with partial implant-supported dentures when chewing soft-textured foods. However, when hard foods are introduced, a lack of adaptability in the masticatory muscles of patients with partial implant-supported dentures becomes evident. Due to the absence of receptors (primarily due to the lack of a periodontal ligament in implants), the muscles lose feedback and fail to adapt to the generated changes. This is evident in the curves traced by the electrical impulses generated by muscles in an EMG, as demonstrated by Grigoriadis’ studies [35]. Dutour concluded in 2008 that implant-supported bridges have minimal impact on muscular activity during chewing due to the low percentage of load received by the prosthesis after IPO [36].
EMG does not exhibit significant changes following the balance of an implant-supported partial denture; thus, there will not be changes in the patient’s subjective sensation either. Regarding age-related EMG, it was concluded that there were no significant differences among different age groups [37]. The relationship between age and EMG can be explained through differences in the width of the PL with age. Over time, the PL loses thickness and its normal activity, potentially leading to the appearance of prematurities and interferences, or occlusal overload resulting in changes in EMG. However, this aspect was not reflected in the EMG values in our study, although a trend toward decreasing EMG values was observed when the time to achieve prosthesis contact decreased. This could be attributed to better adjustment and occlusal balance achieved with lower contact time, reducing the likelihood of prematurities and interferences, which in turn could promote the relaxation of the masticatory muscles.
Regarding methods for analyzing patient occlusion, conventional occlusal analysis methods have proven to be less efficient in achieving their objectives in this study. It was observed that Group 2 achieved better results than those patients who underwent the study using conventional methods. This translates to easier implementation of IPO when digital methods are used, compared to Group 1 where only conventional methods were employed [38,39,40].
After analyzing the obtained data, there is a recognized need for expanding the sample size through multicenter trials.
This study provides us with information that confirms the importance of occlusion in odontology, and particularly in fixed partial implant prostheses. Due to the differences between natural teeth and fixed implant prostheses, it is necessary to advance in new methods of occlusal adjustment in order to increase the life of prostheses.
As a result of this new method, it has been demonstrated that PL width becomes smaller with the age of patients. The importance of this demonstration provides us with the information to ensure better actuation when a fixed implant prosthesis is placed. This provides patients with more satisfaction and a healthier stomatognathic system.
5. Conclusions
- It has been shown that there are many differences between dental implants and teeth.
- The use of digital software improves the results of occlusal adjustment.
- Age affects the sensitivity of patients and the results of the adjustment.
- LPO is influenced by age: the older the person is, the more time is needed to compress the LPO.
Author Contributions
J.D.Z., principal investigator; S.D.Z., writing—review and editing; J.M., validation; B.G.-C., project administration; J.F.-F., project administration; A.D.Z., supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of University of Salamanca (protocol code Nº 587 approved on 17 December 2021) for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author (due to privacy restrictions).
Acknowledgments
We would like to express our gratitude to Dib Bucodental SL for providing the dental office for conducting the study and for granting access to medical records for patient recruitment. Additionally, we extend our thanks to the Odontological Clinic of the University of Salamanca for allowing the use of medical records for patient recruitment.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Swaminathan, Y.; Rao, G. Implant Protected Occlusion. J. Dent. Med. Sci. 2013, 11, 20–25. [Google Scholar] [CrossRef]
- Graves, C.V.; Harrel, S.K.; Rossmann, J.A.; Kerns, D.; Gonzalez, J.A.; Kontogiorgos, E.D.; Al-Hashimi, I.; Abraham, C. The Role of Occlusion in the Dental Implant and Peri-implant Condition: A Review. Open Dent. J. 2016, 10, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J.C.C.; Sukotjo, C. Occlusion for implant-supported fixed dental prostheses in partially edentulous patients: A literature review and current concepts. J. Periodontal. Implant Sci. 2013, 43, 51–57. [Google Scholar] [CrossRef]
- Michalakis, K.X.; Calvani, P.; Hirayama, H. Biomechanical considerations on tooth-implant supported fixed partial dentures. J. Dent. Biomech. 2012, 3, 1758736012462025. [Google Scholar] [CrossRef]
- Haggard, P.; de Boer, L. Oral somatosensory awareness. Neurosci. Biobehav. Rev. 2014, 47, 469–484. [Google Scholar] [CrossRef]
- Lim, W.H.; Liu, B.; Mah, S.J.; Chen, S.; Helms, J.A. The molecular and cellular effects of ageing on the periodontal ligament. J. Clin. Periodontol. 2014, 41, 935–942. [Google Scholar] [CrossRef]
- Yilmaz, G.; Laine, C.M.; Tinastepe, N.; Özyurt, M.G.; Türker, K.S. Periodontal mechanoreceptors and bruxism at low bite forces. Arch. Oral. Biol. 2019, 98, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kweon, H.H.I.; Choi, S.H.; Kim, Y.T. Association between dental implants in the posterior region and traumatic occlusion in the adjacent premolars: A long-term follow-up clinical and radiographic analysis. J. Periodontal. Implant Sci. 2016, 46, 396–404. [Google Scholar] [CrossRef]
- Sheridan, R.A.; Decker, A.M.; Plonka, A.B.; Wang, H.L. The Role of Occlusion in Implant Therapy: A Comprehensive Updated Review. Implant Dent. 2016, 25, 829–838. [Google Scholar] [CrossRef]
- Zhou, T.; Wongpairojpanich, J.; Sareethammanuwat, M.; Lilakhunakon, C.; Buranawat, B. Digital occlusal analysis of pre and post single posterior implant restoration delivery: A pilot study. PLoS ONE 2021, 16, e0252191. [Google Scholar] [CrossRef]
- Oliveira, A.; Bessa, A.; Dias, F.; Oliveira, A. Clinical applications of occlusion principles in implantology—Narrative review. J. Surg. Peridontology Implant Res. 2019, 1, 40–45. [Google Scholar]
- Wiens, J.P.; Priebe, J.W. Occlusal stability. Dent. Clin. N. Am. 2014, 58, 19–43. [Google Scholar] [CrossRef] [PubMed]
- Abichandani, S.; Bhojaraju, N.; Guttal, S.; Srilakshmi, J. Implant protected occlusion: A comprehensive review. Eur. J. Prosthodont. 2013, 1, 29. [Google Scholar] [CrossRef]
- Madani, A.S.; Nakhaei, M.; Alami, M.; Haghi, H.R.; Moazzami, S.M. Post-insertion posterior single-implant occlusion changes at different intervals: A T-scan computerized occlusal analysis. J. Contemp. Dent. Pract. 2017, 18, 927–932. [Google Scholar] [CrossRef] [PubMed]
- Afrashtehfar, K.I.; Qadeer, S. Computerized occlusal analysis as an alternative occlusal indicator. Cranio-J. Craniomandib. Pract. 2016, 34, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Chaithanya, R.; Sajjan, S.; Raju, A.R. A study of change in occlusal contacts and force dynamics after fixed prosthetic treatment and after equilibration—Using Tekscan III. J. Indian Prosthodont. Soc. 2019, 19, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Röhrle, O.; Saini, H.; Lee, P.V.S.; Ackland, D.C. A novel computational method to determine subject-specific bite force and occlusal loading during mastication. Comput. Methods Biomech. Biomed. Eng. 2018, 21, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Roque, M.A.; Gallucci, G.O.; Lee, S.J. Occlusal Pressure Redistribution with Single Implant Restorations. J. Prosthodont. 2017, 26, 275–279. [Google Scholar] [CrossRef]
- Qadeer, S.; Kerstein, R.; Kim, R.J.Y.; Huh, J.B.; Shin, S.W. Relationship between articulation paper mark size and percentage of force measured with computerized occlusal analysis. J. Adv. Prosthodont. 2012, 4, 7–12. [Google Scholar] [CrossRef]
- Dib-Zakkour, J.; Flores-Fraile, J.; Montero-Martin, J.; Dib-Zakkour, S.; Dib-Zaitun, I. Evaluation of the Effectiveness of Dry Needling in the Treatment of Myogenous Temporomandibular Joint Disorders. Medicina 2022, 58, 256. [Google Scholar] [CrossRef]
- Dib, A.; Montero, J.; Sanchez, J.M.; López-Valverde, A. Electromyographic and patient-reported outcomes of a computer-guided occlusal adjustment performed on patients suffering from chronic myofascial pain. Med. Oral Patol. Oral Cir. Bucal. 2015, 20, e135–e143. Available online: http://www.ncbi.nlm.nih.gov/pubmed/25475783 (accessed on 12 November 2017). [CrossRef] [PubMed]
- Lewis, M.B.; Klineberg, I. Prosthodontic considerations designed to optimize outcomes for single-tooth implants. A review of the literature. Aust. Dent. J. 2011, 56, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Nuzzolese, E.; Lepore, M.M.; Cukovic-Bagic, I.; Montagna, F.; Di Vella, G. Forensic sciences and forensic odontology. Int. Dent. J. 2008, 58, 342–348. [Google Scholar] [CrossRef]
- Duyck, J.; Vandamme, K. The effect of loading on peri-implant bone: A critical review of the literature. J. Oral Rehabil. 2014, 41, 783–794. [Google Scholar] [CrossRef]
- Luo, Q.; Ding, Q.; Zhang, L.; Xie, Q. Analyzing the occlusion variation of single posterior implant–supported fixed prostheses by using the T-scan system: A prospective 3-year follow-up study. J. Prosthet. Dent. 2020, 123, 79–84. [Google Scholar] [CrossRef]
- Koos, B.; Godt, A.; Schille, C.; Göz, G. Präzision eines instrumentellen Analyseverfahrens der Okklusion und ihrer resultierenden Kraftverteilung im Zahnbogen. J. Orofac. Orthop. 2010, 71, 403–410. [Google Scholar] [CrossRef]
- Sadowsky, S.J. Occlusal overload with dental implants: A review. Int. J. Implant Dent. 2019, 5, 29. [Google Scholar] [CrossRef] [PubMed]
- Cordaro, L.; Torsello, F.; Rocuzzo, M. Implant loading protocols for the partially edentulous posterior mandible. Int. J. Oral Maxillofac. Implants 2009, 24, 169–179. Available online: http://www.ncbi.nlm.nih.gov/pubmed/19885444 (accessed on 15 March 2022).
- Ding, X.; Liao, S.H.; Zhu, X.H.; Zhang, X.H.; Zhang, L. Effect of diameter and length on stress distribution of the alveolar crest around immediate loading implants. Clin. Implant Dent. Relat. Res. 2009, 11, 279–287. [Google Scholar] [CrossRef]
- Al-Omiri, M.K.; Sghaireen, M.G.; Alhijawi, M.M.; Alzoubi, I.A.; Lynch, C.D.; Lynch, E. Maximum bite force following unilateral implant-supported prosthetic treatment: Within-subject comparison to opposite dentate side. J. Oral Rehabil. 2014, 41, 624–629. [Google Scholar] [CrossRef]
- Kazemi, M.; Geramipanah, F.; Negahdari, R.; Rakhshan, V. Active tactile sensibility of single-tooth implants versus natural dentition: A split-mouth double-blind randomized clinical trial. Clin. Implant Dent. Relat. Res. 2014, 16, 947–955. [Google Scholar] [CrossRef] [PubMed]
- Lossdörfer, S.; Kraus, D.; Jäger, A. Aging affects the phenotypic characteristics of human periodontal ligament cells and the cellular response to hormonal stimulation in vitro. J. Periodontal. Res. 2010, 45, 764–771. [Google Scholar] [CrossRef] [PubMed]
- Benatti, B.B.; Silverio, K.G.; Casati, M.Z.; Sallum, E.A.; Nociti, F.H. Influence of aging on biological properties of periodontal ligament cells. Connect. Tissue Res. 2008, 49, 401–408. [Google Scholar] [CrossRef]
- Denes, B.J.; Mavropoulos, A.; Bresin, A.; Kiliaridis, S. Influence of masticatory hypofunction on the alveolar bone and the molar periodontal ligament space in the rat maxilla. Eur. J. Oral Sci. 2013, 121, 532–537. [Google Scholar] [CrossRef]
- Grigoriadis, A.; Trulsson, M. Excitatory drive of masseter muscle during mastication with dental implants. Sci. Rep. 2018, 8, 8597. [Google Scholar] [CrossRef]
- Grigoriadis, A.; Johansson, R.S.; Trulsson, M. Adaptability of mastication in people with implant-supported bridges. J. Clin. Periodontol. 2011, 38, 395–404. [Google Scholar] [CrossRef]
- Mishellany-Dutour, A.; Renaud, J.; Peyron, M.A.; Rimek, F.; Woda, A. Is the goal of mastication reached in young dentates, aged dentates and aged denture wearers? Br. J. Nutr. 2008, 99, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Kerstein, R.B.; Radke, J. Clinician accuracy when subjectively interpreting articulating paper markings. Cranio-J. Craniomandib. Sleep Pract. 2014, 32, 13–23. [Google Scholar] [CrossRef]
- Carey, J.P.; Craig, M.; Kerstein, R.B.; Radke, J. Determining a Relationship Between Applied Occlusal Load and Articulating Paper Mark Area. Open Dent. J. 2007, 1, 1–7. [Google Scholar] [CrossRef]
- Lee, S.M.; Lee, J.W. Computerized occlusal analysis: Correlation with occlusal indexes to assess the outcome of orthodontic treatment or the severity of malocculusion. Korean J. Orthod. 2016, 46, 27–35. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).