Customized Facial Orthopedics: Proof of Concept for Generating 3D-Printed Extra-Oral Appliance for Early Intervention in Class III Malocclusion
Abstract
1. Introduction
2. Materials and Methods
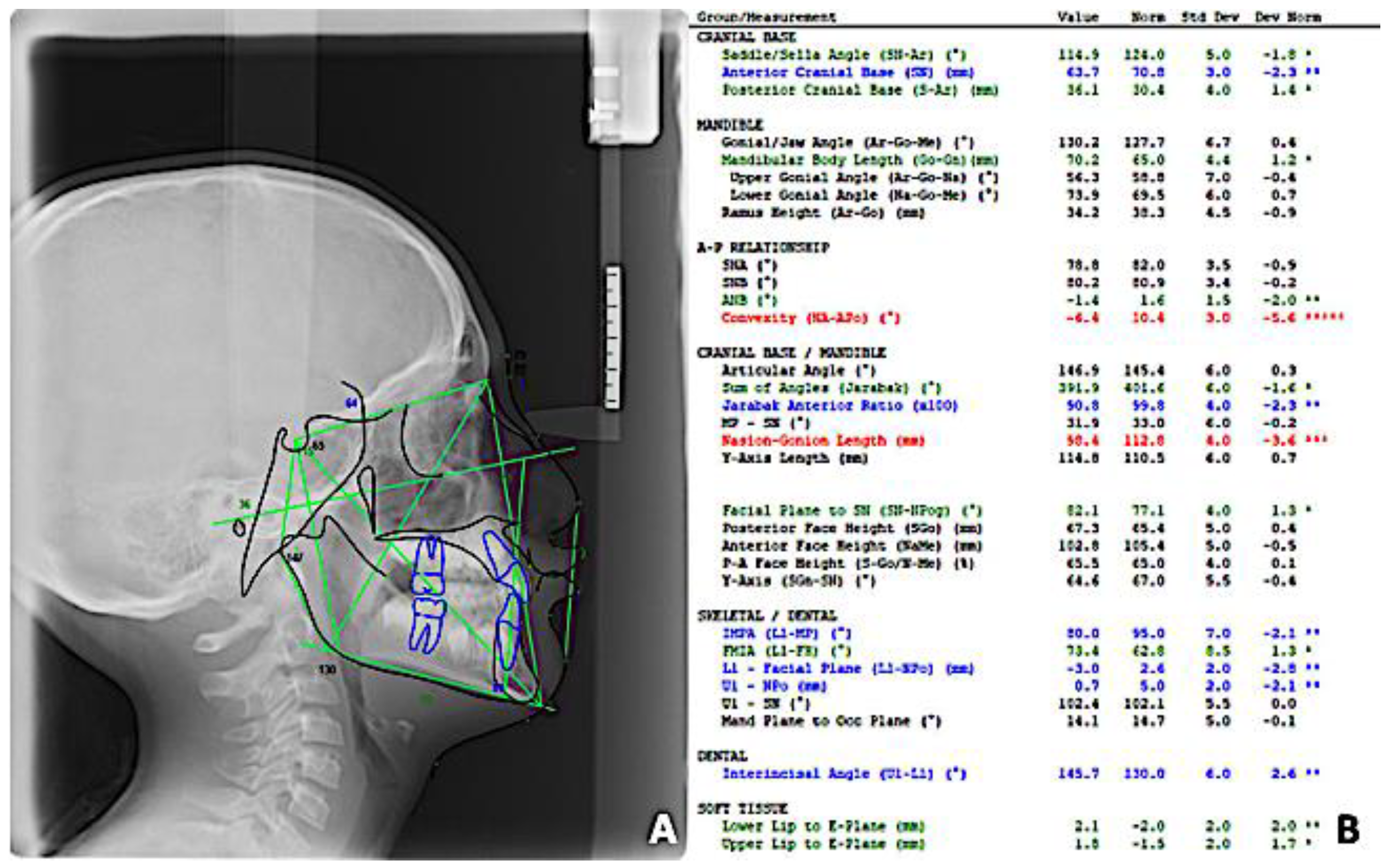
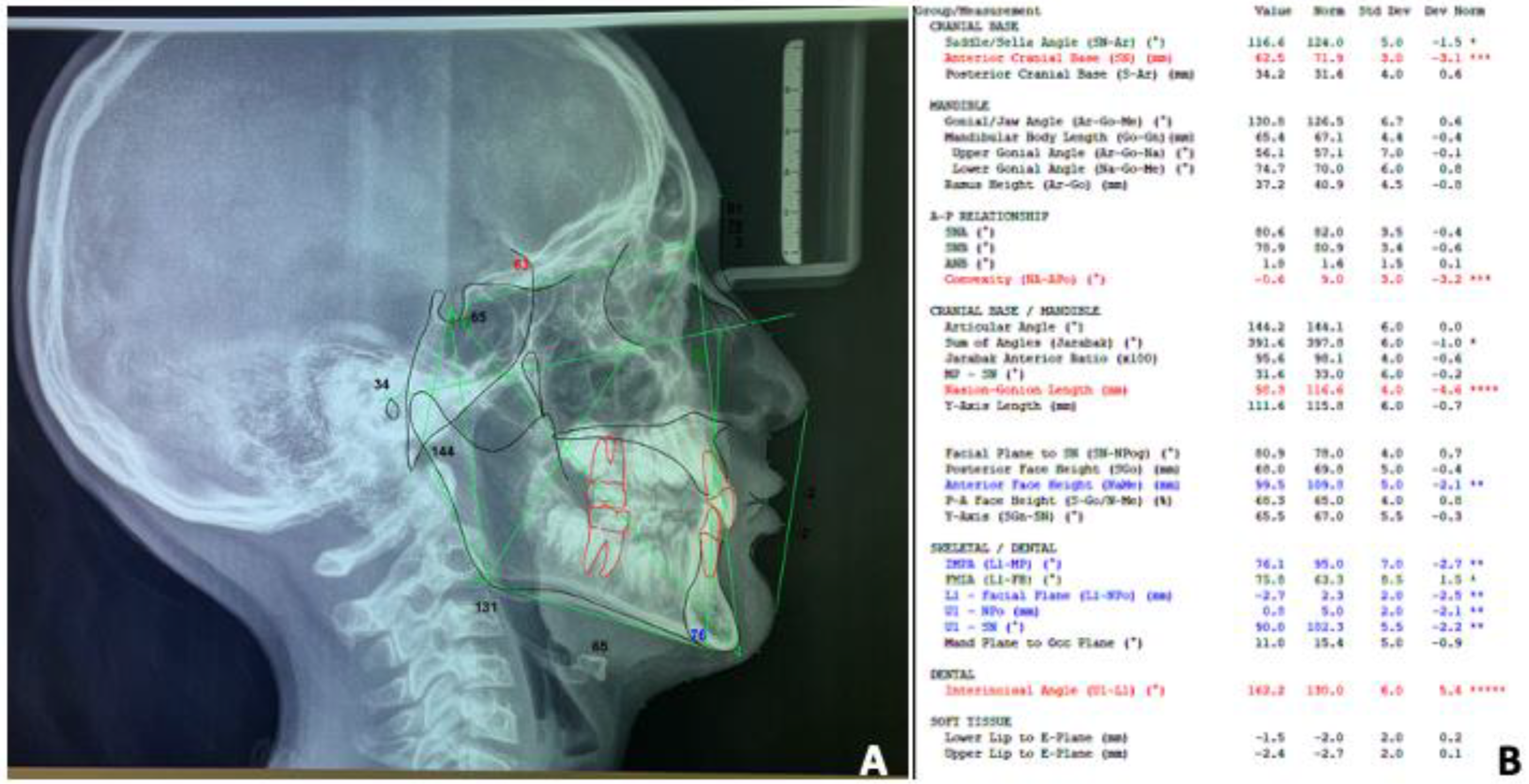
2.1. Clinical Examination
2.2. Customized Chin Cup Appliances
2.2.1. Analogic Workflow (Analogic-CC)
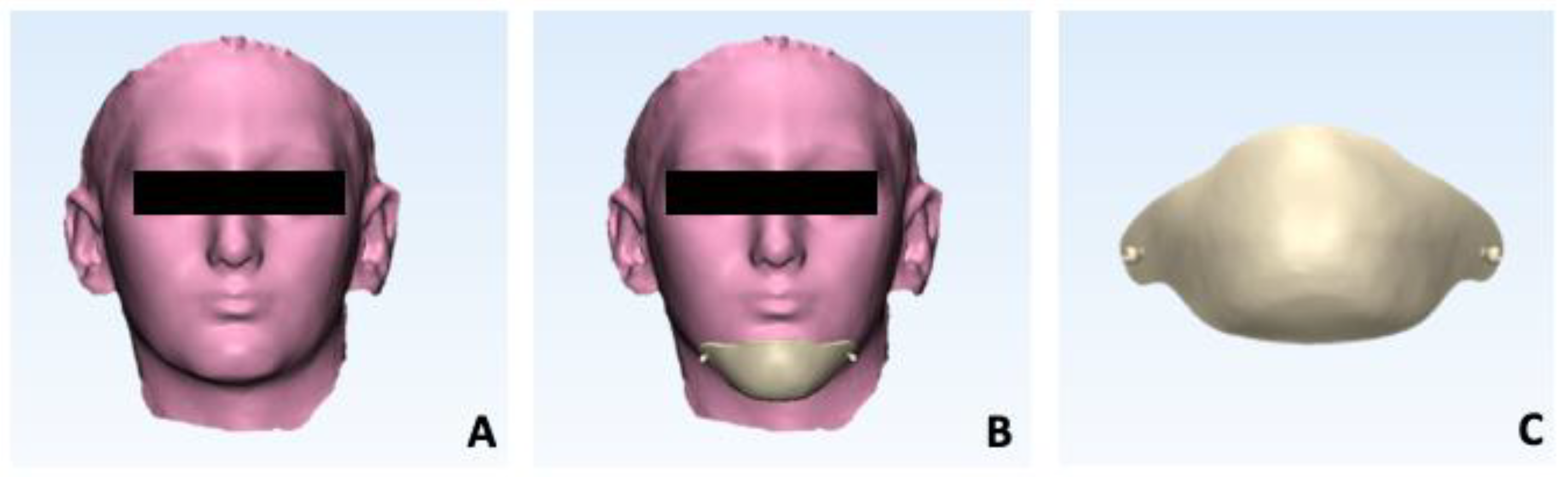
2.2.2. Stereolithography-Based Workflow (FS-CC)
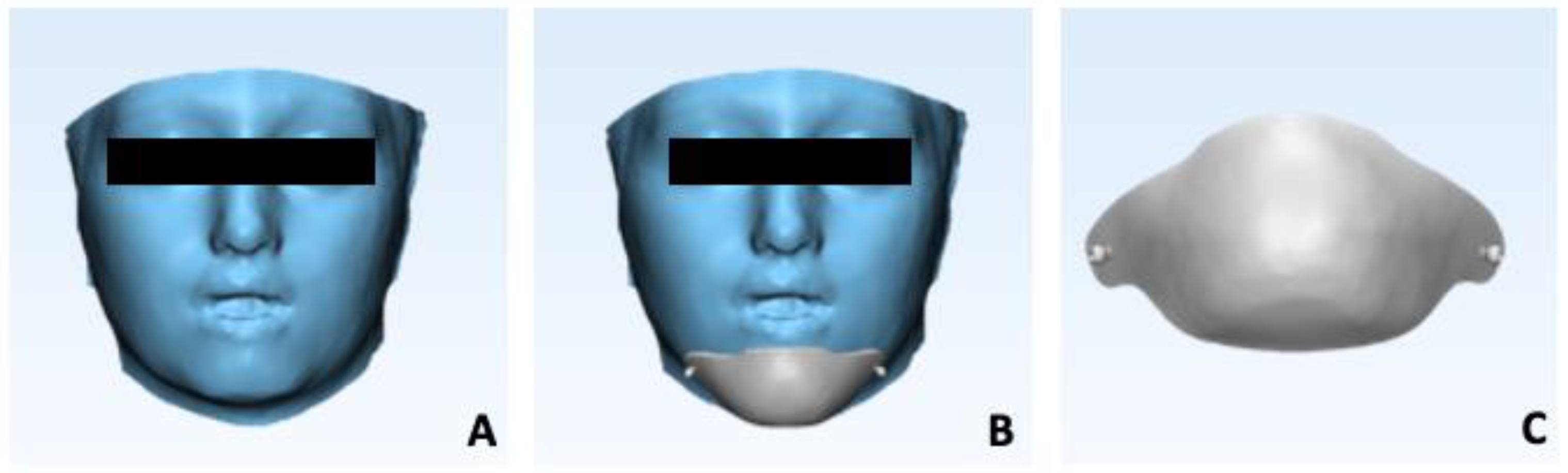
2.2.3. CBCT-Based Workflow (CBCT-CC)
2.3. Treatment Plan
2.4. Superimposition, Matching Percentage Calculation, and Deviation Analysis
3. Results
3.1. Clinical Outcomes
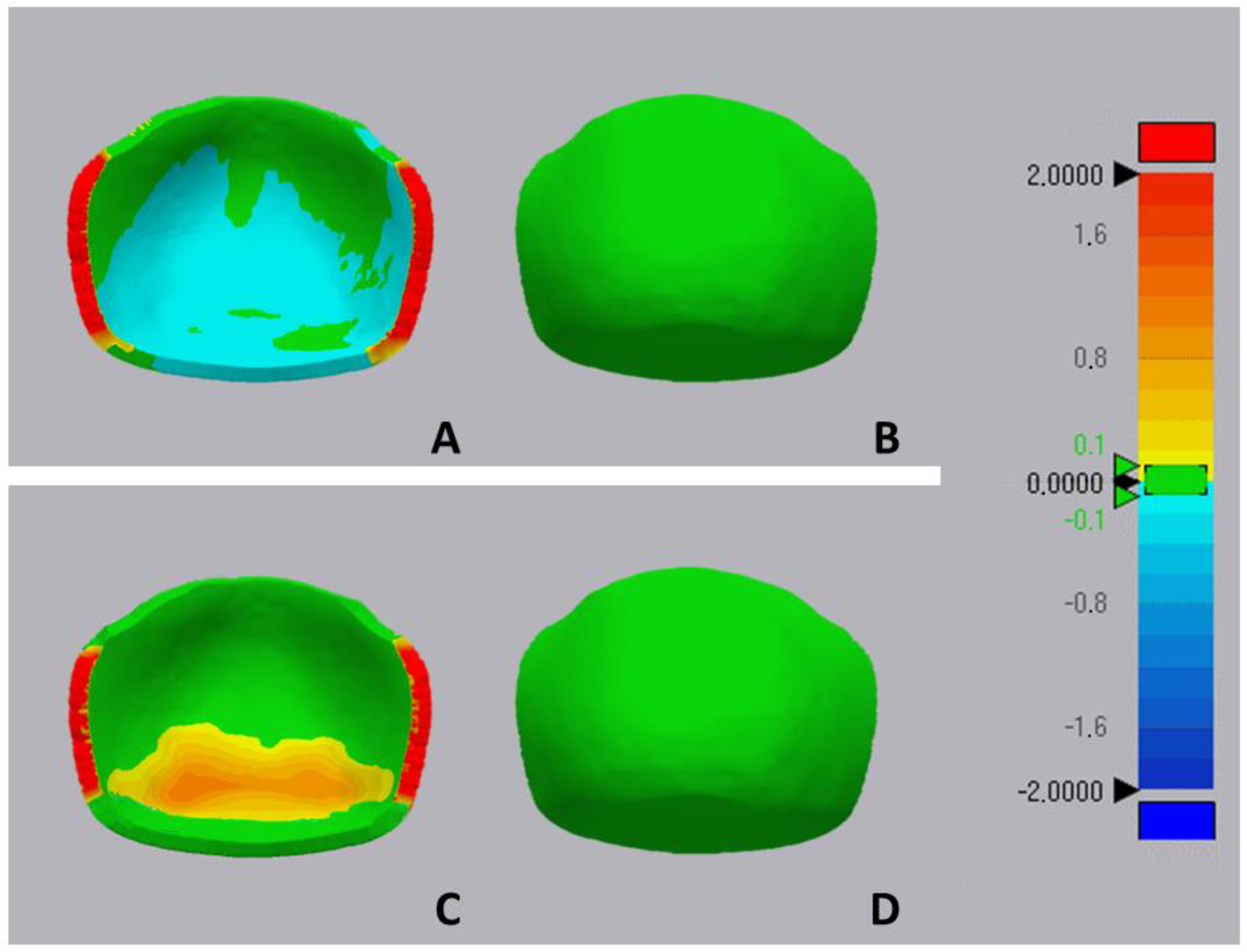
3.2. Deviation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Sanborn, R.T.J.A.O. Differences between the Facial Skeletal Patterns of Class III Malocclusion and Normal Occlusion. Angle Orthod. 2009, 25, 208–222. [Google Scholar]
- Guyer, E.C.; Ellis, E.E., 3rd; McNamara, J.A., Jr.; Behrents, R.G. Components of class III malocclusion in juveniles and adolescents. Angle Orthod. 1986, 56, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.; Andersen, C.E. The morphology of the potential Class III skeletal pattern in the growing child. Am. J. Orthod. 1986, 89, 302–311. [Google Scholar] [CrossRef]
- Karakıs, D.; Kaymak, D.; Dogan, A. The evaluation of maximum bite force in the occlusal rehabilitation of patient with Angle Class III malocclusion: A case report. J. Adv. Prosthodont. 2013, 5, 364–368. [Google Scholar] [CrossRef][Green Version]
- Ha, S.W.; Kim, S.J.; Choi, J.Y.; Baek, S.H. Characterization of facial asymmetry phenotypes in adult patients with skeletal Class III malocclusion using three-dimensional computed tomography and cluster analysis. Korean J. Orthod. 2022, 52, 85–101. [Google Scholar] [CrossRef]
- Almokri, N.M.; Alsaggaf, D.H.; Alsulaimani, F.F.; Zawawi, K.H. Anthropometric and Cephalometric Facial Characteristics of Adult Saudi Patients with Skeletal Class III Malocclusions. Contemp. Clin. Dent. 2023, 14, 232–238. [Google Scholar] [CrossRef]
- Hardy, D. Prevalence of angle class III malocclusion: A systematic review and meta-analysis. Open J. Epidemiol. 2012, 2, 75–82. [Google Scholar] [CrossRef]
- Soh, J.; Sandham, A.; Chan, Y.H. Occlusal status in Asian male adults: Prevalence and ethnic variation. Angle Orthod. 2005, 75, 814–820. [Google Scholar] [CrossRef] [PubMed]
- Toffol, L.D.; Pavoni, C.; Baccetti, T.; Franchi, L.; Cozza, P. Orthopedic treatment outcomes in Class III malocclusion. A systematic review. Angle Orthod. 2008, 78, 561–573. [Google Scholar] [CrossRef] [PubMed]
- Zurfluh, M.A.; Kloukos, D.; Patcas, R.; Eliades, T. Effect of chin-cup treatment on the temporomandibular joint: A systematic review. Eur. J. Orthod. 2015, 37, 314–324. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.G.; Kang, D.S. Prevalence of malocclusion among Latino adolescents. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 313–315. [Google Scholar] [CrossRef]
- Proffit, W.R.; Fields, H.W.; Sarver, D.M. Contemporary Orthodontics; Mosby Elsevier: Philadelphia, PA, USA, 2007. [Google Scholar]
- Liu, Z.P.; Li, C.J.; Hu, H.K.; Chen, J.W.; Li, F.; Zou, S.J. Efficacy of short-term chincup therapy for mandibular growth retardation in Class III malocclusion. Angle Orthod. 2011, 81, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Ritucci, R.; Nanda, R. The effect of chin cup therapy on the growth and development of the cranial base and midface. Am. J. Orthod. Dentofac. Orthop. 1986, 90, 475–483. [Google Scholar] [CrossRef]
- De Clerck, H.J.; Proffit, W.R. Growth modification of the face: A current perspective with emphasis on Class III treatment. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 37–46. [Google Scholar] [CrossRef]
- Fiori, A.; Minervini, G.; Nucci, L.; d’Apuzzo, F.; Perillo, L.; Grassia, V. Predictability of crowding resolution in clear aligner treatment. Prog. Orthod. 2022, 23, 43. [Google Scholar] [CrossRef] [PubMed]
- Chatzoudi, M.I.; Ioannidou-Marathiotou, I.; Papadopoulos, M.A. Clinical effectiveness of chin cup treatment for the management of Class III malocclusion in pre-pubertal patients: A systematic review and meta-analysis. Prog. Orthod. 2014, 15, 62. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Del Mondo, D.; Russo, D.; Cervino, G.; D’Amico, C.; Fiorillo, L. Stem Cells in Temporomandibular Joint Engineering: State of Art and Future Persectives. J. Craniofac. Surg. 2022, 33, 2181–2187. [Google Scholar] [CrossRef]
- Cacciatore, G.; Poletti, L.; Huanca Ghislanzoni, L. A chairside customized chin-cup. J. Clin. Orthod. JCO 2013, 2013, 352. [Google Scholar]
- Ayoub, A.F.; Xiao, Y.; Khambay, B.; Siebert, J.P.; Hadley, D. Towards building a photo-realistic virtual human face for craniomaxillofacial diagnosis and treatment planning. Int. J. Oral. Maxillofac. Surg. 2007, 36, 423–428. [Google Scholar] [CrossRef]
- Miracle, A.C.; Mukherji, S.K. Conebeam CT of the head and neck, part 1: Physical principles. AJNR. Am. J. Neuroradiol. 2009, 30, 1088–1095. [Google Scholar] [CrossRef]
- Leonardi, R.M.; Aboulazm, K.; Giudice, A.L.; Ronsivalle, V.; D’Antò, V.; Lagravère, M.; Isola, G. Evaluation of mandibular changes after rapid maxillary expansion: A CBCT study in youngsters with unilateral posterior crossbite using a surface-to-surface matching technique. Clin. Oral. Investig. 2021, 25, 1775–1785. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, A.; Ronsivalle, V.; Gastaldi, G.; Leonardi, R. Assessment of the accuracy of imaging software for 3D rendering of the upper airway, usable in orthodontic and craniofacial clinical settings. Prog. Orthod. 2022, 23, 22. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Xu, T.; Lin, J. Validation of a three-dimensional facial scanning system based on structured light techniques. Comput. Methods Programs Biomed. 2009, 94, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Blasi, A.; Nucera, R.; Ronsivalle, V.; Candida, E.; Grippaudo, C. Asymmetry index for the photogrammetric assessment of facial asymmetry. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 394–402. [Google Scholar] [CrossRef]
- Franchi, L.; Vichi, A.; Marti, P.; Lampus, F.; Guercio, S.; Recupero, A.; Giuntini, V.; Goracci, C. 3D Printed Customized Facemask for Maxillary Protraction in the Early Treatment of a Class III Malocclusion: Proof-of-Concept Clinical Case. Materials 2022, 15, 3747. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Kim, J.S.; Kim, C.S.; Becker-Weimann, S.Y.; Cha, J.Y.; Choi, S.H. Skin irritation in children undergoing orthodontic facemask therapy. Sci. Rep. 2023, 13, 2200. [Google Scholar] [CrossRef] [PubMed]
- Kwak, H.J.; Park, H.J.; Kim, Y.J.; Lee, D.Y. Factors associated with long-term vertical skeletal changes induced by facemask therapy in patients with Class III malocclusion. Angle Orthod. 2018, 88, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Arreghini, A.; Trigila, S.; Lombardo, L.; Siciliani, G. Objective assessment of compliance with intra- and extraoral removable appliances. Angle Orthod. 2017, 87, 88–95. [Google Scholar] [CrossRef]
- Lee, J.D.; Nguyen, O.; Lin, Y.-C.; Luu, D.; Kim, S.; Amini, A.; Lee, S.J. Facial Scanners in Dentistry: An Overview. Prosthesis 2022, 4, 664–678. [Google Scholar]
- Lavorgna, L.; Cervino, G.; Fiorillo, L.; Di Leo, G.; Troiano, G.; Ortensi, M.; Galantucci, L.; Cicciù, M. Reliability of a Virtual Prosthodontic Project Realized through a 2D and 3D Photographic Acquisition: An Experimental Study on the Accuracy of Different Digital Systems. Int. J. Environ. Res. Public Health 2019, 16, 5139. [Google Scholar] [CrossRef]
- Reddy, N.; Vempalli, S.; Prakash, J.; Suganna, M.; Meenakshi, S.I.; Shivakumar, G.C.; Crimi, S.; Minervini, G. Evaluation of the Effect of Digital Dentistry on the Accuracy of Implant Placement and Prosthesis Fabrication— A Systematic Review and Meta-Analysis. Prosthesis 2023, 5, 666–677. [Google Scholar]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ronsivalle, V.; Gastaldi, G.; Fiorillo, G.; Amato, A.; Loreto, C.; Leonardi, R.; Lo Giudice, A. Customized Facial Orthopedics: Proof of Concept for Generating 3D-Printed Extra-Oral Appliance for Early Intervention in Class III Malocclusion. Prosthesis 2024, 6, 135-145. https://doi.org/10.3390/prosthesis6010011
Ronsivalle V, Gastaldi G, Fiorillo G, Amato A, Loreto C, Leonardi R, Lo Giudice A. Customized Facial Orthopedics: Proof of Concept for Generating 3D-Printed Extra-Oral Appliance for Early Intervention in Class III Malocclusion. Prosthesis. 2024; 6(1):135-145. https://doi.org/10.3390/prosthesis6010011
Chicago/Turabian StyleRonsivalle, Vincenzo, Giorgio Gastaldi, Gianluigi Fiorillo, Alessandra Amato, Carla Loreto, Rosalia Leonardi, and Antonino Lo Giudice. 2024. "Customized Facial Orthopedics: Proof of Concept for Generating 3D-Printed Extra-Oral Appliance for Early Intervention in Class III Malocclusion" Prosthesis 6, no. 1: 135-145. https://doi.org/10.3390/prosthesis6010011
APA StyleRonsivalle, V., Gastaldi, G., Fiorillo, G., Amato, A., Loreto, C., Leonardi, R., & Lo Giudice, A. (2024). Customized Facial Orthopedics: Proof of Concept for Generating 3D-Printed Extra-Oral Appliance for Early Intervention in Class III Malocclusion. Prosthesis, 6(1), 135-145. https://doi.org/10.3390/prosthesis6010011










