The Use of a Surgical Template for the Insertion of Dental Implants and Sinus Lift with the Summers Technique Based on Digital Planning: A Case Report
Abstract
1. Introduction
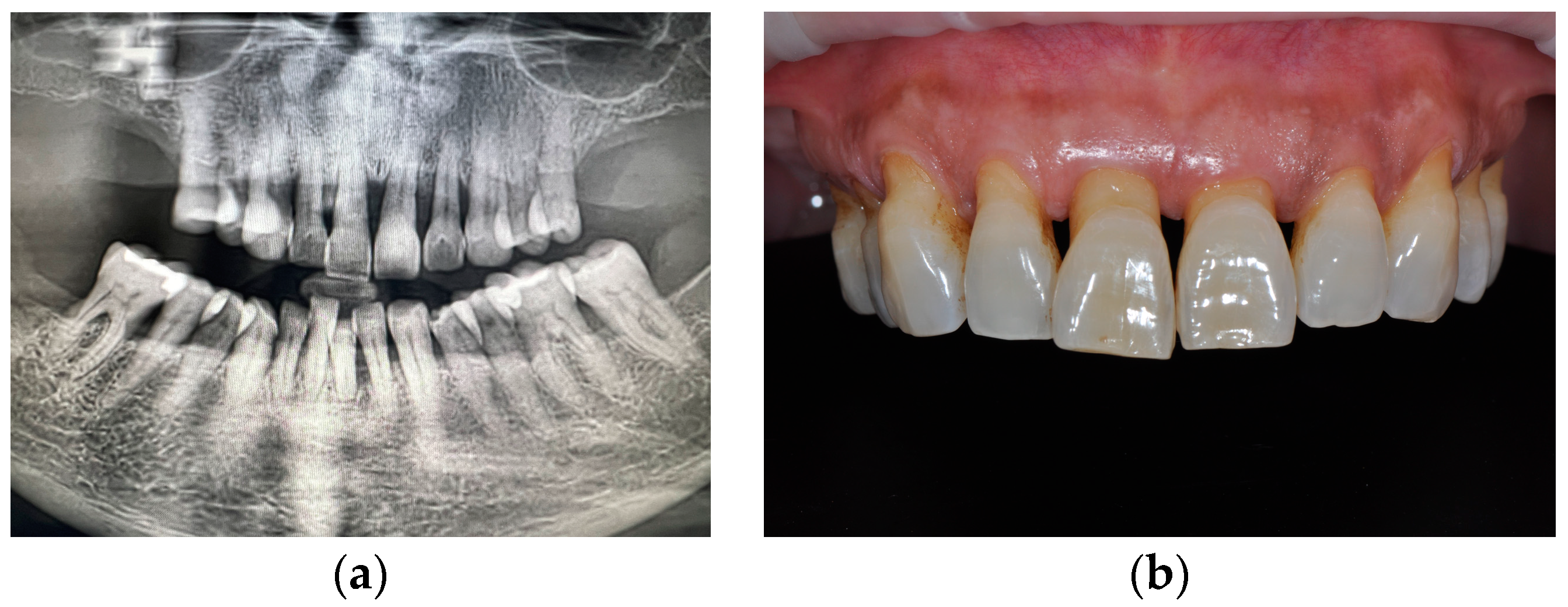
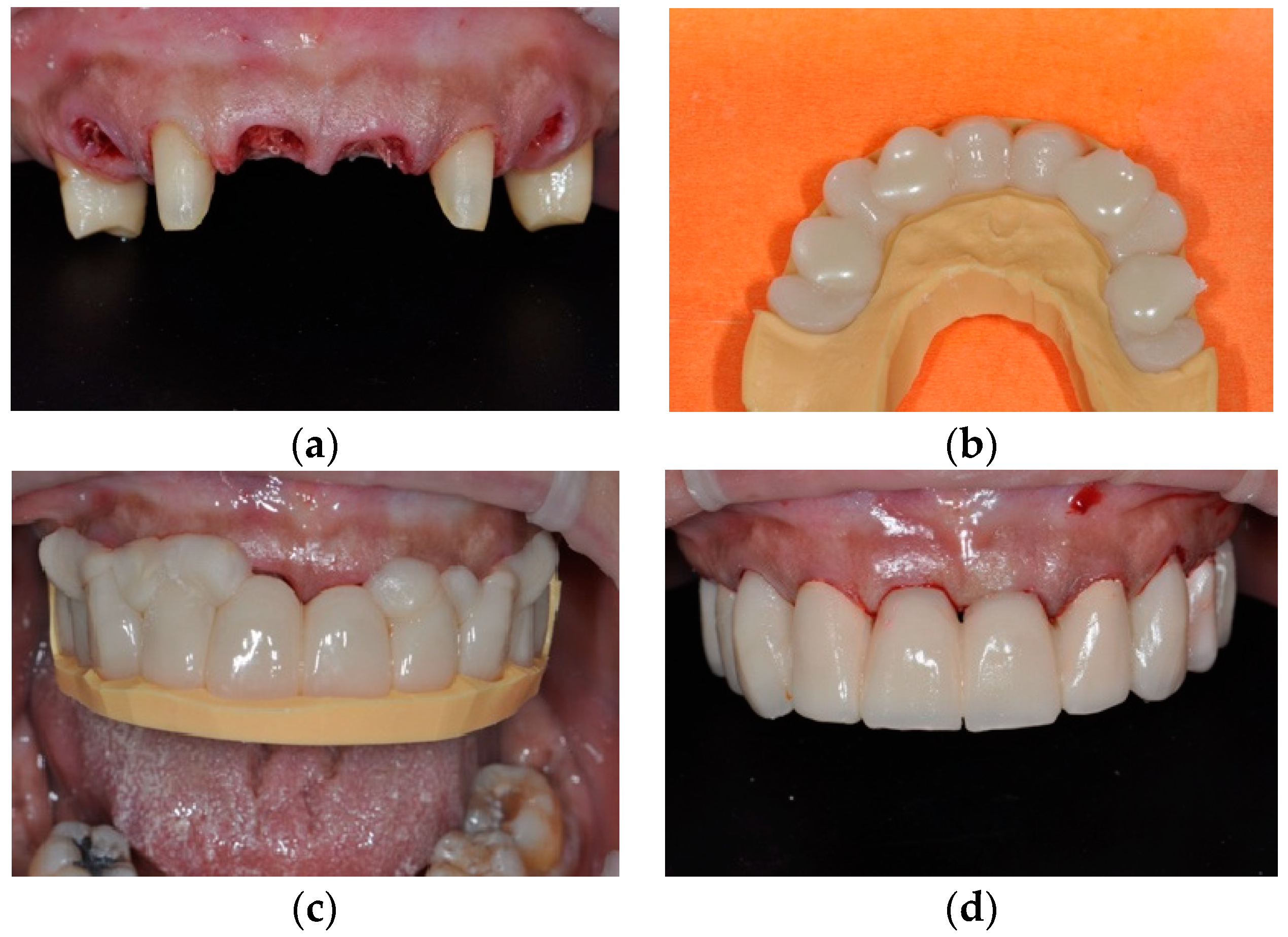
2. Materials and Methods
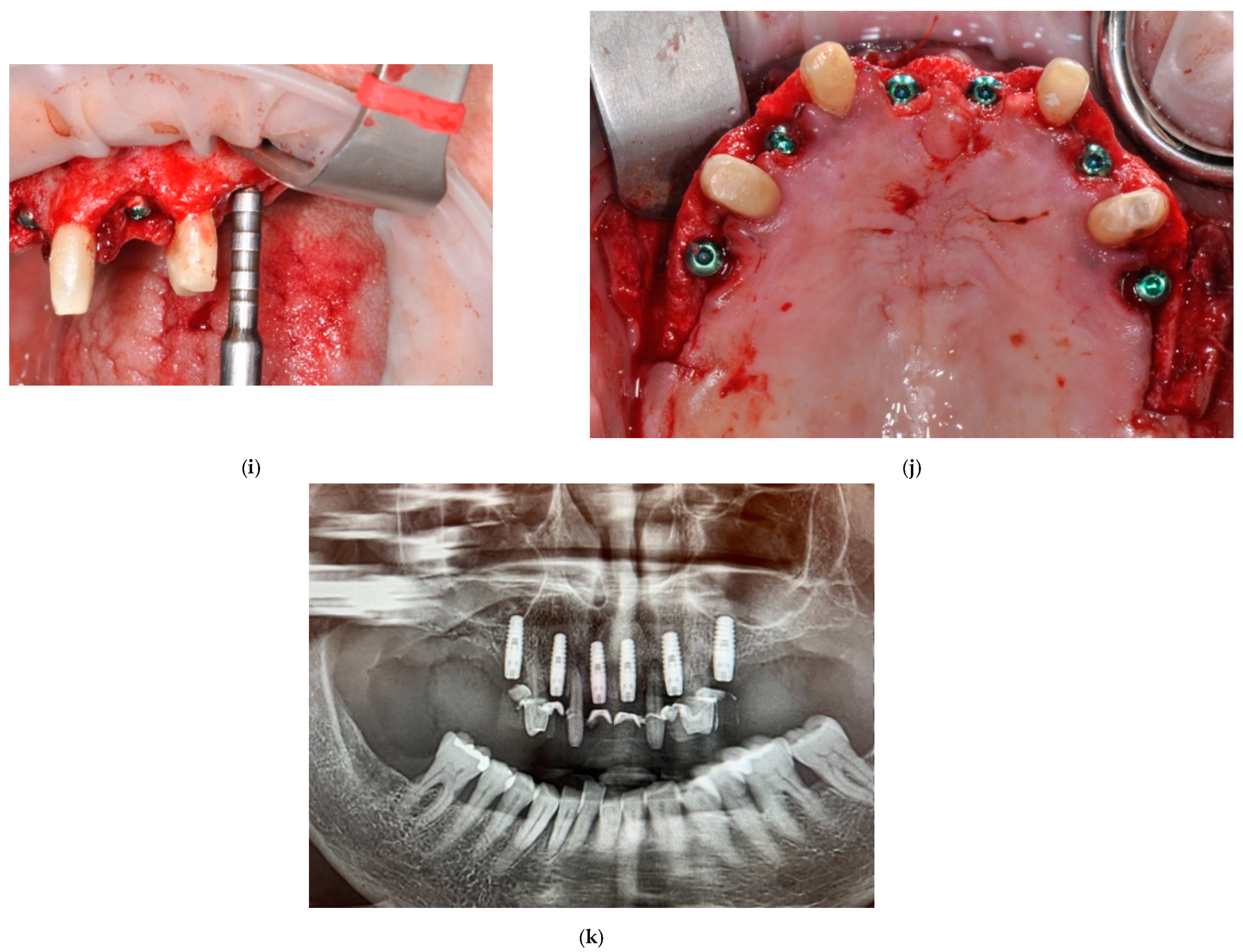
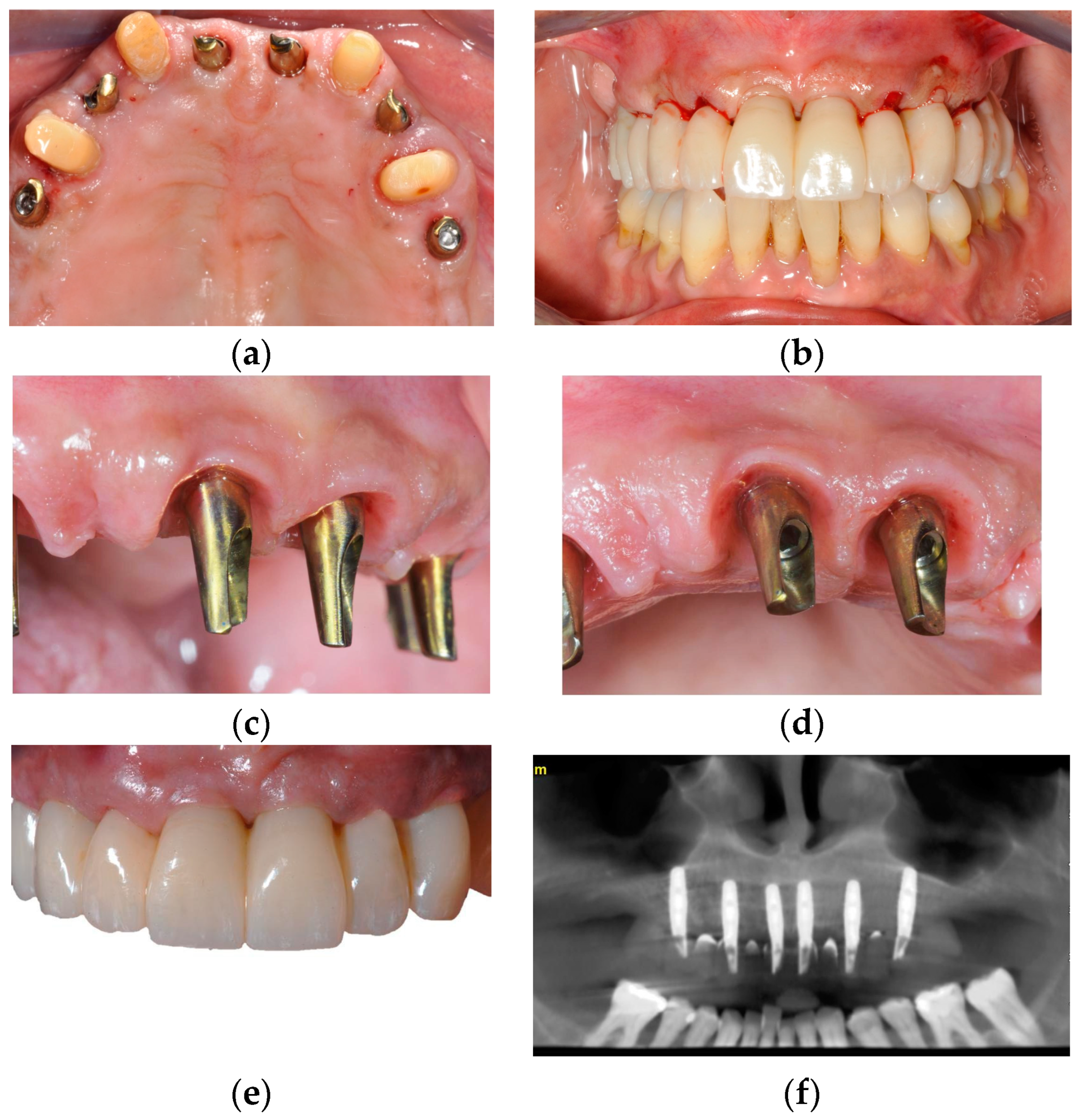
2.1. Surgical Phase
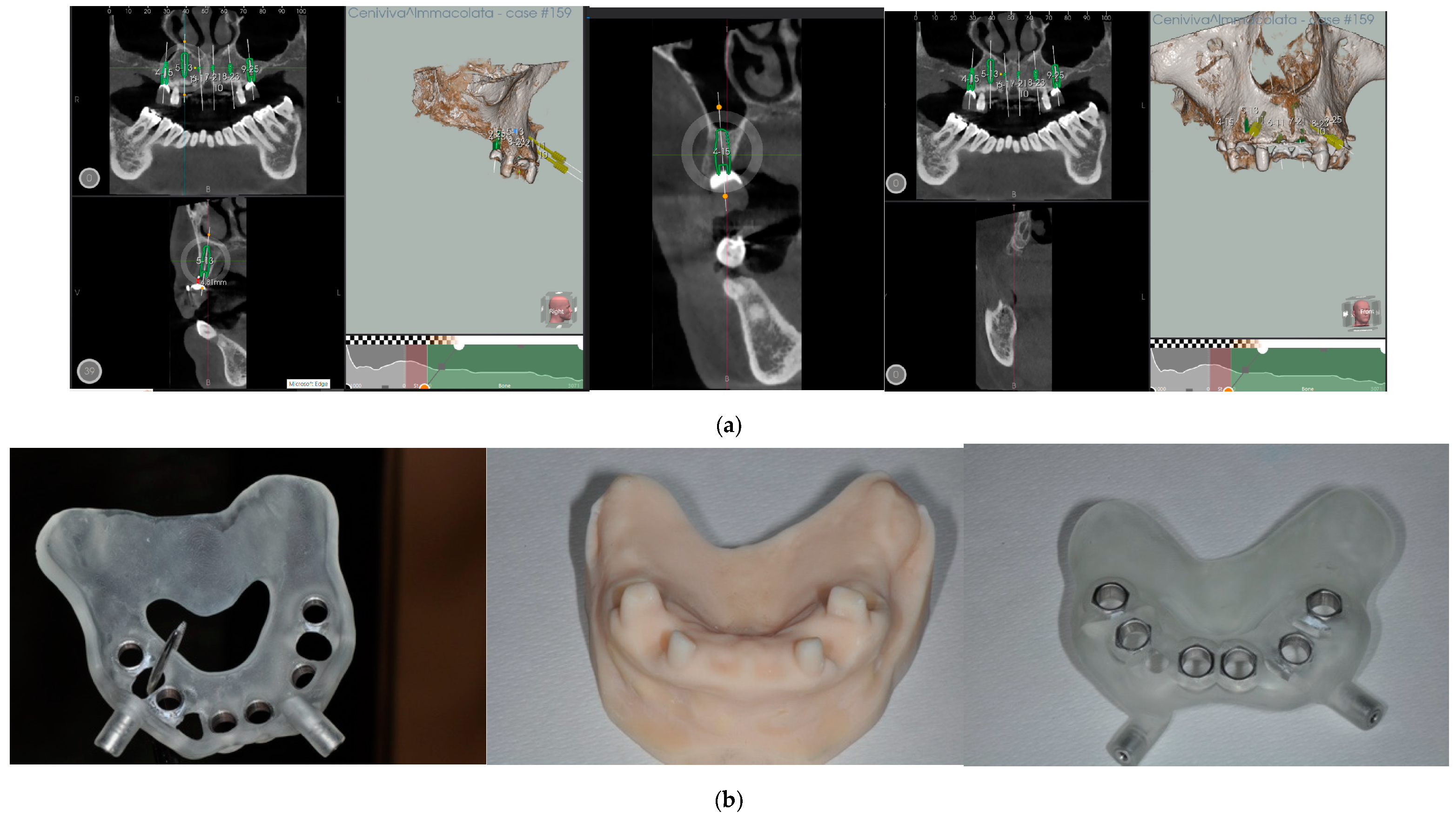
2.2. Computer-Guided Surgical Planning
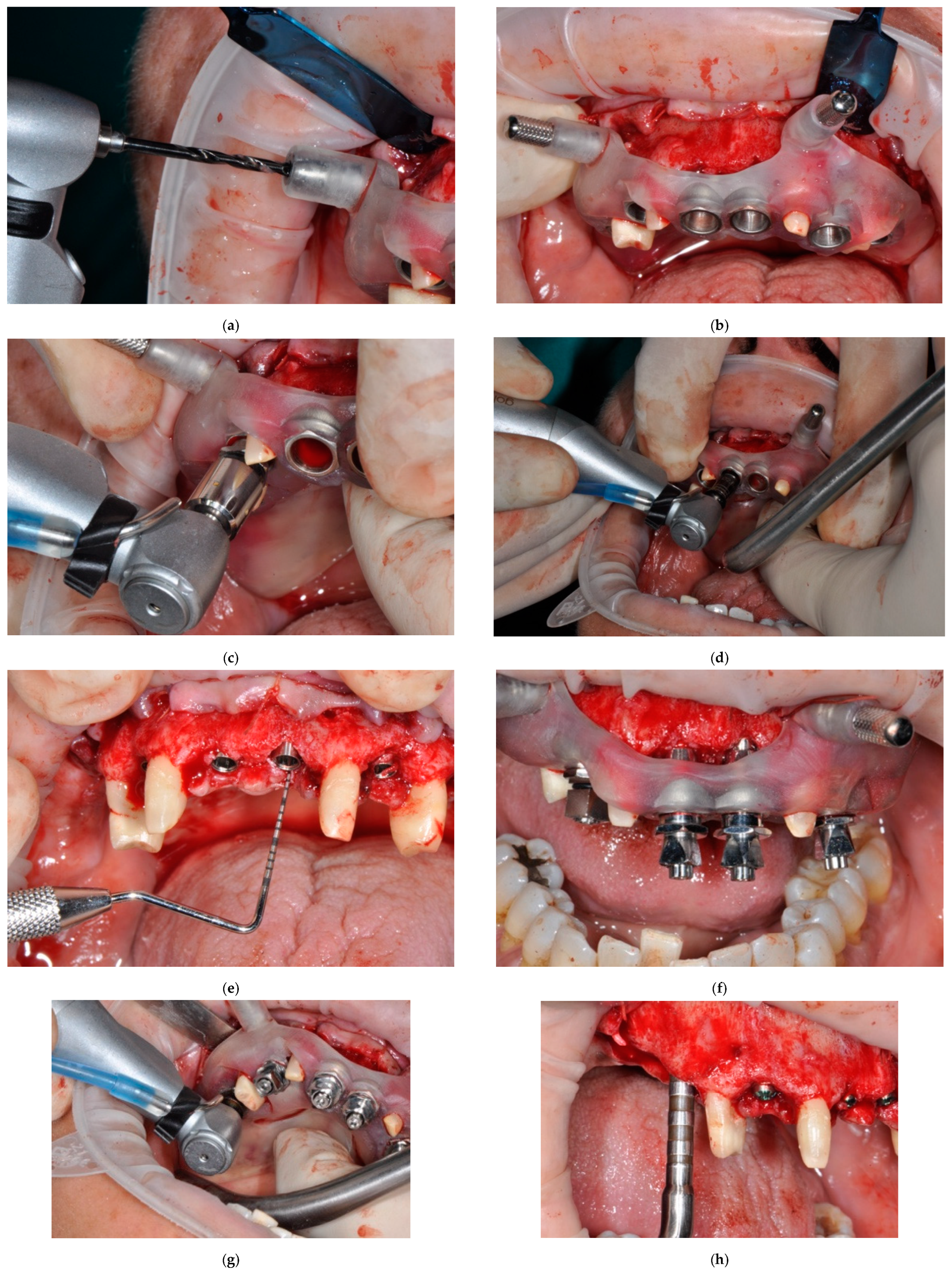
2.3. Surgical Phase: Insertion of the Implants
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Verstreken, K.; Van Cleynenbreugel, J.; Marchal, G.; Naert, I.; Suetens, P.; van Steenberghe, D. Computer-assisted planning of oral implant surgery: A three-dimensional approach. Int. J. Oral Maxillofac. Implant. 1996, 11, 806–810. [Google Scholar]
- Beretta, M.; Poli, P.P.; Maiorana, C. Accuracy of computer-aided template-guided oral implant placement: A prospective clinical study. J. Periodontal Implant. Sci. 2014, 44, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Makarov, N.; Pompa, G.; Papi, P. Computer-assisted implant placement and full-arch immediate loading with digitally prefabricated provisional prostheses without cast: A prospective pilot cohort study. Int. J. Implant. Dent. 2021, 7, 80. [Google Scholar] [CrossRef] [PubMed]
- Tahmaseb, A.; Wu, V.; Wismeijer, D.; Coucke, W.; Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 416–435. [Google Scholar] [CrossRef] [PubMed]
- Hultin, M.; Svensson, K.G.; Trulsson, M. Clinical advantages of computer-guided implant placement: A systematic review. Clin. Oral Implant. Res. 2012, 23 (Suppl. 6), 124–135. [Google Scholar] [CrossRef]
- Vieira, D.M.; Sotto-Maior, B.S.; Barros, C.A.; Reis, E.S.; Francischone, C.E. Clinical accuracy of flapless computer-guided surgery for implant placement in edentulous arches. Int. J. Oral Maxillofac. Implant. 2013, 28, 1347–1351. [Google Scholar] [CrossRef]
- Silvestrini Biavati, A.; Tecco, S.; Migliorati, M.; Festa, F.; Panza, G.; Marzo, G.; Gherlone, E.; Tetè, S. Three-dimensional tomographic mapping related to primary stability and structural miniscrew characteristics. Orthod. Craniofac Res. 2011, 14, 88–99, Erratum in Orthod. Craniofac. Res. 2016, 19, 234. [Google Scholar] [CrossRef] [PubMed]
- Colombo, M.; Mangano, C.; Mijiritsky, E.; Krebs, M.; Hauschild, U.; Fortin, T. Clinical applications and effectiveness of guided implant surgery: A critical review based on randomized controlled trials. BMC Oral Health 2017, 17, 150. [Google Scholar] [CrossRef]
- Song, S.J.; Tao, G.; Shariff, J.; Tarnow, D.P.; Bittner, N. Evaluation of Dimensional Changes and Ridge Contour Around Ovate Pontics Inserted Immediately after Extraction with Alveolar Ridge Preservation in the Esthetic Zone. Int. J. Periodontics Restor. Dent. 2022, 42, 83–91. [Google Scholar] [CrossRef]
- Summers, R.B. A new concept in maxillary implant surgery: The osteotome Technique. Compendium 1994, 15, 152–154. [Google Scholar]
- Spinato, S.; Bernardello, F.; Lombardi, T.; Soardi, C.M.; Messina, M.; Zaffe, D.; Stacchi, C. Influence of apico-coronal positioning of tissue-level implants on marginal bone stability during supracrestal tissue height establishment: A multi-center prospective study. Clin. Implant. Dent. Relat. Res. 2022, 24, 611–620. [Google Scholar] [CrossRef] [PubMed]
- Preiskel Hw Tsolka, P. Treatment outcomes in implant therapy: The influence of surgical and prosthodontic experience. Int. J. Prosthodont. 1995, 8, 273–279. [Google Scholar]
- Lambert, P.M.; Morris, H.F.; Ochi, S. Positive effect of surgical experience with implants on second stage implant survival. J. Oral Maxillofac. Surg. 1997, 55 (Suppl. S5), 12–18. [Google Scholar] [CrossRef] [PubMed]
- Davidowitz, G.; Kotick, P.G. The use of CAD/CAM in dentistry. Dent. Clin. N. Am. 2011, 55, 559–570. [Google Scholar] [CrossRef] [PubMed]
- Nota, A.; Chegodaeva, A.D.; Ryakhovsky, A.N.; Vykhodtseva, M.A.; Pittari, L.; Tecco, S. One-Stage Virtual Plan of a Complex Orthodontic/Prosthetic Dental Rehabilitation. Int. J. Environ. Res. Public. Health 2022, 19, 1474. [Google Scholar] [CrossRef]
- Marchetti, E.; Ratta, S.; Mummolo, S.; Tecco, S.; Pecci, R.; Bedini, R.; Marzo, G. Mechanical Reliability Evaluation of an Oral Implant-Abutment System According to UNI EN ISO 14801 Fatigue Test Protocol. Implant Dent. 2016, 25, 613–618. [Google Scholar] [CrossRef]
- Marchetti, E.; Ratta, S.; Mummolo, S.; Tecco, S.; Pecci, R.; Bedini, R.; Marzo, G. Evaluation of an endosseous oral implant system according to UNI EN ISO 14801 fatigue test protocol. Implant Dent. 2014, 23, 665–671. [Google Scholar] [CrossRef]
- Kaufman, Z.; Paranhos, K.S. Digitally Designed Ovate Pontic as a Predictable Procedure to Improve Accuracy, Hygiene, Esthetics. Compend. Contin. Educ. Dent. 2022, 43, 226–230. [Google Scholar]
- Tecco, S.; Grusovin, M.G.; Sciara, S.; Bova, F.; Pantaleo, G.; Capparé, P. The association between three attitude-related indexes of oral hygiene and secondary implant failures: A retrospective longitudinal study. Int. J. Dent. Hyg. 2018, 16, 372–379. [Google Scholar] [CrossRef]
- Hama, D.R.; Mahmood, B.J. Comparison of accuracy between free-hand and surgical guide implant placement among experienced and non-experienced dental implant practitioners: An in vitro study. J. Periodontal Implant. Sci. 2023, 53, 388–401. [Google Scholar] [CrossRef]
- Fugazzotto, P.A. Immediate implant placement following a modified trephine: Osteotome approach- success rates of 116 implants to 4 years in function. Int. J. Oral Maxillofac. Implants 2002, 17, 113–120. [Google Scholar] [PubMed]
- Tan, W.C.; Lang, N.P.; Zwahlen, M.; Pjetursson, B.E. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. Part II: Transalveolar technique. J. Clin. Periodontol. 2008, 35 (Suppl. S8), 241–254. [Google Scholar] [CrossRef]
- Esposito, M.; Grusovin, M.G.; Rees, J.; Karasoulos, D.; Felice, P.; Alissa, R.; Worthington, H.; Coulthard, P. Effectiveness of sinus lift procedures for dental implant rehabilitation: A Cochrane systematic review. Eur. J. Oral Implantol. 2010, 3, 7–26. [Google Scholar]
- Tatum, H. Maxillary and sinus implant reconstructions. Dent. Clin. N. Am. 1986, 30, 207–229. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Lang, N.P. Sinus floor elevation utilizing the transalveolar approach. Periodontology 2000 2014, 66, 59–71. [Google Scholar] [CrossRef] [PubMed]
- Stacchi, C.; Troiano, G.; Rapani, A.; Lombardi, T.; Sentineri, R.; Speroni, S.; Berton, F.; Di Lenarda, R. Factors influencing the prevalence of peri-implantitis in implants inserted in augmented maxillary sinuses: A multicenter cross-sectional study. J. Periodontol. 2021, 92, 1117–1125. [Google Scholar] [CrossRef]
- Hao, X.H.; Ye, H.; Zhai, Q.K. The relationships between different surgical approaches for maxillary sinus augmentation and implant failure and complications: A retrospective cohort study. Shanghai Kou Qiang Yi Xue 2021, 30, 214–218. (In Chinese) [Google Scholar]
- Lee, J.W.; Yoo, J.Y.; Paek, S.J.; Park, W.-J.; Choi, E.J.; Choi, M.-G.; Kwon, K.-H. Correlations between anatomic variations of maxillary sinus ostium and postoperative complication after sinus lifting. J. Korean Assoc. Oral Maxillofac. Surg. 2016, 42, 278–283. [Google Scholar] [CrossRef]
- Lin, C.-C.; Wu, C.-Z.; Huang, M.-S.; Huang, C.-F.; Cheng, H.-C.; Wang, D.P. Fully Digital Workflow for Planning Static Guided Implant Surgery: A Prospective Accuracy Study. J. Clin. Med. 2020, 9, 980. [Google Scholar] [CrossRef]
- Flügge, T.; Kramer, J.; Nelson, K.; Nahles, S.; Kernen, F. Digital implantology—A review of virtual planning software for guided implant surgery. Part II: Prosthetic set-up and virtual implant planning. BMC Oral Health 2022, 22, 23. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Speroni, S.; Bosco, F.; Ferrini, F.; Pittari, L.; Nota, A.; Tecco, S. The Use of a Surgical Template for the Insertion of Dental Implants and Sinus Lift with the Summers Technique Based on Digital Planning: A Case Report. Prosthesis 2024, 6, 206-215. https://doi.org/10.3390/prosthesis6010016
Speroni S, Bosco F, Ferrini F, Pittari L, Nota A, Tecco S. The Use of a Surgical Template for the Insertion of Dental Implants and Sinus Lift with the Summers Technique Based on Digital Planning: A Case Report. Prosthesis. 2024; 6(1):206-215. https://doi.org/10.3390/prosthesis6010016
Chicago/Turabian StyleSperoni, Stefano, Floriana Bosco, Francesco Ferrini, Laura Pittari, Alessandro Nota, and Simona Tecco. 2024. "The Use of a Surgical Template for the Insertion of Dental Implants and Sinus Lift with the Summers Technique Based on Digital Planning: A Case Report" Prosthesis 6, no. 1: 206-215. https://doi.org/10.3390/prosthesis6010016
APA StyleSperoni, S., Bosco, F., Ferrini, F., Pittari, L., Nota, A., & Tecco, S. (2024). The Use of a Surgical Template for the Insertion of Dental Implants and Sinus Lift with the Summers Technique Based on Digital Planning: A Case Report. Prosthesis, 6(1), 206-215. https://doi.org/10.3390/prosthesis6010016








