Abstract
The biological factors of dental implants have a significant impact on long-term prognosis. In the cement-retained type or screw cement-retained type prosthesis (SCRP) implants, dental luting cement is used between the abutment and the implant fixture. Residual excess cement remaining around the implant and gingiva is one of the major causes of peri-implantitis, which is the most common cause of late implant failure. The TDP implant prosthetic system is a new cementless screw-retained type prosthetic system, which overcomes the limitations of the conventional implant prosthetic systems. Using this system, not only serves to prevent peri-implantitis caused by residual excess cement, but also the risk of screw loosening and fracture is reduced due to the stress distribution through the substructure (link), which is connected to the zirconia crown via frictional force. In this case report, two patients with tooth defects visited our dental hospital for implant treatment. Both patients were treated using the TDP implant prosthetic system. As a result, functional and esthetically excellent implant prostheses were fabricated and delivered to the patients. On the 3-year follow-up examination, both patients showed successful results, respectively.
1. Introduction
Many studies have shown successful dental implant osseointegration thanks to the development of implant technology in dentistry. The success rate of implant osseointegration has significantly increased due to improved implant surface treatment technology [1,2,3]. However, not only do dental implant osseointegration and prosthetic factors influence the long-term success of implants, but also biological factors can too [4,5].
Biological factors that influence the failure of oral implants include the patient’s general condition, smoking, oral hygiene, bone quality, bone graft, parafunctions, bacterial contamination, implant related factors(material, surface properties, design), and prosthodontic factors (occlusal force, type of prosthesis, opposite dentition) [6,7]. Among these, the most common cause of late implant failure is peri-implantitis. Residual excess cement remaining around the implant gingival cuff during the cementation of the implant prostheses is one of the major causes of peri-implantitis [8].
The type of implant prosthesis can be largely divided into two types: a screw-retained type and cement-retained type (and conometric retention system), both of which have differing connection methods [9,10]. In the screw-retained type prosthesis, the prosthesis is connected to the implant fixture or abutment using abutment screws. The advantages of this type of prosthesis include the retrievability of implant prosthesis and a diminished risk of gingival inflammatory reaction caused by residual excess cement residue [11,12].
In the cement-retained type prosthesis, the abutment is firstly connected to the implant fixture via the abutment screw and the prosthesis is adhered by using dental luting cement [13,14]. Cement-type prostheses show a low risk of misfit, which can be a concern in screw-retained prostheses. Moreover, the absence of occlusal screw holes helps develop ideal occlusion with a low risk of partial fracture of the ceramic crown [15]. However, the residual excess cement caused by the cementation of the abutment and crown and improper cleaning of the abutments may cause peri-implantitis [5,11,12,13,14].
Therefore, screw cement-retained type prosthesis (SCRP) was developed to overcome this shortcoming of cement-retained type prosthesis. SCRP enables the removal of residual excess cement by loosening the abutment screw to remove the abutment with the prosthesis. However, the drawbacks of the SCRP include long chair time and complicated procedures for prosthesis cementation. Moreover, one cannot remove implant prosthesis after cementation if they have multiple implants with a large difference in the placement angle between the implants; therefore, the remaining cement requires removal to take place inside the oral cavity [13,14,16].
The TDP implant prosthetic system (Toplan Co., Seoul, Republic of Korea) is a new-generation cementless screw-retained type prosthetic system that overcomes the limitations of conventional implant prosthetic systems. First, since this system is cementless, peri-implant mucositis or peri-implantitis caused by residual excess cement around implants can be prevented. In addition, external stress can be effectively dispersed due to the presence of a prefabricated substructure (link) connected to the zirconia crown. As a result, the risk of screw loosening or screw fracture due to stress concentration is reduced, and this was a major problem of conventional screw-retained type prostheses.
In this case report, two patients were treated with implant prosthesis using the TDP implant prosthetic system. The purpose of this case report is to demonstrate the workflow of this implant prosthetic system and describe how the 3-year follow-up examination of these two patients showed successful results.
2. Case 1
A 78-year-old female patient visited the dental clinic of Daegu Catholic University Medical Center, complaining about a loss of the mandibular left first molar (Figure 1A). The patient had a medical history of hypertension, but she was not taking any medications which needed to be discontinued during the implant procedure. The patient was a non-smoker. For the treatment of choice, it was decided to restore a single implant prosthetic restoration. As a surgical method, flap surgery was planned for bone grafting and implant placement. After the intraoral and radiological examination of the patient, scaling was performed prior to implant placement. The patient received the same pharmacologic protocol of prophylactic oral antibiotics. Amoxicillin sodium (Augmentin; Ilsung pharmaceutical, Seoul, Republic of Korea) with a dosage of 500 mg was to be taken 3 times a day and prescribed routinely, from 1 day before the procedure to 7 days after the procedure. Then, a 4.5 × 10.0 mm implant (AR fixture; Biotem, Seongnam, Republic of Korea) was placed (Figure 1B) with a good initial fixation torque of 40 N/cm2 at placement. After a sufficient healing period of 3 months, the patient received the implant prosthesis.
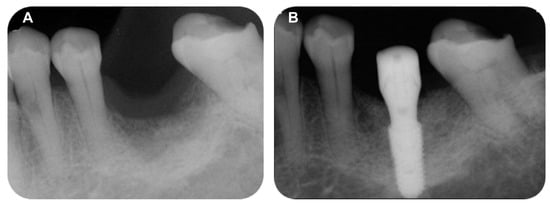
Figure 1.
(A) Pre-operative intraoral periapical radiograph, (B) Post-operative intraoral periapical radiograph.
The multi-abutment (Toplan Co., Seoul, Republic of Korea) was connected to the osseointegrated implant fixture. The height of the multi-abutment was determined using a gingival gauge (Figure 2A), and then the multi-abutment was tightened with a torque of 35 N/cm2 (Figure 2B).
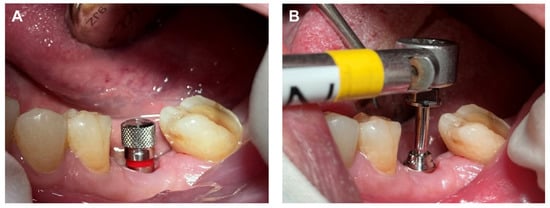
Figure 2.
(A) Multi-abutment height determination with gingival gauge, (B) Multi-abutment connection.
Next, a healing cap was connected to the multi-abutment (Figure 3A). The healing cap served as a normal healing abutment and an impression coping, intended for impression taking through recognition points on the occlusal surface, was also placed. The final impressions were taken using an addition-type silicone impression material (Aquasil LV and XLV; Dentsply Sirona, Milford, DE, USA). In a dental laboratory, the master model obtained from the impression was model-scanned, and the scan data was sent to a computer-aided design (CAD) software program (Trios II; 3Shape, Copenhagen, Denmark) (Figure 3B).
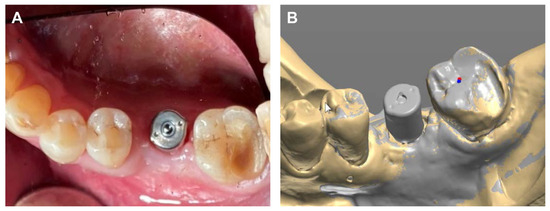
Figure 3.
(A) Healing cap connection, (B) Model scan data.
The final prosthesis was designed on a CAD software program through using the scanned information (Figure 4). The prefabricated link with appropriate height and diameter was selected considering the positional relationship between the implant and adjacent teeth and opposing teeth.
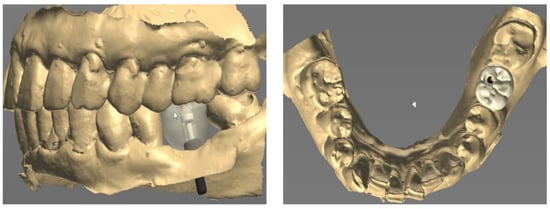
Figure 4.
Prosthetic design of implant prosthesis on CAD software program.
The zirconia crown was fabricated with a zirconia block using a computer-aided manufacturing (CAM) milling machine (Figure 5A). A prefabricated substructure (link) (Toplan Co., Seoul, Republic of Korea) was fitted to the final prosthesis through frictional force (Figure 5B). The space for the link was provided in the inner space of the zirconia crown in advance of the CAD software program through using the digital library data to facilitate the precise connection between the link and the zirconia crown.
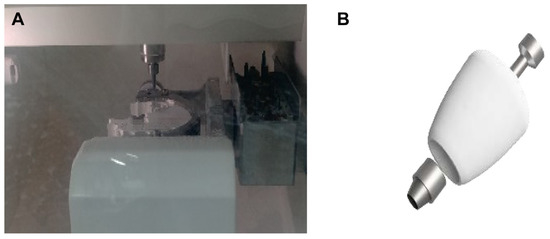
Figure 5.
(A) Milling procedure of final prosthesis, (B) Connection of link and zirconia crown.
The final prosthesis was connected to the multi-abutment through the abutment screw in the oral cavity of the patient. After the intraoral adjustment, the prosthesis was connected to the implant through using an abutment screw with a torque of 25 N/cm2. The screw access hole was sealed using Teflon tape and composite resin (Gradia Direct A3, GC, Tokyo, Japan) to complete the procedure (Figure 6A), and the accuracy of the connection of the implant prosthesis was confirmed through a periapical radiograph (Figure 6B).
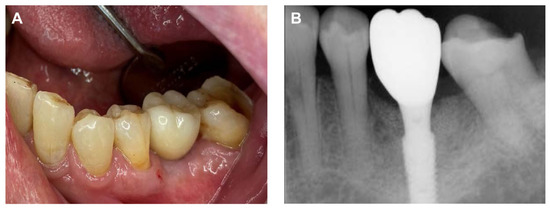
Figure 6.
Final delivery of implant prosthesis. (A) Intraoral photograph, (B) Periapical radiograph.
As part of a maintenance therapy program for the patient, a follow-up examination was performed every 6 months and the patient underwent dental plaque control. Additional periodontal treatment was performed when necessary in additional appointments. In addition, panoramic radiographs were taken every year to evaluate the prognosis of the implant. A 3-year follow-up examination showed successful maintenance of the implant prosthesis in the oral cavity (Figure 7).
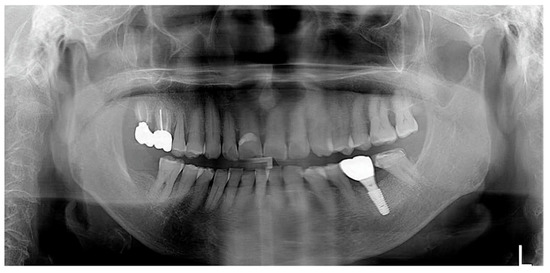
Figure 7.
Panoramic radiograph after 3 years of delivery.
3. Case 2
A 69-year-old female patient visited the dental clinic of Daegu Catholic University Medical Center to restore a missing mandibular left first molar and second molar (Figure 8A). The patient had a medical history of mild diabetes and hypertension, but she was not taking any medications which needed to be discontinued during the implant procedure. The patient was a non-smoker. Through consultation with the patient, it was decided that two implants would be placed. As a surgical method, flap operation was planned for vertical and horizontal bone grafting and implant placement. After the intraoral and radiological examination of the patient, scaling was performed before implant placement. The patient received the same pharmacologic protocol of the patient of case 1. A 4.5 × 10.0 mm and a 5.0 × 8.5 mm implant (AR fixture; Biotem, Seongnam, Republic of Korea) were placed, respectively (Figure 8B). Each implant was placed with the proper initial fixation torque of 30 N/cm2. After a sufficient healing period of 3 months, it was decided the prosthetic treatment procedure would commence.
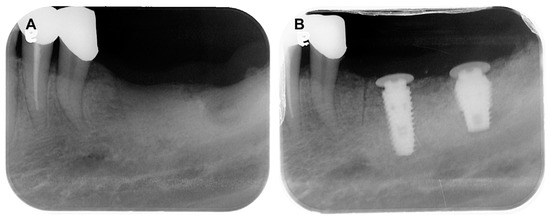
Figure 8.
(A) Pre-operative intraoral periapical radiograph, (B) Post-operative intraoral periapical radiograph.
After the height of the multi-abutments with gingival gauge was determined, the multi-abutments were connected to the osseointegrated implant fixture with a tightening torque of 35 N/cm2 (Figure 9A). Next, healing caps were connected to the multi-abutments (Figure 9B). The final impressions were taken using an addition-type silicone impression material (Aquasil LV and XLV; Dentsply Sirona, Milford, DE, USA).
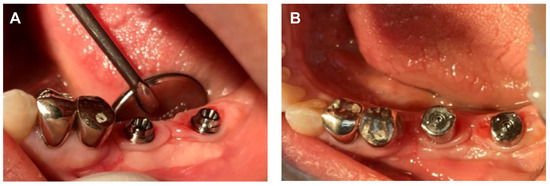
Figure 9.
(A) Multi-abutment connection, (B) Healing cap connection.
Next, the same laboratory process described in case 1 was performed. The prosthesis was designed on the CAD software, and a prefabricated link was selected through the scan data obtained from the model scan (Figure 10). A final prosthesis was obtained by milling zirconia through a CAM milling machine. A prefabricated substructure (link) (Toplan Co., Seoul, Republic of Korea) was fitted to the final prosthesis through frictional force.
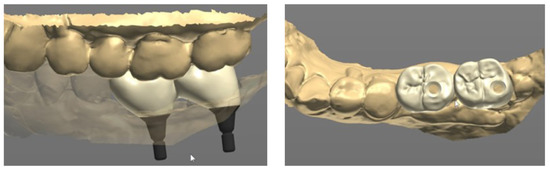
Figure 10.
Prosthetic design of implant prosthesis on CAD software program.
The final prosthesis was connected to the multi-abutments through the abutment screw in the oral cavity of the patient. After the intraoral adjustment, the prosthesis was connected to the implants through the abutment screw with a torque of 25 N/cm2. Teflon tape and composite resin were used to seal the screw access holes (Figure 11A) and the accurate connection of the implant prosthesis was evaluated through using a periapical radiograph (Figure 11B).
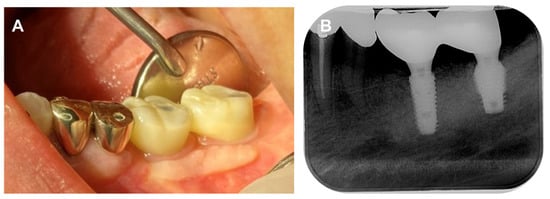
Figure 11.
Final delivery of implant prosthesis. (A) Intraoral photograph, (B) Periapical radiograph.
For this patient, the same periodontal maintenance protocol the patient received in case 1 was performed. Implant prosthesis was successfully maintained at the 3-year follow-up examination (Figure 12).

Figure 12.
Panoramic radiograph after 3 years of delivery.
4. Discussion
In this case report, patients with teeth defects visited our dental hospital for implant treatment and received an implant prostheses using the TDP implant prosthetic system. After 3 years of follow-up, satisfactory results were observed without any complications, respectively.
In this study, the final impression for the implant prosthesis was obtained by connecting the healing cap on the multi-abutment, and temporary prosthesis was not used. However, temporary prosthesis can also be fabricated in this prosthetic system. For this procedure, a temporary abutment is connected to the multi-abutment, and a temporary prosthesis can be manufactured by using model scan data obtained from a conventional impression. Similarly to the healing cap, the temporary abutment also has recognition points; therefore, using oral scanners is also possible. When a temporary prosthesis is used, it has the advantage of being able to secure the soft tissue volume and a proper cervical appearance angle for the final implant prosthesis.
The difference between this prosthetic system and the conventional screw-retained type prosthesis is the presence of a link. The screw-retained type prosthesis shows stress concentration on the lower part of the abutment with the application of an external load, resulting in screw loosening or fracture. However, we used a prosthetic system that enabled adequate stress distribution of externally applied loads due to the 360-degree cylindrical link, resulting in reduced prosthetic complications. The link should be properly fitted to the inner space of zirconia prosthesis to facilitate adequate frictional force. Three-dimensional library information regarding the structural link is provided from the manufacturer to the laboratory, and through this, the laboratory can precisely control the internal space of the zirconia prosthesis.
This prosthetic system also offers the following advantages. First, this prosthetic system enables a digital workflow. Because our dental hospital is not equipped with an oral scanner, conventional rubber impression of the healing cap was taken. However, by model scanning the master cast model, scan data was properly transferred to the CAD software program of the laboratory [17]. By using this scan data, final implant prosthesis is properly fabricated through the digital workflow and successfully delivered to the patients. If one’s dental office is equipped with an oral scanner, implant prosthetic procedures are further simplified. Since the healing cap connected with the multi-abutment has recognition points, the final implant prosthesis can be manufactured simply by scanning the healing cap and adjacent teeth with an oral scanner; therefore, chart time is shortened and patient discomfort is minimized. This digital workflow provides an advantage for the long-term follow-up of patients. If implant prosthesis is used for a long time, prosthetic complications such as crown fracture may occur. If the conventional impression method was previously used, there is no choice but to perform impression taking to remake the implant prosthesis via connecting impression coping. However, as in this study, for prostheses that enable a digital workflow, scan data at the time of initial manufacture can be stored, so it is possible to use this scan data again to manufacture implant prostheses. Therefore, the patient will not experience any discomfort caused by taking a new impression. In addition, if a temporary implant prosthesis is printed using a 3D printer, the patient is less likely to suffer from discomfort during mastication, even during the period whereby the implant prosthesis is being manufactured [18].
Finally, a great advantage of this prosthetic system is that there is no need to separate the multi-abutment once it is connected to the implant fixture. In the conventional implant prosthetic system, to make a final impression for the fabrication of implant prosthesis, the healing abutment connected to the implant fixture should be removed and the impression coping is subsequently connected. At this time, the patient may feel pain or discomfort due to the gingival irritation that may occur when the gingiva is compressed during the tightening and loosening of implant components. Additionally, the conventional implant prosthetic system is inconvenient when it comes to taking periapical radiographs to evaluate the accuracy of the connection of impression coping to the implant fixture. On the other hand, in the TDP implant prosthetic system, the final impression is obtained by connecting the healing cap on the multi-abutment, so the patient’s discomfort is reduced and the chair time is shortened. In addition, unlike other systems, the multi-abutment is directly connected to the implant fixture instead of the healing abutment at the time of the implant’s second surgery, and it is not removed in the subsequent prosthetic process. Therefore, there is also a periodontal advantage obtained by the smooth seating of the multi-abutment on the inside of the gingiva [19].
This prosthetic system has several advantages and a few limitations. First, this system cannot be indicated for implant cases where the intermaxillary space is less than 6 mm. Since the multi-abutment and link are used in this system, if there is less than 6mm of intermaxillary space, the minimum space to seal the screw hole using Teflon tape and composite resin is insufficient. In such a situation, a good alternative would be to fabricate a conventional screw-retained type prosthesis, which has good retention even when the height of the abutment is less than 4 mm. In addition, this prosthetic system provides satisfactory results for implants when the inter-implant angle is less than 30 degrees. Therefore, conventional customized abutments are more suitable for higher values of inter-implant angles.
During the observation period of this case report, no complications were found in the implant prostheses. However, if we consider prosthetic problems that may occur later, there exists a risk of screw loosening or screw fracture, multi-abutment fracture, and zirconia prosthesis fracture. The problem related to the screw can be solved according to the conventional method, and if the multi-abutment is fractured, repair of the prosthesis can be completed simply by replacing the multi-abutment because it is a ready-made product. If the zirconia prosthesis is fractured, the prosthesis can be easily re-manufactured by applying the previously saved scan data of the patient into the CAD software program. However, if the adjacent teeth or opposing teeth are natural teeth, there will also be a possibility of tooth movement or wear over time. Therefore, if a prosthesis needs to be remade, a dental clinician can evaluate and compare the previously existing scan data with the present oral condition. If changes in oral conditions are observed, it may be necessary to take a new impression by connecting a healing cap to the multi-abutment.
In future studies, a finite element analysis on whether this prosthetic system actually exhibits effective stress distribution should be performed, and the prognosis of implant prosthetics should also be observed and evaluated through longer-term follow-up examinations.
5. Conclusions
This clinical case report describes use of the TDP implant prosthetic system, which is a new cementless screw-retained type implant system. The difference between the TDP implant prosthetic system and conventional implant prosthetic system is that it uses a pre-fabricated multi-abutment and link, which play an important role in stress distribution. Two patients who needed implant treatment were aided by implant prostheses made through the use of the TDP implant prosthetic system. As a result, functional and esthetically excellent implant prostheses were fabricated, with successful results observed in the 3-year follow-up examination, respectively. Further follow-up examination is needed to evaluate the long-term prognosis for this implant prosthetic system.
Author Contributions
Conceptualization: H.C. and M.-H.H.; methodology: H.C.; software: M.-H.H.; formal analysis: H.C.; investigation: H.C. and M.-H.H.; data curation: H.C.; writing—original draft preparation: H.C. and M.-H.H.; writing—review and editing: M.-H.H.; supervision: H.C.; funding acquisition: M.-H.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT), grant number (No. 2022R1F1A1066517). The APC was also funded by the National Research Foundation of Korea.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (IRB) of the Daegu Catholic University Medical Center (IRB No.: CR-23-016).
Informed Consent Statement
Written informed consent was obtained for the publication of this case report and accompanying images.
Data Availability Statement
No new data were created or analyzed in this study.
Acknowledgments
The authors thank the F & E dental LAB, Daegu, for fabricating the prosthetic artifact.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Krennmair, G.; Schmidinger, S.; Waldenberger, O. Single-tooth replacement with the Frialit-2 system: A retrospective clinical analysis of 146 implants. Int. J. Oral. Maxillofac. Implant. 2002, 17, 78–85. [Google Scholar]
- Romeo, E.; Lops, D.; Margutti, E.; Ghisolfi, M.; Chiapasco, M.; Vogel, G. Long-term survival and success of oral implants in the treatment of full and partial arches: A 7-year prospective study with the ITI dental implant system. Int. J. Oral. Maxillofac. Implant. 2004, 19, 247–259. [Google Scholar]
- Yaman, F.; Ağaçayak, S.; Atilgan, S.; Benlidayi, E.; Ucan, M.C.; Erol, B.; Kaya, B.; Gunay, A.; Guven, S. Effects of systemic zoledronic acid administration on osseointegration of hydroxyapatite-coated and resorbable blast material surface implants in rabbit models. Int. J. Oral. Maxillofac. Implant. 2012, 27, 1443–1447. [Google Scholar]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.L. Peri-implantitis. J. Periodontol. 2018, 89 (Suppl. S1), S267–S290. [Google Scholar] [CrossRef] [PubMed]
- Fabbri, G.; Sorrentino, R. A biologically driven concept to design the emergence profile around dental implants: Surgical and prosthetic considerations to optimize hard and soft tissue integration. Int. J. Periodont. Restor. Dent. 2021, 41, 913–921. [Google Scholar] [CrossRef] [PubMed]
- Pesce, P.; Menini, M.; Tealdo, T.; Bevilacqua, M.; Pera, F.; Pera, P. Peri-implantitis: A systematic review of recently published papers. Int. J. Prosthodont. 2014, 27, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Pesce, P.; Canullo, L.; Grusovin, M.G.; de Bruyn, H.; Cosyn, J.; Pera, P. Systematic review of some prosthetic risk factors for periimplantitis. J. Prosthet. Dent. 2015, 114, 346–350. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Hirsch, J.M.; Lekholm, U.; Thomsen, P. Biological factors contributing to failures of osseointegrated oral implants. (II). Etiopathogenesis. Eur. J. Oral. Sci. 1998, 106, 721–764. [Google Scholar] [CrossRef] [PubMed]
- Wittneben, J.G.; Joda, T.; Weber, H.P.; Brägger, U. Screw retained vs cement retained implant-supported fixed dental prosthesis. Periodontol. 2000 2017, 73, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Bressan, E.; Venezze, A.C.; Magaz, V.R.; Lops, D.; Ghensi, P. Fixed conometric retention with CAD/CAM conic coupling abutments and prefabricated syncone caps: A case series. Int. J. Periodont. Restor. Dent. 2018, 38, 277–280. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.G., Jr. The positive relationship between excess cement and peri-implant disease: A prospective clinical endoscopic study. J. Periodontol. 2009, 80, 1388–1392. [Google Scholar] [CrossRef] [PubMed]
- Linkevicius, T.; Puisys, A.; Vindasiute, E.; Linkeviciene, L.; Apse, P. Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective case analysis. Clin. Oral. Implant. Res. 2013, 24, 1179–1184. [Google Scholar] [CrossRef] [PubMed]
- Rajan, M.; Gunaseelan, R. Fabrication of a cement- and screw-retained implant prosthesis. J. Prosthet. Dent. 2004, 92, 578–580. [Google Scholar] [CrossRef] [PubMed]
- Valbao, F.P.B., Jr.; Perez, E.G.; Breda, M. Alternative method for retention and removal of cement-retained implant prostheses. J. Prosthet. Dent. 2001, 86, 181–183. [Google Scholar] [CrossRef] [PubMed]
- Sorrentino, R.; Ruggiero, G.; Toska, E.; Leone, R.; Zarone, F. Clinical evaluation of cement-retained implant-supported CAD/CAM monolithic zirconia single crowns in posterior areas: Results of a 6-year prospective clinical study. Prosthesis 2022, 4, 383–393. [Google Scholar] [CrossRef]
- Linkevicius, T.; Vindasiute, E.; Puisys, A.; Peciuliene, V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin. Oral. Implant. Res. 2011, 22, 1379–1384. [Google Scholar] [CrossRef] [PubMed]
- Petre, A.E.; Drafta, S.; Oancea, L. Extraoral scanning of implant prosthetic components under difficult conditions using a transfer device. Appl. Sci. 2022, 12, 5912. [Google Scholar] [CrossRef]
- Lee, H.; Park, S.; Kwon, K.R.; Noh, G. Effects of cementless fixation of implant prosthesis: A finite element study. J. Adv. Prosthodont. 2019, 11, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Alves, C.C.; Muñoz, F.; Cantalapiedra, A.; Ramos, I.; Neves, M.; Blanco, J. Marginal bone and soft tissue behavior following platform switching abutment connection/disconnection--a dog model study. Clin. Oral. Implant. Res. 2015, 26, 983–991. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).