Removable Partial Denture Frameworks in the Age of Digital Dentistry: A Review of the Literature
Abstract
:1. Introduction
2. Methods
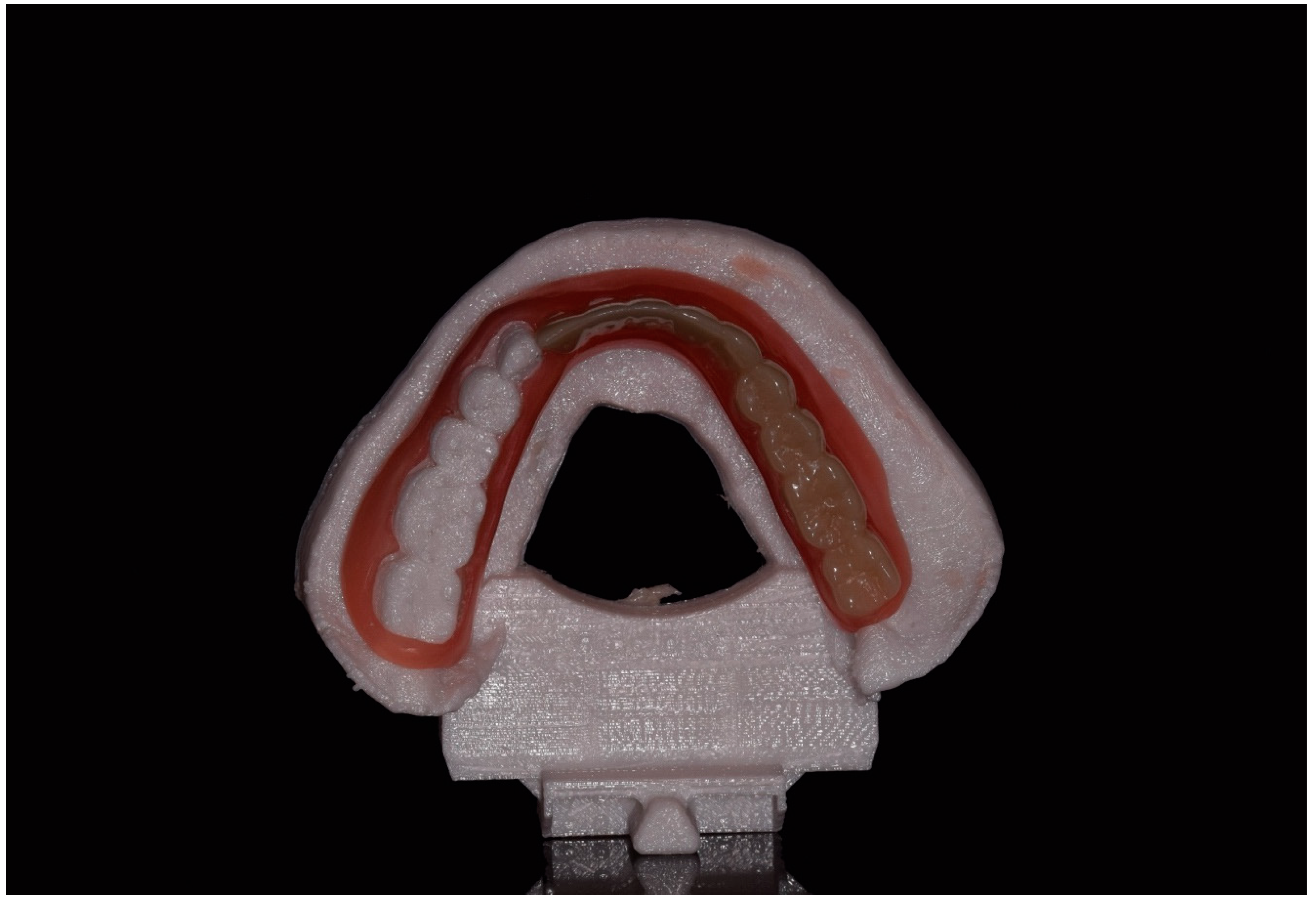
3. The Digital Manufacturing Process
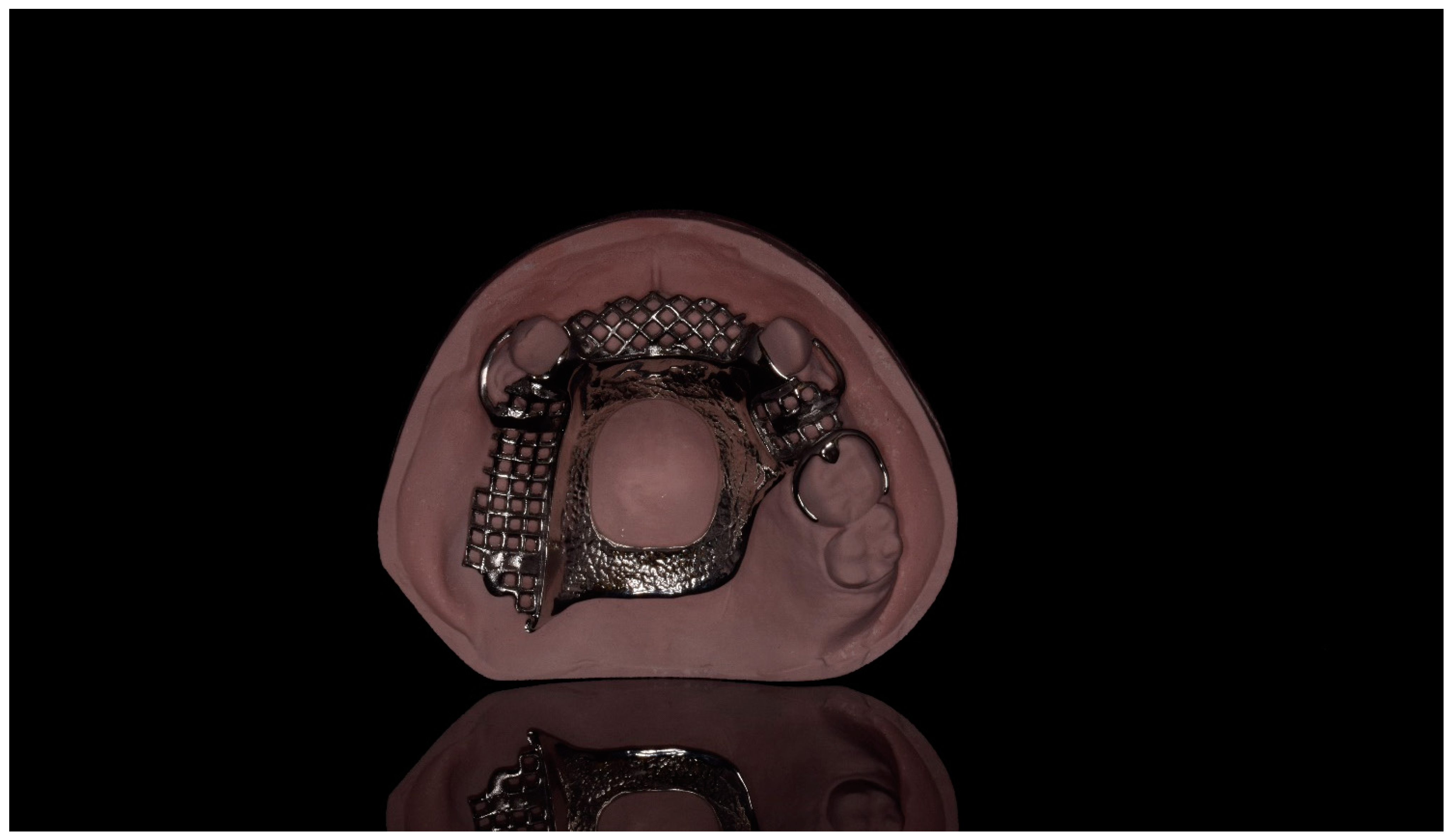
3.1. Milled Frameworks
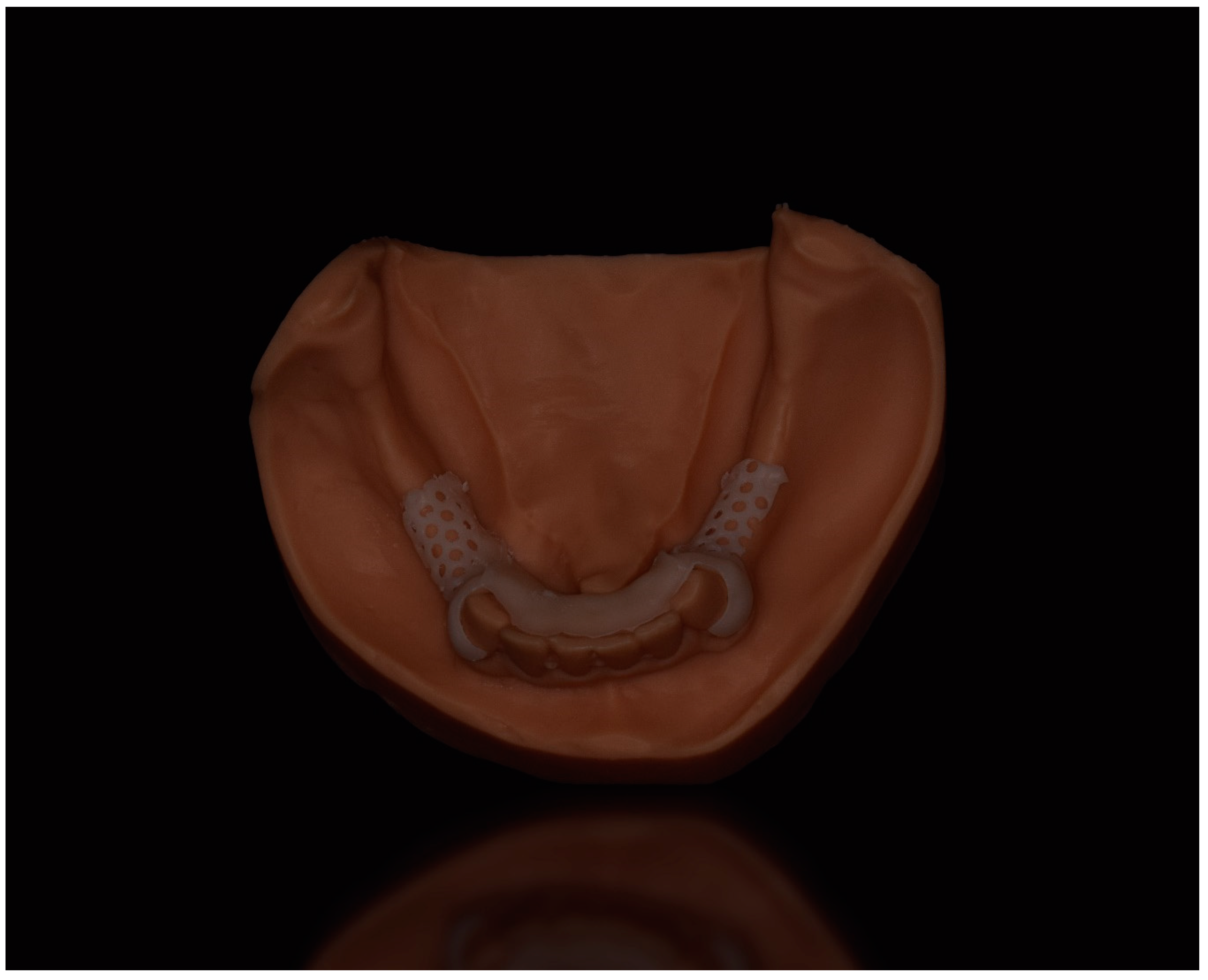
3.2. 3D Printed Frameworks
4. Digital Frameworks: Common Materials and Properties
4.1. Cobalt Chromium
4.2. Titanium
4.3. Polyoxymethylene (POM)
4.4. Polyamide
4.5. Polyaryletherketone Polymers (PAEK)
4.6. Aryl Ketone Polymers (AKP)
4.7. Polyetheretherketone (PEEK)
5. Considerations and Limitations
5.1. Design Principles and Guidelines
5.2. Rigidity of the Major Connector
5.3. Repair and Bonding
5.4. Clinical Studies and Long-Term Follow-Up
6. Conclusions
- While promising, clinical studies on additively manufactured titanium frameworks are required to determine their overall fit, function, and impact on supporting abutment teeth.
- Clasp arms made from thermoplastic polymers require additional bulk to serve as retainers.
- The inherent flexibility of novel polymers limits their use as major connectors, minor connectors, and rest seats.
- Removable partial dentures made from novel polymers are difficult to reline and repair.
- Currently, removable partial dentures made from thermoplastic polymers are best used as interim prostheses as long-term evidence of their function is lacking.
- Future improvements in high performance polymers and digital manufacturing methods may help to address the need of the growing partially edentulous population.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Seraj, Z.; Al-Najjar, D.; Akl, M.; Aladle, N.; Altijani, Y.; Zaki, A.; Al Kawas, S. The effect of number of teeth and chewing ability on cognitive function of elderly in UAE: A pilot study. Int. J. Dent. 2017, 2017, 5732748. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.D.; Turkyilmaz, I.; Garcia, L.T. Removable partial dentures—Treatment now and for the future. Tex. Dent. J. 2010, 127, 365–372. [Google Scholar] [PubMed]
- Dye, B.A.; Thornton-Evans, G.; Li, X.; Iafolla, T. Dental Caries and Tooth Loss in Adults in the United States, 2011–2012; NCHS data brief; National Center for Health Statistics: Hyattsville, MD, USA, 2015; Volume 197. [Google Scholar]
- Fueki, K.; Ohkubo, C.; Yatabe, M.; Arakawa, I.; Arita, M.; Ino, S.; Kanamori, T.; Kawai, Y.; Kawara, M.; Komiyama, O.; et al. Clinical application of removable partial dentures using thermoplastic resin. Part II: Material properties and clinical features of non-metal clasp dentures. J. Prosthodont. Res. 2014, 58, 71–84. [Google Scholar] [CrossRef] [Green Version]
- Sheets, C.G. Modern dentistry and the esthetically aware patient. J. Am. Dent. Assoc. 1987, 115, 103E–105E. [Google Scholar] [CrossRef] [PubMed]
- Akl, M.A.; Mansour, D.E.; Mays, K.; Wee, A.G. Mathematical tooth proportions: A systematic review. J. Prosthodont. 2021, 31, 289–298. [Google Scholar] [CrossRef] [PubMed]
- de-Melo, J.F.; Gjerdet, N.R.; Erichsen, E.S. Metal release from cobalt-chromium partial dentures in the mouth. Acta Odontol. Scand. 1983, 41, 71–74. [Google Scholar] [CrossRef]
- Jabbari, Y.A. Physico-mechanical properties and prosthodontic applications of Co-Cr dental alloys: A review of the literature. J. Adv. Prosthodont. 2014, 6, 138–145. [Google Scholar] [CrossRef] [Green Version]
- Gay, W.D. Laboratory procedures for fitting removable partial denture frameworks. J. Prosthet. Dent. 1978, 40, 227–229. [Google Scholar] [CrossRef]
- Firtell, D.N.; Muncheryan, A.M.; Green, A.J. Laboratory accuracy in casting removable partial denture frameworks. J. Prosthet. Dent. 1985, 54, 856–862. [Google Scholar] [CrossRef]
- Earnshaw, R. The casting shrinkage of cobalt-chromium alloys. Aust. Dent. J. 1958, 3, 159–170. [Google Scholar] [CrossRef]
- Rudd, R.W.; Rudd, K.D. A review of 243 errors possible during the fabrication of a removable partial denture: Part I. J. Prosthet. Dent. 2001, 86, 251–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rudd, R.W.; Rudd, K.D. A review of 243 errors possible during the fabrication of a removable partial denture: Part II. J. Prosthet. Dent. 2001, 86, 262–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rudd, R.W.; Rudd, K.D. A review of 243 errors possible during the fabrication of a removable partial denture: Part III. J. Prosthet. Dent. 2001, 86, 277–288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beuer, D.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Turkyilmaz, I.; Wilkins, G.N. Milling machines in dentistry: A swiftly evolving technology. J. Craniofac. Surg. 2021, 32, 2259–2260. [Google Scholar] [CrossRef]
- Snosi, A.M.; Lotfy, S.M.; Thabet, Y.G.; Sabet, M.E.; Rizk, F.N. Subtractive versus additive indirect manufacturing techniques of digitally designed partial dentures. J. Adv. Prosthodont. 2021, 13, 327–332. [Google Scholar] [CrossRef]
- Arnold, C.; Hey, J.; Schweyen, R.; Setz, J.M. Accuracy of CAD-CAM-fabricated removable partial dentures. J. Prosthet. Dent. 2018, 119, 586–592. [Google Scholar] [CrossRef]
- Schweiger, J.; Edelhoff, D.; Güth, J.F. 3D printing in digital prosthetic dentistry: An overview of recent developments in additive manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef]
- Alifui-Segbaya, F.; Williams, R.J.; George, R. Additive manufacturing: A novel method for fabricating cobalt-chromium removable partial denture frameworks. Eur. J. Prosthodont. Restor. Dent. 2017, 25, 73–78. [Google Scholar]
- 3DRPD|Laser Sintered Partial Removable Dentures. Available online: http://www.3drpd.com (accessed on 13 February 2022).
- Goguta, L.; Lungeanu, D.; Negru, R.; Birdeanu, M.; Jivanescu, A.; Sinescu, C. Selective laser sintering versus selective laser melting and computer aided design-computer aided manufacturing in double crowns retention. J. Prosthodont. Res. 2021, 65, 371–378. [Google Scholar] [CrossRef]
- Suzuki, Y.; Shimizu, S.; Waki, T.; Shimpo, H.; Ohkubo, C. Laboratory efficiency of additive manufacturing for removable denture frameworks: A literature-based review. Dent. Mater. J. 2021, 40, 265–271. [Google Scholar] [CrossRef]
- Oh, K.C.; Yun, B.S.; Kim, J.H. Accuracy of metal 3D printed frameworks for removable partial dentures evaluated by digital superimposition. Dent. Mater. 2022, 38, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Muehlemann, E.; Özcan, M. Accuracy of removable partial denture frameworks fabricated using conventional and digital technologies. Eur. J. Prosthodont. Restor. Dent. 2021; Epub ahead of print. [Google Scholar] [CrossRef]
- Soltanzadeh, P.; Suprono, M.S.; Kattadiyil, M.T.; Goodacre, C.; Gregorius, W. An in vitro investigation of accuracy and fit of conventional and CAD/CAM removable partial denture frameworks. J. Prosthodont. 2019, 28, 547–555. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Abbasi, M.S.; Haider, S.; Ahmed, N.; Habib, S.R.; Altamash, S.; Zafar, M.S.; Alam, M.K. Fit accuracy of removable partial denture frameworks fabricated with CAD/CAM, rapid prototyping, and conventional techniques: A systematic review. BioMed Res. Int. 2021, 2021, 3194433. [Google Scholar] [CrossRef] [PubMed]
- Tasaka, A.; Okano, H.; Shimizu, T.; Kato, Y.; Higuchi, S.; Yamashita, S. Influence of reinforcement bar on accuracy of removable partial denture framework fabricated by casting with a 3D-printed pattern and selective laser sintering. J. Prosthodont. Res. 2021, 65, 213–218. [Google Scholar] [CrossRef]
- Tasaka, A.; Shimizu, T.; Kato, Y.; Okano, H.; Ida, Y.; Higuchi, S.; Yamashita, S. Accuracy of removable partial denture framework fabricated by casting with a 3D printed pattern and selective laser sintering. J. Prosthodont. Res. 2020, 64, 224–230. [Google Scholar] [CrossRef]
- Jang, K.S.; Youn, S.J.; Kim, Y.S. Comparison of castability and surface roughness of commercially pure titanium and cobalt-chromium denture frameworks. J. Prosthet. Dent. 2001, 86, 93–98. [Google Scholar] [CrossRef]
- Ohkubo, C.; Hanatani, S.; Hosoi, T. Present status of titanium removable dentures-a review of the literature. J. Oral Rehabil. 2008, 35, 706–714. [Google Scholar] [CrossRef]
- Black, J.; Hastings, G. Handbook of Biomaterial Properties; Chapman & Hall: London, UK, 1998; p. 186. [Google Scholar]
- Ohkubo, C.; Sato, Y.; Nishiyama, Y.; Suzuki, Y. Titanium removable denture based on a one-metal rehabilitation concept. Dent. Mater. J. 2017, 36, 517–523. [Google Scholar] [CrossRef] [Green Version]
- Ohkubo, C.; Watanabe, I.; Ford, J.P.; Nakajima, H.; Hosoi, T.; Okabe, T. The machinability of cast titanium and Ti-6Al-4V. Biomaterials 2000, 21, 421–428. [Google Scholar] [CrossRef]
- Ohkubo, C.; Hosoi, T.; Ford, J.P.; Watanabe, I. Effect of surface reaction layer on grindability of cast titanium alloys. Dent. Mater. 2006, 22, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Frazier, W.E. Metal additive manufacturing: A review. J. Mater. Eng. Perform. 2014, 23, 1917–1928. [Google Scholar] [CrossRef]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive technology: Update on current materials and applications in dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Tan, F.B.; Song, J.L.; Wang, C.; Fan, Y.-B.; Dai, H.-W. Titanium clasp fabricated by selective laser melting, CNC milling, and conventional casting: A comparative in vitro study. J. Prosthodont. Res. 2019, 63, 58–65. [Google Scholar] [CrossRef]
- Takahashi, K.; Torii, M.; Nakata, T.; Kawamura, N.; Shimpo, H.; Ohkubo, C. Fitness accuracy and retentive forces of additive manufactured titanium clasp. J. Prosthodont. Res. 2020, 64, 468–477. [Google Scholar] [CrossRef]
- de Delgado, M.M.; Garcia, L.T.; Rudd, K.D. Camouflaging partial denture clasps. J. Prosthet. Dent. 1986, 55, 656–660. [Google Scholar] [CrossRef]
- Fitton, J.S.; Davies, E.H.; Howlett, J.A.; Pearson, G. The physical properties of a polyacetal denture resin. Clin. Mater. 1994, 17, 125–129. [Google Scholar] [CrossRef]
- Ohlin, A.; Linder, L. Biocompatibility of polyoxymethylene (Delrin) in bone. Biomaterials 1993, 14, 285–289. [Google Scholar] [CrossRef]
- MacAfee, K.A.; Quinn, P.D. Total temporomandibular joint reconstruction with a Delrin titanium implant. J. Craniofac. Surg. 1992, 3, 160–169. [Google Scholar] [CrossRef]
- Smith, D.C. Recent developments and prospects in dental polymers. J. Prosthet. Dent. 1962, 12, 1066–1078. [Google Scholar] [CrossRef]
- Thomas, S.; Nandini, V. Acetal resin-A quantum leap in aesthetic restorative dentistry. Int. J. Clin. Dent. Sci. 2011, 2, 56–59. [Google Scholar]
- Ardelean, L.C.; Borțun, C.M.; Motoc, M. Metal-free removable partial dentures made of a thermoplastic acetal resin and two polyamide resins. J. Mater. Plast. 2007, 44, 345–348. [Google Scholar]
- Meenakshi, A.; Gupta, R.; Bharti, V.; Sriramaprabu, G.; Prabhakar, R. An evaluation of retentive ability and deformation of acetal resin and cobalt-chromium clasps. J. Clin. Diagn. Res. 2016, 10, ZC37–ZC41. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.C.; Latta, G.H., Jr.; Wicks, R.A.; Swords, R.L.; Scarbecz, M. In vitro deformation of acetyl resin and metal alloy removable partial denture direct retainers. J. Prosthet. Dent. 2003, 90, 586–590. [Google Scholar] [CrossRef]
- Turner, J.W.; Radford, D.R.; Sherriff, M. Flexural properties and surface finishing of acetal resin denture clasps. J. Prosthodont. 1999, 8, 188–195. [Google Scholar] [CrossRef]
- Al-Akhali, M.A.; El-Kerdawy, M.W.; Ibraheim, Z.A.; Abbas, N.A. Comparative study on the microbial adhesion to acetal resin and metallic removable partial denture. Indian J. Dent. 2012, 3, 1–4. [Google Scholar] [CrossRef]
- Vojdani, M.; Giti, R. Polyamide as a denture base material: A literature review. J. Dent. 2015, 16, 1–9. [Google Scholar]
- Watt, D.M. Clinical assessment of nylon as a partial denture base material. Br. Dent. J. 1955, 98, 238–244. [Google Scholar]
- Yunus, N.; Rashid, A.A.; Azmi, L.L.; Hassan, M.I.A. Some flexural properties of a nylon denture base polymer. J. Oral Rehabil. 2005, 32, 65–71. [Google Scholar] [CrossRef]
- Takabayashi, Y. Characteristics of denture thermoplastic resins for non-metal clasp dentures. Dent. Mater. 2010, 29, 353–361. [Google Scholar] [CrossRef] [Green Version]
- Ucar, Y.; Akova, T.; Aysan, I. Mechanical properties of polyamide versus different PMMA denture base materials. J. Prosthodont. 2012, 21, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Hamanaka, I.; Takahashi, Y.; Shimizu, H. Mechanical properties of injection-molded thermoplastic denture base resins. Acta Odontol. Scand. 2011, 69, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Wadachi, J.; Sato, M.; Igarashi, Y. Evaluation of the rigidity of dentures made of injection-molded materials. Dent. Mater. 2013, 32, 508–511. [Google Scholar] [CrossRef] [Green Version]
- Sepúlveda-Navarro, W.F.; Arana-Correa, B.E.; Borges, C.P.; Jorge, J.H.; Urban, V.M.; Campanha, N.H. Color stability of resins and nylon as denture base material in beverages. J. Prosthodont. 2011, 20, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Abuzar, M.A.; Bellur, S.; Duong, N.; Kim, B.B.; Lu, P.; Palfreyman, N.; Surendran, D.; Tran, V.T. Evaluating surface roughness of a poly-amide denture base material in comparison with poly (methyl methacrylate). J. Oral Sci. 2010, 52, 577–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawara, M.; Iwata, Y.; Iwasaki, M.; Komoda, Y.; Iida, T.; Asano, T.; Komiyama, O. Scratch test of thermoplastic denture base resins for non-metal clasp dentures. J. Prosthodont. Res. 2014, 58, 35–40. [Google Scholar] [CrossRef]
- Stafford, G.D.; Huggett, R.; MacGregor, A.R.; Graham, J. The use of nylon as a denture-base material. J. Dent. 1986, 14, 18–22. [Google Scholar] [CrossRef]
- Parvizi, A.; Lindquist, T.; Schneider, R.; Williamson, D.; Boyer, D.; Dawson, D.V. Comparison of the dimensional accuracy of injection-molded denture base materials to that of conventional pressure-pack acrylic resin. J. Prosthodont. 2004, 13, 83–89. [Google Scholar] [CrossRef]
- Audoit, J.; Rivière, L.; Dandurand, J.; Lonjon, A.; Dantras, E.; Lacabanne, C. Thermal, mechanical and dielectric behaviour of poly (aryl ether ketone) with low melting temperature. J. Therm. Anal. Calorim. 2019, 135, 2147–2157. [Google Scholar] [CrossRef] [Green Version]
- Kurtz, S.M. An Overview of PEEK Biomaterials. In PEEK Biomaterials Handbook, 2nd ed.; Kurtz, S.M., Ed.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 3–9. [Google Scholar] [CrossRef]
- Martin, C.; Purevdorj-Gage, L.; Li, W.; Shary, T.J.; Yang, B.; Murphy, R.J.; Wu, C.D. In vitro biofilm formation on aryl ketone polymer (AKP), a new denture material, compared with that on three traditional dental denture materials. Int. J. Dent. 2021, 2021, 4713510. [Google Scholar] [CrossRef]
- Marie, A.; Keeling, A.; Hyde, T.P.; Nattress, B.R.; Pavitt, S.; Murphy, R.J.; Shary, T.J.; Dillon, S.; Osnes, C.; Wood, D.J. Deformation and retentive force following in vitro cyclic fatigue of cobalt-chrome and aryl ketone polymer (AKP) clasps. Dent. Mater. 2019, 35, e113–e121. [Google Scholar] [CrossRef] [PubMed]
- Gentz, F.I.; Brooks, D.I.; Liacouras, P.C.; Petrich, A.; Hamlin, C.M.; Ellert, D.O.; Ye, L. Retentive forces of removable partial denture clasp assemblies made from polyaryletherketone and cobalt-chromium: A comparative study. J. Prosthodont. 2021; Epub ahead of print. [Google Scholar] [CrossRef]
- Ali, Z.; Baker, S.; Sereno, N.; Martin, N. A pilot randomized controlled crossover trial comparing early OHRQoL outcomes of cobalt-chromium versus PEEK removable partial denture Frameworks. Int. J. Prosthodont. 2020, 33, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Devine, J.N. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 2007, 28, 4845–4869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toth, J.M.; Wang, M.; Estes, B.T.; Scifert, J.L.; Seim, H.B.; Turner, A.S. Polyetheretherketone as a biomaterial for spinal applications. Biomaterials 2006, 27, 324–334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Siddiqui, F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J. Prosthodont. Res. 2016, 60, 12–19. [Google Scholar] [CrossRef]
- Peng, T.Y.; Ogawa, Y.; Akebono, H.; Iwaguro, S.; Sugeta, A.; Shimoe, S. Finite-element analysis and optimization of the mechanical properties of polyetheretherketone (PEEK) clasps for removable partial dentures. J. Prosthodont. Res. 2020, 64, 250–256. [Google Scholar] [CrossRef]
- Htun, P.L.; Kyaw, P.P.; Nyan, M.; Win, A.; Tint, K. Innovation of removable partial denture with esthetic clasp assembly: A case report. J. Clin. Dent. Relat. Res. 2020, 1, 1–5. [Google Scholar]
- Ichikawa, T.; Kurahashi, K.; Liu, L.; Matsuda, T.; Ishida, Y. Use of a polyetheretherketone clasp retainer for removable partial denture: A case report. Dent. J. 2019, 7, 4. [Google Scholar] [CrossRef] [Green Version]
- Chen, X.; Mao, B.; Zhu, Z.; Yu, J.; Lu, Y.; Zhang, Q.; Yue, L.; Yu, H. A three-dimensional finite element analysis of mechanical function for 4 removable partial denture designs with 3 framework materials: CoCr, Ti-6Al-4V alloy and PEEK. Sci. Rep. 2019, 9, 13975. [Google Scholar] [CrossRef] [Green Version]
- Lo Russo, L.; Chochlidakis, K.; Caradonna, G.; Molinelli, F.; Guida, L.; Ercoli, C. Removable partial dentures with polyetheretherketone framework: The influence on residual ridge stability. J. Prosthodont. 2021; Epub ahead of print. [Google Scholar] [CrossRef]
- Zoidis, P.; Papathanasiou, I.; Polyzois, G. The use of a modified poly-ether-ether-ketone (PEEK) as an alternative framework material for removable dental prostheses. A clinical report. J. Prosthodont. 2016, 25, 580–584. [Google Scholar] [CrossRef]
- Harb, I.E.; Abdel-Khalek, E.A.; Hegazy, S.A. CAD/CAM constructed poly(etheretherketone) (PEEK) framework of Kennedy class I removable partial denture: A clinical report. J. Prosthodont. 2019, 28, e595–e598. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.J. Revisiting the removable partial denture. Dent. Clin. N. Am. 2019, 63, 263–278. [Google Scholar] [CrossRef] [PubMed]
- Gray, D.; Barraclough, O.; Ali, Z.; Nattress, B. Modern partial dentures-part 2: A review of novel metal-free materials and innovations in polymers. Br. Dent. J. 2021, 230, 813–818. [Google Scholar] [CrossRef]
- Ben-Ur, Z.; Matalon, S.; Aviv, I.; Cardash, H. Rigidity of major connectors when subjected to bending and torsion forces. J. Prosthet. Dent. 1989, 62, 557–562. [Google Scholar] [CrossRef]
- Macura-Karbownik, A.; Chladek, G.; Żmudzki, J.; Kasperski, J. Chewing efficiency and occlusal forces in PMMA, acetal and polyamide removable partial denture wearers. Acta Bioeng. Biomech. 2016, 18, 137–144. [Google Scholar] [PubMed]
- Peng, T.Y.; Shimoe, S.; Fuh, L.J.; Lin, C.-K.; Lin, D.-J.; Kaku, M. Bonding and thermal cycling performances of two (poly)aryl-ether-ketone (PAEKs) materials to an acrylic denture base resin. Polymers 2021, 13, 543. [Google Scholar] [CrossRef]
- Fuhrmann, G.; Steiner, M.; Freitag-Wolf, S.; Kern, M. Resin bonding to three types of polyaryletherketones (PAEKs)-durability and influence of surface conditioning. Dent. Mater. 2014, 30, 357–363. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Taufall, S.; Roos, M.; Schmidlin, P.R.; Lümkemann, N. Bonding of composite resins to PEEK: The influence of adhesive systems and air- abrasion parameters. Clin. Oral Investig. 2018, 22, 763–771. [Google Scholar] [CrossRef]
- Lümkemann, N.; Strickstrock, M.; Eichberger, M.; Zylla, I.-M.; Stawarczyk, B. Impact of air-abrasion pressure and adhesive systems on bonding parameters for polyetheretherketone dental restorations. Int. J. Adhes. Adhes. 2018, 80, 30–38. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Keul, C.; Beuer, F.; Roos, M.; Schmidlin, P.R. Tensile bond strength of veneering resins to PEEK: Impact of different adhesives. Dent. Mater. 2013, 32, 441–448. [Google Scholar] [CrossRef] [Green Version]
- Rosentritt, M.; Preis, V.; Behr, M.; Sereno, N.; Kolbeck, C. Shear bond strength between veneering composite and PEEK after different surface modifications. Clin. Oral Investig. 2015, 19, 739–744. [Google Scholar] [CrossRef] [PubMed]
- Lümkemann, N.; Eichberger, M.; Stawarczyk, B. Bond strength between a high-performance thermoplastic and a veneering resin. J. Prosthet. Dent. 2020, 124, 790–797. [Google Scholar] [CrossRef] [PubMed]
- Muhsin, S.; Wood, D.; Johnson, A.; Hatton, P. Effects of novel Polyetheretherketone (PEEK) clasp design on retentive force at different tooth undercuts. J. Oral Dent. Res. 2018, 5, 13–25. [Google Scholar]
- Ziglam, A. The Effect of Removable Partial Denture Material and Design on Load Distribution over the Supporting Structures. Ph.D. Thesis, University of Sheffield, Sheffield, UK, 2017. [Google Scholar]





| Framework Material | Fabrication Method | Properties |
|---|---|---|
| Cobalt chromium | Conventional lost wax technique | High strength, heat resistance and light weight with favorable resistance to wear, corrosion, and staining. |
| Milled/3D printed castable patterns | ||
| SLS and SLM | ||
| Titanium | Conventional lost wax technique | Biocompatible, resistant to corrosion, ductile, light weight and high strength. |
| Milled/3D printed castable patterns | ||
| SLS and SLM | ||
| Acetal | Injection molding | Biocompatible, high wear resistance and impact strength, low thermal conductivity, and marked flexibility. |
| Milling | ||
| Polyamide | Injection molding | High strength and fracture resistance, heat resistance, stress deflection and significant flexibility. |
| 3D printing | ||
| PAEK (AKP) | Milling | High impact and flexural strength, resistance to water sorption and better resistance to microbial adhesion. |
| PEEK | Milling | Biocompatible, unreactive with other materials, wear resistant, and has a modulus of elasticity that is similar to dentin and bone. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akl, M.A.; Stendahl, C.G. Removable Partial Denture Frameworks in the Age of Digital Dentistry: A Review of the Literature. Prosthesis 2022, 4, 184-201. https://doi.org/10.3390/prosthesis4020019
Akl MA, Stendahl CG. Removable Partial Denture Frameworks in the Age of Digital Dentistry: A Review of the Literature. Prosthesis. 2022; 4(2):184-201. https://doi.org/10.3390/prosthesis4020019
Chicago/Turabian StyleAkl, Mohammed A., and Charles G. Stendahl. 2022. "Removable Partial Denture Frameworks in the Age of Digital Dentistry: A Review of the Literature" Prosthesis 4, no. 2: 184-201. https://doi.org/10.3390/prosthesis4020019
APA StyleAkl, M. A., & Stendahl, C. G. (2022). Removable Partial Denture Frameworks in the Age of Digital Dentistry: A Review of the Literature. Prosthesis, 4(2), 184-201. https://doi.org/10.3390/prosthesis4020019






