Full Digital Model-Free Maxillary Prosthetic Rehabilitation by Means of One-Piece Implants: A Proof of Concept Clinical Report with Three-Years Follow Up
Abstract
:1. Introduction
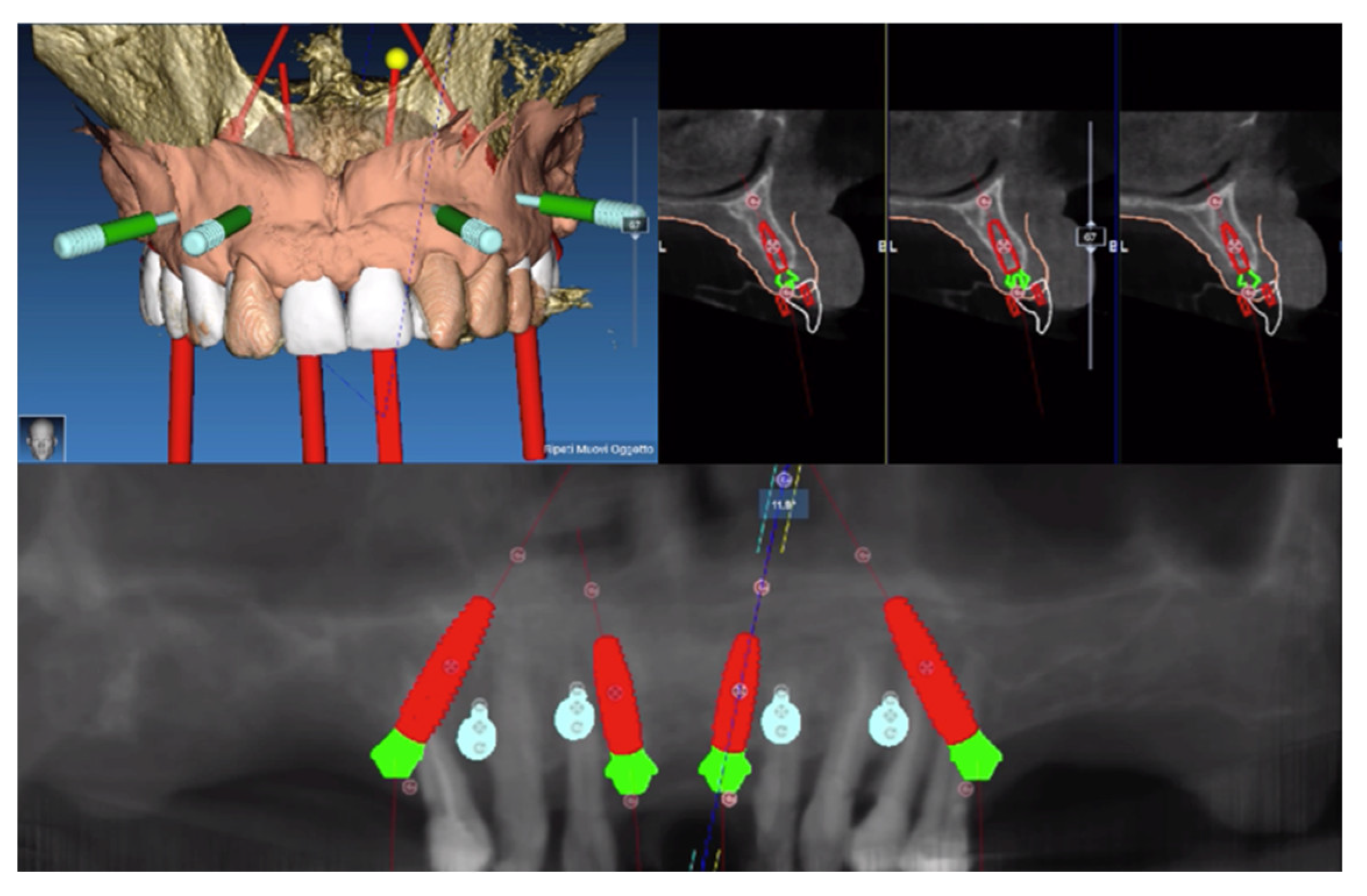
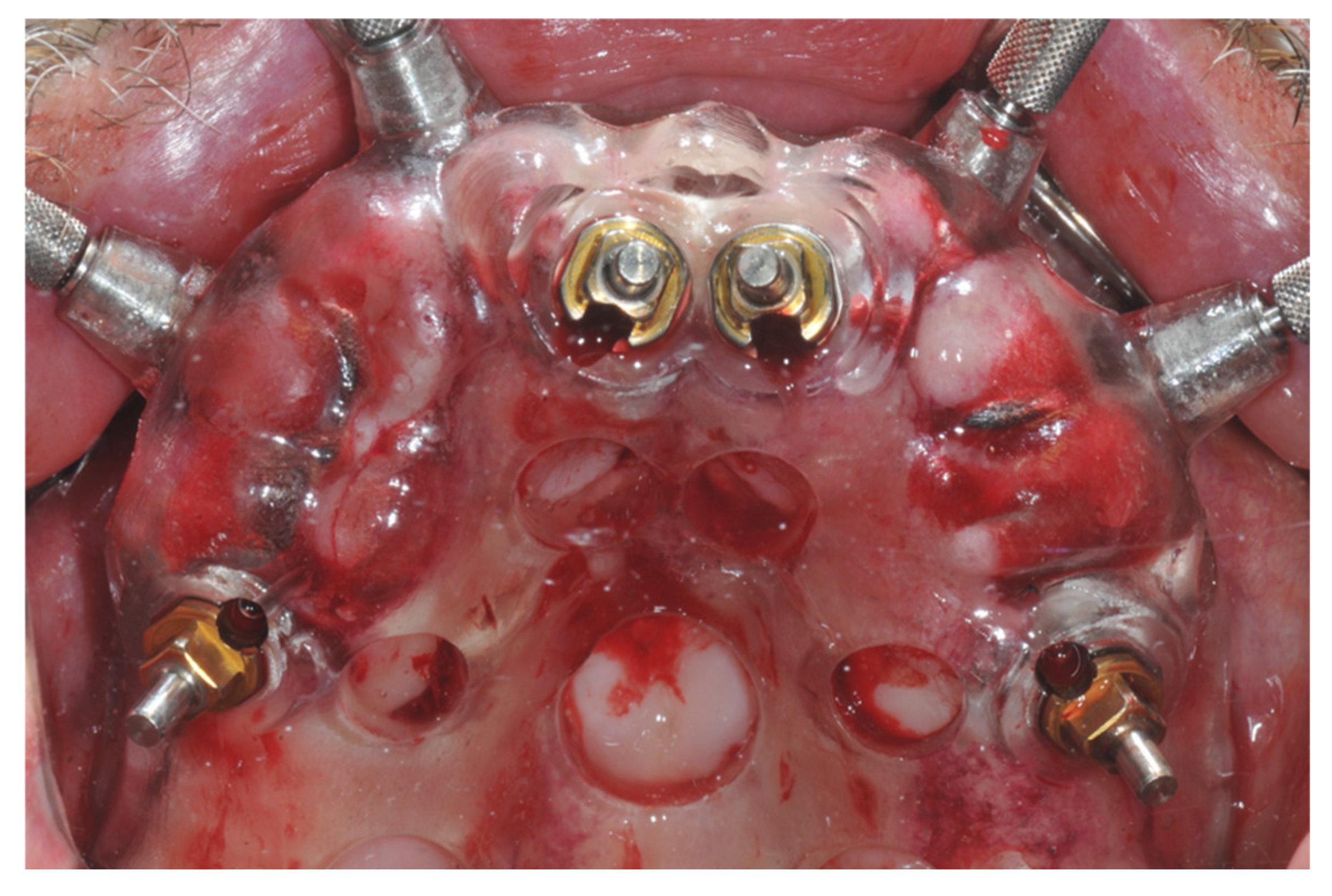
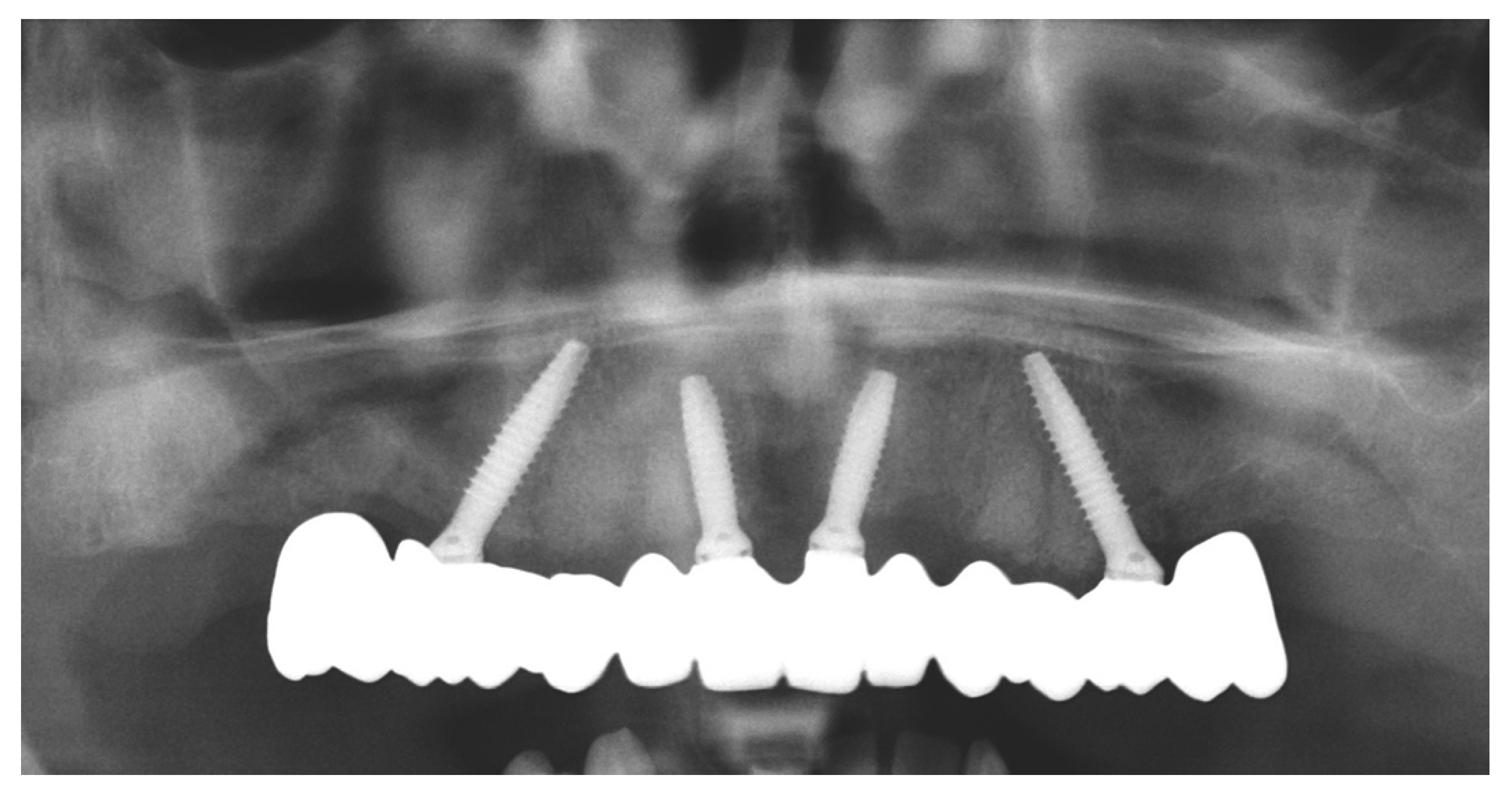
2. Materials and Methods
- 15: 4 × 15 mm 30°
- 11: 3.5 × 11.5 mm 17°
- 21: 3.5 × 11.5 mm 17°
- 25: 4 × 13 mm 30°
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Maiorana, C.; Poli, P.P.; Mascellaro, A.; Ferrario, S.; Beretta, M. Dental implants placed in resorbed alveolar ridges reconstructed with iliac crest autogenous onlay grafts: A 26-year median follow-up retrospective study. J. Cranio-Maxillofac. Surg. 2019, 47, 805–814. [Google Scholar] [CrossRef] [PubMed]
- Lini, F.; Poli, P.P.; Beretta, M.; Cortinovis, I.; Maiorana, C. Long-term retrospective observational cohort study on the survival rate of stepped screw titanium implants followed up to 20 years. Int. J. Oral Maxillofac. Implant. 2019, 34, 999–1006. [Google Scholar] [CrossRef] [PubMed]
- Maiorana, C.; Poli, P.P.; Borgonovo, A.E.; Rancitelli, D.; Frigo, A.C.; Pieroni, S.; Santoro, F. Long-Term Retrospective Evaluation of Dental Implants Placed in Resorbed Jaws Reconstructed with Appositional Fresh-Frozen Bone Allografts. Implant Dent. 2016, 25, 400–408. [Google Scholar] [CrossRef]
- Farronato, D.; Pasini, P.M.; Orsina, A.A.; Manfredini, M.; Azzi, L.; Farronato, M. Farronato Correlation between Buccal Bone Thickness at Implant Placement in Healed Sites and Buccal Soft Tissue Maturation Pattern: A Prospective Three-Year Study. Materials 2020, 13, 511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maiorana, C.; Manfredini, M.; Beretta, M.; Signorino, F.; Bovio, A.; Poli, P.P. Clinical and Radiographic Evaluation of Simultaneous Alveolar Ridge Augmentation by Means of Preformed Titanium Meshes at Dehiscence-Type Peri-Implant Defects: A Prospective Pilot Study. Materials 2020, 13, 2389. [Google Scholar] [CrossRef]
- Maiorana, C.; Ferrario, S.; Poli, P.P.; Manfredini, M. Autogenous Chin Block Grafts in the Aesthetic Zone: A 20-Year Follow-Up Case Report. Case Rep. Dent. 2020, 2020, 1–6. [Google Scholar] [CrossRef]
- Farronato, D.; Pasini, P.M.; Manfredini, M.; Scognamiglio, C.; Orsina, A.A.; Farronato, M. Influence of the implant-abutment connection on the ratio between height and thickness of tissues at the buccal zenith: A randomized controlled trial on 188 implants placed in 104 patients. BMC Oral Health 2020, 20, 53. [Google Scholar] [CrossRef] [Green Version]
- Beretta, M.; Poli, P.P.; Pieriboni, S.; Tansella, S.; Manfredini, M.; Cicciù, M.; Maiorana, C. Peri-Implant Soft Tissue Conditioning by Means of Customized Healing Abutment: A Randomized Controlled Clinical Trial. Materials 2019, 12, 3041. [Google Scholar] [CrossRef] [Green Version]
- Levine, R.A.; Ganeles, J.; Gonzaga, L.; Kan, J.K.; Randel, H.; Evans, C.D.; Chen, S.T. 10 Keys for Successful Esthetic-Zone Single Immediate Implants. Compend. Contin. Educ. Dent. 2017, 38, 248–260. [Google Scholar]
- Linkevicius, T.; Puisys, A.; Steigmann, M.; Vindasiute, E.; Linkeviciene, L. Influence of Vertical Soft Tissue Thickness on Crestal Bone Changes Around Implants with Platform Switching: A Comparative Clinical Study. Clin. Implant Dent. Relat. Res. 2015, 17, 1228–1236. [Google Scholar] [CrossRef]
- Steigmann, M.; Monje, A.; Chan, H.-L.; Wang, H.-L. Emergence Profile Design Based on Implant Position in the Esthetic Zone. Int. J. Periodontics Restor. Dent. 2014, 34, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Zipprich, H.; Weigl, P.; Ratka, C.; Lange, B.; Lauer, H.-C. The micromechanical behavior of implant-abutment connections under a dynamic load protocol. Clin. Implant Dent. Relat. Res. 2018, 20, 814–823. [Google Scholar] [CrossRef]
- Borgonovo, A.E.; Ferrario, S.; Maiorana, C.; Vavassori, V.; Censi, R.; Re, D. A Clinical and Radiographic Evaluation of Zirconia Dental Implants: 10-Year Follow-Up. Int. J. Dent. 2021, 2021, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Durrani, F.; Nahid, R.; Pandey, S.; Singh, P.; Pandey, A. One-piece implants: Careful approach for complex rehabilitation. Natl. J. Maxillofac. Surg. 2021, 12, 266. [Google Scholar] [CrossRef] [PubMed]
- Hagi, D. Stability Determination of One-Piece Ceramic Implants Using the Periotest Device: Follow-up Study of Up to 12 Months. Int. J. Oral Maxillofac. Implant. 2021, 36, 738–744. [Google Scholar] [CrossRef] [PubMed]
- Maiorana, C.; Poli, P.P.; Deflorian, M.; Testori, T.; Mandelli, F.; Nagursky, H.; Vinci, R. Alveolar socket preservation with demineralised bovine bone mineral and a collagen matrix. J. Periodontal Implant Sci. 2017, 47, 194–210. [Google Scholar] [CrossRef] [Green Version]
- Zucchelli, G.; Mazzotti, C.; Mounssif, I.; Mele, M.; Stefanini, M.; Montebugnoli, L. A novel surgical-prosthetic approach for soft tissue dehiscence coverage around single implant. Clin. Oral Implant. Res. 2013, 24, 957–962. [Google Scholar] [CrossRef]
- Deliberador, T.M.; Vieira, J.S.; Bonacin, R.; Storrer, C.L.M.; Santos, F.R.; Giovanini, A.F. Connective tissue graft combined with autogenous bone graft in the treatment of peri-implant soft and hard tissue defect. Quintessence Int. 2015, 46, 139–144. [Google Scholar]
- Venezia, P.; Torsello, F.; D’Amato, S.; Cavalcanti, R. Digital cross-mounting: A new opportunity in prosthetic dentistry. Quintessence Int. 2017, 48, 701–709. [Google Scholar]
- Beretta, M.; Poli, P.P.; Tansella, S.; Aguzzi, M.; Meoli, A.; Maiorana, C. Cast-free digital workflow for implant-supported rehabilitation in a completely edentulous patient: A clinical report. J. Prosthet. Dent. 2021, 125, 197–203. [Google Scholar] [CrossRef]
- Farronato, D.; Manfredini, M.; Mangano, F.; Goffredo, G.; Colombo, M.; Pasini, P.; Orsina, A.; Farronato, M. Ratio between Height and Thickness of the Buccal Tissues: A Pilot Study on 32 Single Implants. Dent. J. 2019, 7, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bittencourt, A.B.B.C.; Neto, C.L.D.M.M.; Penitente, P.A.; Pellizzer, E.P.; dos Santos, D.M.; Goiato, M.C. Comparison of the Morse Cone Connection with the Internal Hexagon and External Hexagon Connections Based on Microleakage—Review. Prague Med. Rep. 2021, 122, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Tahmaseb, A.; Van De Weijden, J.J.; Mercelis, P.; De Clerck, R.; Wismeijer, D. Parameters of passive fit using a new technique to mill implant-supported superstructures: An in vitro study of a novel three-dimensional force measurement-misfit method. Int. J. Oral Maxillofac. Implant. 2010, 25, 247–257. [Google Scholar]
- Mangano, F.G.; Hauschild, U.; Veronesi, G.; Imburgia, M.; Mangano, C.; Admakin, O. Trueness and precision of 5 intraoral scanners in the impressions of single and multiple implants: A comparative in vitro study. BMC Oral Health 2019, 19, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Tesmer, M.; Wallet, S.; Koutouzis, T.; Lundgren, T. Bacterial Colonization of the Dental Implant Fixture–Abutment Interface: An In Vitro Study. J. Periodontol. 2009, 80, 1991–1997. [Google Scholar] [CrossRef]
- do Nascimento, C.; Miani, P.K.; Pedrazzi, V.; Gonçalves, R.B.; Ribeiro, R.F.; Faria, A.C.L.; Macedo, A.P.; de Abulquerque, R.F., Jr. Leakage of saliva through the implant-abutment interface: In vitro evaluation of three different implant connections under unloaded and loaded conditions. Int. J. Oral Maxillofac. Implants 2012, 27, 551–560. [Google Scholar]
- Cochran, D.L.; Hermann, J.S.; Buser, D.; McManus, L.M.; Medina, R.U.; Broggini, N.; Schenk, R.K. Peri-implant inflammation defined by the implant-abutment interface. J. Dent. Res. 2006, 85, 473–478. [Google Scholar]
- Koutouzis, T. Implant-abutment connection as contributing factor to peri-implant diseases. Periodontology 2019, 81, 152–166. [Google Scholar] [CrossRef]
- Vetromilla, B.M.; Brondani, L.P.; Pereira-Cenci, T.; Bergoli, C.D. Influence of different implant-abutment connection designs on the mechanical and biological behavior of single-tooth implants in the maxillary esthetic zone: A systematic review. J. Prosthet. Dent. 2019, 121, 398–403.e3. [Google Scholar] [CrossRef]
- Axiotis, J.-P.; Nuzzolo, P.; Barausse, C.; Gasparro, R.; Bucci, P.; Pistilli, R.; Sammartino, G.; Felice, P. One-Piece Implants with Smooth Concave Neck to Enhance Soft Tissue Development and Preserve Marginal Bone Levels: A Retrospective Study with 1- to 6-Year Follow-Up. BioMed Res. Int. 2018, 2018, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Bolle, C.; Gustin, M.P.; Fau, D.; Exbrayat, P.; Boivin, G.; Grosgogeat, B. Early Periimplant Tissue Healing on 1-Piece Implants with a Concave Transmucosal Design: A Histomorphometric Study in Dogs. Implant. Dent. 2015, 24, 598–606. [Google Scholar] [CrossRef] [PubMed]
- Patzelt, S.B.M.; Bahat, O.; Reynolds, M.A.; Strub, J.R. The All-on-Four Treatment Concept: A Systematic Review. Clin. Implant Dent. Relat. Res. 2014, 16, 836–855. [Google Scholar] [CrossRef] [PubMed]








Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beretta, M.; Manfredini, M.; Poli, P.P.; Tansella, S.; Maiorana, C. Full Digital Model-Free Maxillary Prosthetic Rehabilitation by Means of One-Piece Implants: A Proof of Concept Clinical Report with Three-Years Follow Up. Prosthesis 2022, 4, 202-212. https://doi.org/10.3390/prosthesis4020020
Beretta M, Manfredini M, Poli PP, Tansella S, Maiorana C. Full Digital Model-Free Maxillary Prosthetic Rehabilitation by Means of One-Piece Implants: A Proof of Concept Clinical Report with Three-Years Follow Up. Prosthesis. 2022; 4(2):202-212. https://doi.org/10.3390/prosthesis4020020
Chicago/Turabian StyleBeretta, Mario, Mattia Manfredini, Pier Paolo Poli, Sebastian Tansella, and Carlo Maiorana. 2022. "Full Digital Model-Free Maxillary Prosthetic Rehabilitation by Means of One-Piece Implants: A Proof of Concept Clinical Report with Three-Years Follow Up" Prosthesis 4, no. 2: 202-212. https://doi.org/10.3390/prosthesis4020020
APA StyleBeretta, M., Manfredini, M., Poli, P. P., Tansella, S., & Maiorana, C. (2022). Full Digital Model-Free Maxillary Prosthetic Rehabilitation by Means of One-Piece Implants: A Proof of Concept Clinical Report with Three-Years Follow Up. Prosthesis, 4(2), 202-212. https://doi.org/10.3390/prosthesis4020020








