Preliminary Results of Total Hip Arthroplasty in Subjects at Risk for Dislocation Using a Novel Modular Cementless Dual-Mobility Cup. A Single-Center Prospective Study
Abstract
1. Introduction
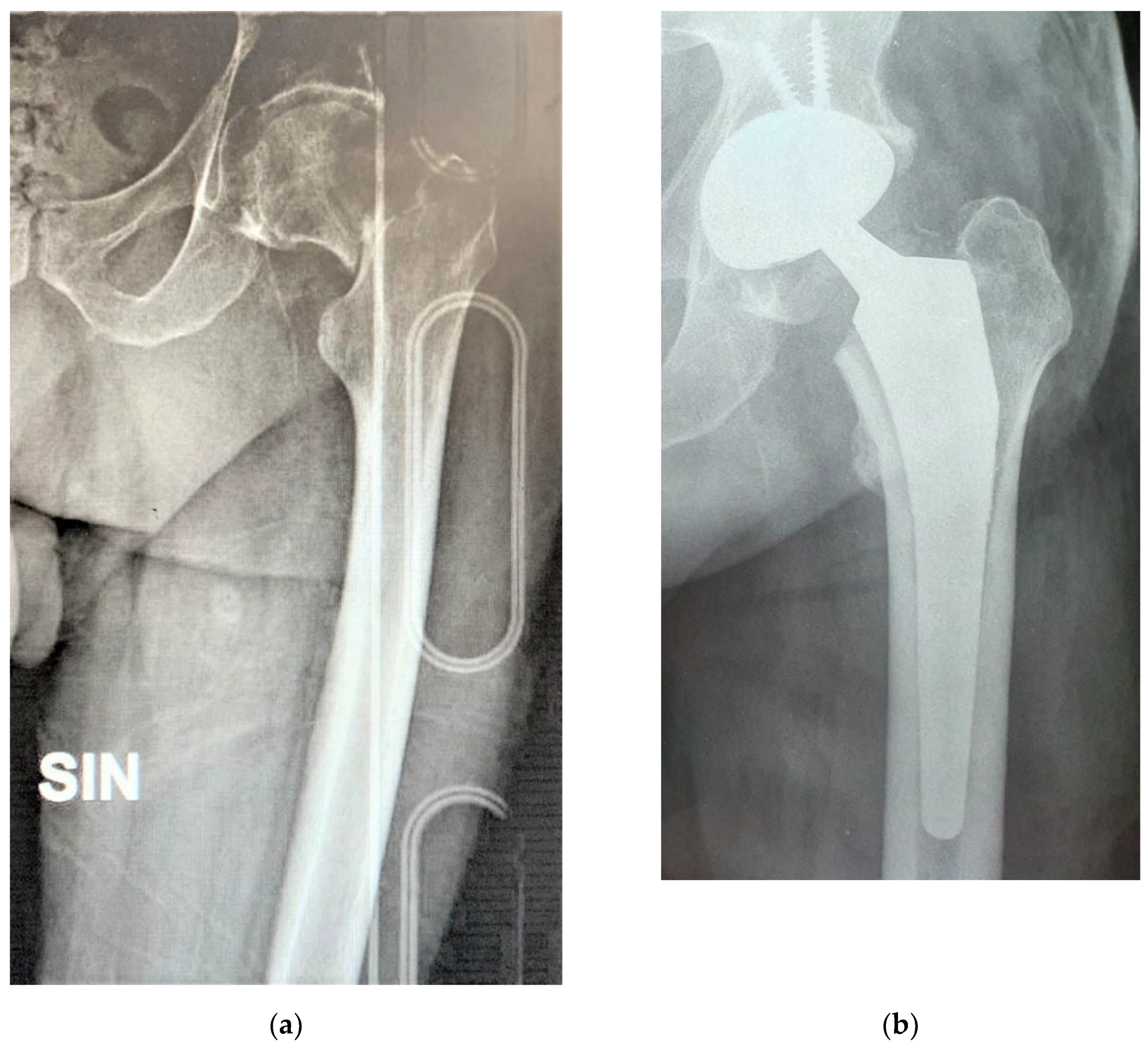
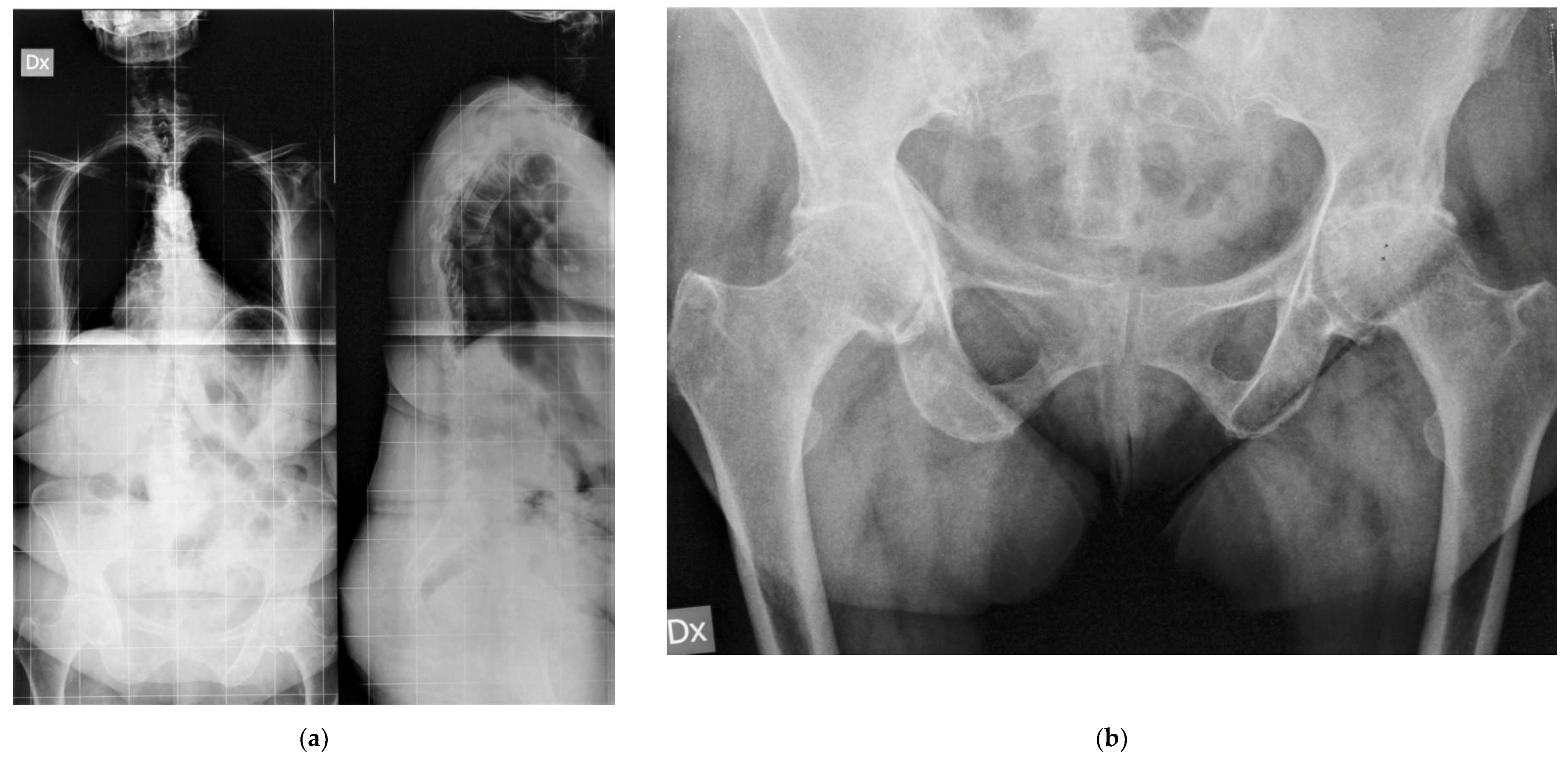
2. Material and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Brooks, P.J. Dislocation following total hip replacement: Causes and cures. Bone Joint J. 2013, 95, 67–69. [Google Scholar] [CrossRef] [PubMed]
- D’Angelo, F.; Zagra, L.; Moretti, B.; Virgilio, A.; Mazzacane, M.; Solarino, G. Retrospective multi-centre study on head adapters in partial revision hip arthroplasty. Hip Int. 2020, 30, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.A. The prevention and treatment of dislocation following total hip arthroplasty: Efforts to date and future strategies. Hip Int. 2015, 25, 388–392. [Google Scholar] [CrossRef] [PubMed]
- Noyer, D.; Caton, J.H. Once upon a time.... Dual mobility: History. Int. Orthop. 2017, 41, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Cuthbert, R.; Wong, J.; Mitchell, P.; Jaiswal, P.K. Dual mobility in primary total hip arthroplasty: Current concepts. EFORT Open Rev. 2019, 4, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Solarino, G.; Piazzolla, A.; Mori, C.M.; Moretti, L.; Patella, S.; Notarnicola, A. Alumina-on-alumina total hip replacement for femoral neck fracture in healthy patients. BMC Musculoskelet. Disord. 2011, 12, 32. [Google Scholar] [CrossRef]
- Adam, P.; Philippe, R.; Ehlinger, M.; Roche, O.; Bonnomet, F.; Molé, D.; Fessy, M.H. Dual mobility cups hip arthroplasty as a treatment for displaced fracture of the femoral neck in the elderly. A prospective, systematic, multicenter study with specific focus on postoperative dislocation. Orthop. Traumatol. Surg. Res. 2012, 98, 296–300. [Google Scholar] [CrossRef]
- De Martino, I.; D’Apolito, R.; Soranoglou, V.G.; Poultsides, L.A.; Sculco, P.K.; Sculco, T.P. Dislocation following total hip arthroplasty using dual mobility acetabular components: A systematic review. Bone Joint J. 2017, 99, 18–24. [Google Scholar] [CrossRef]
- Tristaino, V.; Lantieri, F.; Tornago, S.; Gramazio, M.; Carriere, E.; Camera, A. Effectiveness of psychological support in patients undergoing primary total hip or knee arthroplasty: A controlled cohort study. J. Orthop. Traumatol. 2016, 17, 137–147. [Google Scholar] [CrossRef]
- Buller, L.T.; Best, M.J.; Klika, A.K.; Barsoum, W.K. The influence of psychiatric comorbidity on perioperative outcomes following primary total hip and knee arthroplasty; a 17-year analysis of the National Hospital Discharge Survey database. J Arthroplast. 2015, 30, 165–170. [Google Scholar] [CrossRef] [PubMed]
- De Caro, M.F.; Vicenti, G.; Abate, A.; Picca, G.; Leoncini, V.; Lomuscio, M.; Casalino, A.; Solarino, G.; Moretti, B. Optimal improvement in function after total hip and knee replacement: How deep do you know your patient’s mind? J. Biol. Regul. Homeost. Agents 2015, 29, 95–102. [Google Scholar] [PubMed]
- Toro, G.; Moretti, A.; Paoletta, M.; De Cicco, A.; Braile, A.; Panni, A.S. Neglected femoral neck fractures in cerebral palsy: A narrative review. EFORT Open Rev. 2020, 5, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Mori, C.M.; Vicenti, G.; Carrozzo, M.; Picca, G.; Bizzoca, D.; Leone, A.; Morizio, A.; Solarino, G.; Moretti, B. The fake unlocked femoral nail: A configuration to avoid in stable pertrochanteric femur fractures. Injury 2018, 49 (Suppl. 3), S32–S36. [Google Scholar] [CrossRef] [PubMed]
- Caiaffa, V.; Vicenti, G.; Mori, C.M.; Panella, A.; Conserva, V.; Corina, G.; Scialpi, L.; Solarino, G.; Moretti, B. Unlocked versus dynamic and static distal locked femoral nails in stable and unstable intertrochanteric fractures. A prospective study. Injury 2018, 49 (Suppl. 3), S19–S25. [Google Scholar] [CrossRef]
- D’Arrigo, C.; Perugia, D.; Carcangiu, A.; Monaco, E.; Speranza, A.; Ferretti, A. Hip arthroplasty for failed treatment of proximal femoral fractures. Int. Orthop. 2010, 34, 939–942. [Google Scholar] [CrossRef] [PubMed]
- Cho, C.H.; Yoon, S.H.; Kim, S.Y. Better Functional Outcome of Salvage THA Than Bipolar Hemiarthroplasty for Failed Intertrochanteric Femur Fracture Fixation. Orthopedics 2010, 33, 721. [Google Scholar] [CrossRef]
- Archibeck, M.J.; Carothers, J.T.; Tripuraneni, K.R.; White, R.E., Jr. Total Hip Arthroplasty After Failed Internal Fixation Of Proximal Femoral Fractures. J. Arthroplast. 2013, 28, 168–171. [Google Scholar] [CrossRef]
- Pui, C.M.; Bostrom, M.P.; Westrich, G.H.; Della Valle, C.J.; Macaulay, W.; Mont, M.A.; Padgett, D.E. Increased complication rate following Conversion Total Hip Arthroplasty after cephalomedullary fixation for intertrochanteric hip fractures: A multi-center study. J. Arthroplast. 2013, 28, 45–47. [Google Scholar] [CrossRef]
- Bedard, N.A.; Martin, C.T.; Slaven, S.E.; Pugely, A.J.; Mendoza-Lattes, S.A.; Callaghan, J.J. Abnormally High Dislocation Rates of Total Hip Arthroplasty After Spinal Deformity Surgery. J. Arthroplast. 2016, 31, 2884–2885. [Google Scholar] [CrossRef]
- Salib, C.G.; Reina, N.; Perry, K.I.; Taunton, M.J.; Berry, D.J.; Abdel, M.P. Lumbar fusion involving the sacrum increases dislocation risk in primary total hip arthroplasty. Bone Jt. J. 2019, 101, 198–206. [Google Scholar] [CrossRef]
- Piazzolla, A.; Solarino, G.; Bizzoca, D.; Montemurro, V.; Berjano, P.; Lamartina, C.; Martini, C.; Moretti, B. Spinopelvic parameter changes and low back pain improvement due to femoral neck anteversion in patients with severe unilateral primary hip osteoarthritis undergoing total hip replacement. Eur. Spine J. 2018, 27, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Mudrick, C.A.; Melvin, J.S.; Springer, B.D. Late posterior hip instability after lumbar spinopelvic fusion. Arthroplast. Today 2015, 1, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Vicenti, G.; Solarino, G.; Spinarelli, A.; Carrozzo, M.; Picca, G.; Maddalena, R.; Rifino, F.; Moretti, B. Restoring the femoral offset prevent early migration of the stem in total hip arthroplasty: An EBRA-FCA study. J. Biol. Regul. Homeost. Agents 2016, 30, 207–212. [Google Scholar] [PubMed]
- Prudhon, J.L.; Verdier, R.; Caton, J.H. Low friction arthroplasty and dual mobility cup: A new gold standard. Int. Orthop. 2017, 41, 563–571. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, B.P.; Syku, M.; Sculco, T.P.; Jerabek, S.A.; Mayman, D.J.; Westrich, G.H. Dual-Mobility Constructs in Primary Total Hip Arthroplasty in High-Risk Patients With Spinal Fusions: Our Institutional Experience. Arthroplast. Today 2020, 6, 749–754. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Solarino, G.; Simone, F.; Panella, A.; Carlet, A.; Riefoli, F.; Moretti, B. Preliminary Results of Total Hip Arthroplasty in Subjects at Risk for Dislocation Using a Novel Modular Cementless Dual-Mobility Cup. A Single-Center Prospective Study. Prosthesis 2021, 3, 53-60. https://doi.org/10.3390/prosthesis3010006
Solarino G, Simone F, Panella A, Carlet A, Riefoli F, Moretti B. Preliminary Results of Total Hip Arthroplasty in Subjects at Risk for Dislocation Using a Novel Modular Cementless Dual-Mobility Cup. A Single-Center Prospective Study. Prosthesis. 2021; 3(1):53-60. https://doi.org/10.3390/prosthesis3010006
Chicago/Turabian StyleSolarino, Giuseppe, Filippo Simone, Antonello Panella, Arianna Carlet, Flavia Riefoli, and Biagio Moretti. 2021. "Preliminary Results of Total Hip Arthroplasty in Subjects at Risk for Dislocation Using a Novel Modular Cementless Dual-Mobility Cup. A Single-Center Prospective Study" Prosthesis 3, no. 1: 53-60. https://doi.org/10.3390/prosthesis3010006
APA StyleSolarino, G., Simone, F., Panella, A., Carlet, A., Riefoli, F., & Moretti, B. (2021). Preliminary Results of Total Hip Arthroplasty in Subjects at Risk for Dislocation Using a Novel Modular Cementless Dual-Mobility Cup. A Single-Center Prospective Study. Prosthesis, 3(1), 53-60. https://doi.org/10.3390/prosthesis3010006





