Abstract
Background: In Flanders, the uptake in the population-based colorectal cancer (CRC) screening program (using fecal immunochemical test, FIT) is suboptimal (~50%). This study explored the reasons for inconsistent participation in FIT screening among irregular participants in Flanders. Methods: An online survey with both open questions and fixed statements was sent to irregular participants (2016–2018) in the Flemish CRC screening program. A reminder email followed eight weeks after the first email. Data analysis used both qualitative and quantitative approaches. Post-stratification weights based on gender, age group, and the first two digits of the postcode were employed to reduce non-response bias. Results: In total, 5328 out of 19,592 irregular participants responded to the survey. While the main reasons not to participate were related to ‘postponing participation’ and ‘having other priorities’, the main reasons to participate were related to the importance of (preventive) health checks. The role of general practitioners (GPs) in promoting CRC screening also emerged as an important theme among the respondents’ answers (based on fixed statements). Conclusions: The study reported the main reasons for inconsistent participation in FIT screening for CRC in Flanders. The findings are helpful in guiding tailored interventions to increase FIT screening uptake in the region.
1. Introduction
The Flemish colorectal cancer (CRC) screening program uses a centralized invitation procedure: invitations (with leaflet and fecal immunochemical test, FIT) are sent by the Centre for Cancer Detection (CCD) by post. Participation is free of charge. The target population (50–74 years old) receives a new invitation 24 months after their last screening (or after their last invitation for non-participants) [1]. The cost of diagnostic colonoscopy (DC) following a positive fecal immunochemical test (FIT) screening is reimbursed by the Belgian healthcare system with a certain percentage out-of-pocket expense.
The screening uptake has varied from 48.4% to 52.5% since the start of the program in 2013 and is suboptimal [2,3]. During 2017–2021, among individuals with at least two invitation rounds, 45% were adherent to all the invitations, 14% were irregular participants, and 40% were non-responsive to all invitations [internal data CCD]. In Flanders, the five-year relative survival rate for CRC (2014–2018) is 74.9% [4], and it is even 97.6% for Stage I compared with only 18.7% for Stage IV [5]. These results highlight the clinical importance of participation in CRC screening and screening adherence.
Reasons not to participate in CRC screening have been widely documented, and comprise a ‘lack of symptoms’, ‘feeling healthy’, ‘no family CRC history’, ‘general lack of knowledge’, ‘being unaware of the usefulness of CRC screening’, ‘fear of cancer’, ‘fear of a positive result’, ‘fear of a follow-up colonoscopy’, and ‘lack of a provider recommendation’ [6,7,8,9,10,11,12,13,14,15,16,17]. In Flanders, ‘fear of cancer’, ‘shame’, and ‘feeling healthy’ have emerged as key barriers to screening [18]. Prior research conducted among irregular participants in Catalonia, Spain, and Florida, US, indicated that ‘procrastination’ [19], ‘cancer fear’ and ‘being unaware of the need to repeat screening’ play a role in CRC screening (non)adherence [20,21,22].
It is known that the reasons for inconsistent participation in CRC screening are dependent on the local context and culture. Since this topic has not been researched in Belgium, we conducted the current study to investigate the reasons behind people’s decision to (re)start or skip participation in CRC screening in Flanders (57% of the Belgian population). Our results help to understand the potential triggers to CRC screening by FIT that can be encouraged as well as barriers to screening that can be addressed by, for example, adapting communication materials or strategies in informing the target population in order to eventually increase re(start) FIT screening.
2. Results
2.1. Sociodemographic Characteristics of the Survey Respondents
In total, 5328 of the 19,592 invitees (27.6%) responded to the survey, of whom 640 (12.0%) responded after the reminder email. The sociodemographic characteristics of the survey respondents are presented in Table 1. More men (55.0%) vs. women and more younger people aged 59–64 years (57.9%) vs. 65–75 years responded to the survey. The majority of respondents had a Belgian nationality (92.4%), spoke Dutch (the local language in Flanders) at home (97.4%), and were married or cohabiting without children living at home (59.9%). Three quarters of them had higher than a secondary education, 87.3% were full-time/part-time employees or retired. Almost 87% of the respondents were in a fair or good financial situation (neutral/easy/very easy) and 89% did not have to suspend a medical appointment or medical procedure due to financial problems.

Table 1.
Sociodemographic characteristics of the survey respondents (absolute numbers and unweighted percentages).
2.2. Results of Survey Questions
2.2.1. Reasons Not to Participate
Figure 1 and Figure 2 present reasons not to participate in FIT screening answered by the respondents in open questions and fixed statements (applicable or not), grouped into subthemes. Categories with <20 answers were left out. Only 297 respondents (5.6%) did not fill in the open question or filled in ‘I don’t know’. The first part of the table (in green color) summarizes reasons not to participate that were reported in both the open answers as fixed statements; the second part (in orange and purple colors) summarizes reasons not to participate that were reported only in one source but not the other.
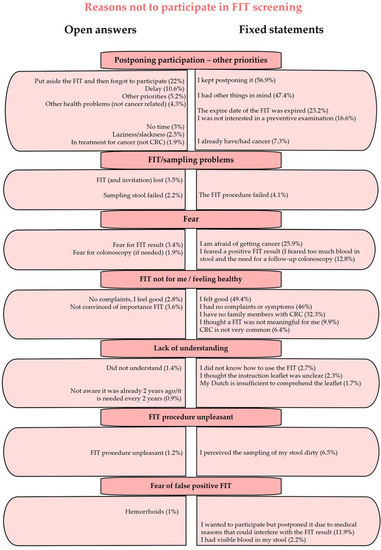
Figure 1.
Reasons not to participate in FIT screening among irregular participants in Flanders which are common between individuals’ self-reported open answers and given fixed statements (Q1 and S1).
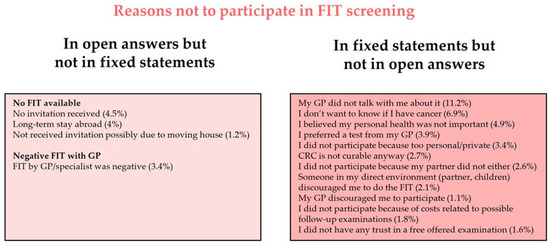
Figure 2.
Reasons not to participate in FIT screening among irregular participants in Flanders which are based on either the individuals’ self-reported open answers or given fixed statements (Q1 and S1) but not the other. GP: general practitioner.
The most reported reasons not to participate in screening in both the open question (~50% of reasons) and fixed statements were related to postponing FIT participation and having other priorities (‘put the FIT aside to forget it’, ‘delay participation’, ‘not interested’, ‘laziness’, or ‘have another cancer/other health problems’). It appeared that non-participation due to ‘fear’, ‘personal feelings and perceptions’ were selected more when given as fixed statements compared with when given as a free-text answer to the open question. For instance, ‘I feel good’ and ‘I had no complaints or symptoms’ were selected by 49.4% and 46.0% of respondents in fixed statements but were only given in the answers to the open question by 2.8% of respondents. ‘Unpleasant sampling procedure’ and ‘fear of a false positive FIT’ were also selected more as a reason not to participate when given as fixed statements, compared with open answers. Other reasons not to participate, given both in open answers and fixed statements, include FIT/sampling problems (‘FIT and invitation lost’; ‘sampling procedure failed’) and lack of understanding (‘insufficiency of Dutch language’; ‘unclear instruction leaflet’).
At the same time, there are reasons not included in the literature (and not given as fixed statements) but mentioned by respondents in Flanders: no FIT available (e.g., ‘no invitation received, possibly due to moving house or staying abroad’, 9.7%) and ‘FIT by GP or specialist was negative’ (3.4%). These reasons seem to be typical of the Flemish context. Several reasons (Figure 2) were selected when given in fixed statements but did not appear in the open answers, e.g., ‘My GP (general practitioner) did not talk with me about it (FIT screening)’ (applicable for 11.2%), or ‘I don’t want to know if I have cancer’ (6.9%).
2.2.2. Reasons to Participate
Figure 3 and Figure 4 present reasons for FIT screening participation, grouped into subthemes, by respondents in both the open question and fixed statements (first part of the table, in green color) or only in the open question but not in fixed statements (second part, in orange color). Categories with <20 answers were left out. Only 79 respondents (2.3%) did not fill in the open question or filled in ‘I don’t know’.
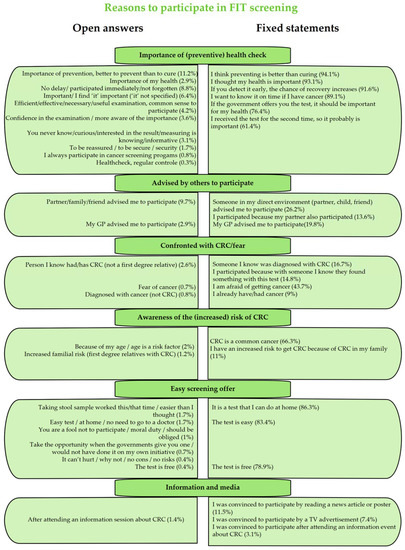
Figure 3.
Reasons to participate in FIT screening among irregular participants in Flanders which are common between individuals’ self-reported open answers and given fixed statements (only delayed entries N = 3401) (Q2 and S2). GP: general practitioner.
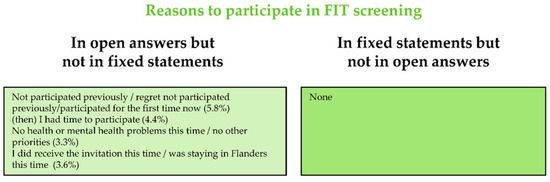
Figure 4.
Reasons to participate in FIT screening among irregular participants in Flanders which are based on either the individuals’ self-reported open answers or given fixed statements (Q2 and S2) but not the other (only delayed entries N = 3401).
The most reported reasons to participate in screening in both the open question (40% of reasons in open answers) and fixed statements were related to the importance of (preventive) health checks: e.g., ‘better to prevent than to cure’ and ‘importance of my health’. Some other reported reasons to participate can be grouped into ‘advised by others to participate’ (~13% of reasons given in the open question) and ‘confronted with CRC and fear’. Although only 23 respondents (0.7%) indicated ‘fear of cancer’ as a reason to participate in the open answers, more than 40% indicated it in the fixed statement as being a reason to participate. In the subtheme ‘awareness of the (increased) risk of CRC’, ‘CRC as a common cancer’ was selected by the respondents among the fixed statements to be a reason to participate, while this was not filled in as an open answer. Other subthemes captured in both open answers and fixed statements were ‘easy screening offer’ (e.g., ‘test is free’) and ‘information and media’ (e.g., ‘information event about CRC screening’, while media comprises information about the ongoing Flemish CRC screening program in newspapers, social media, and TV and radio campaigns).
The reasons to participate that were not given as fixed statements, but were mentioned by the respondents, mainly referred to a previous non-participation, e.g., ‘regretted previous non-participation’ and ‘no other priorities this time’.
2.2.3. Role of GPs, Leaflets and Media
Table 2 below summarizes given statements about the need for more information and the possible role of GPs in FIT participation. The majority rather or completely agreed that ‘the invitation and leaflet contained enough information to make a decision to participate or not’ (83.4%), that ‘the leaflet provided sufficient information about the importance of repeating the test every two years’ (81.9%), and that ‘the sampling instructions were clear enough’ (89%). Fewer than half of the respondents (42.4%) were aware that a new test could be requested for free. More than 65% of the respondents agreed with the statement that ‘their GP should mention the FIT invitation’ and more than 40% agreed with the statement that ‘they would have participated earlier if their GP had recommended FIT for CRC screening’.

Table 2.
Results of survey statements about ‘the need for more information after the FIT invitation and the role of the GPs (S3)’ in absolute numbers and weighted percentages.
2.2.4. Intention for Future Participation
Among the survey respondents, more than 95% (weighted N = 5058) answered they would participate in the future in the CRC screening program (Q3), 2.5% did not know, and 2.5% (weighted N = 135) responded ‘not willing to participate in the future’. ‘Under specialist follow-up due to a positive FIT result’ and ‘no longer in the target population (>74 years)’ are the most reported reasons of not wanting to participate in the future. The second most reported reasons are linked with different disadvantages of CRC screening. Other reasons are listed in Table 3 below.

Table 3.
Reasons for no future FIT participation (Q3).
3. Discussion
This study explored the barriers and triggers to (re)participate in or skip FIT screening among irregular participants in Flanders. To make use of the evidence reported in the literature as well as to capture the context-specific information in Flanders that has not been documented, we used both open questions and fixed statements. We found that some themes emerged in both approaches while other themes only emerged in one approach but not in the other. The two approaches complement each other: while fixed statements remind respondents of the main reasons for inconsistent participation that they could not recall in a short time, open questions help to identify the reasons that are specific for Flanders (not documented in the literature).
We found ‘procrastination, postponing, and having other priorities’ to be the main reasons for not being adherent to FIT screening (based on both open questions and fixed statements). The literature has already indicated delay, other priorities [6,17,19,23], and forgetfulness [24] as common reasons not to participate. ‘Fear’ (of a positive FIT result, of having cancer, and/or of a colonoscopy) also emerged in both the open question and fixed statements, as a reason for being nonadherent to screening. Fear as a reason for CRC screening nonadherence is given elsewhere [17]. Interestingly, fear (being afraid of getting cancer) also came up as a motivation to participate in the program. Benito et al. (2018) [20] already indicated that fear works in two ways: it can both facilitate CRC screening adherence and prevent further screening. Similarly, religion acts as both a facilitator and a barrier to CRC screening [25,26,27]. In our study, only 19/3401 (0.6%) delayed entries and 8/1927 (0.4%) dropouts indicated religion as their reason not to participate in FIT screening (fixed statement). At the same time, 44/3401 (1.3%) delayed entries filled in religion as their reason to participate in FIT screening (open answer). The low percentages of respondents selecting ‘religion’ show that religion is only a minor factor to facilitate or prevent FIT screening in Flanders. As a result, it was not included in our main results.
In the current study, reasons linked to ‘fear’, ‘FIT is not for me’, and ‘feeling healthy’ were given more often in fixed statements compared with open answers These reasons seem to be very common among respondents; however, they are not ranked very highly in terms of importance since the respondents did not mention these when they needed to give only one main reason. Both the lack of knowledge or perceived need of CRC screening and not feeling that participation is personally necessary have been well documented [6,19,28,29]. We found that ‘no FIT available’ (e.g., no invitation received or long-term stay abroad) as a reason for non-participation only emerged in open questions but not in fixed statements, suggesting that this is a context-specific issue of Flanders.
The most important reason for participating in FIT screening—recorded in both open answers and fixed statements—was the ‘importance of (preventive) health checks’. This is an important reason stated in the literature as well [19,30]. ‘Advised by others to participate’ (by partner, children, and GP) was indicated as an important reason to participate, especially in the fixed statements. The importance of social influences for people to participate has also be reported by others [19,22,30,31].
Although only a minority (9.6%) agreed with the statement that they needed more information from a GP after reading the invitation, 65% indicated that a GP should mention the FIT invitation spontaneously and more than 40% would participate earlier if their GP advised it. The role of the GP also occurred differently depending on the approach: in fixed statements, ‘My GP did not talk with me about FIT screening’ emerged as a reason not to participate, while in open answers, ‘a negative FIT result by the GP’ (after a previous positive one in the screening program) was mentioned as a reason not to participate. A GP recommendation has been well reported as an important trigger to participate in CRC screening [17,19,20,28,29,32].
According to the results from fixed statements about the information in the leaflet and instructions on how to use the FIT, the majority of respondents thought that the information was clear enough to decide whether to participate. The FIT invitation by mail was perceived as an easy offer that triggered participation. Green et al. [19] also indicated that the convenience of mailing and doing the test at home is a screening facilitator. Berg-Beckhoff (2022) indicated that ‘when given the FIT offer’ was an important reason to participate [33]. Only in open answers, ‘regret of not having participated previously’ was indicated as a trigger to participate in the current screening round. Although ‘feeling good’ and ‘no CRC in the family’ were not given in open answers as a reason for being nonadherent to FIT screening, many respondents found those reasons applicable when given as fixed statements.
Based on the survey results, in particular the ‘postponing participation’ and ‘having other priorities’, some adjustments have been made to the invitation, leaflet, and the national campaign in Flanders: in the leaflet, the sentence ‘put the kit near the toilet’ was added. In the campaign, ‘no excuse’ was launched as a central theme. These reasons could also result from socially desirable responding.
Recent systematic reviews clearly indicate that outreach interventions based on (a combination of) phone calls, pre- and post-FIT text messaging, mail reminders, and provider alerts improve FIT uptake. Tailored patient messages and financial initiatives do not seem to increase CRC screening [34,35,36]. Huf et al. [37] indicated that serial motivational text messaging with an opt-out design can substantially improve FIT uptake. In an opt-out design, FIT is mailed unless the person opted out of screening while in an opt-in design, FIT is mailed only if the person actively opted in to participate. Somsouk et al. [38] also found that a mailed informational postcard (usual care) combined with up to two phone calls, followed by a mailed FIT and up to two reminder phone calls (if FIT was not returned within two weeks), improved FIT uptake.
In 2022, the Flemish CRC screening program started a pilot project in which a second reminder (by email only) is sent after the first standard reminder (10 weeks after the invitation) in order to increase screening uptake. In a second step, the screening program is investigating if sending an SMS reminder (after the second reminder by email) can increase adherence as well. Apparently, telephone numbers (as well as the email addresses) are predominantly available in ever-participants or individuals that also participated in the other screening programs organized by the CCD. Their contact information is available in the system if they agreed with the use of their contact details for the CRC screening program. Text messaging and telephone-based interventions appear very promising to increase FIT uptake in Flanders, but the impact relies heavily on the availability of accurate phone numbers in the system. A telephone intervention pilot among non-participants has recently been set up in Flanders and preliminary results show that telephone numbers were only available and correct for a minority (<15%) of non-participants.
‘Feeling good’, ‘not having symptoms’, and ‘no CRC in the family’ have also been addressed in the leaflet and information materials of the Flemish program in terms of the aim of screening. These materials highlight that the aim of the test is ‘screening’, meaning that the target individuals need to participate when they do not yet have any symptoms. Fewer than half of the respondents were aware that a free FIT could be requested if needed (e.g., a lost or expired test), so this information has been added in the leaflet and to the website of the screening program. A significant proportion of irregular participants stated that their previous non-participation was only temporarily due to a specific reason (e.g., I participated because ‘I had time this year’, ‘I received the invitation this year’, or ‘I was in Belgium’). It appears that they would normally participate when the temporary situation was over.
Our study highlights the need to strengthen the role of GPs in promoting CRC screening and screening adherence among their patients. Survey respondents would have participated (earlier) if their GP had advised them to do so. This indicates ‘GP not talking about CRC screening’ as a reason for their patients’ non-participation. GPs might need to do this proactively (not related to an immediate invitation) since some patients do not even know what information about CRC screening they can expect from their GPs. They agreed with the fixed statements about the role of GPs in informing and promoting CRC screening to them, but they did mention this theme themselves in the open answers. The CCD is planning a pilot to test if a one-minute motivational talk can increase CRC adherence among non-participants.
An important limitation of this study is that the online survey was only sent to ever-participants who provided the CCD with a valid email address. These included more men, at younger ages (e.g., 59–64 years old), with a higher socio-economic status, higher educational level, and speaking the local language. Therefore, our results might not be representative for the entire eligible population. However, the focus of the study is to increase adherence to CRC screening among inconsistent participants; tackling never-participants will be our next step. Furthermore, with a large sample size, our study could still capture the responses of 764 people in the oldest age category (70–75 years, 14.3% of the study population), 250 people with a (very) difficult financial situation (13%) of which approximately 200 (11%) ever suspended a medical procedure because of financial reasons, 134 persons with the lowest educational level—no degree or only primary degree (7%)—and 49 people speaking a language other than Dutch (2.6%).
4. Materials and Methods
4.1. Study Design—Online Survey
The current study is a cross-sectional study in which we combined qualitative (categorized open questions) and quantitative approaches (fixed statements and closed questions). An online email survey (in Dutch) was sent in October 2019 to the irregular participants of the 2016–2018 survey seasons, including (1) delayed entries: those who did not participate after their previous FIT invitation in 2016, but participated after the most recent one in 2018; and (2) dropouts: those who participated after their previous FIT invitation in 2016 but did not participate after the most recent one in 2018 in the Flemish CRC screening program. A reminder email was sent to the entire study population (due to the anonymous approach) eight weeks after the first email (December 2019). The survey was based on the literature [6,8,19,20,22,30] and the results of 26 telephone interviews among irregular participants in the Flemish CRC screening program, and was piloted on an external panel before being performed in the eligible population. Only participants who had once provided a valid email address in their participation form (sent together with their stool sample) received a link to the online survey.
4.2. Overview of the Survey Questions
The survey questions concerning reasons for inconsistent participation—(re)starting or skipping a screening round—during 2016–2018 in the Flemish CRC screening program are given below. We used a combined approach in which we provided both fixed statements (Table 4 and Supplementary Tables S1–S3) based on a search of the literature [6,8,19,20,22,30] and previous research in Flanders [18], and open questions to answer with free text (Table 4). Note that only one main answer per respondent to each open question was included, while with fixed statements, people were allowed to select all statements that were applicable to them. The two methods of obtaining information complemented each other: the fixed statements helped to remind respondents of the most reported reasons in a similar setting in other countries and regions, while with open questions, we could capture reasons that are specific to the Flemish context or that have not been recorded in the literature. All the questions and statements were asked to both delayed entries and dropouts, except for the questions and statements on reasons to participate, which were only asked of the delayed entries since we were specifically interested in understanding the motivations that drove people to (re)start FIT screening in the current round. Based on this knowledge, we could develop and provide tailored interventions to increase FIT screening in Flanders.

Table 4.
Summary of the open survey questions and fixed statements.
4.3. Statistical Analysis
4.3.1. Post-Stratification Weights
Non-response bias is common in survey studies. This bias occurs when individuals with certain characteristics over- or under-respond to a survey. Our preliminary findings showed significant differences between respondents and non-respondents in terms of gender (male/female), age group (59–64/65–69/70–74 years), and the first two digits of their postcode (15–39/80–99) (all p-values < 0.001). More specifically, males responded more to our survey compared with females (55% of respondents vs. 51% of non-respondents were males). More people aged 59–64 years, but fewer people aged 70–75 years responded to our survey (ages 59–64 years: 58% among respondents vs. 51% among non-respondents; ages 70–75 years: 14% among respondents vs. 21% among non-respondents). While some areas—presented by the first two postcode digits—had a larger proportion of respondents vs. non-respondents (e.g., 29: 5.5% among respondents vs. 4.9% among non-respondents, 90: 5.1% among respondents vs. 4.1% among non-respondents), other areas had a lower proportion of respondents vs. non-respondents (e.g., 18: 1.8% among respondents vs. 2.4% among non-respondents, 99: 1.9% among respondents vs. 2.3% among non-respondents) (Supplementary Tables S4–S6).
To reduce non-response bias, we constructed post-stratification weights based on gender, age group, and the first two digits of the postcode [39]. Each respondent was assigned with a weight—corresponding to the person’s profile which is a combination of gender, age group, and the first two digits of the respondent’s postcode—so that when we adjusted for the post-stratification weights in our analyses, the distribution of the respondent population (5328 subjects) would replicate the distribution of the total study population (19,468 subjects) to whom we sent the survey in terms of gender, age group, and the first two digits of the postcode [40]. For ease of presentation, each weighted number of the respondents presented in our results (after applying post-stratification weights) was rounded to the nearest integer.
4.3.2. Main Data Analysis
We used the SPSS (version 25) to collect and openly code information from respondents’ answers to the open questions (qualitative data) and analyze the data thematically. The absolute numbers and the corresponding percentages of respondents who had certain answers or selected certain statements were presented. All quantitative analyses were performed using RStudio software (version 1.3.1056; RStudio, PBC, Boston, MA, USA).
4.4. Privacy and Ethics
Response to the online survey served as informed consent. No ethical approval was needed. Respondents’ anonymity was ensured throughout the study. No incentive was given.
5. Conclusions
This study investigated the reasons for (re)starting or skipping FIT screening among irregular participants in the Flemish CRC screening program by exploring their responses to both fixed statements and open questions via an online survey. The most reported reasons not to participate in FIT screening were related to ‘postponing participation’ and ‘having other priorities’, whereas the most reported reasons to participate were related to the importance of (preventive) health checks. A large proportion of respondents agreed with statements about the influence of GPs on their decision to participate in CRC screening.
Based on the survey results, adjustments have been made to the screening materials (invitation, leaflets) and campaigns of the Flemish CRC screening program. The CCD is also developing several other interventions to increase FIT uptake in Flanders, including sending a second reminder email after the first reminder letter, contacting non-participants by telephone, and launching community projects that involve community healthcare workers in having face-to-face conversations with non-participants in order to sensibilize them on the importance of FIT screening.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/gidisord5010001/s1, Table S1: Statements 1—What has influenced the decision not to participate (31 statements); Table S2: Statements 2—What has influenced the decision to participate? (22 statements, delayed entrees only); Table S3: Statements 3: Opinions about the GP role, information in the invitation and leaflet (11 statements); Table S4: Gender difference between the response and non-response groups to the survey; Table S5: Age difference between the response and non-response groups to the survey; Table S6: Postcode difference (first 2 digits) between the response and non-response groups to the survey.
Author Contributions
Conceptualization, S.H.; writing—original draft preparation, S.H. and TNT.; writing—review and editing, S.H. and T.N.T.; statistical analysis, S.H. and T.N.T.; visualization, S.H. and T.N.T.; supervision, S.H. All authors have read and agreed to the published version of the manuscript.
Funding
The Flemish CRC screening program is funded exclusively by the Agency for Care and Health, part of the Flemish Ministry of Welfare, Public Health and Family (https://www.vlaanderen.be/en), accessed on 13 December 2022. The Flemish Ministry was not involved in any phase of this study (design, data collection, analysis, interpretation, or writing the manuscript).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
When participating in the screening program, all participants filled out a written informed consent explaining that personal information can be used for scientific research and evaluation to improve the CRC screening programme.
Data Availability Statement
Data on screening uptake, gender, and age-specific proportions of the target screening population can be requested by contacting the Centre for Cancer Detection in Flanders at https://www.bevolkingsonderzoek.be. The survey data that support the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available due to privacy restrictions.
Acknowledgments
We acknowledge the Flemish Colorectal Cancer Screening Task Force for functioning as a sounding board and colleagues of the Centre for Cancer Detection for their feedback on the initial draft of the online survey.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hoeck, S.; van de Veerdonk, W.; De Brabander, I. Do socioeconomic factors play a role in nonadherence to follow-up colonoscopy after a positive faecal immunochemical test in the Flemish colorectal cancer screening programme? Eur. J. Cancer Prev. 2020, 29, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Centre for Cancer Detection & Belgian Cancer Registry. Monitoring Report of the Flemish Colorectal Cancer Screening Programme. 2021. Available online: https://dikkedarmkanker.bevolkingsonderzoek.be/sites/default/files/2022-03/Jaarrapport%202021%20BVO%20naar%20kanker_0.pdf (accessed on 26 April 2022).
- Website Bevolkingsonderzoek In Cijfers. Available online: https://bevolkingsonderzoek.incijfers.be//jive?cat_open_code=ddk_extern (accessed on 16 December 2022).
- Belgian Cancer Register (BCR). Cancer Fact Sheet, Colorectal Cancer, ICD10: C18-20; BCR: Brussels, Belgium, 2018; Available online: https://kankerregister.org/media/docs/CancerFactSheets/2018/Cancer_Fact_Sheet_ColorectalCancer_2018.pdf (accessed on 16 December 2022).
- Hoeck, S.; De Schutter, H.; Van Hal, G. Why do participants in the Flemish colorectal cancer screening program not undergo a diagnostic colonoscopy after a positive fecal immunochemical test? Acta Clin. Belg. 2022, 77, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Hall, N.J.; Rubin, G.P.; Dobson, C.; Weller, D.; Wardle, J.; Ritchie, M.; Rees, C.J. Attitudes and beliefs of non-participants in a population-based screening programme for colorectal cancer. Health Expect. 2015, 18, 1645–1657. [Google Scholar] [CrossRef] [PubMed]
- van Dam, L.; Korfage, I.J.; Kuipers, E.J.; Hol, L.; van Roon, A.H.; Reijerink, J.C.; van Ballegooijen, M.; van Leerdam, M.E. What influences the decision to participate in colorectal cancer screening with faecal occult blood testing and sigmoidoscopy? Eur. J. Cancer 2013, 49, 2321–2330. [Google Scholar] [CrossRef]
- Bradley, D.T.; Treanor, C.; McMullan, C.; Owen, T.; Graham, A.; Anderson, D. Reasons for non-participation in the Northern Ireland Bowel Cancer Screening Programme: A qualitative study. BMJ Open 2015, 5, e008266. [Google Scholar] [CrossRef]
- Palmer, C.K.; Thomas, M.C.; Von Wagner, C.; Raine, R. Reasons for non-uptake and subsequent participation in the NHS Bowel Cancer Screening Programme: A qualitative study. Br. J. Cancer 2014, 110, 1705–1711. [Google Scholar] [CrossRef]
- Woudstra, A.J.; Dekker, E.; Essink-Bot, M.L.; Suurmond, J. Knowledge, attitudes and beliefs regarding colorectal cancer screening among ethnic minority groups in the Netherlands—A qualitative study. Health Expect. 2015, 19, 1312–1323. [Google Scholar] [CrossRef]
- Dawson, G.; Crane, M.; Lyons, C.; Burnham, A.; Bowman, T.; Travaglia, J. A qualitative investigation of factors influencing participation in the bowel screening in New South Wales. Health Promot. J. Aust. 2016, 27, 48–53. [Google Scholar] [CrossRef]
- Chapple, A.; Ziebland, S.; Hewitson, P.; McPherson, A. What affects the uptake of screening for bowel cancer using a faecal occult blood test (FOBt): A qualitative study. Soc. Sci. Med. 2008, 66, 2425–2435. [Google Scholar] [CrossRef]
- Honein-AbouHaidar, G.N.; Kastner, M.; Vuong, V.; Perrier, L.; Daly, C.; Rabeneck, L.; Straus, S.; Baxter, N.N. Systematic Review and Meta-study Synthesis of Qualitative Studies Evaluating Facilitators and Barriers to Participation in Colorectal Cancer Screening. Cancer Epidemiol. Biomark. Prev. 2016, 25, 907–917. [Google Scholar] [CrossRef]
- Keighley, M.R.B.; O’Morain, C.; Giacosa, A.; Ashorn, M.; Burroughs, A.; Crespi, M.; Delvaux, M.; Faivre, J.; Hagenmuller, F.; Lamy, V.; et al. Public awareness of risk factors and screening for colorectal cancer in Europe. Eur. J. Cancer Prev. 2004, 13, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Wee, C.C.; McCarthy, E.P.; Phillips, R.S. Factors associated with colon cancer screening: The role of patient factors and physician counseling. Prev. Med. 2005, 41, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Berkowitz, Z.; Hawkins, N.A.; Peipins, L.A.; White, M.C.; Nadel, M.R. Beliefs, Risk Perceptions, and Gaps in Knowledge as Barriers to Colorectal Cancer Screening in Older Adults. J. Am. Geriatr. Soc. 2008, 56, 307–314. [Google Scholar] [CrossRef] [PubMed]
- Kroupa, R.; Ondrackova, M.; Kovalcikova, P.; Dastych, M.; Pavlik, T.; Kunovsky, L.; Dolina, J. Viewpoints of the target population regarding barriers and facilitators of colorectal cancer screening in the Czech Republic. World J. Gastroenterol. 2019, 25, 1132–1141. [Google Scholar] [CrossRef] [PubMed]
- Hoeck, S.; Van Roy, K.; Willems, S. Barriers and facilitators to participate in the colorectal cancer screening programme in Flanders (Belgium): A focus group study. Acta Clin. Belg. 2022, 77, 37–44. [Google Scholar] [CrossRef]
- Green, B.B.; BlueSpruce, J.; Tuzzio, L.; Vernon, S.W.; Shay, L.A.; Catz, S.L. Reasons for never and intermittent completion of colorectal cancer screening after receiving multiple rounds of mailed fecal tests. BMC Public Health 2017, 17, 531. [Google Scholar] [CrossRef]
- Benito, L.; Farre, A.; Binefa, G.; Vidal, C.; Cardona, A.; Pla, M.; García, M. Factors related to longitudinal adherence in colorectal cancer screening: Qualitative research findings. Cancer Causes Control 2018, 29, 103–114. [Google Scholar] [CrossRef]
- Christy, S.M.; Schmidt, A.; Wang, H.-L.; Sutton, S.K.; Davis, S.N.; Chavarria, E.; Abdulla, R.; Quinn, G.; Vadaparampil, S.T.; Schultz, I.; et al. Understanding Cancer Worry among Patients in a Community Clinic-Based Colorectal Cancer Screening Intervention Study. Nurs. Res. 2018, 67, 275–285. [Google Scholar] [CrossRef]
- Duncan, A.; Turnbull, D.; Gregory, T.; Cole, S.R.; Young, G.P.; Flight, I.; Wilson, C. Using the Transtheoretical Model of Behaviour Change to describe readiness to rescreen for colorectal cancer with faecal occult blood testing. Health Promot. J. Aust. 2012, 23, 122–128. [Google Scholar] [CrossRef]
- Dominitz, J.A. Barriers and Facilitators to Colorectal Cancer Screening. Gastroenterol. Hepatol. 2021, 17, 550–552. [Google Scholar]
- Ylitalo, K.R.; Camp, B.G.; Meyer, M.R.U.; Barron, L.A.; Benavidez, G.; Hess, B.; Laschober, R.; Griggs, J.O. Barriers and Facilitators of Colorectal Cancer Screening in a Federally Qualified Health Center (FQHC). J. Am. Board Fam. Med. 2019, 32, 180–190. [Google Scholar] [CrossRef] [PubMed]
- Dressler, J.; Johnsen, A.; Madsen, L.; Rasmussen, M.; Jorgensen, L. Factors affecting patient adherence to publicly funded colorectal cancer screening programmes: A systematic review. Public Health 2021, 190, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Kretzler, B.; König, H.-H.; Hajek, A. Religious Attendance and Cancer Screening Behavior. Front. Oncol. 2020, 10, 583925. [Google Scholar] [CrossRef] [PubMed]
- Dharni, N.; Armstrong, D.; Chung-Faye, G.; Wright, A.J. Factors influencing participation in colorectal cancer screening-a qualitative study in an ethnic and socio-economically diverse inner city population. Health Expect. 2017, 20, 608–617. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Roy, S.; Kim, J.; Farazi, P.A.; Siahpush, M.; Su, D. Barriers of colorectal cancer screening in rural USA: A systematic review. Rural Remote Health 2019, 19, 5181. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.P.; Gelb, C.A. Opportunities to Expand Colorectal Cancer Screening Participation. J. Women’s Health 2016, 25, 990–995. [Google Scholar] [CrossRef]
- Gordon, N.P.; Green, B.B. Factors associated with use and non-use of the Fecal Immunochemical Test (FIT) kit for Colorectal Cancer Screening in Response to a 2012 outreach screening program: A survey study. BMC Public Health 2015, 15, 546. [Google Scholar] [CrossRef]
- Clarke, N.; Kearney, P.M.; Gallagher, P.; McNamara, D.; O’Morain, C.A.; Sharp, L. Negative emotions and cancer fatalism are independently associated with uptake of Faecal Immunochemical Test-based colorectal cancer screening: Results from a population-based study. Prev. Med. 2021, 145, 106430. [Google Scholar] [CrossRef]
- Goodwin, B.C.; Crawford-Williams, F.; Ireland, M.J.; March, S. General practitioner endorsement of mail-out colorectal cancer screening: The perspective of nonparticipants. Transl. Behav. Med. 2020, 10, 366–374. [Google Scholar] [CrossRef]
- Berg-Beckhoff, G.; Leppin, A.; Nielsen, J.B. Reasons for participation and non-participation in colorectal cancer screening. Public Health 2022, 205, 83–89. [Google Scholar] [CrossRef]
- Facciorusso, A.; Demb, J.; Mohan, B.P.; Gupta, S.; Singh, S. Addition of Financial Incentives to Mailed Outreach for Promoting Colorectal Cancer Screening: A Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2122581. [Google Scholar] [CrossRef] [PubMed]
- Issaka, R.B.; Avila, P.; Whitaker, E.; Bent, S.; Somsouk, M. Population health interventions to improve colorectal cancer screening by fecal immunochemical tests: A systematic review. Prev. Med. 2019, 118, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.; Dickey, S.; Wang, H.-L.; Washington, A.; Polo, R.; Gwede, C.K.; Luque, J.S. Systematic Review of Interventions to Increase Stool Blood Colorectal Cancer Screening in African Americans. J. Community Health 2021, 46, 232–244. [Google Scholar] [CrossRef] [PubMed]
- Huf, S.W.; Asch, D.A.; Volpp, K.G.; Reitz, C.; Mehta, S.J. Text Messaging and Opt-out Mailed Outreach in Colorectal Cancer Screening: A Randomized Clinical Trial. J. Gen. Intern. Med. 2021, 36, 1958–1964. [Google Scholar] [CrossRef]
- Somsouk, M.; Rachocki, C.; Mannalithara, A.; Garcia, D.; Laleau, V.; Grimes, B.; Issaka, R.B.; Chen, E.; Vittinghoff, E.; Shapiro, J.A.; et al. Effectiveness and Cost of Organized Outreach for Colorectal Cancer Screening: A Randomized, Controlled Trial. J. Natl. Cancer Inst. 2020, 112, 305–313. [Google Scholar] [CrossRef]
- Royal, K.D. Survey research methods: A guide for creating post-stratification weights to correct for sample bias. Educ. Health Prof. 2019, 2, 48. [Google Scholar] [CrossRef]
- European Social Survey. Documentation of ESS Post-Stratification Weights. Available online: https://www.europeansocialsurvey.org/docs/methodology/ESS_post_stratification_weights_documentation.pdf (accessed on 27 October 2022).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).