Uvulopalatopharyngoplasty Versus Expansion Sphincter Pharyngoplasty: A Single Centre Experience
Abstract
1. Introduction
2. Results
2.1. Study Population
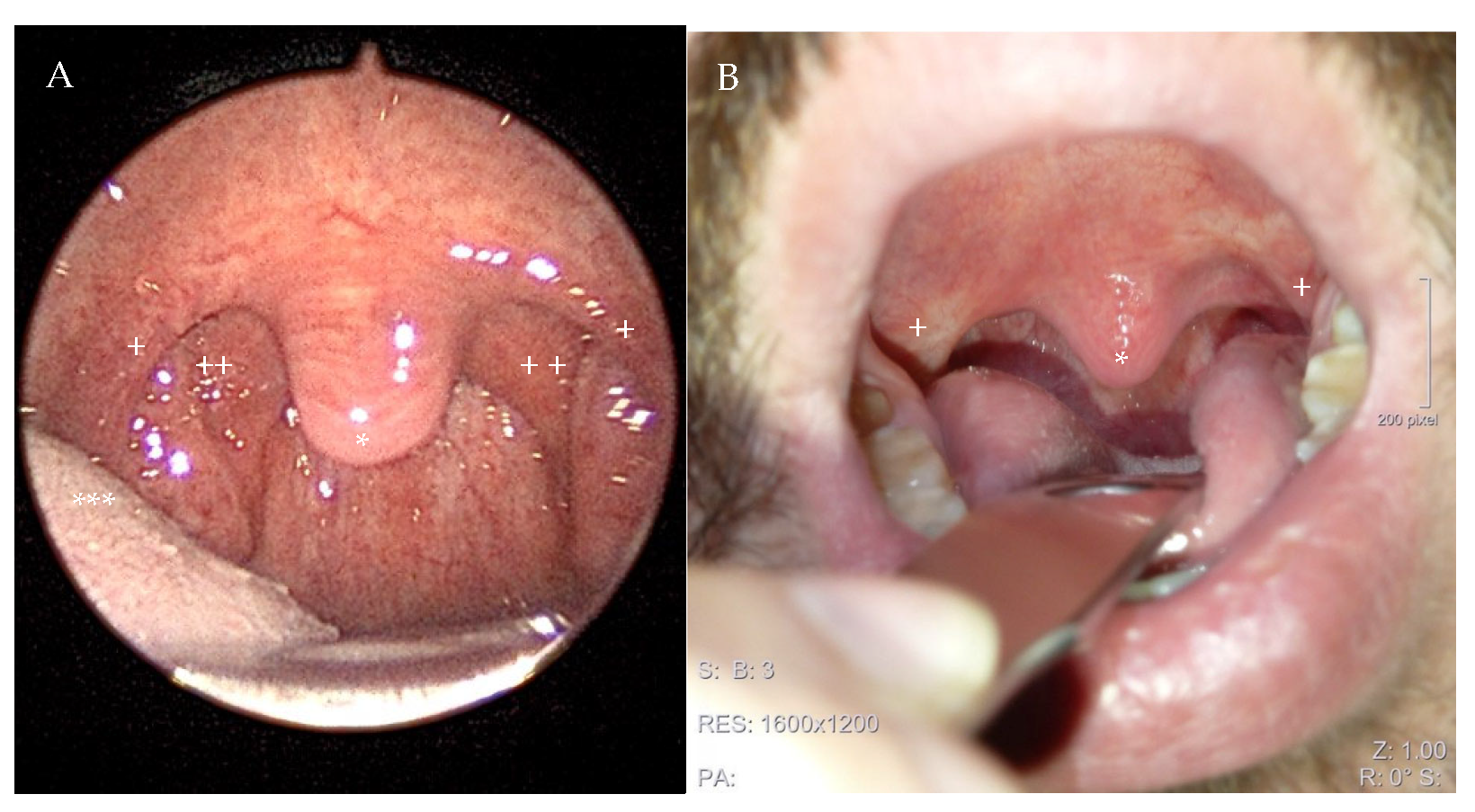
2.2. Surgical Procedure
2.3. Preoperative Sleeping Parameters
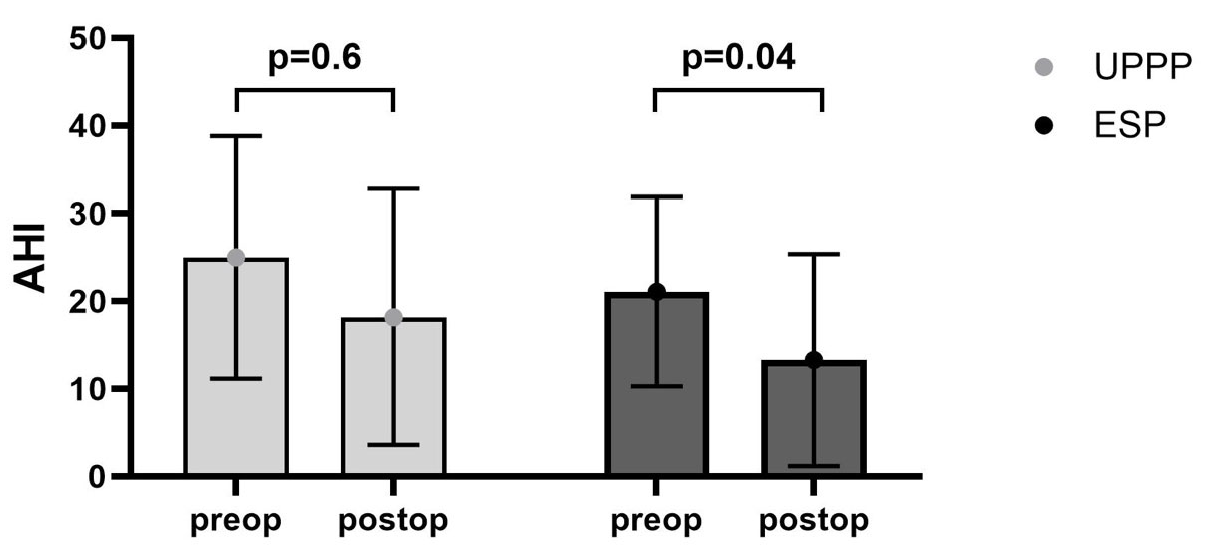
2.4. Postoperative Sleeping Parameters
2.5. Patient Reported Outcome
3. Discussion
4. Materials and Methods
4.1. Surgical Technique
4.2. Data Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vlad, A.M.; Stefanescu, C.D.; Stefan, I.; Zainea, V.; Hainarosie, R. Comparative Efficacy of Velopharyngeal Surgery Techniques for Obstructive Sleep Apnea: A Systematic Review. Medicina 2023, 59, 1147. [Google Scholar] [CrossRef] [PubMed]
- Powell, N.B.; Riley, R.W.; Robinson, A. Surgical management of obstructive sleep apnea syndrome. Clin. Chest Med. 1998, 19, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Riley, R.W.; Powell, N.B.; Guilleminault, C.; Clerk, A.; Troell, R. Obstructive sleep apnea. Trends in therapy. West. J. Med. 1995, 162, 143–148. [Google Scholar] [PubMed]
- Steinbichler, T.B.; Bender, B.; Giotakis, A.I.; Dejaco, D.; Url, C.; Riechelmann, H. Comparison of two surgical suture techniques in uvulopalatopharyngoplasty and expansion sphincter pharyngoplasty. Eur. Arch. Otorhinolaryngol. 2018, 275, 623–628. [Google Scholar] [CrossRef]
- Friedman, M. Sleep Apnea and Snoring: Surgical and Non-Surgical Therapy; Saunders Elsevier Inc.: Amsterdam, The Netherlands, 2009. [Google Scholar]
- Fujita, S.; Conway, W.; Zorick, F.; Roth, T. Surgical correction of anatomic azbnormalities in obstructive sleep apnea syndrome: Uvulopalatopharyngoplasty. Otolaryngol. Head Neck Surg. 1981, 89, 923–934. [Google Scholar] [CrossRef]
- Ikematsu, T. Study of snoring. Therapy. J. Jpn. Otol. Rhinol. Laryngol. Soc. 1964, 64, 434–435. [Google Scholar]
- Iannella, G.; Pace, A.; Magliulo, G.; Vicini, C.; Lugo, R.; Vanderveken, O.M.; de Vries, N.; Pang, K.; Thuler, E.; Jacobowitz, O.; et al. International expert consensus statement: Surgical failure in obstructive sleep apnea. Sleep. Breath. 2024, 28, 2601–2616. [Google Scholar] [CrossRef]
- Stuck, B.A.; Arzt, M.; Fietze, I.; Galetke, W.; Hein, H.; Heiser, C.; Herkenrath, S.D.; Hofauer, B.; Maurer, J.T.; Mayer, G.; et al. Teil-Aktualisierung S3-Leitlinie Schlafbezogene Atmungsstörungen bei Erwachsenen. Somnologie 2020, 24, 176–208. [Google Scholar] [CrossRef]
- Pirsig, W.; Schafer, J.; Yildiz, F.; Nagel, J. Uvulopalatopharyngoplasty without complications: A Fujita complication. Laryngorhinootologie 1989, 68, 585–590. [Google Scholar] [CrossRef]
- Cahali, M.B. Lateral pharyngoplasty: A new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope 2003, 113, 1961–1968. [Google Scholar] [CrossRef]
- Pang, K.P.; Pang, E.B.; Win, M.T.; Pang, K.A.; Woodson, B.T. Expansion sphincter pharyngoplasty for the treatment of OSA: A systemic review and meta-analysis. Eur. Arch. Otorhinolaryngol. 2016, 273, 2329–2333. [Google Scholar] [CrossRef] [PubMed]
- Pang, K.P.; Woodson, B.T. Expansion sphincter pharyngoplasty: A new technique for the treatment of obstructive sleep apnea. Otolaryngol. Head Neck Surg. 2007, 137, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Senaratna, C.V.; Perret, J.L.; Lodge, C.J.; Lowe, A.J.; Campbell, B.E.; Matheson, M.C.; Hamilton, G.S.; Dharmage, S.C. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep. Med. Rev. 2016, 34, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Sarny, S.; Ossimitz, G.; Habermann, W.; Stammberger, H. Hemorrhage following tonsil surgery: A multicenter prospective study. Laryngoscope 2011, 121, 2553–2560. [Google Scholar] [CrossRef]
- Ruehland, W.R.; Rochford, P.D.; O’Donoghue, F.J.; Pierce, R.J.; Singh, P.; Thornton, A.T. The new AASM criteria for scoring hypopneas: Impact on the apnea hypopnea index. Sleep 2009, 32, 150–157. [Google Scholar] [CrossRef]
- Pang, K.P.; Rotenberg, B.W. The SLEEP GOAL as a success criteria in obstructive sleep apnea therapy. Eur. Arch. Otorhinolaryngol. 2016, 273, 1063–1065. [Google Scholar] [CrossRef]
- Mendes, F.A.; Marone, S.A.; Duarte, B.B.; Arenas, A.C. Epidemiologic profile of patients with snoring and obstructive sleep apnea in a university hospital. Int. Arch. Otorhinolaryngol. 2014, 18, 142–145. [Google Scholar] [CrossRef]
- Pepin, J.L.; Woehrle, H.; Liu, D.; Shao, S.; Armitstead, J.P.; Cistulli, P.A.; Benjafield, A.V.; Malhotra, A. Adherence to Positive Airway Therapy After Switching From CPAP to ASV: A Big Data Analysis. J. Clin. Sleep. Med. 2018, 14, 57–63. [Google Scholar] [CrossRef]
- Veasey, S.C.; Rosen, I.M. Obstructive Sleep Apnea in Adults. N. Engl. J. Med. 2019, 380, 1442–1449. [Google Scholar] [CrossRef]
- Sommer, U.J.; Heiser, C.; Gahleitner, C.; Herr, R.M.; Hormann, K.; Maurer, J.T.; Stuck, B.A. Tonsillectomy with Uvulopalatopharyngoplasty in Obstructive Sleep Apnea. Dtsch. Arztebl. Int. 2016, 113, 1–8. [Google Scholar] [CrossRef]
- Vanderveken, O.M.; Maurer, J.T.; Hohenhorst, W.; Hamans, E.; Lin, H.S.; Vroegop, A.V.; Anders, C.; de Vries, N.; Van de Heyning, P.H. Evaluation of drug-induced sleep endoscopy as a patient selection tool for implanted upper airway stimulation for obstructive sleep apnea. J. Clin. Sleep. Med. 2013, 9, 433–438. [Google Scholar] [CrossRef]
- Remmers, J.E.; deGroot, W.J.; Sauerland, E.K.; Anch, A.M. Pathogenesis of upper airway occlusion during sleep. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 1978, 44, 931–938. [Google Scholar] [CrossRef]
- Gan, Y.J.; Lim, L.; Chong, Y.K. Validation study of WatchPat 200 for diagnosis of OSA in an Asian cohort. Eur. Arch. Otorhinolaryngol. 2017, 274, 1741–1745. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Kwon, S.H.; Lee, E.J.; Yoon, Y.J. Can Intracapsular Tonsillectomy Be an Alternative to Classical Tonsillectomy? A Meta-analysis. Otolaryngol. Head Neck Surg. 2017, 157, 178–189. [Google Scholar] [CrossRef] [PubMed]
- Maniaci, A.; Di Luca, M.; Lechien, J.R.; Iannella, G.; Grillo, C.; Grillo, C.M.; Merlino, F.; Calvo-Henriquez, C.; De Vito, A.; Magliulo, G.; et al. Lateral pharyngoplasty vs. traditional uvulopalatopharyngoplasty for patients with OSA: Systematic review and meta-analysis. Sleep. Breath. 2022, 26, 1539–1550. [Google Scholar] [CrossRef] [PubMed]
- Vicini, C.; Hendawy, E.; Campanini, A.; Eesa, M.; Bahgat, A.; AlGhamdi, S.; Meccariello, G.; DeVito, A.; Montevecchi, F.; Mantovani, M. Barbed reposition pharyngoplasty (BRP) for OSAHS: A feasibility, safety, efficacy and teachability pilot study. “We are on the giant’s shoulders”. Eur. Arch. Otorhinolaryngol. 2015, 272, 3065–3070. [Google Scholar] [CrossRef]
- Emara, T.A.; Elmonem, M.; Khaled, A.M.; Genedy, H.A.H.; Youssef, R.S. Anterolateral advancement pharyngoplasty versus barbed reposition pharyngoplasty in patients with obstructive sleep apnea. Eur. Arch. Otorhinolaryngol. 2024, 281, 1991–2000. [Google Scholar] [CrossRef]
- Emara, T.A.; Hassan, M.H.; Mohamad, A.S.; Anany, A.M.; Ebrahem, A.E. Anterolateral Advancement Pharyngoplasty: A New Technique for Treatment of Obstructive Sleep Apnea. Otolaryngol. Head Neck Surg. 2016, 155, 702–707. [Google Scholar] [CrossRef]
- De Vito, A.; Carrasco Llatas, M.; Ravesloot, M.J.; Kotecha, B.; De Vries, N.; Hamans, E.; Maurer, J.; Bosi, M.; Blumen, M.; Heiser, C.; et al. European position paper on drug-induced sleep endoscopy: 2017 Update. Clin. Otolaryngol. 2018, 43, 1541–1552. [Google Scholar] [CrossRef]
- Stuck, B.A.; Kopke, J.; Hormann, K.; Verse, T.; Eckert, A.; Bran, G.; Duber, C.; Maurer, J.T. Volumetric tissue reduction in radiofrequency surgery of the tongue base. Otolaryngol. Head Neck Surg. 2005, 132, 132–135. [Google Scholar] [CrossRef]
- Bender, B.; Blassnigg, E.C.; Bechthold, J.; Kral, F.; Riccabona, U.; Steinbichler, T.; Riechelmann, H. Microdebrider-assisted intracapsular tonsillectomy in adults with chronic or recurrent tonsillitis. Laryngoscope 2015, 125, 2284–2290. [Google Scholar] [CrossRef]

| Variable | Value | Count | Percent |
|---|---|---|---|
| Sex | female | 16 | 14% |
| male | 98 | 86% | |
| Age | ≤30 | 21 | 18% |
| 31–40 | 30 | 26% | |
| 41–50 | 38 | 33% | |
| ≥51 | 25 | 22% | |
| BMI (in kg/m2) | underweight (<18.5 kg/m2) | 2 | 2% |
| normal (18.5–25 kg/m2) | 18 | 16% | |
| Overweight (25–30 kg/m2) | 64 | 56% | |
| Obese (>30 kg/m2) | 30 | 26% | |
| Smoking | yes | 46 | 40% |
| no | 60 | 53% | |
| missing | 8 | 7% | |
| OSA-severity | Non (AHI * < 5/h) | 30 | 26% |
| Mild (AHI 5–15/h) | 34 | 30% | |
| Moderate (AHI 15–30/h) | 26 | 23% | |
| Severe (AHI > 30/h) | 14 | 12% | |
| Missing | 10 | 9% | |
| Surgical procedure | UPPP | 43 | 38% |
| ESP | 71 | 62% | |
| Radiofrequency ablation of the tongue base | yes | 52 | 46% |
| no | 62 | 54% | |
| tonsillectomy | yes | 104 | 91% |
| no | 10 | 9% |
| Variable | Value | UPPP (n = 43) | ESP (n = 71) * |
|---|---|---|---|
| Tonsillar size (Brodksy classification) | 0 | 1 (2%) | 2 (3%) |
| 1 | 14 (33%) | 24 (34%) | |
| 2 | 21 (49%) | 28 (39%) | |
| 3 | 5 (12%) | 4 (6%) | |
| 4 | 2 (5%) | 3 (4%) | |
| BMI (in kg/m2) | underweight (<18.5 kg/m2) | 1 (2%) | 1 (1%) |
| normal (18.5–25 kg/m2) | 9 (21%) | 9 (13%) | |
| Overweight (25–30 kg/m2) | 21 (49%) | 43 (60%) | |
| Obese (>30 kg/m2) | 12 (28%) | 18 (25%) |
| ESP | UPPP | |
|---|---|---|
| total patient count | 71 | 43 |
| AHI * preoperative | 21.1 ± 10.8/h | 25.0 ± 13.8/h |
| AHI * postoperative | 13.3 ± 12.1/h | 18.2 ± 14.6/h |
| p value | 0.04 | 0.6 |
| success rate ** | 41% | 27% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steinbichler, T.B.; Bender, B.; Hartl, R.; Strasser, V.; Sontheimer, D.; Buricic, S.; Kofler, B.; Högl, B.; Riechelmann, H.; Hofauer, B. Uvulopalatopharyngoplasty Versus Expansion Sphincter Pharyngoplasty: A Single Centre Experience. Clocks & Sleep 2025, 7, 38. https://doi.org/10.3390/clockssleep7030038
Steinbichler TB, Bender B, Hartl R, Strasser V, Sontheimer D, Buricic S, Kofler B, Högl B, Riechelmann H, Hofauer B. Uvulopalatopharyngoplasty Versus Expansion Sphincter Pharyngoplasty: A Single Centre Experience. Clocks & Sleep. 2025; 7(3):38. https://doi.org/10.3390/clockssleep7030038
Chicago/Turabian StyleSteinbichler, Teresa Bernadette, Birte Bender, Roland Hartl, Verena Strasser, Daniel Sontheimer, Sladjana Buricic, Barbara Kofler, Birgit Högl, Herbert Riechelmann, and Benedikt Hofauer. 2025. "Uvulopalatopharyngoplasty Versus Expansion Sphincter Pharyngoplasty: A Single Centre Experience" Clocks & Sleep 7, no. 3: 38. https://doi.org/10.3390/clockssleep7030038
APA StyleSteinbichler, T. B., Bender, B., Hartl, R., Strasser, V., Sontheimer, D., Buricic, S., Kofler, B., Högl, B., Riechelmann, H., & Hofauer, B. (2025). Uvulopalatopharyngoplasty Versus Expansion Sphincter Pharyngoplasty: A Single Centre Experience. Clocks & Sleep, 7(3), 38. https://doi.org/10.3390/clockssleep7030038






