Mindfulness, Subjective Cognitive Functioning, Sleep Timing and Time Expansion during COVID-19 Lockdown: A Longitudinal Study in Italy
Abstract
1. Introduction
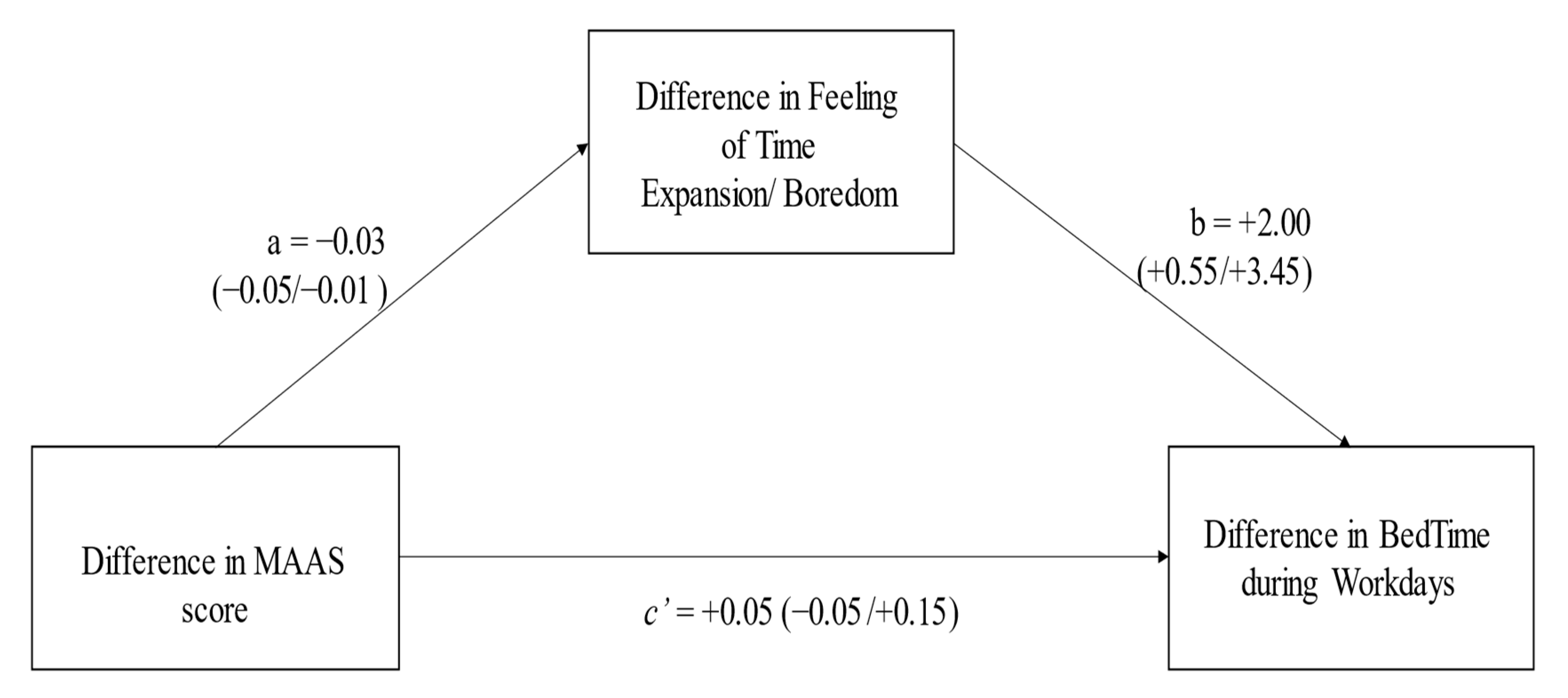
2. Results
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. Materials
4.3. Procedure
4.4. Data Analysis
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Report of the WHO—China Joint Mission on Coronavirus Disease 2019 (COVID-19); World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19) (accessed on 2 March 2023).
- World Health Organization. Novel Coronavirus (2019—nCoV): Situation Report-10; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200130-sitrep-10-ncov.pdf?sfvrsn=d0b2e480_2 (accessed on 2 March 2023).
- World Health Organization. WHO Timeline on COVID-19; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/news-room/detail/27-04-2020-who-timeline---COVID-19 (accessed on 2 March 2023).
- Balanzá-Martínez, V.; Atienza-Carbonell, B.; Kapczinski, F.; De Boni, R.B. Lifestyle behaviours during the COVID-19—Time to connect. Acta Psychiatr. Scand. 2020, 141, 399–400. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, K.M.; Harris, C.; Drawve, G. Fear of COVID-19 and the mental health consequences in America. Psychol. Trauma 2020, 12, S17–S21. [Google Scholar] [CrossRef] [PubMed]
- Lau, H.; Khosrawipour, V.; Kocbach, P.; Mikolajczyk, A.; Schubert, J.; Bania, J.; Khosrawipour, T. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in Chine. J. Travel Med. 2020, 27, taaa037. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological impact of COVID-19 in Spain: Early data report. Psychol. Trauma 2020, 12, 550–552. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatr. 2020, 11, 790. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological response and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Blume, C.; Schmidt, M.H.; Cajochen, C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr. Biol. 2020, 30, R783–R801. [Google Scholar] [CrossRef]
- Chen, P.J.; Pusica, Y.; Sohaei, D.; Prassas, I.; Diamandis, E.P. An overview of mental health during the COVID-19 pandemic. Diagnosis 2021, 8, 403–412. [Google Scholar] [CrossRef]
- Fiorenzato, E.; Zabberoni, S.; Costa, A.; Cona, G. Cognitive and mental health changes and their vulnerability factors related to COVID-19 lockdown in Italy. PLoS ONE 2021, 16, e0246204. [Google Scholar] [CrossRef]
- Ingram, J.; Hand, C.J.; Maciejewski, G. Social isolation during COVID-19 lockdown impairs cognitive function. Appl. Cognit. Psychol. 2021, 35, 935–947. [Google Scholar] [CrossRef]
- Lee, Y.; Lui, L.M.W.; Chen-Li, D.; Lia, Y.; Mansur, R.B.; Brietzke, E.; Rosenblat, J.D.; Ho, R.; Rodrigues, N.B.; Lipsitz, O.; et al. Government response moderates the mental health impact of COVID-19: A systematic review and meta-analysis of depression outcomes across countries. J. Affect. Disord. 2021, 290, 364–377. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.A.; Alhaj, O.A.; Humood, A.M.; Alenezi, A.F.; Fekih-Romdhare, F.; AlRasheed, M.M.; Saif, Z.Q.; Bragazzi, N.L.; Oandi-Perumal, S.R.; BaHammam, A.S.; et al. Sleep disturbances during the COVID-19 pandemic: A systematic review, meta-analysis, and meta-regression. Sleep Med. Rev. 2022, 62, 101591. [Google Scholar] [CrossRef] [PubMed]
- Kira, I.A.; Alpay, E.H.; Ayna, Y.E.; Shuwiekh, H.A.M.; Ashby, J.S.; Turkeli, A. The effects of COVID-19 continuous traumatic stressors on mental health and cognitive functioning: A case example from Turkey. Curr. Psychol. 2022, 41, 7371–7382. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, J.; Gerardo, B.; Silva, A.R.; Pinto, P.; Barbosa, R.; Soares, S.; Baptista, B.; Paquete, C.; Cabral-Pinto, M.; Vilar, M.M.; et al. Effects of restraining measures due to COVID-19: Pre-and post-lockdown cognitive status and mental health. Curr. Psychol. 2022, 41, 7383–7392. [Google Scholar] [CrossRef] [PubMed]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef] [PubMed]
- Droit-Volet, S.; Gil, S.; Martinelli, N.; Andant, N.; Clinchamps, M.; Parreira, L.; Rouffiac, K.; Dambrun, M.; Huguet, P.; Dubuis, B.; et al. Time and COVID-19 stress in the lockdown situation: Time free “Dying” of boredom and sadness. PLoS ONE 2020, 15, e0236465. [Google Scholar] [CrossRef]
- Ogden, R.S. The passage of time during the UK COVID-19 lockdown. PLoS ONE 2020, 15, e0235871. [Google Scholar] [CrossRef]
- Sobol, M.; Blachnio, A.; Przepiórka, A. Time of pandemic: Temporal perspectives related to compliance with public health regulations concerning the COVID-19 pandemic. Soc. Sci. Med. 2020, 265, 113408. [Google Scholar] [CrossRef]
- Torboli, D.; Mioni, G.; Busse, C.; Cagnin, A.; Vallesi, A. Subjective experience of time in dementia with Lewy bodies during COVID-19 lockdown. Curr. Psychol. 2023, 42, 4653–4662. [Google Scholar] [CrossRef]
- Ogden, R. Distorsions to the passage of time during England’s second national lockdown: A role for depression. PLoS ONE 2021, 16, e0250412. [Google Scholar] [CrossRef]
- Wittmann, M. Subjective passage of time during the pandemic: Routine, boredom, and memory. KronoScope 2020, 20, 260–271. [Google Scholar] [CrossRef]
- Droit-Volet, S.; Martinelli, N.; Chevalère, J.; Belletier, C.; Dezecache, G.; Gil, S.; Huguet, P. The persistence of slowed time experience during the COVID-19 pandemic: Two longitudinal studies in France. Front. Psychol. 2021, 12, 721716. [Google Scholar] [CrossRef] [PubMed]
- Martinelli, N.; Gil, S.; Bellertier, C.; Chevalère, J.; Dezecache, G.; Huguet, P.; Droit-Volet, S. Time and emotion during lockdown and the COVID-19 epidemic determinants of our experience of time? Front. Psychol. 2021, 11, 616169. [Google Scholar] [CrossRef] [PubMed]
- Martinelli, N.; Gil, S.; Chevalère, J.; Dezecache, G.; Huguet, P.; Droit-Volet, S. The impact of the COVID-19 pandemic on vulnerable people suffering from depression: Two studies on adults in France. Int. J. Environ. Res. Public Health 2021, 18, 3250. [Google Scholar] [CrossRef] [PubMed]
- Isham, E.A.; Lomayesva, S.; Teng, J. Time estimation and passage of time judgment predict eating behaviors during COVID-19 lockdown. Front. Psychol. 2022, 13, 961092. [Google Scholar] [CrossRef]
- Wessels, M.; Utegaliyev, N.; Bernhard, C.; Welsch, R.; Oberfeld, D.; Thönes, S.; von Castell, C. Adapting to the pandemic: Longitudinal effects of social restrictions on time perception and boredom during the COVID-19 pandemic in Germany. Sci. Rep. 2022, 12, 1863. [Google Scholar] [CrossRef]
- Kosak, F.; Schelhorn, I.; Wittmann, M. The subjective experience of time during the pandemic in Germany: The big slowdown. PLoS ONE 2022, 17, e0267709. [Google Scholar] [CrossRef]
- Meng, F.; Xuan, B. Boredom proneness on Chinese college students’ phubbing during the COVID-19 outbreak: The mediating effects of self-control and bedtime procrastination. J. Heathc Eng. 2023, 2023, 4134283. [Google Scholar] [CrossRef]
- Ma, X.; Meng, D.; Zhu, L.; Xu, H.; Guo, J.; Yang, L.; Yu, L.; Fu, Y.; Mu, L. Bedtime procrastination predicts the prevalence and severity of poor sleep quality of Chinese undergraduate students. J. Am. Coll. Health 2022, 70, 1104–1111. [Google Scholar] [CrossRef]
- Zavada, A.; Gordijn, M.C.M.; Beersma, D.G.M.; Daan, S.; Roenneberg, T. Comparison of the Munich Chronotype questionnaire with the Horne-Ostberg’s Morningness-Eveningness score. Chronobiol. Int. 2005, 22, 267–278. [Google Scholar] [CrossRef]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; Dutil, C.; Featherstone, R.; Ross, R.; Giangregorio, L.; Saunders, T.J.; Janssen, I.; Poitras, V.J.; Kho, M.E.; Ross-White, A.; et al. Sleep timing, sleep consistency, and health in adults: A systematic review. Appl. Physiol. Nutr. Metab. 2020, 45, S232–S247. [Google Scholar] [CrossRef] [PubMed]
- Adan, A.; Archer, S.N.; Hidalgo, M.P.; Di Milia, L.; Natale, V.; Randler, C. Circadian typology: A comprensive review. Chronobiol. Int. 2012, 29, 1153–1175. [Google Scholar] [CrossRef] [PubMed]
- Myers, P.M.; Tilley, A. The relationship between diurnal type and time duration estimation at morning and evening times of day. Pers. Individ. Differ. 2003, 35, 1141–1150. [Google Scholar] [CrossRef]
- Esposito, M.J.; Natale, V.; Martoni, M.; Occhionero, M.; Fabbri, M.; Cicogna, P.C. Prospective time estimation over a night without sleep. Biol. Rhythm Res. 2007, 38, 443–450. [Google Scholar] [CrossRef]
- Stolarski, M.; Ledzińska, M.; Matthews, G. Morning is tomorrow, evening is today: Relationship between chronotype and time perspective. Biol. Rhythm Res. 2013, 44, 181–196. [Google Scholar] [CrossRef]
- Nowack, K.; van der Meer, E. Are larks future-oriented and owls presente-oriented? Age and sex-related shifts in chronotype-time perspective associations. Chronobiol. Int. 2013, 30, 1240–1250. [Google Scholar] [CrossRef]
- Milfont, M.I.; Schwarzenthal, M. Explaining why larks are future-oriented and owls are present-oriented: Self-control mediates the chronotype-time perspective relationships. Chronobiol. Int. 2014, 31, 581–583. [Google Scholar] [CrossRef]
- Nowack, K.; van der Meer, E. Impact of chronotype and time perspective on the processing of scripts. Int. J. Psychophysiol. 2014, 92, 49–58. [Google Scholar] [CrossRef]
- McGowan, N.M.; Brannigan, R.; Doyle, D.; Coogan, A.N. Diurnal preference, circadian phase of entrainment and time perspectives: Just what are the relationship? Pers. Individ. Differ. 2017, 112, 79–84. [Google Scholar] [CrossRef]
- Beracci, A.; Fabbri, M.; Martoni, M. Morningness-eveningness preference, time perspective, and passage of time judgments. Cogn. Sci. 2022, 46, e13109. [Google Scholar] [CrossRef]
- Depner, C.M.; Melanson, E.L.; Eckel, R.H.; Snell-Bergeon, J.K.; Perreault, L.; Bergman, B.C.; Higgins, J.A.; Guerin, M.K.; Stothard, E.R.; Morton, S.J.; et al. Ad libitum weekend recovery sleep fails to prevent metabolic dysregulation during a repeating pattern of insufficient sleep and weekend recovery sleep. Curr. Biol. 2019, 29, 957–967. [Google Scholar] [CrossRef] [PubMed]
- Marelli, S.; Castelnuovo, A.; Somma, A.; Castronovo, V.; Mombelli, S.; Bottoni, D.; Leither, C.; Fossati, A.; Ferini-Strambi, L. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J. Neurol. 2021, 268, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Salfi, F.; Lauriola, M.; D’Atri, A.; Amicucci, G.; Viselli, L.; Tempesta, D.; Ferrara, M. Demographic, psychological, chronobiological, and work-related predictors of sleep disturbances during the COVID-19 lockdown in Italy. Sci. Rep. 2021, 11, 11416. [Google Scholar] [CrossRef]
- Salfi, F.; D’Atri, A.; Amicucci, G.; Viselli, L.; Gorgoni, M.; Scarpelli, S.; Alfonsi, V.; Ferrara, M. The fall of vulnerability to sleep disturbances in evening chronotypes when working from home and its implications for depression. Sci. Rep. 2022, 12, 12249. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life; Hyperion Books: New York, NY, USA, 1994. [Google Scholar]
- Bishop, S.R. Mindfulness: A proposed operational definition. Clin. Psychol. Sci. Pract. 2004, 11, 230–241. [Google Scholar] [CrossRef]
- Brown, K.W.; Ryan, R.M. The benefits of being present: Mindfulness and its role in psychological well-being. J. Personal. Soc. Psychol. 2003, 84, 822–848. [Google Scholar] [CrossRef]
- Rau, H.K.; Williams, P.G. Dispositional mindfulness: A critical review of construct validation research. Personal. Individ. Differ. 2016, 93, 32–43. [Google Scholar] [CrossRef]
- Hunter, A.; Eastwood, J.D. Does state boredom cause failures of attention? Examining the relation between trail boredom, state boredom, and sustained attention. Exp. Brain Res. 2018, 236, 2483–2492. [Google Scholar] [CrossRef]
- Berkovic-Ohana, A.; Glicksohn, J.; Goldstein, A. Mindfulness induced changes in gamma band activity-implications for the default mode network, self-reference and attention. Clin. Neurophysiol. 2012, 123, 700–710. [Google Scholar] [CrossRef]
- Kramer, R.S.S.; Weger, U.W.; Sharma, D. The effect of mindfulness meditation on time perception. Coscious. Cogn. 2013, 22, 846–852. [Google Scholar] [CrossRef] [PubMed]
- Sucala, M.; David, D. Mindful about time in a fast forward world. The effects of mindfulness exercise on time perception. Transl. J. Psychol. 2013, 14, 243–253. [Google Scholar]
- Wittmann, M.; Peter, J.; Gutina, O.; Otten, S.; Kohls, N.; Meisssner, K. Individual differences in self-attributed mindfulness levels are related to the experience of time and cognitive self-control. Personal. Individ. Differ. 2014, 64, 41–45. [Google Scholar] [CrossRef]
- Droit-Volet, S.; Fanget, M.; Dambrum, M. Mindfulness meditation and relaxation training increases time sensitivity. Conscious. Cogn. 2015, 31, 86–97. [Google Scholar] [CrossRef]
- Wittmann, M.; Otten, S.; Schötz, E.; Sarikaya, A.; Lehnen, H.; Jo, H.-G.; Kohls, N.; Schmidt, S.; Meissner, K. Subjective expansion of extended time-spans in experienced meditators. Front. Psychol. 2015, 5, 1589. [Google Scholar] [CrossRef]
- Welner, L.; Wittmann, M.; Bertschy, G.; Glersch, A. Dispositional mindfulness and subjective time in healthy individuals. Front. Psychol. 2016, 7, 786. [Google Scholar] [CrossRef]
- Droit-Volet, S.; Chaulet, M.; Dutheil, F.; Dambrum, M. Mindfulness meditation, time judgment and time experience: Importance of the time scale considered (seconds or minutes). PLoS ONE 2019, 14, e0223567. [Google Scholar] [CrossRef]
- Droit-Volet, S.; Heros, J. Time judgments as a function of mindfulness meditation, anxiety and mindfulness awareness. Mindfulness 2017, 8, 266–275. [Google Scholar] [CrossRef]
- Droit-Volet, S.; Chaulet, C.; Dambrun, M. Time and meditation: When does the perception of time change with mindfulness exercise? Mindfulness 2018, 9, 1557–1570. [Google Scholar] [CrossRef]
- Droit-Volet, S.; Dambrun, M. Awareness of the passage of time and self-consciousness: What do meditators report? Psych J. 2019, 8, 51–65. [Google Scholar] [CrossRef]
- Shallcross, A.J.; Visvanathan, P.D.; Sperber, S.H.; Duberstein, Z.T. Waking up to the problem of sleep: Can mindfulness help? A review of theory and evidence for the effects of mindfulness for sleep. Curr. Opin. Psychol. 2019, 13, 37–41. [Google Scholar] [CrossRef]
- Mirolli, M.; Simione, L.; Martoni, M.; Fabbri, M. Accept anxiety to improve sleep: The impact of the COVID-19 lockdown on the relationships between mindfulness, distress and sleep quality. Int. J. Environ. Res. Public Health 2021, 18, 13149. [Google Scholar] [CrossRef] [PubMed]
- Fabbri, M.; Simione, L.; Martoni, M.; Mirolli, M. The relationship between acceptance and sleep-wake quality before, during, and after the first Italian COVID-19 lockdown. Clocks Sleep 2022, 4, 172–184. [Google Scholar] [CrossRef]
- Teoh, A.N.; Wong, J.W.K. Mindfulness is associated with better sleep quality in young adults by reducing boredom and bedtime procrastination. Behav. Sleep Med. 2023, 21, 61–71. [Google Scholar] [CrossRef]
- Smith, G.V.; Della Sala, S.; Logie, R.H.; Maylor, E.A.M. Prospective and retrospective memory in normal ageing and dementia: A questionnaire study. Memory 2000, 8, 311–321. [Google Scholar] [CrossRef]
- Maylor, E.A.; Smith, G.; Della Sala, S.; Logie, R.H. Prospective and retrospective memory in normal aging and dementia: An experimental study. Mem. Cognit. 2002, 30, 871–884. [Google Scholar] [CrossRef]
- Waldum, E.R.; Sahakyan, L. A role for memory in prospective timing informs timing in prospective memory. J. Exp. Psychol. Gen. 2013, 142, 809–826. [Google Scholar] [CrossRef]
- Hicks, R.; Miller, G.; Kinsbourne, M. Prospective and retrospective judgments of time as a function of amount of information processed. Am. J. Psychol. 1976, 89, 719–730. [Google Scholar] [CrossRef]
- Wearden, J.H. Passage of time judgements. Conscious. Cogn. 2015, 38, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Block, R.A.; Zakay, D. Prospective remembering involves time estimation and memory processes. In Timing the Future. The Case for a Time-Based Prospective Memory; Glicksohn, J., Myslobodsky, M.S., Eds.; World Scientific Publishing, Tuck Link: Singapore, 2006; pp. 25–50. [Google Scholar]
- Tonetti, L.; Occhionero, M.; Boreggiani, M.; Conca, A.; Dondi, P.; Elbaz, M.; Fabbri, M.; Gauriau, C.; Giupponi, G.; Leger, D.; et al. Sleep and prospective memory: A retrospective study in different clinical populations. Int. J. Environ. Res. Public Health 2020, 17, 6113. [Google Scholar] [CrossRef] [PubMed]
- Borbély, A.A.; Daan, S.; Wirz-Justice, A.; Deboer, T. The two-process model of sleep regulation: A reappraisal. J. Sleep Res. 2016, 25, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Bzdok, D.; Dunbar, R.I.M. The neurobiology of social distance. Trends Cogn. Sci. 2020, 24, 717–733. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.; Smith, G.; Maylor, E.; Della Sala, S.; Logie, R. The Prospective and Retrospective Memory Questionnaire (PRMQ): Normative data and latent structure in a large non-clinical sample. Memory 2003, 11, 261–275. [Google Scholar] [CrossRef]
- Huang, T.; Redline, S. Cross-sectional and prospective associations of actigraphy-assessed sleep regularity with metabolic abnormalities: The multi-ethnic study of atherosclerosis. Diabetes Care 2019, 42, 1422–1429. [Google Scholar] [CrossRef] [PubMed]
- Concenas-Silva, R.; Droit-Volet, S.; Gherardi-Donato, E.C.S. Chronic stress impairs temporal memory. Timing Time Percept. 2019, 7, 108–130. [Google Scholar] [CrossRef]
- Park, T.; Reilly-Spong, M.; Gross, C.R. Mindfulness: A systematic review of instruments to measure an emergent patient reported outcome (PRO). Qual. Life Res. 2013, 22, 2639–2659. [Google Scholar] [CrossRef]
- Agorastosand, A.; Olff, M. Traumatic stress and the circadian system: Neurobiology, timing and treatment of posttraumatic chronodisruption. Eur. J. Psychotraumatol. 2020, 11, 1833644. [Google Scholar] [CrossRef]
- Schwartze, M.M.; Frenzel, A.C.; Goetz, T.; Pekrun, R.; Reck, C.; Marx, A.K.G.; Fiedler, D. Boredom makes me sick: Adolescents’ boredom trajectories and their health-related quality of life. Int. J. Environ. Res. Public Health 2021, 18, 6308. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Veneziani, C.A.; Voci, A. The Italian adaptation of the Mindful Awareness Attention Scale and its relation with individual differences and quality of life indexes. Mindfulness 2015, 6, 373–381. [Google Scholar] [CrossRef]
- Baminiwatta, A.; Solangaarachchi, I. Trends and developments in mindfulness research over 55 years: A bibliometric analysis of publications indexed in web of science. Mindfulness 2021, 12, 2099–2116. [Google Scholar] [CrossRef] [PubMed]
- Randler, C.; Kretz, S. Associative mating in morningness-eveningness. Int. J. Psychol. 2011, 46, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Natale, V. Validazione di una scala ridotta di mattutinità (rMEQ) [Validation of a reduced scale of Morningness-Eveningness Questionnaire (rMEQ)]. Bolletino Di Psicol. Appl. 1999, 229, 19–26. [Google Scholar]
- Natale, V.; Esposito, M.J.; Martoni, M.; Fabbri, M. Validity of the reduced version of the Morningness-Eveningness Questionnaire. Sleep Biol. Rhythm 2006, 4, 72–74. [Google Scholar] [CrossRef]
- Wittmann, M.; Lehnhoff, S. Age effects in perception of time. Psychol. Rep. 2005, 97, 921–935. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Wen, Z.; Ye, B. Analyses of mediating effects: The development of methods and models. Adv. Psychol. Sci. 2014, 22, 731–745. [Google Scholar] [CrossRef]
| Pre-Lockdown | During Lockdown | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Chronotypes | M | SD | M | SD | F | p = | η2p |
| MAAS score | Evening-types | 62.00 | 14.67 | 60.40 | 16.28 | 0.26 | 0.77 | 0.01 |
| Intermediate-types | 59.38 | 9.11 | 56.71 | 10.47 | ||||
| Morning-types | 63.63 | 13.58 | 56.38 | 19.91 | ||||
| Mean Survey Time | 61.67 | 12.45 | 58.83 | 15.53 | 4.11 | 0.05 | 0.10 | |
| Retrospective score | Evening-types | 30.60 | 8.68 | 30.80 | 10.60 | 0.06 | 0.94 | 0.003 |
| Intermediate-types | 31.19 | 9.49 | 31.19 | 8.36 | ||||
| Morning-types | 27.75 | 13.60 | 32.00 | 13.05 | ||||
| Mean Survey Time | 29.89 | 10.59 | 31.33 | 10.67 | 1.25 | 0.27 | 0.03 | |
| Prospective score | Evening-types | 32.60 | 10.06 | 35.40 | 16.12 | 0.13 | 0.88 | 0.007 |
| Intermediate-types | 33.81 | 7.74 | 35.00 | 10.52 | ||||
| Morning-types | 35.00 | 10.74 | 37.38 | 14.07 | ||||
| Mean Survey Time | 33.80 | 9.51 | 35.93 | 13.57 | 1.44 | 0.24 | 0.04 | |
| Total PRMQ score | Evening-types | 30.80 | 9.40 | 32.50 | 13.93 | 0.01 | 0.99 | 0.001 |
| Intermediate-types | 31.71 | 8.55 | 32.52 | 10.00 | ||||
| Morning-types | 30.38 | 12.97 | 34.13 | 14.40 | ||||
| Mean Survey Time | 30.96 | 10.31 | 33.05 | 12.78 | 1.99 | 0.17 | 0.05 | |
| BedTime Workdays (hh:mm) | Evening-types | 01:32 | 01:13 | 03:24 | 02:51 | 2.45 | 0.10 | 0.12 |
| Intermediate-types | 24:16 | 01:16 | 01:43 | 02:33 | ||||
| Morning-types | 23:03 | 01:41 | 02:41 | 05:02 | ||||
| Mean Survey Time | 24:17 | 01:21 | 02:36 | 03:29 | 16.32 | 0.0001 | 0.31 | |
| Wake-UP Time Workdays (hh:mm) | Evening-types | 09:12 | 01:52 | 11:22 | 03:05 | 1.72 | 0.19 | 0.09 |
| Intermediate-types | 08:25 | 01:52 | 09:43 | 02:39 | ||||
| Morning-types | 06:30 | 01:04 | 10:57 | 04:41 | ||||
| Mean Survey Time | 08:02 | 01:36 | 10:41 | 03:28 | 20.03 | 0.0001 | 0.36 | |
| BedTime Free days (hh:mm) | Evening-types | 02:36 | 01:32 | 02:15 | 01:47 | 3.76 | 0.033 | 0.17 |
| Intermediate-types | 01:58 | 01:46 | 01:47 | 01:33 | ||||
| Morning-types | 24:53 | 02:11 | 24:08 | 01:33 | ||||
| Mean Survey Time | 01:49 | 01:50 | 01:23 | 01:38 | 2.46 | 0.13 | 0.06 | |
| Wake-UP Time Free days (hh:mm) | Evening-types | 10:54 | 02:01 | 10:30 | 03:25 | 1.07 | 0.36 | 0.06 |
| Intermediate-types | 10:25 | 02:05 | 09:34 | 02:32 | ||||
| Morning-types | 09:21 | 02:14 | 09:04 | 01:43 | ||||
| Mean Survey Time | 10:13 | 02:07 | 09:43 | 02:34 | 1.96 | 0.17 | 0.05 | |
| Time In Bed Workdays (Sleep Duration Workdays) (hh:mm) | Evening-types | 07:40 | 01:15 | 07:58 | 01:12 | 0.30 | 0.74 | 0.02 |
| Intermediate-types | 08:10 | 00:55 | 08:01 | 01:20 | ||||
| Morning-types | 07:26 | 00:49 | 08:16 | 01:24 | ||||
| Mean Survey Time | 07:46 | 00:59 | 08:05 | 01:19 | 2.58 | 0.12 | 0.07 | |
| Time in Bed Free days (Sleep Duration Free days) (hh:mm) | Evening-types | 08:18 | 00:55 | 08:15 | 03:08 | 0.45 | 0.64 | 0.02 |
| Intermediate-types | 08:26 | 00:54 | 07:47 | 02:01 | ||||
| Morning-types | 08:29 | 01:31 | 08:56 | 01:33 | ||||
| Mean Survey Time | 08:25 | 01:07 | 08:20 | 02:14 | 0.06 | 0.81 | 0.002 | |
| MidPoint of Sleep (hh:mm) | Evening-types | 05:46 | 01:26 | 07:06 | 02:02 | 2.85 | 0.07 | 0.14 |
| Intermediate-types | 04:52 | 01:34 | 05:43 | 01:55 | ||||
| Morning-types | 03:27 | 01:26 | 06:11 | 03:25 | ||||
| Mean Survey Time | 04:41 | 01:29 | 06:20 | 02:27 | 14.87 | 0.0001 | 0.29 | |
| Social JetLag (hh:mm) | Evening-types | 01:28 | 01:02 | 02:02 | 03:34 | 1.42 | 0.26 | 0.07 |
| Intermediate-types | 01:51 | 00:57 | 01:29 | 02:34 | ||||
| Morning-types | 02:20 | 01:29 | 03:07 | 04:38 | ||||
| Mean Survey Time | 01:53 | 01:10 | 02:13 | 03:35 | 0.25 | 0.62 | 0.007 | |
| Passage of Present Time | Evening-types | 1.00 | 1.41 | 1.50 | 2.17 | 0.70 | 0.51 | 0.04 |
| Intermediate-types | 1.29 | 1.45 | 0.10 | 2.00 | ||||
| Morning-types | 0.63 | 1.60 | 0.38 | 2.33 | ||||
| Mean Survey Time | 0.97 | 1.49 | 0.66 | 2.17 | 0.70 | 0.50 | 0.02 | |
| Past Intervals | Evening-types | 1.25 | 0.57 | 0.88 | 0.94 | 0.86 | 0.43 | 0.05 |
| Intermediate-types | 0.95 | 0.82 | 0.68 | 0.90 | ||||
| Morning-types | 0.88 | 0.74 | 0.47 | 0.65 | ||||
| Mean Survey Time | 1.03 | 0.71 | 0.68 | 0.83 | 4.32 | 0.045 | 0.11 | |
| Life Periods | Evening-types | 0.73 | 0.83 | 0.19 | 0.93 | 1.41 | 0.26 | 0.07 |
| Intermediate-types | 0.59 | 0.74 | 0.53 | 0.54 | ||||
| Morning-types | 0.98 | 0.73 | 0.82 | 0.67 | ||||
| Mean Survey Time | 0.77 | 0.77 | 0.51 | 0.71 | 2.83 | 0.10 | 0.07 | |
| Feeling of Time Pressure | Evening-types | 2.78 | 0.64 | 1.96 | 0.98 | 0.54 | 0.59 | 0.03 |
| Intermediate-types | 2.61 | 0.78 | 2.32 | 0.89 | ||||
| Morning-types | 2.55 | 0.46 | 1.78 | 0.80 | ||||
| Mean Survey Time | 2.65 | 0.63 | 2.02 | 0.89 | 22.42 | 0.0001 | 0.38 | |
| Feeling of Time Expansion/Boredom | Evening-types | 1.46 | 0.85 | 1.82 | 0.77 | 0.77 | 0.47 | 0.04 |
| Intermediate-types | 1.28 | 0.70 | 1.85 | 0.83 | ||||
| Morning-types | 1.48 | 0.57 | 2.33 | 0.70 | ||||
| Mean Survey Time | 1.41 | 0.71 | 2.00 | 0.77 | 20.32 | 0.0001 | 0.36 | |
| Temporal Metaphor of Speed | Evening-types | 2.87 | 0.69 | 2.07 | 0.73 | 0.04 | 0.96 | 0.002 |
| Intermediate-types | 2.68 | 0.73 | 2.38 | 0.92 | ||||
| Morning-types | 2.50 | 0.98 | 2.50 | 0.69 | ||||
| Mean Survey Time | 2.68 | 0.80 | 2.32 | 0.78 | 3.90 | 0.056 | 0.10 | |
| Temporal Metaphor of Slowness | Evening-types | 1.67 | 0.96 | 1.43 | 0.93 | 0.16 | 0.85 | 0.01 |
| Intermediate-types | 1.16 | 0.40 | 1.75 | 0.77 | ||||
| Morning-types | 1.58 | 0.34 | 1.38 | 0.63 | ||||
| Mean Survey Time | 1.47 | 0.57 | 1.52 | 0.78 | 0.07 | 0.79 | 0.002 | |
| 1dMAAS | 2dRETRO | 3dPRO | 4dPRMQ | 5dBTW | 6dWTW | 7dBTF | 8dWTF | 9dTIBW | 10dTIBF | 11dMPoS | 12dSJL | 13dPT | 14dTI | 15dLP | 16dFP | 17dFE/B | 18dMoSpeed | 19dMoSlow | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | −0.49 ** | −0.63 *** | −0.65 *** | −0.002 | +0.13 | +0.05 | +0.17 | −0.37 | −0.15 | −0.09 | −0.01 | −0.33 | +0.07 | −0.03 | −0.16 | −0.45 ** | −0.22 | −0.03 |
| 2 | 1 | +0.54 *** | +0.82 *** | −0.05 | −0.17 | +0.14 | +0.24 | +0.36 | −0.15 | +0.07 | −0.01 | +0.15 | −0.18 | −0.10 | −0.04 | +0.17 | +0.06 | −0.01 | |
| 3 | 1 | +0.92 *** | +0.03 | −0.10 | +0.10 | +0.06 | +0.39 | +0.01 | +0.02 | +0.06 | +0.30 | +0.02 | +0.07 | +0.03 | +0.27 | +0.19 | +0.03 | ||
| 4 | 1 | +0.001 | −0.14 | +0.11 | +0.14 | +0.42 | −0.06 | +0.05 | +0.03 | +0.27 | −0.05 | −0.003 | +0.004 | +0.25 | +0.16 | +0.02 | |||
| 5 | 1 | +0.94 *** | +0.15 | +0.11 | +0.005 | +0.004 | −0.98 *** | −0.82 *** | +0.02 | −0.03 | +0.13 | +0.18 | +0.34 | −0.08 | +0.03 | ||||
| 6 | 1 | −0.02 | +0.07 | −0.34 | −0.09 | −0.96 *** | −0.77 *** | −0.04 | −0.006 | +0.19 | +0.11 | +0.19 | −0.16 | +0.13 | |||||
| 7 | 1 | +0.49 ** | +0.48 ** | +0.29 | −0.21 | −0.15 | −0.09 | −0.19 | −0.25 | +0.01 | +0.34 | +0.02 | −0.20 | ||||||
| 8 | 1 | +0.10 | −0.69 *** | −0.25 | +0.11 | −0.001 | +0.10 | −0.13 | +0.15 | −0.02 | +0.08 | −0.31° | |||||||
| 9 | 1 | +0.28 | +0.11 | +0.01 | +0.17 | −0.06 | −0.20 | +0.16 | +0.39 | +0.25 | −0.29 | ||||||||
| 10 | 1 | +0.10 | −0.24 | −0.07 | −0.27 | +0.07 | −0.15 | +0.30 | −0.07 | +0.17 | |||||||||
| 11 | 1 | +0.78 *** | +0.02 | +0.02 | −0.12 | −0.16 | −0.28 | +0.11 | −0.03 | ||||||||||
| 12 | 1 | −0.03 | −0.008 | −0.24 | −0.14 | −0.28 | +0.05 | −0.13 | |||||||||||
| 13 | 1 | +0.51 ** | +0.14 | +0.26 | −0.09 | +0.50 ** | −0.49 ** | ||||||||||||
| 14 | 1 | +0.13 | +0.36 | −0.20 | +0.59 *** | −0.28 | |||||||||||||
| 15 | 1 | +0.23 | −0.16 | +0.04 | +0.05 | ||||||||||||||
| 16 | 1 | −0.03 | +0.47 ** | −0.23 | |||||||||||||||
| 17 | 1 | −0.06 | +0.08 | ||||||||||||||||
| 18 | 1 | −0.30 | |||||||||||||||||
| 19 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fabbri, M. Mindfulness, Subjective Cognitive Functioning, Sleep Timing and Time Expansion during COVID-19 Lockdown: A Longitudinal Study in Italy. Clocks & Sleep 2023, 5, 313-332. https://doi.org/10.3390/clockssleep5020024
Fabbri M. Mindfulness, Subjective Cognitive Functioning, Sleep Timing and Time Expansion during COVID-19 Lockdown: A Longitudinal Study in Italy. Clocks & Sleep. 2023; 5(2):313-332. https://doi.org/10.3390/clockssleep5020024
Chicago/Turabian StyleFabbri, Marco. 2023. "Mindfulness, Subjective Cognitive Functioning, Sleep Timing and Time Expansion during COVID-19 Lockdown: A Longitudinal Study in Italy" Clocks & Sleep 5, no. 2: 313-332. https://doi.org/10.3390/clockssleep5020024
APA StyleFabbri, M. (2023). Mindfulness, Subjective Cognitive Functioning, Sleep Timing and Time Expansion during COVID-19 Lockdown: A Longitudinal Study in Italy. Clocks & Sleep, 5(2), 313-332. https://doi.org/10.3390/clockssleep5020024





