Differences in Sleep Offset Timing between Weekdays and Weekends in 79,161 Adult Participants in the UK Biobank
Abstract
:1. Introduction
2. Results
2.1. Demographics and Participant Descriptive Statistics
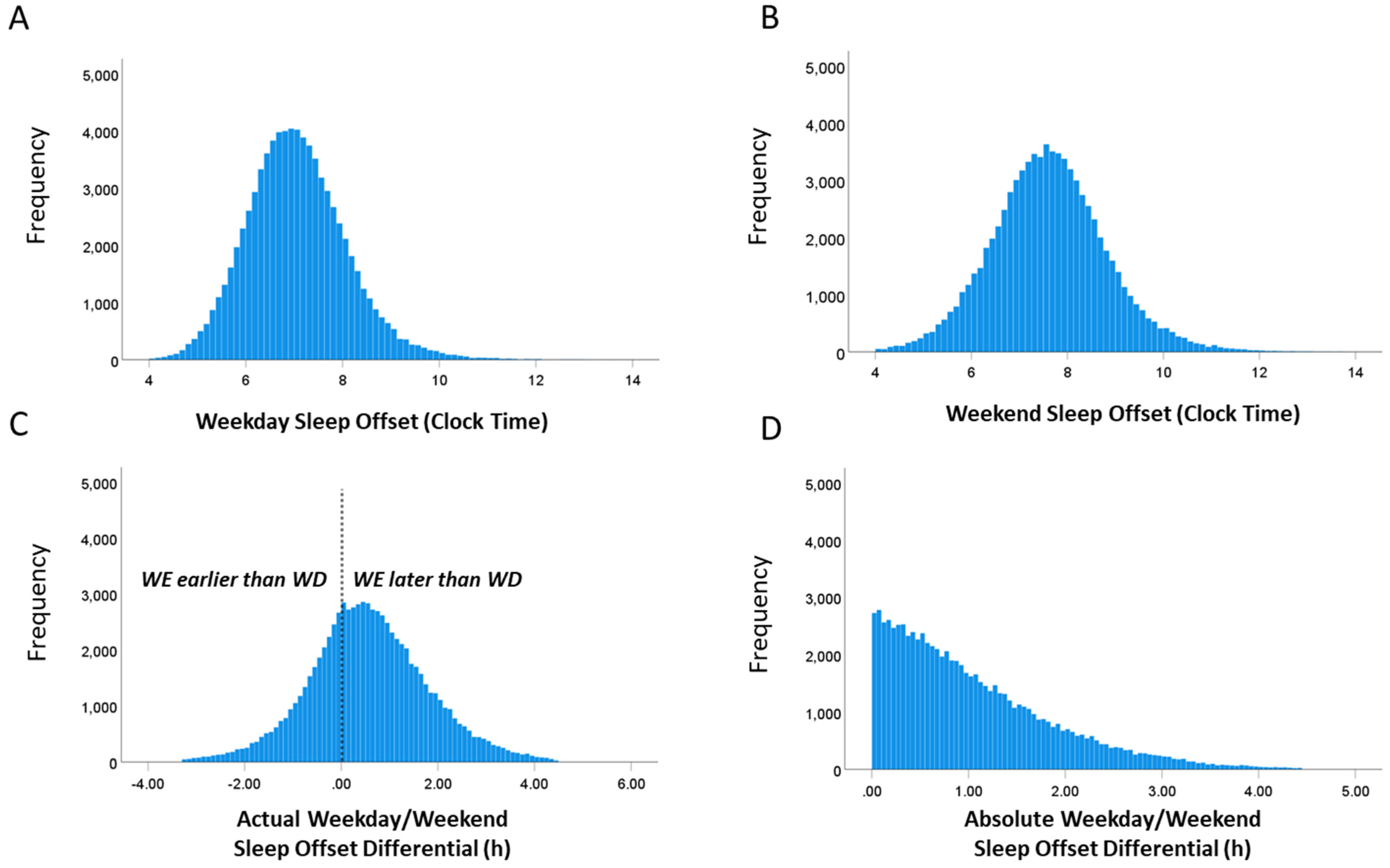
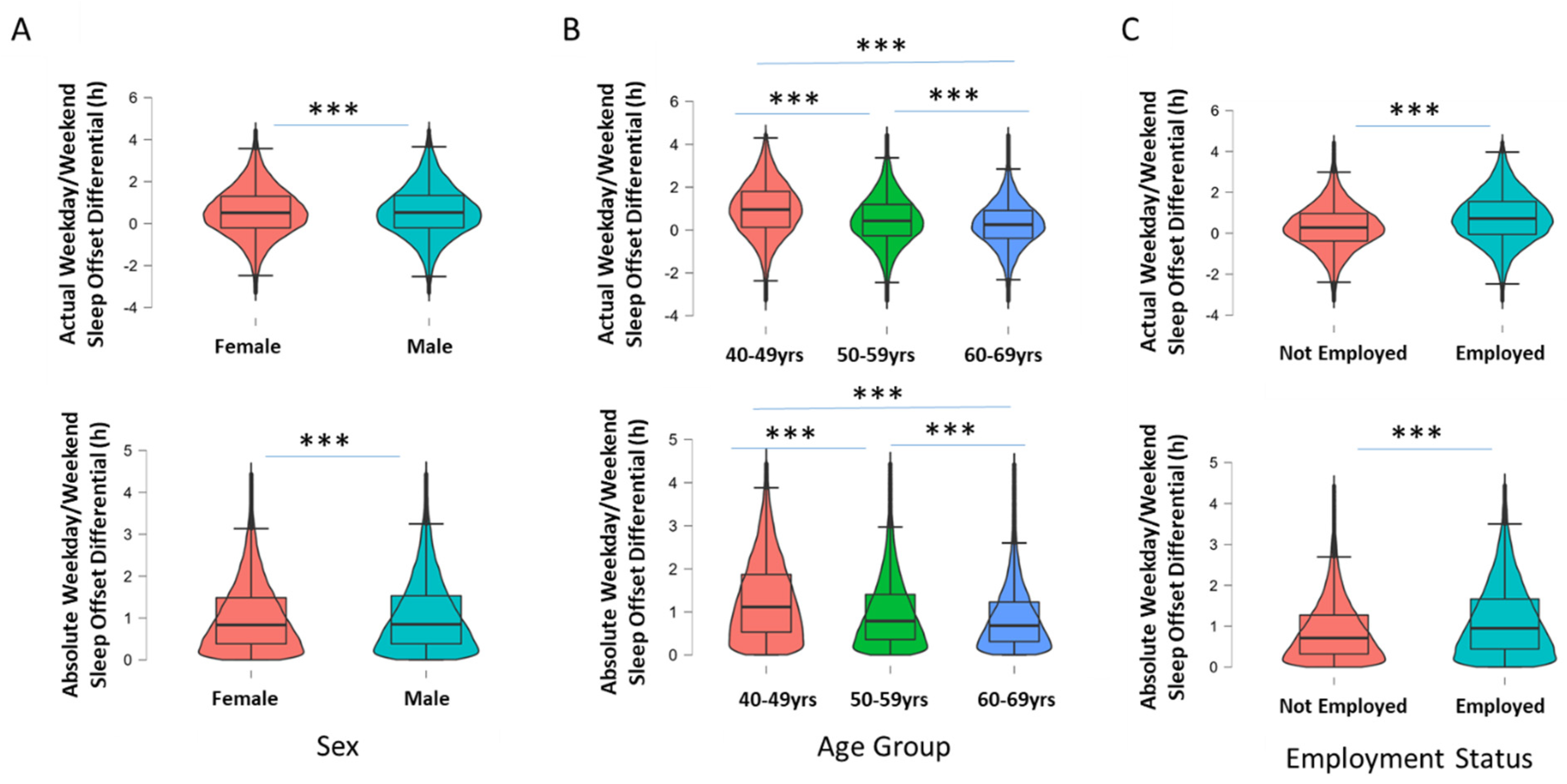
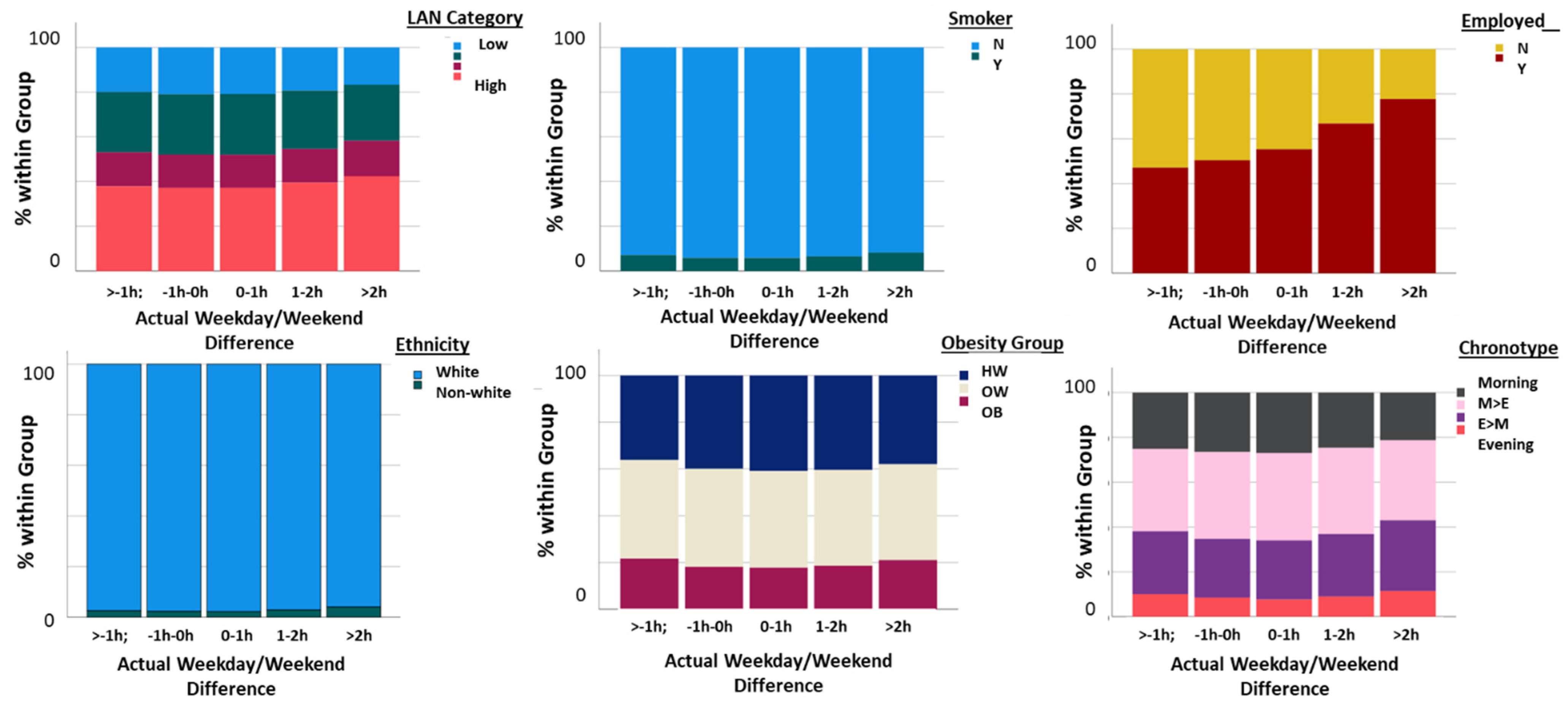
2.2. Weekday and Weekend Sleep Offset Differential
2.3. Association of WD/WE Sleep Offset Difference with Cardiometabolic Health
2.4. Multiple Regression Analysis
2.5. Weekday–Weekend Day Differences in People with Diabetes Mellitus
3. Discussion
Strengths and Limitations
4. Materials and Methods
4.1. Sample
4.2. Participant Measures
4.3. Sleep Offset Differences between Week and Weekend Days
4.4. Data Screening and Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Makarem, N.; Zuraikat, F.M.; Aggarwal, B.; Jelic, S.; St-Onge, M.-P. Variability in Sleep Patterns: An Emerging Risk Factor for Hypertension. Curr. Hypertens. Rep. 2020, 22, 19. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T.; Pilz, L.K.; Zerbini, G.; Winnebeck, E.C. Chronotype and Social Jetlag: A (Self) Critical Review. Biology 2019, 8, 54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fischer, D.; Lombardi, D.A.; Marucci-Wellman, H.; Roenneberg, T. Chronotypes in the US—Influence of age and sex. PLoS ONE 2017, 12, e0178782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raman, S.; Coogan, A.N. Effects of societal-level COVID-19 mitigation measures on the timing and quality of sleep in Ireland. Sleep Med. 2022, 91, 179–184. [Google Scholar] [CrossRef]
- Roenneberg, T.; Allebrandt, K.V.; Merrow, M.; Vetter, C. Social Jetlag and Obesity. Curr. Biol. 2012, 22, 939–943. [Google Scholar] [CrossRef] [Green Version]
- Hashizaki, M.; Nakajima, H.; Kume, K. Monitoring of Weekly Sleep Pattern Variations at Home with a Contactless Biomotion Sensor. Sensors 2015, 15, 18950–18964. [Google Scholar] [CrossRef] [Green Version]
- Jonasdottir, S.S.; Minor, K.; Lehmann, S. Gender differences in nighttime sleep patterns and variability across the adult lifespan: A global-scale wearables study. Sleep 2021, 44, zsaa169. [Google Scholar] [CrossRef]
- Korman, M.; Tkachev, V.; Reis, C.; Komada, Y.; Kitamura, S.; Gubin, D.; Kumar, V.; Roenneberg, T. COVID-19-mandated social restrictions unveil the impact of social time pressure on sleep and body clock. Sci. Rep. 2020, 10, 22225. [Google Scholar] [CrossRef]
- Rezaei, N.; Grandner, M.A. Changes in sleep duration, timing and variability during the Covid-19 pandemic: Large-scale Fitbit data from 6 major US cities. Sleep Health 2021, 7, 303. [Google Scholar] [CrossRef]
- Garefelt, J.; Gershagen, S.; Kecklund, G.; Westerlund, H.; Platts, L.G. How does cessation of work affect sleep? Prospective analyses of sleep duration, timing and efficiency from the Swedish Retirement Study. J. Sleep Res. 2021, 30, e13157. [Google Scholar] [CrossRef]
- Kohyama, J. Pupils with negative social jetlag in Japan are hypothesised to constitute a discrete population. Med. Hypotheses 2020, 144, 110249. [Google Scholar] [CrossRef] [PubMed]
- Komada, Y.; Okajima, I.; Kitamura, S.; Inoue, Y. A survey on social jetlag in Japan: A nationwide, cross-sectional internet survey. Sleep Biol. Rhythm. 2019, 17, 417–422. [Google Scholar] [CrossRef] [Green Version]
- McMahon, D.M.; Burch, J.B.; Wirth, M.D.; Youngstedt, S.D.; Hardin, J.W.; Hurley, T.G.; Blair, S.N.; Hand, G.A.; Shook, R.P.; Drenowatz, C.; et al. Persistence of social jetlag and sleep disruption in healthy young adults. Chronobiol. Int. 2018, 35, 312–328. [Google Scholar] [CrossRef] [PubMed]
- Kuula, L.; Gradisar, M.; Martinmäki, K.; Richardson, C.; Bonnar, D.; Bartel, K.; Lang, C.; Leinonen, L.; Pesonen, A.K. Using big data to explore worldwide trends in objective sleep in the transition to adulthood. Sleep Med. 2019, 62, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Bureau of Labor Statistics. Job Flexibilities and Work Schedules Summary—2017–2018. Data from the American Time Use Survey. 2019. Available online: https://www.bls.gov/news.release/flex2.nr0.htm (accessed on 1 January 2020).
- Eurofound. Fifth European Working Conditions Survey; Publications Office of the European Union: Luxembourg, Germany, 2012. Available online: https://op.europa.eu/s/vKgh (accessed on 1 January 2020).
- Vetter, C.; Winnebeck, E.C.; Roenneberg, T. Asking the Clock: How to Use Information from Questionnaires for Circadian Phenotyping. Methods Mol. Biol. 2021, 2130, 79–85. [Google Scholar] [CrossRef]
- Zhang, R.; Tomasi, D.; Shokri-Kojori, E.; Wiers, C.E.; Wang, G.-J.; Volkow, N.D. Sleep inconsistency between weekends and weekdays is associated with changes in brain function during task and rest. Sleep 2020, 43, zsaa076. [Google Scholar] [CrossRef] [Green Version]
- Kelly, R.M.; Finn, J.; Healy, U.; Gallen, D.; Sreenan, S.; McDermott, J.H.; Coogan, A.N. Greater social jetlag associates with higher HbA1c in adults with type 2 diabetes: A cross sectional study. Sleep Med. 2020, 66, 1–9. [Google Scholar] [CrossRef]
- Paine, S.-J.; Gander, P.H. Differences in circadian phase and weekday/weekend sleep patterns in a sample of middle-aged morning types and evening types. Chronobiol. Int. 2016, 33, 1009–1017. [Google Scholar] [CrossRef]
- Windred, D.P.; Jones, S.E.; Russell, A.; Burns, A.C.; Chan, P.; Weedon, M.N.; Rutter, M.K.; Olivier, P.; Vetter, C.; Saxena, R.; et al. Objective assessment of sleep regularity in 60 000 UK Biobank participants using an open-source package. Sleep 2021, 44, zsab254. [Google Scholar] [CrossRef]
- Duffy, J.F.; Wright, K.P., Jr. Entrainment of the human circadian system by light. J. Biol. Rhythm. 2005, 20, 326–338. [Google Scholar] [CrossRef]
- Nadybal, S.M.; Collins, T.W.; Grineski, S.E. Light pollution inequities in the continental United States: A distributive environmental justice analysis. Environ. Res. 2020, 189, 109959. [Google Scholar] [CrossRef]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social Jetlag: Misalignment of Biological and Social Time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Hiscock, R.; Bauld, L.; Amos, A.; Platt, S. J Public Smoking and socioeconomic status in England: The rise of the never smoker and the disadvantaged smoker. Health 2012, 34, 390–396. [Google Scholar]
- Shan, Z.; Li, Y.; Zong, G.; Guo, Y.; Li, J.; Manson, J.E.; Hu, F.B.; Willett, W.C.; Schernhammer, E.S.; Bhupathiraju, S.N. Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: Results from two large US cohorts of female nurses. BMJ 2018, 363, k4641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roenneberg, T.; Merrow, M. The Circadian Clock and Human Health. Curr. Biol. 2016, 26, R432–R443. [Google Scholar] [CrossRef] [PubMed]
- Vetter, C. Circadian disruption: What do we actually mean? Eur. J. Neurosci. 2020, 51, 531–550. [Google Scholar] [CrossRef] [Green Version]
- Mokhlesi, B.; Hagen, E.W.; Finn, L.A.; Hla, K.M.; Carter, J.R.; Peppard, P.E. Obstructive sleep apnoea during REM sleep and incident non-dipping of nocturnal blood pressure: A longitudinal analysis of the Wisconsin Sleep Cohort. Thorax 2015, 70, 1062–1069. [Google Scholar] [CrossRef] [Green Version]
- Parsons, M.J.; Moffitt, T.E.; Gregory, A.M.; Goldman-Mellor, S.; Nolan, P.M.; Poulton, R.; Caspi, A. Social jetlag, obesity and metabolic disorder: Investigation in a cohort study. Int. J. Obes. 2015, 39, 842–848. [Google Scholar] [CrossRef] [Green Version]
- Lyall, L.M.; Wyse, C.A.; Graham, N.; Ferguson, A.; Lyall, D.M.; Cullen, B.; Celis Morales, C.A.; Biello, S.M.; Mackay, D.; Ward, J.; et al. Association of disrupted circadian rhythmicity with mood disorders, subjective wellbeing, and cognitive function: A cross-sectional study of 91,105 participants from the UK Biobank. Lancet Psychiatry 2018, 5, 507–514. [Google Scholar] [CrossRef] [Green Version]
- Cramer, A.O.; van Ravenzwaaij, D.; Matzke, D.; Steingroever, H.; Wetzels, R.; Grasman, R.P.; Waldorp, L.J.; Wagenmakers, E.J. Hidden multiplicity in exploratory multiway ANOVA: Prevalence and remedies. Psychon. Bull. Rev. 2016, 23, 640–647. [Google Scholar] [CrossRef]
- Cohen, S.; Williamson, G.M. Perceived stress in a probability sample of the United States. In Psychology and Health; Spacapan, S., Oskamp, S., Eds.; Sage: Newbury Park, CA, USA, 1988; pp. 31–67. [Google Scholar]




| Sample Size | % or Mean (SD) | |
|---|---|---|
| Sociodemographic variables | ||
| Age (years) | 79,161 | 56.55 (7.79) |
| Sex | 79,161 | |
| Female | 45,353 | 57.3% |
| Male | 33,808 | 42.7% |
| Townsend Deprivation Score | 79,072 | −1.82 (2.77) |
| Quintile 1 | 15,859 | −4.83 (0.55) |
| Quintile 2 | 15,767 | −3.59 (0.30) |
| Quintile 3 | 15,813 | −2.50 (0.34) |
| Quintile 4 | 15,819 | −0.87 (0.64) |
| Quintile 5 | 15,814 | 2.71 (1.82) |
| Ethnicity | 78,944 | |
| White | 76,840 | 97.3% |
| Mixed | 391 | 0.5% |
| Asian | 657 | 0.8% |
| Black | 507 | 0.6% |
| Chinese | 174 | 0.2% |
| Other | 375 | 0.5% |
| Work Status | 79,161 | |
| Working | 46,438 | 58.7% |
| Not working | 32,723 | 41.3% |
| Health-related Variables | ||
| BMI (kg/m2) | 79,161 | 26.61 (4.46) |
| Smoker: | 78,991 | |
| Yes | 5037 | 6.4% |
| No | 73,954 | 93.6% |
| Alcohol: | 79,128 | |
| Never | 4304 | 5.4 |
| Special occasions only | 7297 | 9.2 |
| 1–3 times pm | 8377 | 10.6 |
| 1–2 times pw | 19,669 | 24.9 |
| 3–4 times pw | 20,936 | 26.5 |
| Daily/Almost daily | 18,545 | 23.4 |
| Physical Activity(MET/h) | 77,576 | 35.91 (35.66) |
| Sedentary time (h/week) | 79,105 | 4.89 (2.13) |
| Diabetes mellitus Disgnosis | 2697 | 3.4% |
| HbA1c (mmol/mol) | 74,106 | 35.39 (5.50) |
| Systolic blood pressure (mm hg) | 75,537 | 138.76 (19.34) |
| Diastolic blood pressure (mm hg) | 75,538 | 81.58 (10.56) |
| Sleep-related variables | ||
| Sleep Offest on Weekdays (hh:mm) Sleep Offset on Weekends (hh:mm) Actual Weekday-Weekend Difference (h:mm) | 79,161 79,161 79,161 | 07:03 (01:02) 07:37 (01:11) 00:34 (01:13) |
| Absolute Weekday-Weekend Difference (h:mm) | 79,161 | 1:03 (00:50) |
| Self-Reported Sleep Duration (h:mm) | 78,992 | 7:11 (00:58) |
| R2 | R2 Change | β | B | SE | CI 95% (B) | |
|---|---|---|---|---|---|---|
| Model 1 | 0.045 *** | |||||
| Age | −0.212 *** | −0.023 | 0.000 | −0.024/−0.022 | ||
| Sex | 0.035 *** | 0.060 | 0.007 | 0.047/0.073 | ||
| Model 2 | 0.048 *** | 0.003 *** | ||||
| Age | −0.181 *** | −0.019 | 0.001 | −0.020/−0.018 | ||
| Sex | 0.032 *** | 0.054 | 0.007 | 0.041/0.067 | ||
| Deprivation | 0.025 *** | 0.008 | 0.001 | 0.05/0.010 | ||
| LAN | 0.011 * | 0.019 | 0.008 | 0.04/0.034 | ||
| Smoker | 0.018 *** | 0.063 | 0.014 | 0.036/0.089 | ||
| Work Status | 0.050 *** | 0.085 | 0.008 | 0.069/0.101 | ||
| Model 3 | 0.050 *** | 0.002 *** | ||||
| Age | −0.177 *** | −0.019 | 0.001 | −0.020/−0.018 | ||
| Sex | 0.031 *** | 0.053 | 0.007 | 0.040/0.066 | ||
| Deprivation | 0.024 *** | 0.007 | 0.001 | 0.005/0.010 | ||
| LAN | 0.010 * | 0.017 | 0.008 | 0.003/0.032 | ||
| Smoker | 0.016 *** | 0.053 | 0.014 | 0.026/0.080 | ||
| Work Status | 0.051 *** | 0.086 | 0.008 | 0.070/0.102 | ||
| Sleep Duration | −0.005 | −0.004 | 0.003 | −0.011/0.003 | ||
| Chronotype | 0.043 *** | 0.074 | 0.007 | 0.061/0.088 | ||
| Model 4 | 0.052 *** | 0.002 ** | ||||
| Age | −0.181 *** | −0.019 | 0.001 | −0.021/−0.018 | ||
| Sex | 0.027 *** | 0.047 | 0.007 | 0.018/0.062 | ||
| Deprivation | 0.020 *** | 0.006 | 0.001 | 0.003/0.008 | ||
| LAN | 0.011 * | 0.018 | 0.008 | 0.03/0.033 | ||
| Smoker | 0.015 *** | 0.051 | 0.013 | 0.026/0.080 | ||
| Work Status | 0.050 *** | 0.085 | 0.008 | 0.069/0.101 | ||
| Sleep Duration | −0.006 | −0.005 | 0.003 | −0.012/0.01 | ||
| Chronotype | 0.041 *** | 0.071 | 0.007 | 0.057/0.084 | ||
| BMI | 0.038 *** | 0.007 | 0.001 | 0.006/0.009 | ||
| HbA1c | 0.005 | 0.001 | 0.001 | −0.000/0.002 | ||
| Sedentary Behaviour | 0.11 ** | 0.004 | 0.002 | 0.001/0.007 | ||
| Physical Activity | −0.006 | −0.000 | 0.000 | −0.000/−0.000 | ||
| SBP | −0.004 | −0.000 | 0.000 | −0.001/0.000 | ||
| DBP | 0.001 | 0.000 | 0.000 | −0.001/0.001 |
| R2 | R2 Change | β | B | SE | CI 95% (B) | |
|---|---|---|---|---|---|---|
| Model 1 | 0.036 *** | |||||
| Age | −0.191 *** | −0.024 | 0.003 | −0.031/−0.018 | ||
| Sex | 0.013 | 0.024 | 0.047 | −0.69/0.117 | ||
| Model 2 | 0.045 *** | 0.009 * | ||||
| Age | −0.138 *** | −0.018 | 0.004 | −0.025/−0.010 | ||
| Sex | 0.009 | 0.016 | 0.048 | −0.078/0.109 | ||
| Deprivation | 0.018 | 0.005 | 0.008 | −0.111/0.022 | ||
| LAN | 0.036 | 0.027 | 0.022 | −0.015/0.070 | ||
| Smoker | −0.008 | −0.025 | 0.083 | −0.188/0.139 | ||
| Work Status | 0.097 ** | 0.171 | 0.054 | 0.066/0.276 | ||
| Model 3 | 0.046 *** | 0.002 | ||||
| Age | −0.136 *** | −0.017 | 0.004 | −0.025/−0.010 | ||
| Sex | 0.010 | 0.018 | 0.048 | −0.078/0.109 | ||
| Deprivation | 0.016 | 0.005 | 0.008 | −0.112/0.021 | ||
| LAN | 0.037 | 0.028 | 0.022 | −0.015/0.070 | ||
| Smoker | −0.009 | −0.027 | 0.083 | −0.190/0.137 | ||
| Work Status | 0.094 ** | 0.167 | 0.054 | 0.066/0.276 | ||
| Sleep Duration | −0.023 | −0.018 | 0.021 | −0.060/0.023 | ||
| Chronotype | 0.015 | 0.026 | 0.047 | −0.066/0.119 | ||
| Model 4 | 0.049 *** | 0.003 | ||||
| Age | −0.127 *** | −0.017 | 0.004 | −0.025/−0.010 | ||
| Sex | 0.009 | 0.018 | 0.048 | −0.078/0.109 | ||
| Deprivation | 0.012 | 0.005 | 0.008 | −0.112/0.021 | ||
| LAN | 0.035 | 0.028 | 0.022 | −0.015/0.070 | ||
| Smoker | −0.009 | −0.027 | 0.083 | −0.19/0.137 | ||
| Work Status | 0.096 ** | 0.167 | 0.054 | 0.066/0.276 | ||
| Sleep Duration | 0.021 | −0.018 | 0.021 | −0.060/0.023 | ||
| Chronotype | 0.014 | 0.026 | 0.047 | −0.066/0.119 | ||
| BMI | 0.038 | 0.007 | 0.001 | 0.006/0.009 | ||
| HbA1c | −0.013 | 0.001 | 0.001 | −0.000/0.002 | ||
| Sedentary Behaviour | 0.13 | 0.004 | 0.010 | −0.001/0.001 | ||
| Physical Activity | −0.015 | 0.000 | 0.000 | −0.001/0.001 | ||
| SBP | −0.023 | 0.001 | 0.002 | −0.004/0.002 | ||
| DBP | 0.022 | 0.002 | 0.003 | −0.004/0.007 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kelly, R.M.; McDermott, J.H.; Coogan, A.N. Differences in Sleep Offset Timing between Weekdays and Weekends in 79,161 Adult Participants in the UK Biobank. Clocks & Sleep 2022, 4, 658-674. https://doi.org/10.3390/clockssleep4040050
Kelly RM, McDermott JH, Coogan AN. Differences in Sleep Offset Timing between Weekdays and Weekends in 79,161 Adult Participants in the UK Biobank. Clocks & Sleep. 2022; 4(4):658-674. https://doi.org/10.3390/clockssleep4040050
Chicago/Turabian StyleKelly, Rachael M., John H. McDermott, and Andrew N. Coogan. 2022. "Differences in Sleep Offset Timing between Weekdays and Weekends in 79,161 Adult Participants in the UK Biobank" Clocks & Sleep 4, no. 4: 658-674. https://doi.org/10.3390/clockssleep4040050
APA StyleKelly, R. M., McDermott, J. H., & Coogan, A. N. (2022). Differences in Sleep Offset Timing between Weekdays and Weekends in 79,161 Adult Participants in the UK Biobank. Clocks & Sleep, 4(4), 658-674. https://doi.org/10.3390/clockssleep4040050






