High Adherence to a Mediterranean Alcohol-Drinking Pattern and Mediterranean Diet Can Mitigate the Harmful Effect of Alcohol on Mortality Risk
Abstract
:1. Introduction
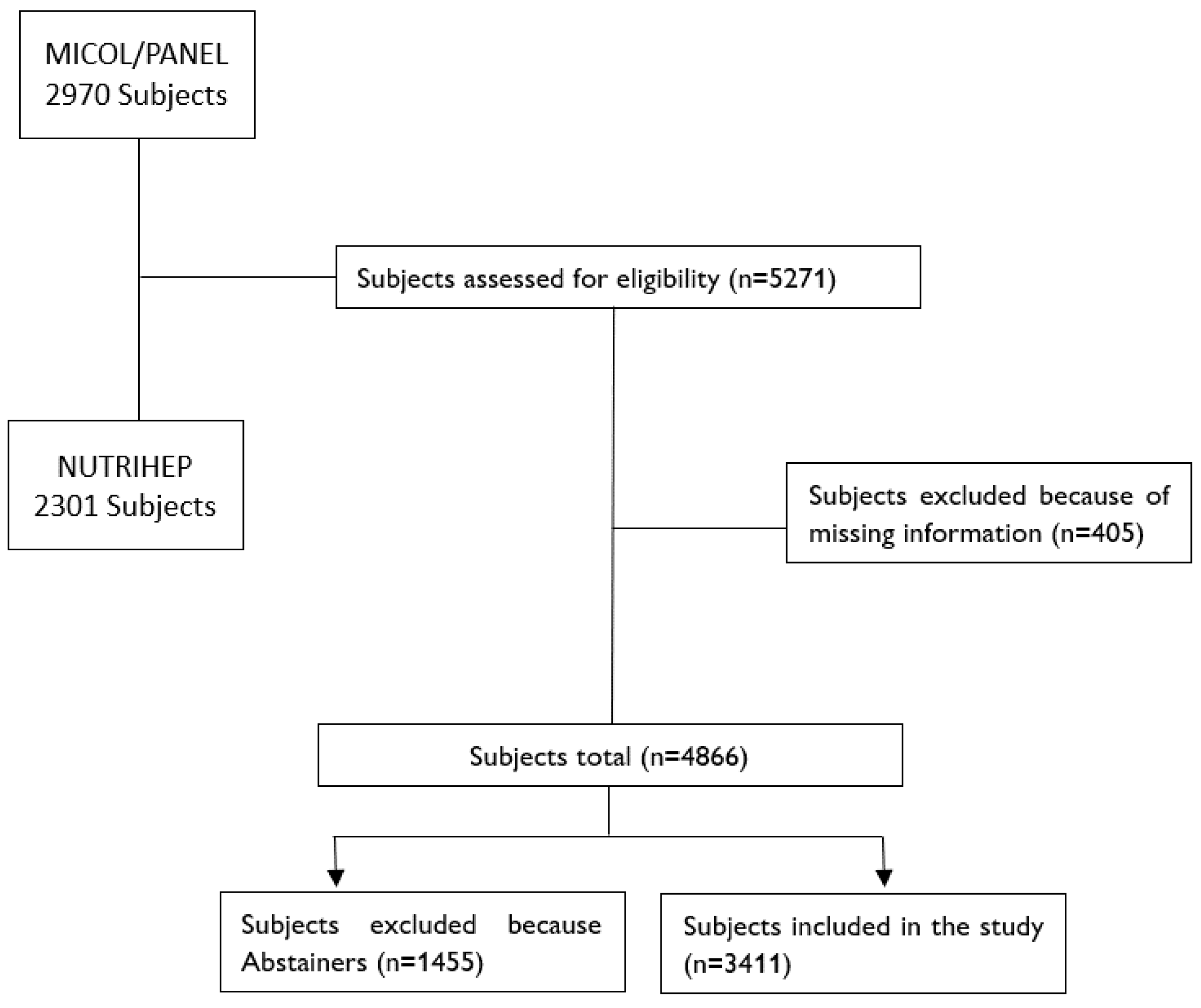
2. Materials and Methods
2.1. Data Collection
2.2. Outcome Assessment
2.3. Exposure Assessment
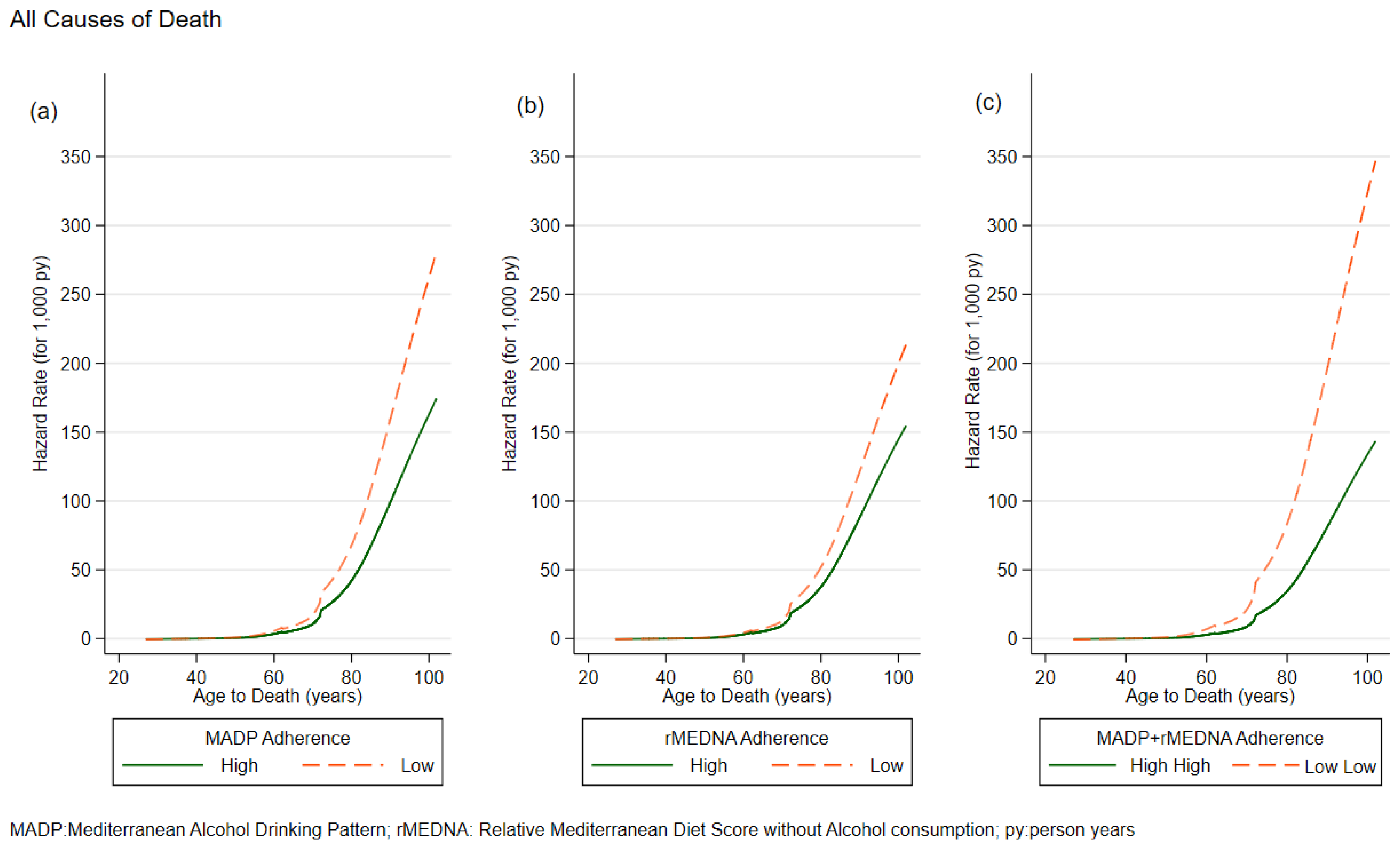
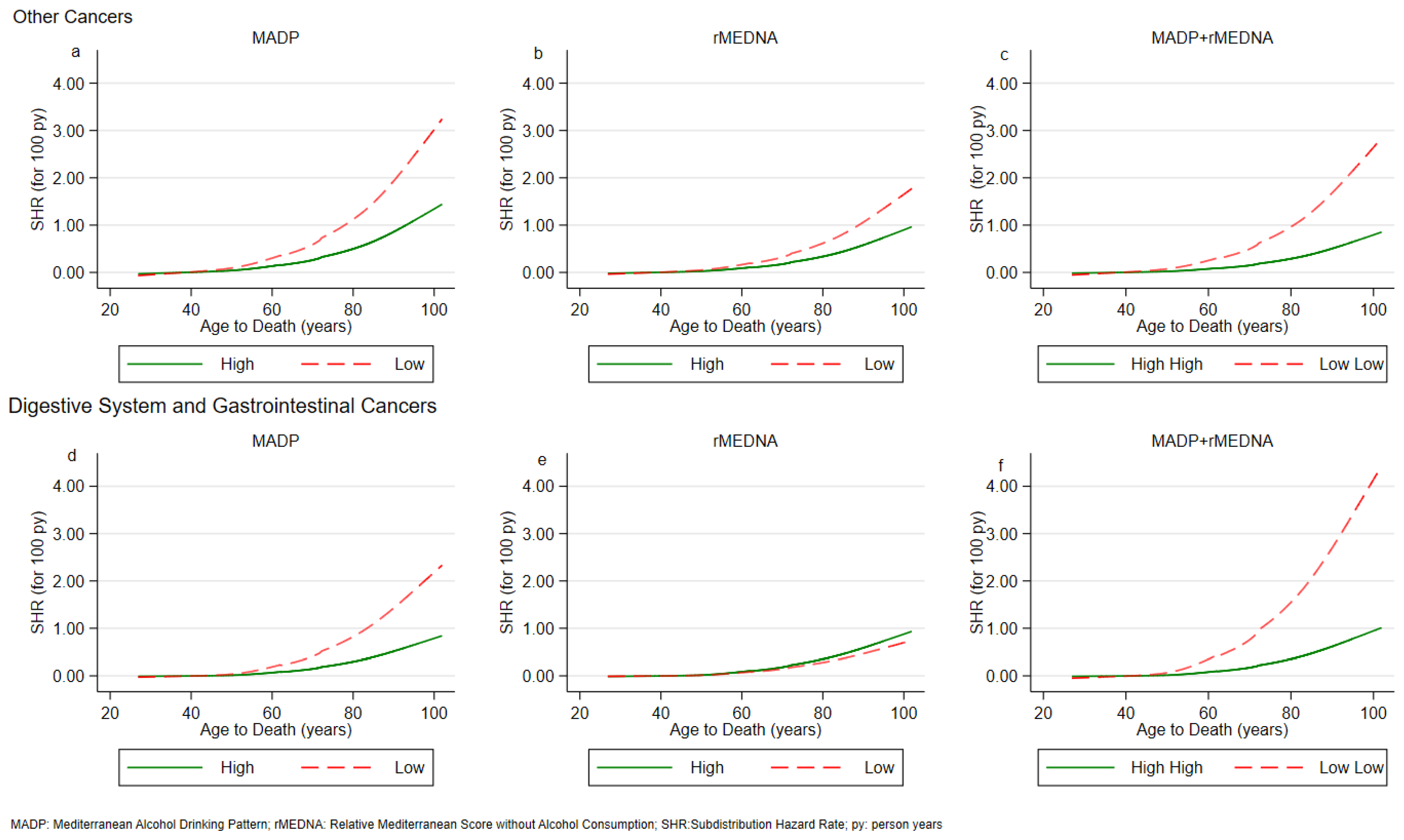
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ding, C.; O’Neill, D.; Bell, S.; Stamatakis, E.; Britton, A. Association of Alcohol Consumption with Morbidity and Mortality in Patients with Cardiovascular Disease: Original Data and Meta-Analysis of 48,423 Men and Women. BMC Med. 2021, 19, 167. [Google Scholar] [CrossRef] [PubMed]
- Wood, A.M.; Kaptoge, S.; Butterworth, A.S.; Willeit, P.; Warnakula, S.; Bolton, T.; Paige, E.; Paul, D.S.; Sweeting, M.; Burgess, S.; et al. Risk Thresholds for Alcohol Consumption: Combined Analysis of Individual-Participant Data for 599 912 Current Drinkers in 83 Prospective Studies. Lancet 2018, 391, 1513–1523. [Google Scholar] [CrossRef] [PubMed]
- Xi, B.; Veeranki, S.P.; Zhao, M.; Ma, C.; Yan, Y.; Mi, J. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J. Am. Coll. Cardiol. 2017, 70, 913–922. [Google Scholar] [CrossRef] [PubMed]
- Murphy, N.; Ferrari, P.; Soerjomataram, I. Alcohol and Cancer: Epidemiology and Biological Mechanisms. Nutrients 2021, 13, 3173. [Google Scholar] [CrossRef]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Alcohol Consumption and Ethyl Carbamate; IARC Press: Lyon, France, 2010; Volume 96, pp. 3–1383. [Google Scholar]
- Mostofsky, E.; Chahal, H.S.; Mukamal, K.J.; Rimm, E.B.; Mittleman, M.A. Alcohol and Immediate Risk of Cardiovascular Events: A Systematic Review and Dose-Response Meta-Analysis. Circulation 2016, 133, 979–987. [Google Scholar] [CrossRef] [PubMed]
- Bataller, R.; Arab, J.P.; Shah, V.H. Alcohol-Associated Hepatitis. N. Engl. J. Med. 2022, 387, 2436–2448. [Google Scholar] [CrossRef] [PubMed]
- Tsuker, M.B. Development of pediatric neuropathology in the USSR. Zhurnal Nevropatol. I Psikhiatrii Im. SS Korsakova 1967, 67, 1650–1652. [Google Scholar]
- Virani, S.S.; Newby, L.K.; Arnold, S.V.; Bittner, V.; Brewer, L.C.; Demeter, S.H.; Dixon, D.L.; Fearon, W.F.; Hess, B.; Johnson, H.M.; et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2023, 148, e9–e119. [Google Scholar] [CrossRef]
- GBD 2020 Alcohol Collaborators Population-Level Risks of Alcohol Consumption by Amount, Geography, Age, Sex, and Year: A Systematic Analysis for the Global Burden of Disease Study 2020. Lancet 2022, 400, 185–235. [CrossRef]
- Morales, G.; Martínez-González, M.A.; Barbería-Latasa, M.; Bes-Rastrollo, M.; Gea, A. Mediterranean Diet, Alcohol-Drinking Pattern and Their Combined Effect on All-Cause Mortality: The Seguimiento Universidad de Navarra (SUN) Cohort. Eur. J. Nutr. 2021, 60, 1489–1498. [Google Scholar] [CrossRef]
- Bazal, P.; Gea, A.; Martínez-González, M.A.; Salas-Salvadó, J.; Asensio, E.M.; Muñoz-Bravo, C.; Fiol, M.; Muñoz, M.A.; Lapetra, J.; Serra-Majem, L.L.; et al. Mediterranean Alcohol-Drinking Pattern, Low to Moderate Alcohol Intake and Risk of Atrial Fibrillation in the PREDIMED Study. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 676–683. [Google Scholar] [CrossRef] [PubMed]
- Gea, A.; Bes-Rastrollo, M.; Toledo, E.; Garcia-Lopez, M.; Beunza, J.J.; Estruch, R.; Martinez-Gonzalez, M.A. Mediterranean Alcohol-Drinking Pattern and Mortality in the SUN (Seguimiento Universidad de Navarra) Project: A Prospective Cohort Study. Br. J. Nutr. 2014, 111, 1871–1880. [Google Scholar] [CrossRef] [PubMed]
- Misciagna, G.; Leoci, C.; Guerra, V.; Chiloiro, M.; Elba, S.; Petruzzi, J.; Mossa, A.; Noviello, M.R.; Coviello, A.; Minutolo, M.C.; et al. Epidemiology of Cholelithiasis in Southern Italy. Part II: Risk Factors. Eur. J. Gastroenterol. Hepatol. 1996, 8, 585–594. [Google Scholar] [CrossRef] [PubMed]
- The NUTRIHEP Collaborating Group; Cozzolongo, R.; Osella, A.R.; Elba, S.; Petruzzi, J.; Buongiorno, G.; Giannuzzi, V.; Leone, G.; Bonfiglio, C.; Lanzilotta, E.; et al. Epidemiology of HCV Infection in the General Population: A Survey in a Southern Italian Town. Am. J. Gastroenterol. 2009, 104, 2740–2746. [Google Scholar] [CrossRef] [PubMed]
- Sever, P. New Hypertension Guidelines from the National Institute for Health and Clinical Excellence and the British Hypertension Society. J. Renin-Angiotensin-Aldosterone Syst. 2006, 7, 61–63. [Google Scholar] [CrossRef] [PubMed]
- UNESCO International Standard Classification of Education (ISCED-97) 2006. Available online: https://unesdoc.unesco.org/ark:/48223/pf0000146967?posInSet=1&queryId=a8d996ff-eddd-4153-9468-5d7f9e8f7199 (accessed on 14 November 2023).
- International Standard Classification of Occupations, International Labour Office. Available online: https://www.ilo.org/public/english/bureau/stat/isco/docs/resol08.pdf (accessed on 14 November 2023).
- Kaaks, R. Validation and Calibration of Dietary Intake Measurements in the EPIC Project: Methodological Considerations. European Prospective Investigation into Cancer and Nutrition. Int. J. Epidemiol. 1997, 26, S15–S25. [Google Scholar] [CrossRef]
- WHO International Classification of Diseases, 10th ed.; WHO: Geneva, Switzerland, 2010; Volume 2, ISBN 978 92 4 154834 2.
- Buckland, G.; Gonzalez, C.A.; Agudo, A.; Vilardell, M.; Berenguer, A.; Amiano, P.; Ardanaz, E.; Arriola, L.; Barricarte, A.; Basterretxea, M.; et al. Adherence to the Mediterranean Diet and Risk of Coronary Heart Disease in the Spanish EPIC Cohort Study. Am. J. Epidemiol. 2009, 170, 1518–1529. [Google Scholar] [CrossRef]
- International Olive Council (IOC). EU Olive Oil Figures. 2019. 2022. Available online: https://www.internationaloliveoil.org/wp-content/uploads/2022/12/IOC-Olive-Oil-Dashboard-2.html#production-1 (accessed on 20 November 2023).
- Barbería-Latasa, M.; Bes-Rastrollo, M.; Pérez-Araluce, R.; Martínez-González, M.Á.; Gea, A. Mediterranean Alcohol-Drinking Patterns and All-Cause Mortality in Women More Than 55 Years Old and Men More Than 50 Years Old in the “Seguimiento Universidad de Navarra” (SUN) Cohort. Nutrients 2022, 14, 5310. [Google Scholar] [CrossRef]
- Fine, J.P.; Gray, R.J. A Proportional Hazards Model for the Subdistribution of a Competing Risk. J. Am. Stat. Assoc. 1999, 94, 496–509. [Google Scholar] [CrossRef]
- Coviello, V.; Boggess, M. Cumulative Incidence Estimation in the Presence of Competing Risks. Stata J. 2004, 4, 103–112. [Google Scholar] [CrossRef]
- Ikemoto, K.; Takahashi, K.; Ozawa, T.; Isobe, H. Akaike’s Information Criterion for Stoichiometry Inference of Supramolecular Complexes. Angew. Chem. Int. Ed. 2023, 62, e202219059. [Google Scholar] [CrossRef] [PubMed]
- Bartoš, F.; Aust, F.; Haaf, J.M. Informed Bayesian Survival Analysis. BMC Med. Res. Methodol. 2022, 22, 238. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.-M.; Sundararajan, V. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data from 6 Countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Ren, J. Interaction between High-Fat Diet and Alcohol Dehydrogenase on Ethanol-Elicited Cardiac Depression in Murine Myocytes. Obesity 2007, 15, 2932–2941. [Google Scholar] [CrossRef] [PubMed]
- Moreira Júnior, R.E.; De Carvalho, L.M.; Pedersen, A.S.B.; Damasceno, S.; Maioli, T.U.; De Faria, A.M.C.; Godard, A.L.B. Interaction between High-Fat Diet and Ethanol Intake Leads to Changes on the Fecal Microbiome. J. Nutr. Biochem. 2019, 72, 108215. [Google Scholar] [CrossRef] [PubMed]
- Renaud, S.C.; Guéguen, R.; Siest, G.; Salamon, R. Wine, Beer, and Mortality in Middle-Aged Men From Eastern France. Arch. Intern. Med. 1999, 159, 1865. [Google Scholar] [CrossRef] [PubMed]
- Streppel, M.T.; Ocke, M.C.; Boshuizen, H.C.; Kok, F.J.; Kromhout, D. Long-Term Wine Consumption Is Related to Cardiovascular Mortality and Life Expectancy Independently of Moderate Alcohol Intake: The Zutphen Study. J. Epidemiol. Community Health 2009, 63, 534–540. [Google Scholar] [CrossRef]
- Klatsky, A.L.; Friedman, G.D.; Armstrong, M.A.; Kipp, H. Wine, Liquor, Beer, and Mortality. Am. J. Epidemiol. 2003, 158, 585–595. [Google Scholar] [CrossRef]
- Grønbæk, M. Type of Alcohol Consumed and Mortality from All Causes, Coronary Heart Disease, and Cancer. Ann. Intern. Med. 2000, 133, 411. [Google Scholar] [CrossRef]
- Baglietto, L.; English, D.R.; Hopper, J.L.; Powles, J.; Giles, G.G. Average volume of alcohol consumed, type of beverage, drinking pattern and the risk of death from all causes. Alcohol Alcohol. 2006, 41, 664–671. [Google Scholar] [CrossRef]
- Strandberg, T.E.; Strandberg, A.Y.; Salomaa, V.V.; Pitkala, K.; Tilvis, R.S.; Miettinen, T.A. Alcoholic Beverage Preference, 29-Year Mortality, and Quality of Life in Men in Old Age. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2007, 62, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Hrelia, S.; Di Renzo, L.; Bavaresco, L.; Bernardi, E.; Malaguti, M.; Giacosa, A. Moderate Wine Consumption and Health: A Narrative Review. Nutrients 2022, 15, 175. [Google Scholar] [CrossRef] [PubMed]
- Mukamal, K.J.; Conigrave, K.M.; Mittleman, M.A.; Camargo, C.A.; Stampfer, M.J.; Willett, W.C.; Rimm, E.B. Roles of Drinking Pattern and Type of Alcohol Consumed in Coronary Heart Disease in Men. N. Engl. J. Med. 2003, 348, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Cordova, A.; Sumpio, B. Polyphenols Are Medicine: Is It Time to Prescribe Red Wine for Our Patients? Int. J. Angiol. 2009, 18, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Ditano-Vázquez, P.; Torres-Peña, J.D.; Galeano-Valle, F.; Pérez-Caballero, A.I.; Demelo-Rodríguez, P.; Lopez-Miranda, J.; Katsiki, N.; Delgado-Lista, J.; Alvarez-Sala-Walther, L.A. The Fluid Aspect of the Mediterranean Diet in the Prevention and Management of Cardiovascular Disease and Diabetes: The Role of Polyphenol Content in Moderate Consumption of Wine and Olive Oil. Nutrients 2019, 11, 2833. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.K.; Andersen, A.T.; Sørensen, T.I.A.; Becker, U.; Thorsen, T.; Grønbæk, M. Alcoholic Beverage Preference and Risk of Becoming a Heavy Drinker. Epidemiology 2002, 13, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Surial, B.; Bertholet, N.; Daeppen, J.-B.; Darling, K.; Calmy, A.; Günthard, H.; Stöckle, M.; Bernasconi, E.; Schmid, P.; Rauch, A.; et al. The Impact of Binge Drinking on Mortality and Liver Disease in the Swiss HIV Cohort Study. J. Clin. Med. 2021, 10, 295. [Google Scholar] [CrossRef]
- Ekstedt, M.; Franzén, L.E.; Holmqvist, M.; Bendtsen, P.; Mathiesen, U.L.; Bodemar, G.; Ekstedt, M.; Franzén, L.E.; Holmqvist, M.; Bendtsen, P.; et al. Alcohol Consumption Is Associated with Progression of Hepatic Fibrosis in Non-Alcoholic Fatty Liver Disease. Scand. J. Gastroenterol. 2009, 44, 366–374. [Google Scholar] [CrossRef]
- Sofi, F.; Cesari, F.; Abbate, R.; Gensini, G.F.; Casini, A. Adherence to Mediterranean Diet and Health Status: Meta-Analysis. BMJ 2008, 337, a1344. [Google Scholar] [CrossRef]
- Rigotti, N.A.; Kruse, G.R.; Livingstone-Banks, J.; Hartmann-Boyce, J. Treatment of Tobacco Smoking: A Review. JAMA 2022, 327, 566. [Google Scholar] [CrossRef]
- Lau, B.; Cole, S.R.; Gange, S.J. Competing Risk Regression Models for Epidemiologic Data. Am. J. Epidemiol. 2009, 170, 244–256. [Google Scholar] [CrossRef] [PubMed]
- Shaper, A.G.; Wannamethee, G.; Walker, M. Alcohol and Mortality in British Men: Explaining the U-Shaped Curve. Lancet 1988, 2, 1267–1273. [Google Scholar] [CrossRef] [PubMed]
| Mediterranean Alcohol Drinking Pattern | |||||
|---|---|---|---|---|---|
| All Sample ¥ | High (7–9) | Moderate (4–6) | Low (0–3) | p-Value | |
| N *** | 3411 | 1810 | 1508 | 93 | |
| Age at enrolment (yrs) * | 50.98 (16.01) | 54.79 (15.62) | 46.27 (15.38) | 53.16 (13.31) | <0.001 |
| DBP (mmHg) * | 124.98 (16.98) | 126.09 (17.90) | 123.33 (15.53) | 129.92 (18.32) | <0.001 |
| SBP (mmHg) * | 77.59 (9.39) | 77.08 (9.91) | 78.09 (8.67) | 79.41 (9.29) | 0.002 |
| Weight (kg) * | 72.98 (14.52) | 73.50 (14.22) | 71.86 (14.78) | 81.26 (12.78) | <0.001 |
| BMI (kg/m2) * | 27.13 (4.80) | 27.57 (4.67) | 26.50 (4.92) | 28.85 (3.87) | <0.001 |
| Kcal days * | 2185.4 (722.8) | 2165.5 (682.8) | 2168.4 (746.7) | 2849.4 (778.6) | <0.001 |
| Triglycerides (mmol/L) * | 1.38 (0.98) | 1.42 (0.95) | 1.31 (0.99) | 1.61 (1.13) | <0.001 |
| Total Cholesterol (mmol/L) * | 5.12 (1.02) | 5.18 (0.99) | 5.03 (1.06) | 5.43 (0.98) | <0.001 |
| HDL (mmol/L) * | 1.34 (0.35) | 1.33 (0.34) | 1.34 (0.34) | 1.41 (0.48) | 0.099 |
| LDL (mmol/L) * | 3.16 (0.87) | 3.21 (0.85) | 3.09 (0.89) | 3.27 (0.87) | <0.001 |
| Glucose (mmol/L) * | 5.84 (1.34) | 5.93 (1.33) | 5.70 (1.34) | 6.25 (1.30) | <0.001 |
| GPT (μkat/L) * | 0.27 (0.21) | 0.27 (0.23) | 0.27 (0.18) | 0.37 (0.22) | <0.001 |
| Wine (g alcohol/d) * | 15.77 (17.86) | 16.47 (11.13) | 12.73 (21.39) | 51.40 (21.19) | <0.001 |
| Beer (g alcohol/d) * | 1.87 (4.22) | 0.75 (2.00) | 2.42 (4.43) | 14.89 (7.69) | <0.001 |
| Spirit (g alcohol/d) * | 1.19 (2.97) | 0.74 (1.61) | 1.39 (3.09) | 6.82 (9.03) | <0.001 |
| Gender *** | |||||
| Female | 1464 (42.9) | 701 (47.9) | 759 (51.8) | 4 (0.3) | <0.001 |
| Male | 1947 (57.1) | 1109 (57.0) | 749 (38.5) | 89 (4.6) | |
| Smoker *** | |||||
| Never/Former | 2823 (82.8) | 1550 (54.9) | 1216 (43.1) | 57 (2.0) | <0.001 |
| Current | 588 (17.2) | 260 (44.2) | 292 (49.7) | 36 (6.1) | |
| CCI ** | 2 (1–4) | 3 (1–5) | 2 (0–3) | 4 (2–5) | <0.001 |
| rMED ** | 8 (6–10) | 8 (7–10) | 8 (6–11) | 7 (5–8) | <0.001 |
| rMEDNA categories | |||||
| High Adherence | 654 (19.2) | 354 (54.1) | 293 (44.8) | 7 (1.1) | <0.001 |
| Moderate Adherence | 1697 (49.8) | 996 (58.7) | 658 (38.8) | 43 (2.5) | |
| Low Adherence | 1060 (31.1) | 460 (43.4) | 557 (52.5) | 43 (4.1) | |
| Age at Death (yrs) ** | 67.4 (55.0–78.3) | 71.6 (58.7–81.6) | 61.8 (50.9–74.0) | 69.1 (59.0–77.07) | <0.001 |
| Observation time ** (yrs) | 16.8 (16.1–17.0) | 16.8 (16.0–17.1) | 16.8 (16.2–16.9) | 16.8 (16.0–17.2) | 0.003 |
| Status *** | |||||
| Alive and/or Censored | 2819 (82.6) | 1406 (49.9) | 1345 (47.7) | 68 (2.4) | <0.001 |
| Dead | 592 (17.4) | 404 (68.2) | 163 (27.5) | 25 (4.2) | |
| Cause of Death *** | |||||
| CVD | 175 (29.6) | 126 (72.0) | 44 (25.1) | 5 (2.9) | 0.026 |
| Cr | 111 (18.8) | 71 (64.0) | 31 (27.9) | 9 (8.1) | |
| DS | 83 (14.0) | 49 (59.0) | 27 (32.5) | 7 (8.4) | |
| DOC | 223 (37.7) | 158 (70.9) | 61 (27.4) | 4 (1.8) | |
| Education *** | |||||
| Primary School | 1021 (29.9) | 591 (57.9) | 403 (39.5) | 27 (2.6) | <0.001 |
| Secondary School | 1061 (31.1) | 563 (53.1) | 460 (43.4) | 38 (3.6) | |
| High School | 1005 (29.5) | 463 (46.1) | 522 (51.9) | 20 (2.0) | |
| Graduate | 324 (9.5) | 193 (59.6) | 123 (38.0) | 8 (2.5) | |
| Job *** | |||||
| Managers and Professionals | 216 (6.3) | 96 (44.4) | 112 (51.9) | 8 (3.7) | <0.001 |
| Craft, Agricultural and Sales Workers | 814 (23.9) | 401 (49.3) | 384 (47.2) | 29 (3.6) | |
| Elementary Occupations | 799 (23.4) | 429 (53.7) | 351 (43.9) | 19 (2.4) | |
| Housewife | 415 (12.2) | 200 (48.2) | 207 (49.9) | 8 (1.9) | |
| Pensioner | 1164 (34.2) | 619 (65.9) | 295 (31.4) | 26 (2.8) | |
| Unemployed | 216 (6.3) | 64 (28.6) | 157 (70.1) | 3 (1.3) | |
| Marital Status *** | |||||
| Single | 561 (16.4) | 212 (37.8) | 344 (61.3) | 5 (0.9) | <0.001 |
| Married/Cohabiting | 2611 (76.5) | 1451 (55.6) | 1082 (41.4) | 78 (3.0) | |
| Separated/Divorced | 73 (2.1) | 28 (38.4) | 40 (54.8) | 5 (6.8) | |
| Widower | 166 (4.9) | 119 (71.7) | 42 (25.3) | 5 (3.0) | |
| MADP | ||
|---|---|---|
| Moderate (4–6) | Low (0–3) | |
| HR (95% CI) | HR (95% CI) | |
| All causes of Death | 1.09 (0.89; 1.34) | 1.46 (0.93; 2.28) |
| SHR (95% CI) | SHR (95% CI) | |
| CVD | 1.09 (0.74; 1.59) | 0.81 (0.30; 2.19) |
| Cr | 094 (0.60; 1.45) | 2.25 * (1.08; 4.70) |
| DS | 1.58 (0.94; 2.65) | 2.77 * (1.16; 6.63) |
| DOC | 1.08 (0.76; 1.53) | 0.52 (0.17; 1.62) |
| rMEDNA | ||
|---|---|---|
| Moderate (4–6) | Low (0–3) | |
| HR (95% CI) | HR (95% CI) | |
| All causes | 1.13 (0.90; 1.43) | 1.27 (0.96; 1.68) |
| SHR (95% CI) | SHR (95% CI) | |
| CVD | 0.97 (0.65; 1.45) | 0.82 (0.49; 1.38) |
| Cr | 1.58 (0.91; 2.75) | 1.83 * (1.00; 3.40) |
| DS | 1.07 (0.60; 1.90) | 0.79 (0.37; 1.69) |
| DOC | 1.18 (0.80; 1.75) | 1.35 (0.86; 2.13) |
| All Causes | CVD | DS | Cr | DOC | |
|---|---|---|---|---|---|
| HR (95% CI) | SHR (95% CI) | SHR (95% CI) | SHR (95% CI) | SHR (95% CI) | |
| MADP#rMEDNA | |||||
| High–High | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| High–Moderate | 1.24(0.93; 1.65) | 1.13 (0.69; 1.85) | 0.85 (0.42; 1.74) | 2.04 (0.99; 4.18) | 1.31 (0.82; 2.12) |
| High–Low | 1.26 (0.87; 1.22) | 0.83 (0.42; 1.65) | 0.62 (0.21; 1.78) | 1.67 (0.71; 3.96) | 1.59 (0.90; 2.79) |
| Moderate–High | 1.37 (0.90; 2.08) | 1.45 (0.70; 3.00) | 1.18 (0.40; 3.46) | 1.52 (0.56; 4.11) | 1.46 (0.71; 3.02) |
| Moderate–Moderate | 1.17 (0.82; 1.66) | 1.01 (0.54; 1.88) | 1.70 (0.77; 3.74) | 1.04 (0.42; 2.57) | 1.29 (0.72; 2.31) |
| Moderate–Low | 1.50 * (1.01; 2.26) | 1.13 (0.54; 2.36) | 0.77 (0.24; 2.45) | 2.82 * (1.21; 6.55) | 1.48 (0.75; 2.89) |
| Low–High | 0.57 (0.08; 4.12) | 1.71 (0.23; 12.8) | NE | NE | NE |
| Low–Moderate | 1.78 (0.97; 3.27) | 0.69 (0.16; 2.95) | 1.74 (0.47; 6.42) | 4.87 * (1.71; 13.9) | 0.73 (0.17; 3.09) |
| Low–Low | 2.29 * (1.04; 5.04) | 0.79 (0.11; 5.63) | 4.38 * (1.22; 15.8) | 3.33(0.72; 15.4) | 0.72 (0.10; 5.05) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campanella, A.; Bonfiglio, C.; Cuccaro, F.; Donghia, R.; Tatoli, R.; Giannelli, G. High Adherence to a Mediterranean Alcohol-Drinking Pattern and Mediterranean Diet Can Mitigate the Harmful Effect of Alcohol on Mortality Risk. Nutrients 2024, 16, 59. https://doi.org/10.3390/nu16010059
Campanella A, Bonfiglio C, Cuccaro F, Donghia R, Tatoli R, Giannelli G. High Adherence to a Mediterranean Alcohol-Drinking Pattern and Mediterranean Diet Can Mitigate the Harmful Effect of Alcohol on Mortality Risk. Nutrients. 2024; 16(1):59. https://doi.org/10.3390/nu16010059
Chicago/Turabian StyleCampanella, Angelo, Caterina Bonfiglio, Francesco Cuccaro, Rossella Donghia, Rossella Tatoli, and Gianluigi Giannelli. 2024. "High Adherence to a Mediterranean Alcohol-Drinking Pattern and Mediterranean Diet Can Mitigate the Harmful Effect of Alcohol on Mortality Risk" Nutrients 16, no. 1: 59. https://doi.org/10.3390/nu16010059
APA StyleCampanella, A., Bonfiglio, C., Cuccaro, F., Donghia, R., Tatoli, R., & Giannelli, G. (2024). High Adherence to a Mediterranean Alcohol-Drinking Pattern and Mediterranean Diet Can Mitigate the Harmful Effect of Alcohol on Mortality Risk. Nutrients, 16(1), 59. https://doi.org/10.3390/nu16010059






