Abstract
The negative chronotropic effects of eight Vaughan Williams Class I antiarrhythmic drugs were examined in guinea pig right atrial tissue preparations. The drugs decreased the spontaneous beating rate at concentrations overlapping with their therapeutic blood levels. Cibenzoline, aprindine, flecainide, and propafenone showed stronger effects; 10 µM of each drug decreased the beating rate to about 75% of initial values. Disopyramide, mexiletine, pilsicainide, and ranolazine showed weaker effects; 10 µM of each drug decreased the beating rate to about 90% of initial values. The potency of drugs correlated with the reported IC50 values to block the L-type Ca2+ channel current rather than the Na+ and K+ channel currents. The reported IC50 values for the blockade of the hyperpolarization-activated inward current (If) and the Na+-Ca2+ exchanger current were much higher than those for the blockade of the L-type Ca2+ channel current. These results indicate that the negative chronotropic effects of Class I antiarrhythmic drugs can be largely explained by their blockade of the L-type Ca2+ channel.
1. Introduction
Vaughan Williams Class I antiarrhythmic drugs, which block the voltage-dependent Na+ channel, exert their antiarrhythmic effects mainly through inhibition of the propagation of ectopic excitation through the myocardium [1,2,3]. They are used variously depending on their mode of action on the voltage-dependent Na+ channel, and on their pharmacokinetic properties. Class I antiarrhythmic drugs are moderately effective against various types of arrhythmia. However, the potential negative inotropic and chronotropic effects that might cause decreases in cardiac output limit their use in patients with reduced cardiac function. On the other hand, the development and clinical use of Class I antiarrhythmic drugs with novel modes of action on the Na+ channels are now in progress [2,3,4,5]. To optimize the clinical usage of Class I antiarrhythmic drugs and to develop new antiarrhythmic drugs with higher efficacy and safety, understanding the mechanism of their cardiosuppressive effects is essential.
The action potential of the myocardium is formed by several major ion channel currents. In the working myocardium (atrial and ventricular myocardium; Figure 1A), the inwardly rectifying K+ current (IK1) maintains the resting membrane potential. The inward Na+ and Ca2+ channel currents (INa and ICa) cause the rapid depolarization and the following plateau phase, respectively. The delayed rectifier potassium current (IK) flowing outward causes repolarization. In the sinus node (Figure 1B), several inward currents, including the hyperpolarization-activated cation current (If) and the Ca2+ channel current, causes the diastolic depolarization. This is followed by the action potential upstroke that is caused mainly by the Ca2+ channel current (ICa). The delayed rectifier potassium current (IK) is the major current for repolarization but its declination also contributes to the earlier half of diastolic depolarization. It is established that Class I antiarrhythmic drugs block the Na+ channel and reduce the upstroke of the action potential in the working myocardium. The resulting slowing of action potential propagation contributes to their antiarrhythmic effects. On the other hand, the ion channels that are responsible for the negative inotropic and chronotropic effects of Class I antiarrhythmic drugs are less understood.
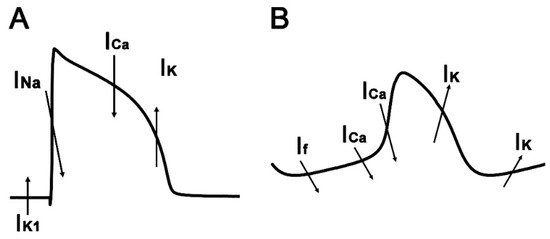
Figure 1.
The action potential waveform of the working myocardium (A) and the sinus node (B). The ion channel currents responsible for each segment are indicated by arrows. The upward and downward arrows indicate outward and inward currents, respectively.
In our previous study, we examined the negative inotropic effects of Class I antiarrhythmic drugs on isolated guinea pig ventricular myocardium and demonstrated that the negative inotropic effects correlate with the L-type Ca2+ channel blockade rather than the Na+ channel blockade [6]. In the present study, we examined the negative chronotropic effects of eight Class I antiarrhythmic drugs using isolated guinea pig right atria to obtain a birds-eye overview concerning the factors underlying their negative chronotropic effects. The results showed that negative chronotropic effects are observed in the therapeutic blood concentration range of these drugs. We analyzed the correlation between the decrease in the beating rate and blockade of Na+, Ca2+, and K+ channels, and concluded that the negative chronotropy could be best explained by blockade of the L-type Ca2+ channel.
2. Materials and Methods
2.1. Measurement of Beating Rate
The negative chronotropic effects of eight Class I antiarrhythmic drugs were examined in the isolated right atria from Hartley strain male guinea pigs. The procedures were the same as those in our previous studies [6,7,8]. The right atria were mounted in an organ bath that was filled with a physiological salt solution of the following composition: 118.4 mM NaCl, 4.7 mM KCl, 2.5 mM CaCl2, 1.2 mM MgSO4, 1.2 mM KH2PO4, 24.9 mM NaHCO3, and 11 mM glucose (pH = 7.4, 37 °C), gassed with 95% O2-5% CO2 and maintained at 36 ± 0.5 °C. The beating rate was analyzed by Power Lab System (AD Instruments, Dunedin, New Zealand).
2.2. Drugs and Chemicals
Pilsicainide was purchased from Alomone Labs (Jerusalem, Israel), disopyramide from FUJIFILM Wako Pure Chemical Corporation (Osaka, Japan), cibenzoline and aprindine from Cosmo Bio Co., Ltd. (Tokyo, Japan), flecainide and mexiletine from Sigma Aldrich (St. Louis, MO, USA), propafenone from LKT Laboratories, Inc. (St. Paul, MN, USA), and ranolazine from Tokyo Chemical Industry Co., Ltd. (Tokyo, Japan). Disopyramide, flecainide, propafenone, and ranolazine were dissolved in dimethyl sulfoxide and other chemicals in distilled water. Small aliquots of the drug solutions were added to the solution in the organ bath to obtain the desired final concentrations.
2.3. Statistics
All data were expressed as mean ± standard error of the mean (S.E.M). IC50 values were calculated by non-linear regression analysis using GraphPad Prism 8 (GraphPad Software Inc., San Diego, CA, USA). Pearson’s correlation coefficients (r) were used for evaluating correlations between the IC50 for the negative chronotropy and the IC50 for Na+, Ca2+, or K+ channel blockade. An r value closer to 1 was considered a strong correlation. Statistical analyses were performed using GraphPad Prism 8 (GraphPad Software Inc., San Diego, CA, USA). A p-value less than 0.05 was considered significant.
3. Results
The spontaneous beating rate of the guinea pig right atrial preparations were well maintained; the beating rate before the addition of drugs was 214.3 ± 2.6 bpm (n = 40). Class I antiarrhythmic drugs decreased the spontaneous beating rate of the right atria (Figure 2). The effects were dependent on the concentration of the drugs ranging from 0.1 µM to 30 µM; this concentration range includes or largely overlaps with the therapeutic plasma concentration of the drugs (Table 1). There was a difference in the potency among the drugs. Cibenzoline, aprindine, flecainide, and propafenone showed stronger effects; the beating rate in the presence of 10 µM of each drug was 74.3 ± 3.1% (n = 5) for cibenzoline, 75.0 ± 2.4% (n = 5) for aprindine, 78.4 ± 1.4% (n = 5) for flecainide, and 74.8 ± 3.4% (n = 5) for propafenone. Disopyramide, mexiletine, pilsicainide, and ranolazine showed weaker effects; the beating rate in the presence of 10 µM of each drug was 89.8 ± 4.4% (n = 5) for disopyramide, 94.8 ± 1.0% (n = 5) for mexiletine, 92.3 ± 1.0% (n = 5) for pilsicainide, and 92.1 ± 1.1% (n = 5) for ranolazine.
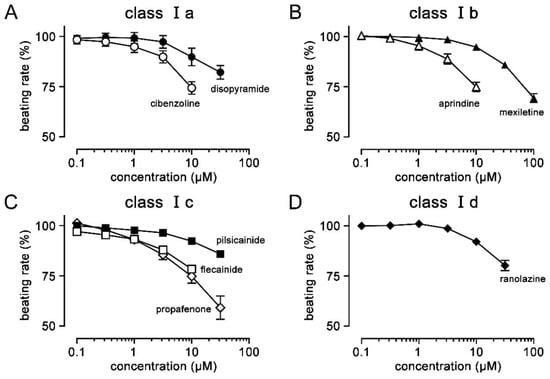
Figure 2.
Negative chronotropic effects of Class I antiarrhythmic drugs. The effects of drugs belonging to the Vaughn Williams classification Ia, Ib, Ic, and Id were shown in panels (A–D), respectively. The beating rate was expressed as a percentage of the values before application. Symbols and vertical bars indicate the mean ± S.E.M. (n = 5).

Table 1.
Therapeutic concentration range and IC50 values (µM) of Class I antiarrhythmic drugs.
To clarify whether the negative chronotropic effects of Class I antiarrhythmic drugs correlate with their Na+ channel-blocking effects, we analyzed our data using the reported potency of drugs against the Na+ channels (Table 1). The concentration of each drug was expressed as a ratio against its IC50 value for the Na+ channel current (Table 1) and was plotted on the ordinate. If the negative chronotropic effects were the result of Na+ channel blockade, the plot would converge on a single concentration-response curve. The result was actually different where the concentration-response curves were scattered, indicating that there was more than a 100-fold difference in the potency among the drugs (Figure 3A). Additionally, to examine the correlation by another method, virtual IC50 values for the negative chronotropy with each drug were calculated assuming that the beating rate reaches zero at the bottom of the concentration-response curve. The IC50 values for the negative chronotropy did not correlate with the IC50 values for the Na+ channel blockade (Figure 3B; r = 0.213, p = 0.613).
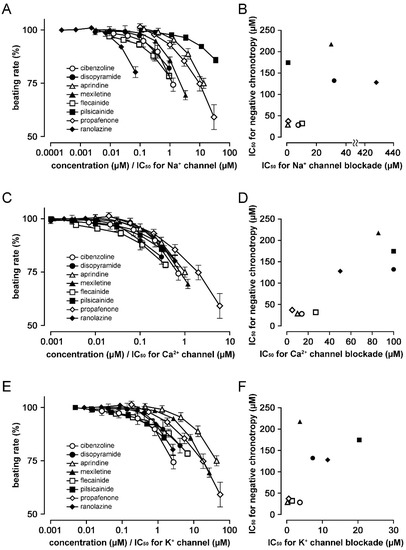
Figure 3.
Correlation between the negative chronotropic effects of Class I antiarrhythmic drugs and blockade of Na+, Ca2+, and K+ channels. The values for the negative chronotropic effects shown in Figure 2 were re-plotted against the concentration of each agent normalized as a ratio against the IC50 values (µM) of drugs for Na+ (A), Ca2+ (C), and K+ (E) channels. The correlation of IC50 values for negative chronotropy (ordinate) and IC50 values (abscissa) for the Na+ (B), Ca2+ (D), and K+ (F) channel blockade was plotted. IC50 values for each drug are shown in Table 1. The symbols used were open circles for cibenzoline, closed circles for disopyramide, open triangles for aprindine, closed triangles for mexiletine, open squares for flecainide, closed squares for pilsicainide, open diamonds for propafenone, and closed diamonds for ranolazine.
In contrast, when the concentration of each drug was expressed as a ratio against its IC50 value for the Ca2+ channel blockade (Table 1), the negative chronotropic effects of all drugs tended to converge on a single concentration-response curve; the difference in potency among drugs was decreased to less than 10-fold (Figure 3C). There was a strong correlation between the virtual IC50 for negative chronotropy and the IC50 for the L-type Ca2+ channel current (Figure 3D; r = 0.893, p = 0.0028).
To clarify whether the negative chronotropic effects of Class I antiarrhythmic drugs can be explained by their K+ channel-blocking effects, we analyzed our data using the reported potency of drugs against the hERG channel (Table 1). When the concentration of each drug was expressed as a ratio against the IC50 value for the hERG channel current, there was more than a 100-fold difference in the potency among the drugs (Figure 3E). The virtual IC50 for the negative chronotropy correlated relatively weakly with the IC50 for hERG channel blockade (Figure 3F; r = 0.610, p = 0.108).
4. Discussion
In the present study, we examined the negative chronotropic effects of eight Class I antiarrhythmic drugs in isolated guinea pig right atria under identical experimental conditions to obtain a birds-eye overview concerning the factor(s) underlying their cardio-suppressive effects (Figure 2). The results revealed that Class I antiarrhythmic drugs cause negative chronotropy in the concentration range overlapping with their therapeutic plasma concentration range (Table 1). In addition, differences in the negative chronotropic effects among drugs were observed; cibenzoline, aprindine, flecainide, and propafenone were more potent than disopyramide, mexiletine, pilsicainide, and ranolazine (Figure 2; Table 1).
Class I antiarrhythmic drugs are sub-classified based on their effects on the Na+ channel and action potential duration [2]. Class Ia antiarrhythmic drugs block the Na+ channel with intermediate potency; they also block K+ channels and prolong the action potential duration. Among the Class Ia drugs examined, cibenzoline showed stronger negative chronotropic effects than disopyramide. Class Ib antiarrhythmic drugs rapidly dissociate from the Na+ channel. Among the Class Ib drugs that were examined, aprindine showed stronger negative chronotropic effects than mexiletine. Class Ic antiarrhythmic drugs dissociate very slowly from the inactivated Na+ channel. Among the Class Ic drugs that were examined, flecainide and propafenone showed stronger negative chronotropic effects than pilsicainide. Class Id is a new subclass that is defined as inhibitors of the persistent Na+ current (Late INa). Ranolazine, which belongs to this subclass, showed a weak negative chronotropic effect, but this is unlikely to be the result of Na+ channel blockade, as discussed below. Thus, the negative chronotropic effect of Class I antiarrhythmic drugs does not correlate with the Vaughn Williams subclassification based on their Na+ channel-blocking properties. Thus, their effects on ion channels other than the Na+ channel had to be considered.
The action potential of the sinus node, the cardiac pacemaker, has a characteristic waveform that is different from that of the working myocardium [30]. In atrial and ventricular cardiomyocytes (Figure 1A), the inward rectifier K+ channel current (IK1) repolarizes the membrane potential towards the K+ equilibrium potential to maintain a resting membrane potential of around −80 mV. The rapid opening of the voltage-dependent Na+ channel results in a rapid depolarization forming the action potential upstroke. Class I antiarrhythmic drugs inhibit the propagation of excitation through inhibition of this rapid depolarization. In contrast, in the sinus node cardiomyocytes which lack IK1 (Figure 1B), the membrane potential oscillates in a more depolarized membrane potential range. The maximum diastolic potential of the sinus node is −55 to −65 mV, at which the voltage-dependent Na+ channels are mostly inactivated. Thus, the contribution of the Na+ channel current to the sinus node action potential is very small, if any. In fact, tetrodotoxin, which blocks both the transient and persistent components of the Na+ channel current, has no effect or only a small effect on the sinus node action potential waveform and firing rate [31,32,33]. Moreover, the negative chronotropic effects of Class I antiarrhythmic drugs did not correlate with their Na+ channel-blocking effects (Figure 3). These results and considerations confirm that factors other than the Na+ channel blockade are the cause for negative chronotropy.
In the sinus node, the action potential upstroke is formed by the L-type Ca2+ channel current. This is preceded by a diastolic depolarization phase which is formed by several ionic mechanisms including the L-type Ca2+ channel current [30]. Pharmacological inhibition of the diastolic depolarization prolongs the time until the next rapid depolarization and causes negative chronotropy. The L-type Ca2+ channel current is the most important pacemaking current because the membrane potential range for diastolic depolarization overlaps with the threshold voltage range for the activation of the L-type Ca2+ channel. Ca2+ antagonists including Class IV antiarrhythmic drugs are reported to block the L-type Ca2+ channel and decrease the slope of the diastolic depolarization, as well as the rapid depolarization, resulting in negative chronotropy [34]. In the present study, both the concentration-response relationship analysis (Figure 3C) and the correlation analysis with IC50 values (Figure 3D) showed that the chronotropic effects of Class I antiarrhythmic drugs strongly correlate with their L-type Ca2+ channel blocking potencies (Figure 3). At concentrations corresponding to their estimated IC50 value for the L-type Ca2+ channel blockade, the beating rate of the right atria was decreased to about 80% of the initial rate. This was the same as the case with the Ca2+ antagonist, nifedipine [35,36]. These results indicated that the negative chronotropic effects of Class I antiarrhythmic drugs are mediated by the L-type Ca2+ channel blockade.
Other ionic mechanisms that are involved in the diastolic depolarization are unlikely to be the major mechanism mediating the negative chronotropic effect of Class I antiarrhythmic drugs. The time-dependent delayed rectifier K+ channel current (IK) increases during the action potential and causes repolarization towards the maximum diastolic potential. A gradual decline in this current also contributes to the early phase of diastolic depolarization. Blockade of the delayed rectifier K+ channel current appears to result in negative chronotropy only at high concentrations of the blocker. E-4031, a selective blocker of the delayed rectifier K+ channel current, only decreased the beating rate of the guinea pig right atria to 80% of the initial value at 100 nM, even though its IC50 value was 7.7 nM [37,38]; this data point for E-4031 would be located on the upper right position in Figure 3E. This means that the negative chronotropic effects of most Class I antiarrhythmic drugs are stronger than those that are attributable to K+ channel blockade, and implies that mechanisms other than the K+ channel blockade are the determinants of negative chronotropic potency. The observation that the correlation between negative chronotropy and delayed rectifier K+ channel blockade was relatively weak also supports this view (Figure 3E,F).
The hyperpolarization-activated cation current (If) has been postulated to play a major role for pacemaking of the sinus node [39], although a controversy still remains concerning its degree of contribution [40]. Ivabradine, a blocker of this channel, decreases beating rate and is clinically used as a bradycardiac agent, but the drug was reported to also block the delayed rectifier K+ channel current [41]. Concerning the Class I antiarrhythmic drugs that were examined, aprindine, cibenzoline, and propafenone were reported to block this current with IC50 values of 43.7 µM, 46.8 µM, and 14.3 µM, respectively [12]. Other drugs have very weak or no effect on this channel. This suggests that blocking the hyperpolarization-activated cation current might also play a role in negative chronotropy, particularly for propafenone. However, blockade of the hyperpolarization-activated cation current cannot be the major determinant of the negative chronotropic effects among Class I antiarrhythmic drugs as the blocking effect of other drugs is either very weak or absent.
The Na+-Ca2+ exchanger generates a net inward current when it pumps out one Ca2+ in exchange for the influx of three Na+. This current has been postulated to contribute to the diastolic depolarization of the sinus node [33], but concerning the guinea pig sinus node, experimental [8] and computational [42] evidence against the contribution of this current has also been reported. Among the Class I antiarrhythmic drugs that were examined in the present study, only aprindine and cibenzoline were reported to inhibit this current with IC50 values of 84 µM and 52 µM, respectively [43,44,45].
The T-type Ca2+ channel current was reported to be involved in the diastolic depolarization of the sinus node in various animal species; the contribution of this current appears to be larger in animals of smaller size, during early developmental stages, and under pathological conditions [46,47]. A selective T-type Ca2+ channel blocker, R(-)-efonidipine, caused negative chronotropy in the guinea pig right atria, but the effect was small [48]. The sustained inward current is an inward current that is activated in the membrane potential range of the diastolic depolarization of the sinus node [49], whose molecular identity was reported to be a subtype of the voltage-dependent L-type Ca2+ channel, CaV1.3 [50]. To the best of our knowledge, blockade of the T-type Ca2+ channel or the CaV1.3 L-type Ca2+ channel has not been reported with the antiarrhythmic drugs that were examined in the present study.
The present results and the discussion above led us to the conclusion that the major common mechanism for the negative chronotropic effects of Class I antiarrhythmic drugs is the blockade of the L-type Ca2+ channel. At concentrations corresponding to their reported IC50 values for the L-type Ca2+ channel blockade, the beating rate of the right atria was decreased to about 80% of the initial value. This is different from the case with negative inotropy, in which the contractile force was decreased to about 50% of the initial value at concentrations corresponding to their reported IC50 value for the L-type Ca2+ channel blockade [6]. In the case of myocardial contraction, the intracellular Ca2+ activating the myofilaments is supplied either by the transsarcolemmal influx through the L-type Ca2+ channel or by the subsequent Ca2+-induced-Ca2+ release from the sarcoplasmic reticulum. Thus, the L-type Ca2+ channel is involved in the contractile mechanism, and it is reasonable that the extent of Ca2+ channel blockade directly correlates with negative inotropy. In contrast, in the case of sinus node pacemaking, the L-type Ca2+ channel and other ionic mechanisms mentioned above work additively to form the diastolic depolarization. Thus, the role of the L-type Ca2+ channel blockade in the negative chronotropy induced by class I antiarrhythmic drugs is partial.
Our present and previous studies indicated that the Na+ channel blockade itself plays only a minor role in the negative chronotropic and inotropic effects of Class I antiarrhythmic drugs [6]. This implies that modifying the mode of action of Class I antiarrhythmic drugs on the Na+ channel may increase their therapeutic potential without increasing the risk of cardiosuppression. A promising trend is the development of blockers selective for the persistent component of the Na+ channel current, late INa [51]. Ranolazine, a late INa blocker with multiple sites of action on the sarcolemma and sarcoplasmic reticulum, and also affects energy metabolism [29,52,53], showed a weak negative chronotropic effect (Figure 2). More selective blockers of late INa, GS-458967 [54] and NCC-3902 [7], were reported to inhibit the automaticity of the pulmonary vein myocardium, which is attracting attention as the ectopic pacemaker that is responsible for atrial fibrillation [55,56]. In canine rapid atrial pacing models, NCC-3902 prolonged the effective refractory period and intra-atrial conduction time in a dose-dependent manner and suppressed the induction of atrial fibrillation [57]. These compounds appear to have no cardiosuppressive or arrhythmogenic effects so far, and their development as antiarrhythmic drugs are highly anticipated.
In conclusion, the present study showed that the negative chronotropic effects of Class I antiarrhythmic drugs correlate with the blockade of Ca2+ channels, but not with the Na+ and K+ channels. Thus, novel blockers of the Na+ channel with minimum cardiosuppression can probably be developed, provided that they have no Ca2+ channel-blocking activity.
Author Contributions
Conceptualization, H.H. and H.T.; investigation, H.H. and K.O.; writing—original draft preparation, H.T.; writing—review and editing, H.H., S.H., I.N. and H.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by JSPS KAKENHI Grant numbers JP20K16013, JP20K07299 and JP20K07091. H.H. received Nagai Memorial Research Scholarship from the Pharmaceutical Society of Japan (N-201503).
Institutional Review Board Statement
All experiments were performed in accordance with the Guiding Principles for the Care and Use of Laboratory Animals approved by The Japanese Pharmacological Society and the Guide for the Care and Use of Laboratory Animals at the Faculty of Pharmaceutical Sciences, Toho University (22-41-507).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Vaughan Williams, E.M. Classification of antiarrhythmic drugs. Pharmacol. Ther. 1975, 1, 115–138. [Google Scholar] [CrossRef]
- Lei, M.; Wu, L.; Terrar, D.A.; Huang, C.L. Modernized Classification of Cardiac Antiarrhythmic Drugs. Circulation 2018, 138, 1879–1896. [Google Scholar] [CrossRef] [PubMed]
- The Japanese Circulation Society and Japanese Heart Rhythm Society Joint Working Group. JCS/JHRS 2020 Guideline on Pharmacotherapy of Cardiac Arrhythmias. Circ. J. 2022, 86, 1790–1924. [Google Scholar] [CrossRef]
- Roden, D.M. Pharmacology and toxicology of Nav1.5-class I anti-arrhythmic drugs. Card. Electrophysiol. Clin. 2014, 6, 695–704. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, M.; Nattel, S. The past, present, and potential future of sodium channel block as an atrial fibrillation suppressing strategy. J. Cardiovas. Pharmacol. 2015, 66, 432–440. [Google Scholar] [CrossRef]
- Hiiro, H.; Hashimoto, T.; Mizoguchi, M.; Kaneko, M.; Deguchi, N.; Takahashi, Y.; Hamaguchi, S.; Namekata, I.; Tanaka, H. Negative inotropic effects of class I antiarrhythmics on guinea pig ventricular myocardium: Correlation with L-type Ca2+ channel blockade. Biol. Pharm. Bull. 2023, 46, 133–137. [Google Scholar] [CrossRef]
- Namekata, I.; Hiiro, H.; Odaka, R.; Saito, T.; Hamaguchi, S.; Tsukamoto, T.; Ishikawa, R.; Katayama, Y.; Kondo, Y.; Tanaka, H. Inhibitory effect of a late sodium current blocker, NCC-3902, on the automaticity of the guinea pig pulmonary vein myocardium. Biol. Pharm. Bull. 2022, 45, 1644–1652. [Google Scholar] [CrossRef]
- Namekata, I.; Jitsukata, K.; Fukuda, A.; Odaka, R.; Hamaguchi, S.; Tanaka, H. Intracellular Ca2+-mediated mechanisms for the pacemaker depolarization of the mouse and guinea pig sinus node tissue. Biomolecules 2022, 12, 377. [Google Scholar] [CrossRef]
- Takada, M.; Goto, T.; Kotake, T.; Saito, M.; Kawato, N.; Nakai, M.; Gunji, T.; Shibakawa, M. Appropriate Dosing of Antiarrhythmic Drugs in Japan Requires Therapeutic Drug Monitoring*. J. Clin. Pharm. Ther. 2005, 30, 5–12. [Google Scholar] [CrossRef]
- Kodama, I.; Ogawa, S.; Inoue, H.; Kasanuki, H.; Kato, T.; Mitamura, H.; Hiraoka, M.; Sugimoto, T. Profiles of aprindine, cibenzoline, pilsicainide and pirmenol in the framework of the Sicilian Gambit. The Guideline Committee for Clinical Use of Antiarrhythmic Drugs in Japan (Working Group of Arrhythmias of the Japanese Society of Electrocardiology). Jpn. Circ. J. 1999, 63, 1–12. [Google Scholar] [CrossRef]
- Hiramatsu, M.; Wu, L.M.; Hirano, Y.; Kawano, S.; Furukawa, T.; Hiraoka, M. Block of HERG current expressed in HEK293 cells by the Na-channel blocker cibenzoline. Heart Vessels. 2004, 19, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Tamura, A.; Ogura, T.; Umemura, H.; Reien, Y.; Kishimoto, T.; Nagai, T.; Komuro, I.; Miyazaki, M.; Nakaya, H. Effects of antiarrhythmic drugs on the hyperpolarization-activated cyclic nucleotide-gated channel current. J. Pharmacol. Sci. 2009, 110, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Satoh, H. Comparative actions of cibenzoline and disopyramide on I(Kr) and I(Ks) currents in rat sino-atrial nodal cells. Eur. J. Pharmacol. 2000, 407, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Harchi, A.E.; Zhang, Y.H.; Hussein, L.; Dempsey, C.E.; Hancox, J.C. Molecular determinants of hERG potassium channel inhibition by disopyramide. J. Mol. Cell. Cardiol. 2012, 52, 185–190. [Google Scholar] [CrossRef]
- Yoshida, H.; Horie, M.; Otani, H.; Takano, M.; Tsuji, K.; Kubota, T.; Fukunami, M.; Sasayama, S. Characterization of a novel missense mutation in the pore of HERG in a patient with long QT syndrome. J. Cardiovas. Electrophysiol. 1999, 10, 1262–1270. [Google Scholar] [CrossRef] [PubMed]
- Yonemizu, S.; Masuda, K.; Kurata, Y.; Notsu, T.; Higashi, Y.; Fukumura, K.; Li, P.; Ninomiya, H.; Miake, J.; Tsuneto, M.; et al. Inhibitory effects of class I antiarrhythmic agents on Na+ and Ca2+ currents of human iPS cell-derived cardiomyocytes. Regen. Ther. 2019, 10, 104–111. [Google Scholar] [CrossRef]
- Ono, K.; Kiyosue, T.; Arita, M. Comparison of the inhibitory effects of mexiletine and lidocaine on the calcium current of single ventricular cells. Life Sci. 1986, 39, 1465–1470. [Google Scholar] [CrossRef] [PubMed]
- Gualdani, R.; Tadini-Buonisegni, F.; Roselli, M.; Defrenza, I.; Contino, M.; Colabufo, N.A.; Lentini, G. Inhibition of hERG potassium channel by the antiarrhythmic agent mexiletine and its metabolite m-hydroxymexiletine. Pharmacol. Res. Perspect. 2015, 3, e00160. [Google Scholar] [CrossRef]
- Heath, B.M.; Cui, Y.; Worton, S.; Lawton, B.; Ward, G.; Ballini, E.; Doe, C.P.; Ellis, C.; Patel, B.A.; McMahon, N.C. Translation of flecainide- and mexiletine-induced cardiac sodium channel inhibition and ventricular conduction slowing from nonclinical models to clinical. J. Pharmacol. Toxicol. Methods 2011, 63, 258–268. [Google Scholar] [CrossRef]
- Kramer, J.; Obejero-Paz, C.A.; Myatt, G.; Kuryshev, Y.A.; Bruening-Wright, A.; Verducci, J.S.; Brown, A.M. MICE models: Superior to the HERG model in predicting Torsade de Pointes. Sci. Rep. 2013, 3, 2100. [Google Scholar] [CrossRef]
- Melgari, D.; Zhang, Y.; El Harchi, A.; Dempsey, C.E.; Hancox, J.C. Molecular basis of hERG potassium channel blockade by the class Ic antiarrhythmic flecainide. J. Mol. Cell. Cardiol. 2015, 86, 42–53. [Google Scholar] [CrossRef]
- Inomata, N.; Ishihara, T.; Akaike, N. SUN 1165: A new antiarrhythmic Na current blocker in ventricular myocytes of guinea-pig. Comp. Biochem. Physiol. C Comp. Pharmacol. Toxicol. 1987, 87, 237–243. [Google Scholar] [CrossRef]
- Wu, L.M.; Orikabe, M.; Hirano, Y.; Kawano, S.; Hiraoka, M. Effects of Na+ channel blocker, pilsicainide, on HERG current expressed in HEK-293 cells. J. Cardiovasc. Pharmacol. 2003, 42, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Siddoway, L.A.; Roden, D.M.; Woosley, R.L. Clinical Pharmacology of Propafenone: Pharmacokinetics, Metabolism and Concentration-Response Relations. Am. J. Cardiol. 1984, 54, 9D–12D. [Google Scholar] [CrossRef]
- Antzelevitch, C.; Nesterenko, V.; Shryock, J.C.; Rajamani, S.; Song, Y.; Belardinelli, L. The role of late I Na in development of cardiac arrhythmias. Handb. Exp. Pharmacol. 2014, 221, 137–168. [Google Scholar] [CrossRef] [PubMed]
- Delgado, C.; Tamargo, J.; Henzel, D.; Lorente, P. Effects of propafenone on calcium current in guinea-pig ventricular myocytes. Br. J. Pharmacol. 1993, 108, 721–727. [Google Scholar] [CrossRef]
- Arias, C.; González, T.; Moreno, I.; Caballero, R.; Delpón, E.; Tamargo, J.; Valenzuela, C. Effects of propafenone and its metabolite, 5-hydroxypropafenone, on HERG channels. Cardiovas. Res. 2003, 57, 660–669. [Google Scholar] [CrossRef] [PubMed]
- Antzelevitch, C.; Burashnikov, A.; Sicouri, S.; Belardinelli, L. Electrophysiological Basis for the Antiarrhythmic Actions of Ranolazine. Heart Rhythm. 2011, 8, 1281. [Google Scholar] [CrossRef]
- Antzelevitch, C.; Belardinelli, L.; Zygmunt, A.C.; Burashnikov, A.; Di Diego, J.M.; Fish, J.M.; Cordeiro, J.M.; Thomas, G. Electrophysiological effects of ranolazine, a novel antianginal agent with antiarrhythmic properties. Circulation 2004, 110, 904–910. [Google Scholar] [CrossRef]
- Satoh, H. Sino-atrial nodal cells of mammalian hearts: Ionic currents and gene expression of pacemaker ionic channels. J. Smooth Muscle Res. 2003, 39, 175–193. [Google Scholar] [CrossRef]
- Kodama, I.; Nikmaram, M.R.; Boyett, M.R.; Suzuki, R.; Honjo, H.; Owen, J.M. Regional differences in the role of the Ca2+ and Na+ currents in pacemaker activity in the sinoatrial node. Am. J. Physiol. 1997, 272, H2793–H2806. [Google Scholar] [CrossRef] [PubMed]
- Muramatsu, H.; Nathan, R.D.; Shimura, T. A TTX-sensitive transient Na+ current recorded in morphologically identified primary pacemaker cells. J. Nippon. Med. Sch. 1999, 66, 350–352. [Google Scholar] [CrossRef]
- Sanders, L.; Rakovic, S.; Lowe, M.; Mattick, P.A.D.; Terrar, D.A. Fundamental importance of Na+–Ca2+ exchange for the pacemaking mechanism in the guina-pig sino-atrial node. J. Physiol. 2006, 571, 639–649. [Google Scholar] [CrossRef] [PubMed]
- Masumiya, H.; Tanaka, H.; Shigenobu, K. Effects of Ca2+ channel antagonists on sinus node: Prolongation of late phase 4 depolarization by efonidipine. Eur. J. Pharmacol. 1997, 335, 15–21. [Google Scholar] [CrossRef]
- Yamamoto, M.; Gotoh, Y.; Imaizumi, Y.; Watanabe, M. Mechanisms of long-lasting effects of benidipine on Ca current in guinea-pig ventricular cells. Br. J. Pharmacol. 1990, 100, 669–676. [Google Scholar] [CrossRef]
- Hof, R.P.; Scholtysik, G. Effects of the calcium antagonist PY 108-068 on myocardial tissues in vitro and on reflex tachycardia in vivo. J. Cardiovas. Pharmacol. 1983, 5, 176–183. [Google Scholar] [CrossRef]
- Wettver, E.; Scholtysik, G.; Schaad, A.; Himmel, H.; Ravens, U. Effects of the new class III antiarrhythmic drug E-4031 on myocardial contractility and electrophysiological parameters. J. Cardiovas. Pharmacol. 1991, 17, 480–487. [Google Scholar] [CrossRef]
- Zhou, Z.; Gong, Q.; Ye, B.; Fan, Z.; Makielski, J.C.; Robertson, G.A.; January, C.T. Properties of HERG channels stably expressed in HEK293 cells studied at physiological temperature. Biophys. J. 1998, 74, 230–241. [Google Scholar] [CrossRef] [PubMed]
- Denyer, J.C.; Brown, H.F. Pacemaking in rabbit isolated sino-atrial node cells during Ca+ block of the hyperpolarization-activated current if. J. Physiol. 1990, 429, 401–409. [Google Scholar] [CrossRef]
- Sohn, H.G.; Vassalle, M. Cesium effects on dual pacemaker mechanisms in guinea pig sinoatrial node. J. Mol. Cell. Cardiol. 1995, 27, 563–577. [Google Scholar] [CrossRef] [PubMed]
- Melgari, D.; Brack, K.E.; Zhang, C.; Zhang, Y.; El Harchi, A.; Mitcheson, J.S.; Dempsey, C.E.; Ng, G.A.; Hancox, J.C. hERG potassium channel block by the HCN channel inhibitor bradycardic agent ivabradine. J. Am. Heart Assoc. 2015, 4, e001813. [Google Scholar] [CrossRef]
- Himeno, Y.; Toyoda, F.; Satoh, H.; Amano, A.; Cha, C.Y.; Matsuura, H.; Noma, A. Minor contribution of cytosolic Ca2+ transients to the pacemaker rhythm in guinea pig sinoatrial node cells. Am. J. Physiol. Heart Circ. Physiol. 2011, 300, H251–H261. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Iwamoto, T.; Shigekawa, M.; Kimura, J. Inhibitory effect of aprindine on Na+/Ca2+ exchange current in guinea-pig cardiac ventricular myocytes. Br. J. Pharmacol. 2002, 136, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Koide, Y.; Kimura, J. Topics on the Na+/Ca2+ exchange: Pharmacological characterization of Na+/Ca2+ exchanger inhibitors. J. Pharmacol. Sci. 2006, 102, 7–16. [Google Scholar] [CrossRef]
- Yamakawa, T.; Watanabe, Y.; Watanabe, H.; Kimura, J. Inhibitory effect of cibenzoline on Na+/Ca2+ exchange current in guinea-pig cardiac ventricular myocytes. J. Pharmacol. Sci. 2012, 120, 59–62. [Google Scholar] [CrossRef] [PubMed]
- Ono, K.; Iijima, T. Pathophysiological significance of T-type Ca2+ channels: Properties and functional roles of T-type Ca2+ channels in cardiac pacemaking. J. Pharmacol. Sci. 2005, 99, 197–204. [Google Scholar] [CrossRef]
- Ono, K.; Iijima, T. Cardiac T-type Ca2+ channels in the heart. J. Mol. Cell. Cardiol. 2010, 48, 65–70. [Google Scholar] [CrossRef]
- Tanaka, H.; Komikado, C.; Namekata, I.; Nakamura, H.; Suzuki, M.; Tsuneoka, Y.; Shigenobu, K.; Takahara, A. Species difference in the contribution of T-type Ca2+ current to cardiac pacemaking as revealed by R(−)-efonidipine. J. Pharmacol. Sci. 2008, 107, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Mitsuiye, T.; Shinagawa, Y.; Noma, A. Sustained inward current during pacemaker depolarization in mammalian sinoatrial node cells. Circ. Res. 2000, 87, 88–91. [Google Scholar] [CrossRef] [PubMed]
- Toyoda, F.; Mesirca, P.; Dubel, S.; Ding, W.G.; Striessnig, J.; Mangoni, M.E.; Matsuura, H. Cav1.3 L-type Ca2+ channel contributes to the heartbeat by generating a dihydropyridine-sensitive persistent Na+ current. Sci. Rep. 2017, 7, 7869. [Google Scholar] [CrossRef]
- Belardinelli, L.; Giles, W.R.; Rajamani, S.; Karagueuzian, H.S.; Shryock, J.C. Cardiac late Na+ current: Proarrhythmic effects, roles in long QT syndromes, and pathological relationship to CaMKII and oxidative stress. Heart Rhythm. 2014, 12, 440–448. [Google Scholar] [CrossRef]
- Parikh, A.; Mantravadi, R.; Kozhevnikov, D.; Roche, M.A.; Ye, Y.; Owen, L.J.; Puglisi, J.L.; Abramson, J.J.; Salama, G. Ranolazine stabilizes cardiac ryanodine receptors: A novel mechanism for the suppression of early afterdepolarization and torsades de pointes in long QT type 2. Heart Rhythm. 2012, 9, 953–960. [Google Scholar] [CrossRef]
- Rouhana, S.; Virsolvy, A.; Fares, N.; Richard, S.; Thireau, J. Ranolazine: An old drug with emerging potential; lessons from pre-clinical and clinical investigations for possible repositioning. Pharmaceuticals 2021, 15, 31. [Google Scholar] [CrossRef]
- Irie, M.; Hiiro, H.; Hamaguchi, S.; Namekata, I.; Tanaka, H. Involvement of the persistent Na+ current in the diastolic depolarization and automaticity of the guinea pig pulmonary vein myocardium. J. Pharmacol. Sci. 2019, 141, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Namekata, I.; Tsuneoka, Y.; Tanaka, H. Electrophysiological and pharmacological properties of the pulmonary vein myocardium. Biol. Pharm. Bull. 2013, 36, 2–7. [Google Scholar] [CrossRef]
- Takahara, A.; Hagiwara, M.; Namekata, I.; Tanaka, H. Pulmonary vein myocardium as a possible pharmacological target for the treatment of atrial fibrillation. J. Pharmacol. Sci. 2014, 126, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Namekata, I.; Hiiro, H.; Odaka, R.; Saito, T.; Hamaguchi, S.; Tsukamoto, T.; Hamaguchi, S.; Ishikawa, R.; Kawai, Y.; Katayama, Y.; et al. NCC-3902, a novel late sodium current blocker, exhibit potent antiarrhythmic effect in isolated guinea pig pulmonary vein and canine rapid atrial pacing model. In Proceedings of the 95th Annual Meeting of the Japanese Pharmacological Society, Fukuoka, Japan, 7–9 March 2022. 1-LBS-02. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).