Neonatal Intracranial Hemorrhage with a Dramatic Outcome Due to Maternal Anti CD36 Antibodies
Abstract
:1. Introduction
2. Case Presentation
2.1. Laboratory Investigations
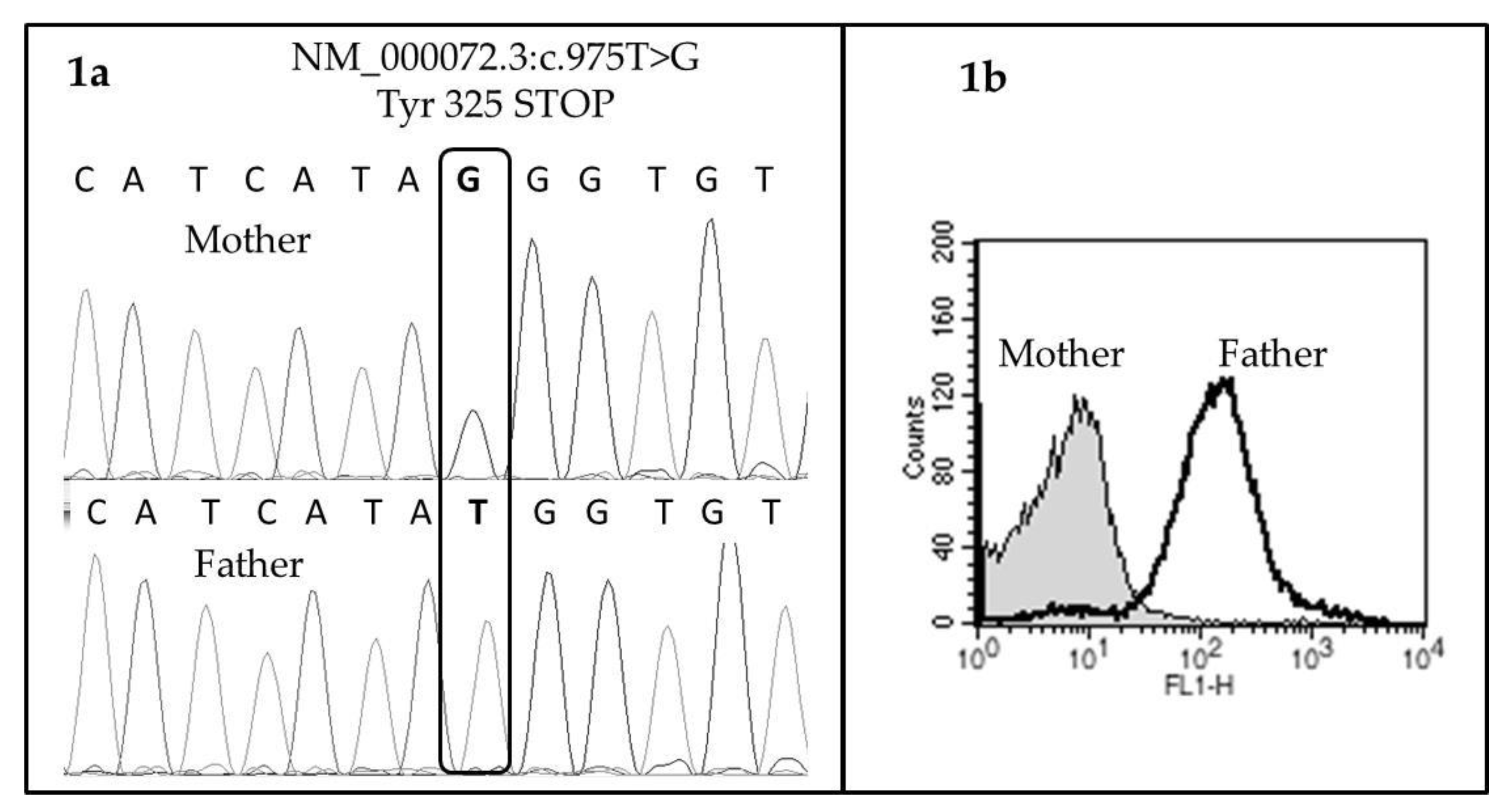
2.2. CD36 Deficiency on Maternal Platelets and Identification of the Mutation
3. How to Manage a Future Pregnancy?
4. Conclusions
Conflicts of Interest
References
- Curtis, B.R.; Aster, R.H. Incidence of the Nak(a)-negative platelet phenotype in African Americans is similar to that of Asians. Transfusion 1996, 36, 331–334. [Google Scholar] [CrossRef] [PubMed]
- Kiefel, V.; Santoso, S.; Weisheit, M.; Mueller-Eckhardt, C. Monoclonal antibody—Specific immobilization of platelet antigens (MAIPA): A new tool for the identification of platelet-reactive antibodies. Blood 1987, 70, 1722–1726. [Google Scholar] [PubMed]
- Daviet, L.; Craig, A.G.; McGregor, L.; Pinches, R.; Wild, T.F.; Berendt, A.R.; Newbold, C.I.; Mcgregor, J.L. Characterization of two vaccinia CD36 recombinant-virus-generated monoclonal antibodies (10/5, 13/10): Effects on malarial cytoadherence and platelet functions. Eur. J. Biochem. 1997, 243, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Yanai, H.; Chiba, H.; Fujiwara, H.; Morimoto, M.; Abe, K.; Yoshida, S.; Takahashi, Y.; Fuda, H.; Hui, S.-P.; Akita, H.; et al. Phenotype-genotype correlation in CD36 deficiency types I. and II. Thromb. Haemost. 2000, 84, 436–441. [Google Scholar] [CrossRef] [PubMed]
- Aitman, T.J.; Cooper, L.D.; Norsworthy, P.J.; Wahid, F.N.; Gray, J.K.; Curtis, B.R.; McKeigue, P.M.; Kwiatkowski, D.; Greenwood, B.M.; Snow, R.W.; et al. Malaria susceptibility and CD36 mutation. Nature 2000, 405, 1015–1016. [Google Scholar] [CrossRef] [PubMed]
- Curtis, B.R.; Ali, S.; Glazier, A.M.; Ebert, D.D.; Aitman, T.J.; Aster, R.H. Isoimmunization against CD36 (glycoprotein IV): Description of four cases of neonatal isoimmune thrombocytopenia and brief review of the literature. Transfusion 2002, 42, 1173–1179. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, G.; Drame, M.; Martageix, C.; Kaplan, C. Prediction of the fetal status in noninvasive management of alloimmune thrombocytopenia. Blood 2011, 117, 3209–3213. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertrand, G.; Renac, V.; Lefaix, M.-C.; Nivet, C.; Trudel, E.; Richard, L. Neonatal Intracranial Hemorrhage with a Dramatic Outcome Due to Maternal Anti CD36 Antibodies. Reports 2019, 2, 7. https://doi.org/10.3390/reports2010007
Bertrand G, Renac V, Lefaix M-C, Nivet C, Trudel E, Richard L. Neonatal Intracranial Hemorrhage with a Dramatic Outcome Due to Maternal Anti CD36 Antibodies. Reports. 2019; 2(1):7. https://doi.org/10.3390/reports2010007
Chicago/Turabian StyleBertrand, Gérald, Virginie Renac, Marie-Christine Lefaix, Carl Nivet, Elise Trudel, and Lucie Richard. 2019. "Neonatal Intracranial Hemorrhage with a Dramatic Outcome Due to Maternal Anti CD36 Antibodies" Reports 2, no. 1: 7. https://doi.org/10.3390/reports2010007
APA StyleBertrand, G., Renac, V., Lefaix, M.-C., Nivet, C., Trudel, E., & Richard, L. (2019). Neonatal Intracranial Hemorrhage with a Dramatic Outcome Due to Maternal Anti CD36 Antibodies. Reports, 2(1), 7. https://doi.org/10.3390/reports2010007




