Abstract
Background: An effective risk assessment and management methodology is essential to minimize/mitigate health risks associated with firefighting activities. The use of a self-contained breathing apparatus (SCBA) is mandatory during structure fires to protect firefighters from hazardous fire effluents, yet the protectiveness of the SCBA system has rarely been evaluated. Objective: This study characterizes, for the first time, the levels of 18 polycyclic aromatic hydrocarbons (PAHs) inside the SCBA facemask, during 7 structure-firefighting exercises and estimates associated respiratory risks. Methods: Cotton disk samples were collected via passive air sampling and analyzed using liquid chromatography with fluorescence and UV–Vis detection. Results: Levels of total PAHs (∑PAHs: 9.17–29.6 ng/m3) and ∑PAHscarcinogenic (0.41–5.73 ng/m3) were below the occupational limits defined by governmental agencies. The low-molecular-weight PAHs were predominant (79.5–91.4%), and the (possible/known) carcinogenic naphthalene (0.26–2.00 ng/m3), anthracene (0.088–0.31 ng/m3), chrysene (0.046–0.39 ng/m3), benzo(b+j)fluoranthene (0.18–0.40 ng/m3), and benzo(a)pyrene (0.041–0.18 ng/m3) were detected in all samples. The respiratory health risk analysis demonstrated negligible risks associated with the inhalation of PAHs. A health principal component analysis could identify firefighters at increased respiratory risk. Conclusions: The effectiveness of SCBA was demonstrated, reinforcing the need to ensure its correct use during all the phases of structure fires, including during overhaul.
1. Introduction
The occupational activity as a firefighter is carcinogenic to humans (Group 1), and there is scientific evidence suggesting that this occupation is genotoxic, induces epigenetic alterations, oxidative stress, chronic inflammation, and modulates receptor-mediated effects [1]. An efficient fire risk assessment and management approach promotes firefighters’ health by identifying occupational hazards and improving safety measures [2,3]. Concerning chemical risk factors, firefighters are exposed to a wide variety of health-hazardous compounds presented in fire emissions [e.g., carbon monoxide, flame retardants, metals, dioxins, phthalates, particulate matter, volatile organic compounds, including polycyclic aromatic hydrocarbons (PAHs)] [1,4]. Inhalation is the main route of firefighters’ exposure to fire emissions, and to mitigate or minimize the negative impacts on firefighters’ health, fire risk assessment and management methodologies are crucial to implement. The upper respiratory tract is the most protected area when using a flash hood or self-contained breathing apparatus (SCBA) during forest or structure (urban) fires, respectively. During structure fires, concentrations of fire effluents are considerably higher compared to the levels registered during wildland fires [1] and more complex due to the wide variety of burned materials (e.g., plastics, paint, varnishes, furniture, rubber, etc.) and the superior flame temperature reached in those events [5,6,7,8]. Previous studies monitored the presence of PAHs in the personal air of firefighters during structure fires [9,10,11,12,13,14,15] and reported total levels of PAHs ranging from 0.0083 mg/m3 during emergency fire suppression [14] and 78.2 mg/m3 in a controlled residential fire [11]. The majority of studies reported PAH concentrations exceeding the available occupational guidelines set by the National Institute for Occupational Safety and Health (NIOSH; 100 µg/m3) [16] and the occupational limit defined by the Occupational Safety and Health Administration (OSHA; 200 µg/m3) [17]. These findings raised concerns about firefighters’ exposure via inhalation to fire emissions released during structure fires, even when using SCBAs, as they often remove the equipment to relieve physical and thermal discomfort, particularly during overhaul and fire investigation phases, when hazardous emissions may still be present in the environment. After entering the respiratory tract, the inhaled fire pollutants can reach the alveolar region and be absorbed by the pulmonary capillaries directly into the bloodstream, principally the ultrafine particles and the most volatile compounds [18,19,20]. Despite the use of personal protective equipment (PPE), firefighters’ occupational exposure also occurs through dermal contact and ingestion [1,21,22]. Firefighters often report that even after wearing turnout gear with the SCBA system, they continue smelling like smoke following the decontamination procedures performed after firefighting activities. This in-field observation of firefighters’ exhaled breath raised concern about how and where the respiratory exposure occurred while using the PPE and SCBA during the firefighting activity. Literature related to the air quality of the SCBA’s air and the evaluation of firefighters’ exposure to fire pollutants during structure fires while using the SCBA system is very scarce [23,24,25]. A study performed by Teixeira et al. [23] reported that PAHs’ levels inside the SCBA system during firefighting activities were significantly lower than those detected outside the respiratory protection. Nevertheless, the PAH concentrations present within the SCBA facepiece were still sufficient to induce cytotoxic effects in human alveolar and bronchial in vitro cell lines and permeate a co-culture model of air–blood barrier [23]. Replying to these scientific challenges highlighted by a group of Portuguese firefighters, this work assesses the concentrations of PAHs inside the SCBA facemask used by sapper firefighters during structure-firefighting exercises. Eighteen PAHs [16 compounds from the United States Environmental Protection Agency (USEPA) included in the priority pollutants list, benzo(j)fluoranthene, and dibenzo(a,l)pyrene] were quantified inside the SCBA used by sapper firefighters during 7 controlled-structure fires. A comprehensive respiratory health risk analysis was performed for each participant to evaluate individual occupational risks during structure firefighting based on well-established WHO and USEPA methodologies.
2. Materials and Methods
2.1. Selection of Study Participants
A total of 46 recruiters of sapper firefighters and 4 instructors from the Regiment of Sapper Firefighters (n = 320; representing 16% of active sapper firefighters) of the Municipality of Porto (North of Portugal) voluntarily participated in this observational cross-sectional study after the collection of their authorizations for free participation in the study. Each participant filled out a structured questionnaire adapted from the World Health Organization (WHO) [26], which was previously revised and validated by the Ethics Committee of the University of Porto (Report No. 105/CEUP/2020). The main inclusion criteria were to be a contracted sapper firefighter directly involved in programmed structural firefighting training activities. The participants with reported respiratory disorder were not considered in this monitorization study. An alphanumeric code was attributed to each participant to pseudo-anonymize the collected samples.
2.2. Collection of SCBA Samples
The 7 events of controlled structure fires were performed between March 2022 and February 2023. Each fire event was performed by a team of up to 5 sapper firefighters’ trainers supervised by at least 2 instructors (Figure S1a of the Supplementary Material). The firefighting exercises were performed in the training facilities situated in Baltar, Municipality of Paredes (North of Portugal), specifically in a concrete two-floor house, without interior lining and paint, and with few furniture and materials (Figure S1b). The fire was ignited by burning wooden pallets in a predefined area of the building. All the doors and windows were completely closed to create the most realistic scenario (Figure S1c). A member of the research team used clean nitrile gloves to stick a cotton disk (5.8 cm diameter; density of 71.89 mg/cm3) on the inner side of the SCBA facepiece of each firefighter, immediately before placing the SCBA system. All participants wore the SCBA from their entrance into the building until the end of the training exercise. It is estimated that the flow rate of air from SCBA is 40 L/min with a capacity for ~20–30 min, depending on the breathing rate of the subject. The cotton disk was removed by a researcher in a clean environment at the end of the firefighting exercise. The duration of structural firefighting exercises ranged from 2 to 3 h, and the firefighters used the SCBA for up to 30 consecutive minutes. After removal from the SCBA facemask, the little sticker used was completely removed from the cotton disk. All samples were stored in a zip bag, transported refrigerated to the laboratory, and preserved in a freezer (−20 °C) until chemical analysis. A set of three cotton disks were transported to and from the sampling site to evaluate cross-contamination.
2.3. Extraction and Chromatographic Analysis of PAHs
The extraction of PAHs from cotton disks was performed in an ultrasonic bath (J.P. Selecta, S.A., Barcelona, Spain) for 20 min with 20 mL of acetonitrile. The extracts were dried with a rotary evaporator (Buchi Rotavapor, R-200) at 20 °C, being the residue redissolved in 300 µL of acetonitrile, and filtered with a polytetrafluoroethylene filter (0.45 µm). The chromatographic analysis of PAHs was based on the analytical method previously reported by Castro et al. [27]. Briefly, 18 PAHs [acenaphthene, acenaphthylene, anthracene, benz(a)anthracene, benzo(a)pyrene (BaP), benzo(b+j)fluoranthene, benzo(g,h,i)perylene, benzo(k)fluoranthene, chrysene, dibenz(a,h)anthracene, dibenzo(a,l)pyrene, fluoranthene, fluorene, indeno(1,2,3-c,d)pyrene, naphthalene, phenanthrene, pyrene] were separated in a C18 column (EC 150/4 Nucleosil 100-5 C18 PAH, 150 × 4.0 mm; 5 µm particle size; Macherey-Nagel, Düren, Germany) over 40 min at a flow rate of 0.8 mL/min. The chromatographic analysis was performed in a Shimadzu LC system (Shimadzu Corporation, Kyoto, Japan) equipped with an LC-20AB pump, DGU-20A5R degasser, and photodiode array SPD-M20A and fluorescence RF-20AXS detectors online at a controlled temperature (25 ± 1 °C, CTO-20AC model, Shimadzu Corporation, Kyoto, Japan). The limits of detection (LOD) and quantification ranged between 0.07 and 37.2 µg/L and from 0.22 to 124.1 µg/L, respectively. The recoveries obtained with this methodology ranged between 62.3 ± 18.0% and 112.0 ± 1.1%. Calibration standards and blank extracts were analyzed daily and regularly. The samples were analyzed in triplicate.
2.4. Health Risk Evaluation
The respiratory health risk analysis was performed for each study participant through the determination of total BaP equivalents (BaPEq, ng/m3), the lifetime lung cancer risk (LLCR, dimensionless), the total dose rate (D, ng/kg/day), and the total carcinogenic risks (TR, dimensionless) based on USEPA and WHO methodologies, as applied in previous studies [28,29,30]. The BaPEq [Equation (1)] was determined based on available toxic equivalent factors (TEFs) settled by USEPA to different PAHs relatively to the carcinogenic BaP [1.0 × 10−4 for naphthalene, acenaphthylene, acenaphthene, fluorene, phenanthrene, fluoranthene, and pyrene; 1.0 × 10−2 for anthracene, chrysene, benzo(k)fluoranthene, and benzo(g,h,i)perylene; 0.1 for benz(a)anthracene, benzo(b+j)fluoranthene, and indeno(1,2,3-c,d)pyrene; 1 for BaP and dibenzo(a,h)anthracene; 100 for dibenzo(a,l)pyrene] and its respective concentration (ng/m3) quantified inside the firefighter’ facemask [31].
The LLCR (dimensionless) was calculated, based on Equation (2), using the BaP unit risk value (8.7 × 10−5 per 1 ng/m3) [32] and considering an exposure time (ET) of 8 h per day during an average lifetime of 70 years, according to the WHO methodology [32,33].
The D (ng/kg/day) was estimated based on the levels of each PAH found inside the respiratory facemask and according to Equation (3) [34].
BrWA is the age-specific weighted average breathing rate accounting for the age and intensity levels of the activities performed by firefighters (2.7 × 10−2 m3/min due to moderate physical intensity during firefighting activities) [35]; BW is the age-specific body weight (kg) of each participant; C is the concentration (ng/m3) of PAH inside the facemask; OF is the occupancy factor, which refers to the occupation at the exposure local (considered 1 since firefighters are on exposure local all the sampled period); N is the total exposure time per day estimated for the study population (25 min/day).
The TR (dimensionless) was determined based on the USEPA pre-established chronic inhalation unit risks [3.4 × 10−5 μg/m3 for naphthalene; 1.1 × 10−5 μg/m3 for chrysene; 1.1 × 10−4 μg/m3 for benz(a)anthracene, benzo(b)fluoranthene, benzo(k)fluoranthene, and indeno(1,2,3-c,d)pyrene; 1.1 × 10−3 μg/m3 for BaP] [36]. The expression used is presented in Equation (4):
where EFR represents the exposure frequency (250 days of exposure per year); ED is the exposure duration—the career time of each sapper firefighter (years); ET is the exposure time of each participant (25 min/day, i.e., 0.42 h/day); C is the concentration of PAH monitored inside the SCBA facemask (ng/m3); AT is the number of days over which the exposure might occur (14,600 days, i.e., 40 years of career × 365 days/year [37]).
2.5. Data Analysis
Data analysis was carried out with Microsoft Office Excel (v. 16.0 Microsoft Corporation, Washington, DC, USA) and SPSS statistical software (IBM SPSS Statistics 20, v. 28.0, Armonk, NY, USA). When applicable, samples were adjusted for blank concentrations. Whenever the concentrations of a compound was below the LOD, the value was replaced by LOD/√2 [38]. The results are presented as median and/or range since normal distribution was not demonstrated by a Shapiro–Wilk’s test. Spearman correlation coefficients were determined to explore the (co)relation between PAHs’ levels inside the SCBA facemask and all the determined health risk parameters. Statistical analysis was carried out, and whenever significant differences were observed between the groups compared, a p value ≤ 0.05 or 0.01 for a confidence level of 95% and 99% is presented, respectively.
3. Results
3.1. Exposure Assessment Through SCBA
A total of 50 male sapper firefighters with a median age of 25.0 years old and a median body mass index (BMI) of 24.4 kg/m2 were enrolled in the study (Table 1). About 34% of firefighters presented BMI values that suggest overweight (>25 kg/m2) [39,40]. However, increased muscle mass due to the physical preparation of a firefighter may contribute to increased BMI, not necessarily representing increased body fat [39]. Four sapper firefighter instructors reported a career time ranging from 17.8 to 22.8 years, although 92% of study participants were sapper recruiters with a career time duration between 1.0 and 8.1 years. The recruiters with a career time higher than 1 year (13%), previously worked as volunteer firefighters in local fire stations.

Table 1.
Characterization of firefighters enrolled in the study.
The median total PAH (∑PAHs) levels extracted from the cotton disks was 11.2 ng/m3, ranging from 9.17 to 29.6 ng/m3 (Figure 1a). Overall, the concentrations of ∑PAHs were increased in fire event 5 (15.0 ng/m3), followed by events 4 (14.1 ng/m3), 6 and 7 (10.7 and 10.5 ng/m3, respectively), 1 and 2 (10.4 ng/m3), and event 3 (9.82 ng/m3); significant differences were observed between samples from event 2 with events 4 and 5 (p < 0.001); fire 3 with events 4, 5, 6, and 7 (p ≤ 0.007); event 6 with fire event 4 and 5 (p = 0.013 and p = 0.002, respectively); and in fire event 7 with samples from exercise 5 (p = 0.009). Acenaphthene, acenaphthylene, dibenz(a,h)anthracene, dibenzo(a,l)pyrene, and indeno(1,2,3-c,d)pyrene were not detected in all collected samples. Regarding exposure to carcinogenic PAHs [BaP—known carcinogen (Group 1), and naphthalene, anthracene, benz(a)anthracene, benzo(b+j)fluoranthene, benzo(k)fluoranthene, and chrysene—possible carcinogens (Group 2B) [41,42], total concentrations (∑PAHscarcinogenic) varied between 0.41 and 5.73 ng/m3 (median of 1.09 ng/m3; p < 0.001), representing 6.30 to 16.0% of ∑PAHs (Figure 1b). Significant differences were found between extracts from exercise 5 and all the other fire exercises (p ≤ 0.003, except for exercise 4), exercise 4 and exercises 2, 3, and 6 (p ≤ 0.013), and between exercises 3 and 6 (p = 0.007). A similar distribution was found for ∑PAHscarcinogenic [fire event 5 (2.97 ng/m3) > event 4 (2.21 ng/m3) > events 6 and 7 (1.53 and 0.96 ng/m3, respectively) > fire event 2 (0.79 ng/m3) > events 3 and 1 (0.72 ng/m3). The individual levels of the quantified PAHs in the cotton disks of sappers’ facemasks participating in each fire event are presented in Table 2.
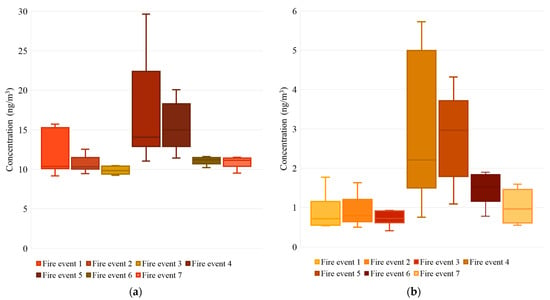
Figure 1.
Concentrations (median, P25-P75, and range; N = 3; ng/m3) of (a) total PAHs and (b) total carcinogenic PAHs detected inside the SCBA facemasks.

Table 2.
Levels of PAHs (median, range; ng/m3) detected inside the sappers’ facemask during structure firefighting exercises.
Naphthalene, phenanthrene, pyrene, and fluoranthene were the predominant compounds inside the SCBA’ facemask during firefighting exercises, representing 18.2–39.2% of ∑PAHs in all firefighting exercises (Table 2) (p ≤ 0.001). It is important to emphasize that (possible/probable) carcinogenic PAHs, naphthalene, anthracene, chrysene, benzo(b+j)fluoranthene, and BaP were detected inside the SCBA’ facemasks during firefighting training exercises (Table 2). Overall, the low-molecular weight (LMW) PAHs (2–3 rings) were the more prevalent compounds (79.5–91.4% of ∑PAHs), followed by those with 4 (5.0–16.0% of ∑PAHs) and with 5 or more benzenic rings (1.90–4.70% of ∑PAHs) (Figure 2).
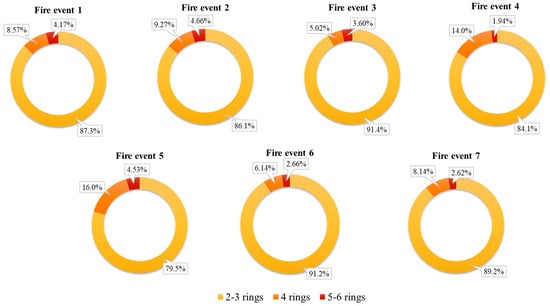
Figure 2.
Distribution of PAHs according to the number of aromatic rings in each fire event.
3.2. Respiratory Health Risk Assessment
The median ∑BaPEq determined with the levels of PAHs found inside each firefighter’ facemask varied between 0.064 and 0.22 ng/m3 with maximum values reaching 0.43 ng/m3 in fire event 5; significant differences were found between the samples collected in fire event 5 with all the other fire exercises, except event 1 (p ≤ 0.050), fire exercises 3 and 5 (p < 0.001); fire event 3 with events 1 and 4 (p = 0.050), and between events 2 and 6 (p = 0.030 and p = 0.025, respectively) (Figure 3a). The compounds that contribute most for the BaPEq values were BaP (64.5–79.5%), benzo(b+j)fluoranthene (14.6–31.1%), and benz(a)anthracene (1.44–5.74%). Median BaPEq values determined for fluorene and phenanthrene varied between 7.14 × 10−6–4.10 × 10−5 ng/m3 and from 4.56 × 10−5–1.82 × 10−4 ng/m3, respectively. The estimated firefighters’ LLCR related to personal exposure to PAHs, via the inhaled air inside the SCBA respiratory facemask, varied between 6.54 × 10−10 to 2.24 × 10−9, a negligible value when compared to the WHO recommended health-based guideline of 10−5 [32].
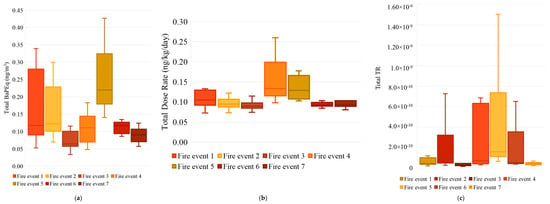
Figure 3.
Levels (median, P25–P75, and range) of estimated health risk parameters: (a) total BaPEq (ng/m3), (b) total dose rate (ng/kg/day), and (c) total TR (dimensionless) for the sapper firefighters enrolled in the 7 firefighting-training exercises.
The median D determined for each sapper firefighter enrolled in training structure fire events ranged from 8.91 × 10−2 to 0.13 ng/kg/day, with maximum values reaching 0.26 ng/kg/day in fire event 4; some significant differences were registered [events 3 and 4 (p < 0.001); exercises 2, 6, and 7 with event 4 (p ≤ 0.003); fire events 2, 3, 6, and 7 with event 5 (p ≤ 0.004); fire events 3 and 6 with event 1 (p ≤ 0.050)] (Figure 3b). The major PAHs’ contributors to D were phenanthrene (4.28 × 10−3–1.79 × 10−2 ng/kg/day), naphthalene (2.23 × 10−3–1.79 × 10−2 ng/kg/day), fluoranthene (2.12 × 10−3–7.32 × 10−3 ng/kg/day), and pyrene (1.34 × 10−3–1.03 × 10−2 ng/kg/day). Median D values for fluorene and benzo(b+j)fluoranthene varied between 6.88 × 10−4–3.69 × 10−3 ng/kg/day and from 1.61 × 10−3–3.41 × 10−3 ng/kg/day, respectively.
The total estimated TR associated with the air monitored inside the SCBA’ facemask are represented in Figure 3c. The calculated median ∑TR levels varied between 3.17 × 10−11 and 1.59 × 10−10, with a maximum of 1.50 × 10−9 during fire event 5. Significant differences were found between event 3 and exercises 2, 4, 5, and 6 (p ≤ 0.050); fire event 7 with events 2, 4, 5, and 6 (p ≤ 0.037); exercises 1 and 5 (p = 0.007); and fire event 6 with exercises 4 and 5 (p = 0.037) (Figure 3c). The major contributors to ∑TR were BaP (47.8–71.7%), naphthalene (5.27–53.2%), and benzo(b+j)fluoranthene (13.0–20.7). The median TR levels of benz(a)anthracene and benzo(k)fluoranthene ranged from 4.56 × 10−13–6.71 × 10−12 and 4.73 × 10−13–4.48 × 10−12, accounting for up to 4.72 and 4.30% of ∑TR risks, respectively. ∑TR values were well below the USEPA acceptable risk level of 10−4 and 10−6 [43]. The performed risk analysis is an additional indicator of the effectiveness of SCBA’ system in protecting the respiratory health of firefighters.
Putting all the respiratory health risk parameters together, strong positive correlations were found between ∑BaPEq and LLCR (r = 1), and ∑D with ∑PAHs and ∑PAHscarcinogenic (r = 0.855 and r = 0.648, respectively) (Figure 4). Also, the concentrations of ∑PAHs were positively correlated with the levels of ∑PAHscarcinogenic (r = 0.821) (Figure 4). Moderate positive correlations were also observed between ∑TR and ∑PAHs (r = 0.647) and ∑PAHscarcinogenic (r = 0.624) with ∑D (r = 0.527) (Figure 4).
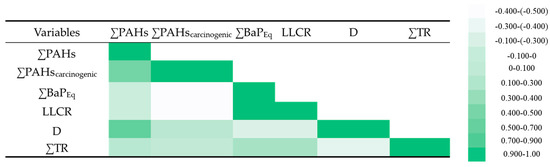
Figure 4.
Spearman correlations determined between the levels of ∑PAHs (ng/m3), ∑PAHcarcinogenic (ng/m3) monitored inside the SCBA facemask during structure-firefighting-training exercises and the estimated respiratory health risk parameters [∑BaPEq (ng/m3), LLCR, total D (ng/k/day), and ∑TR].
3.3. Principal Component Analysis
A principal component analysis (PCA) was carried out with the levels of quantified PAHs and all the parameters assessed during the health risk analysis to evaluate their (co)relationship. The obtained biplot is presented in Figure 5. The two main components were extracted with two functions (F1 and F2 with eigenvalues of 4.25 and 0.96, respectively). A Kaiser–Meyer–Olkin sampling adequacy of 0.707 was obtained, representing 86.7% of sample variability. F1 accounted for 70.8% of the total variance, and it was strongly influenced by the concentrations of ∑PAHs, ∑PAHscarcinogenic, and ∑D, with square cosine values varying between 0.621 and 0.805. F2 contributed 15.9% of the data, and it was more affected by the total BaPEq and the lung cancer risk with a square cosine value of 0.245 for both variables. This PCA model allowed the separation of 50% of collected samples, based on the air content in PAHs and associated respiratory health risks, allowing for the identification of sapper firefighters at increased respiratory health risk (Figure 5).

Figure 5.
Model of principal component analysis (PCA) performed with original data on the respiratory health risk analysis (total PAHs, total carcinogenic PAHs, dose, BaPEq, carcinogenic risks, and lung cancer) determined for sapper firefighters enrolled in controlled-structure fires and using the SCBA system.
4. Discussion
A previous study performed by Teixeira et al. [23] simultaneously assessed the PAHs’ levels inside and outside the SCBA facemask of sapper firefighters during three firefighting exercises. The study reported levels of ∑PAHs 90 to 20437 times lower inside than outside the SCBA (1.96–10.4 ng/m3 versus 11.5–28.0 μg/m3), with estimated indoor-to-outdoor ratios lower than unity, revealing the contribution of outside PAHs (Table 3). In the present study, the concentrations of ∑PAHs (9.17–29.6 ng/m3) monitored inside facemasks were well below the levels reported outside the SCBA during previously monitored training firefighting activities [23]. Also, the concentrations of ∑PAHs and ∑PAHscarcinogenic (0.41–5.73 ng/m3) inside the SCBA facemask were slightly higher than the preliminary results of the team (1.96–10.4 and 0.77–0.93 ng/m3, respectively) [23]. The observed variability of results can be attributed to varied factors that affect firefighters’ exposure through the air monitored inside the SCBA facemask, namely individual breathing rate, the composition of SCBA–supplied air and the firefighter’s exhaled air, and the fit of the facemask to the firefighter’s face. Also, the lack of standard protocols of cleaning/maintenance of SCBA might also contribute to the variability observed in the PAH levels monitored inside the facemask.

Table 3.
Concentrations of PAHs (median, range) monitored outside (µg/m3) and inside (ng/m3) SCBA facemask and inside-to-outside (I/O) ratios retrieved from Teixeira et al. [23].
Different authors have already demonstrated the increased levels of fire-related pollutants, including PAHs, in the personal air of firefighters outside the respiratory facemask during structure fires [9,10,11,12,13,14,15]. Some of those studies reported concentrations exceeding the settled occupational guidelines proposed by NIOSH (100 µg/m3) [16] and OSHA (200 µg/m3) [17]. The PAHs’ levels determined inside the sappers’ facemasks demonstrated the efficiency of the SCBA system in protecting firefighters from fire contaminants, with detected values significantly lower than available occupational limits (NIOSH/OSHA) as well as the values reported in the literature for airborne PAHs during structure fires (3.6 µg/m3–23.8 mg/m3) [17]. The correct use of the SCBA system in its optimum operational conditions, including its tightness to firefighters’ faces to minimize the infiltration of fire pollutants, effectively protects these workers from exposure to airborne fire-related pollutants, including PAHs, among other toxic compounds released during structure fires [44,45]. Additionally, some authors highlighted the importance of implementing decontamination procedures immediately after a firefighting activity and before firefighters arrive at the fire station to reduce their occupational exposure (inhalation, dermal contact) and cross-contamination at the fire station [46,47,48,49,50]. However, at some fire stations, it is common practice to store both wildland and structural firefighting PPE in a common room or inside the firefighter’s storage locker, where other clean clothes and personal objects are stored. Recently, Kim and Ham [24] compared the levels of carbon monoxide (CO) and dioxide (CO2), water, and oil mist in the SCBA’s air with the respective air concentrations inside the room where the SCBA system was charged. The SCBA cylinders were filled in different environments, namely in a clean room inside the fire station without interference from harmful substances (control group) and inside a contaminated environment, namely the heavy vehicles garage (case group). The reported concentrations of CO (5.0–8.7 ppm versus 0 ppm in the case and control groups, respectively:), oil mist (0–0.17 versus 0–0.4 mg/m3), CO2 (533.3–783.3 versus 500.0–583.3 ppm), and water vapor (30.0–41.7 versus 30.0–60.0 mg/m3) inside the SCBA were predominantly superior to the air levels found inside the charging room [24]. Those authors concluded that the hygiene and safety of the procedure of SCBA charging can be affected by the contaminants present in the air of the room where the refill occurred [24]. An alternative for the use of SCBA, during overhaul, was developed by Staack and co-authors [51] based on an air-purifying respirator with chemical, biological, radiological, and nuclear canisters. This respiratory device was tested in two types of simulated overhaul environments, more specifically in a “standard” and “high-exposure” scenarios [51]. Those authors concluded that the respirator allowed for the maintenance of contaminant levels below the occupational exposure limits, and it could be used if the SCBA was not a feasible option [51]. Despite these findings, it was reported that in a high-exposure scenario with increased air temperature and relative humidity, some volatile organic compounds were found inside the respiratory mask, making it not recommended the use of this device in these conditions [51]. Moreover, Staack et al. [51] reinforced the use of SCBA as preferred respiratory protection during the entire fire event, including the overhaul phase [51]. In this context, firefighters must recognize the critical importance of properly cleaning and maintaining PPE, including SCBA equipment, and firefighting materials and tools, also ensuring their appropriate storage, contributing to preventing cross-contamination, and ensuring the safety and adequate functionality of all equipment.
Firefighting activities, principally in structure fires, encompass moderate to intense physical exercise performed in a very smoky and hot environment, which promotes higher breathing rates and consequently exposes firefighters to increased inhalation rates of fire pollutants, including PAHs. Overall, the health risk analysis performed in this study, LLCR, dose rate, and carcinogenic risks associated with firefighters’ exposure to structure fires with the use of SCBA, demonstrated the existence of negligible risks since they were within or below the guidelines recommended by WHO and USEPA [32,43]. The dose rate of each firefighter depends on the body weight of each individual and their physical preparedness for the firefighting activity. Therefore, firefighters with higher fat mass index are expected to present increased dose rates, which may have implications for potential respiratory health risks. However, this parameter was not evaluated in this study, and these authors cannot infer the contribution of this parameter to the health risk analysis. Additional studies, including firefighters’ health risk assessment, are needed to corroborate these results achieved in this work.
The developed PCA model demonstrated the relationship between exposure to PAHs and the associated respiratory health risks. This study demonstrates the negligible impacts of the PAHs detected inside the SCBA, demonstrating the effectiveness of respiratory protection. However, when the SCBA’ facemask does not fit properly in the face of firefighter, it may represent a primary route of exposure, via inhalation, to fire effluents. Several authors in the literature pointed out that in some situations, principally during the fire overhaul and investigation, some firefighters tend to experience thermal and physical discomfort and associated fatigue by removing the SCBA system, which may also contribute to increasing their exposure to fire effluents [45,50,52]. Also, maintenance and cleaning failures of the SCBA system, including the facemask, and/or its inadequate storage inside the fire station, may contribute to a secondary source of exposure to fire-related pollutants [53,54]. Moreover, a cross-contamination of cleaned PPE and SCBA devices can occur through direct contact with fire-pollutants accumulated in firefighting tools and vehicles, which are transported from the fire scene to the indoor areas of the fire station [53,54]. The PCA model developed based on respiratory health risk analysis is useful to identify subjects at increased risk of respiratory burden, principally in real and/or high-exposure scenarios and/or when the operational capability and proper maintenance of the SCBA system are suspected. To overcome these operational difficulties, firefighting forces are committed and engaged in the reduction in fire effluents cross-contamination by implementing PPE, including SCBA systems, firefighting materials, and vehicles decontamination at the fire scene or at their first arrival at the fire station [55,56,57,58,59,60]. Nevertheless, it was demonstrated that the SCBA system must be used in all phases of a structure fire, including during overhaul and fire investigation, as well as during training exercises, to reduce the respiratory health burden. Also, regular maintenance needs to be ensured, and the cleaning, storage, and loading of the SCBA system need to be performed in a clean and well-ventilated area, away from sources of pollution, including fire-contaminated devices and diesel exhaust, among other garage emissions.
This work was performed in a real training scenario frequently used by several firefighting forces situated in the Porto Metropolitan area to perform firefighting and rescue exercises. This work describes an observational study representing the firefighting training exercises regularly performed in Portugal. However, the nature of the study makes it difficult to replicate due to the unique characteristics of each firefighting exercise, local meteorological conditions, and the SCBA systems used. Additional limitations of this study are related to the exposure assessment by passive air sampling inside the SCBA facemask during the firefighting exercises, since this was the only sampling method authorized by fire chiefs and instructors to secure the safety of sapper firefighters during the monitored training exercises. This study has a limited sample size and a relatively small dataset, which may not represent large groups of firefighters. The SCBAs’ equipment monitored was randomly selected by fire chiefs and instructors, representing the firefighting protective devices available in the monitored firefighting force. Additionally, only one class of organic compounds released during fires, 18 PAHs, was assessed. However, other fire-related pollutants (e.g., heavy metals, carbon monoxide, etc.) might also be present inside the SCBA facemask, and their synergistic/antagonist effects on respiratory risks remain unknown. Additional studies monitoring real structure firefighting activities are needed to corroborate and explore the findings of this work.
5. Conclusions
The present work demonstrates the presence of PAHs inside the SCBA’s facemask used by sapper firefighters during structure-firefighting exercises at levels ranging between 9.17 and 29.6 ng/m3 and from 0.41 and 5.73 ng/m3 for ∑PAHs and ∑PAHscarcinogenic, respectively. The determined levels were well below available occupational limits recommended by OSHA and NIOSH (200 and 100 µg/m3, respectively). The LMW PAHs were the most predominant compounds (79.5–91.4% of ∑PAHs), while high-molecular-weight compounds represented 1.90–4.70% of ∑PAHs. An individual occupational respiratory risk analysis was performed, and ∑BaPEq concentrations (0.064 and 0.22 ng/m3) were used to estimate sapper firefighters’ LLCRs (6.54 × 10−10 to 2.24 × 10−9), which were well below the health-based guideline level (10−5) proposed by the WHO. The values of ∑D ranged from 8.91 × 10−2 to 0.13 ng/kg/day, and ∑TR values (3.17 × 10−11 to 1.59 × 10−10) were well below the USEPA acceptable risk level (10−4 to 10−6). Therefore, the results obtained in this study demonstrate the effectiveness of the use of SCBA in reducing firefighters’ exposure to PAHs released during structure fires.
As an important part of fire risk assessment and management, educational and training programs have been implemented to increase the awareness of exposure to fire effluents and associated health risks, thus improving the management of PPEs and overall safety practices. The SCBA system must be used in all phases of a structure fire, including during overhaul and fire investigation, since during these phases, the exposure to hazardous fire pollutants can occur. Also, the regular maintenance of SCBA systems needs to be ensured, as well as the adequate cleaning, storage, and loading of the respiratory system, preferably performed in a clean and well-ventilated area, away from sources of pollution, including fire-contaminated devices and diesel exhaust (e.g., fire stations’ garages).
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/fire8050182/s1, Figure S1: Representation of (a) one group of sapper firefighters using the complete PPE, including the SCBA face mask with the cotton disk on the inner side of the device, (b) a room with furniture inside the concrete house where the fire was initiated, and (c) a firefighting training exercise.
Author Contributions
J.T.: methodology, writing—original draft preparation; C.D.-M.: funding acquisition; A.S.-S.: supervision; F.R.: writing—review and editing, funding acquisition, supervision, project administration; M.O.: conceptualization, writing—review and editing, funding acquisition, supervision, project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the Fundação para a Ciência e a Tecnologia, Ministério da Ciência, Tecnologia e Ensino Superior (FCT-MCTES) through the 4FirHealth project (http://doi.org/10.54499/PCIF/SSO/0090/2019 (accessed on 1 April 2025)).
Institutional Review Board Statement
The study received the Ethic approval from The Ethic Committee of University of Porto (Report Nr. 105/CEUP/2020).
Informed Consent Statement
Signed informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets generated during the current study will be made available upon request to the corresponding author on reasonable request.
Acknowledgments
This work received additional support through UIDB/50006/2020, UIDP/50006/2020, LA/P/0008/2020, and 2022.05381.PTDC by FCT-MCTES. M. Oliveira and F. Rodrigues are thankful for the scientific contracts CEECIND/03666/2017 and 2023.06819.CEECIND financed by FCT-MCTES. The authors thank the cooperation and support of all firefighters and the agents of Autoridade Nacional de Emergência e Proteção Civil.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- International Agency for Research on Cancer (IARC). Occupational exposure as a firefighter. In IARC Monographs on the Identification of Carcinogenic Hazards to Humans; IARC: Lyon, France, 2023. [Google Scholar]
- Cuenca-Lozano, M.; Ramírez-García, C. Occupational hazards in firefighting: Systematic literature review. Saf. Health Work. 2023, 14, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Tian, X.; Cheng, Y.; Chen, S.; Liu, S.; Wang, Y.; Niu, X.; Sun, J. The emission characteristics and health risks of firefighter-accessed fire: A review. Toxics 2024, 12, 739. [Google Scholar] [CrossRef] [PubMed]
- Barros, B.; Oliveira, M.; Morais, S. Biomonitoring of firefighting forces: A review on biomarkers of exposure to health-relevant pollutants released from fires. J. Toxicol. Environ. Health B 2023, 26, 127–171. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Chen, Y.; Feng, Y.; Song, W.; Cao, F.; Zhang, Y.; Li, Q.; Yang, X.; Chen, J. Different formation mechanisms of PAH during wood and coal combustion under different temperatures. Atmos. Environ. 2020, 222, 117084. [Google Scholar] [CrossRef]
- Li, T.; Chen, H.; Fung, J.C.H.; Chan, D.H.L.; Yu, A.L.C.; Leung, K.K.M.; Yu, J.Z. Large presence of bromine and toxic metals in ambient fine particles from urban fires. Atmos. Environ. 2023, 295, 119554. [Google Scholar] [CrossRef]
- Mazumder, N.-U.-S.; Hossain, M.T.; Jahura, F.T.; Girase, A.; Hall, A.S.; Lu, J.; Ormond, R.B. Firefighters’ exposure to per-and polyfluoroalkyl substances (PFAS) as an occupational hazard: A review. Front. Mater. 2023, 10, 1143411. [Google Scholar] [CrossRef]
- Hwang, J.; Xu, C.; Agnew, R.J.; Clifton, S.; Malone, T.R. Health risks of structural firefighters from exposure to polycyclic aromatic hydrocarbons: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 4209. [Google Scholar] [CrossRef]
- Feunekes, F.D.J.R.; Jongeneelen, F.J.; Laana, H.v.d.; Schoonhof, F.H.G. Uptake of Polycyclic Aromatic Hydrocarbons Among Trainers in a Fire-Fighting Training Facility. Am. Ind. Hyg. Assoc. J. 1997, 58, 23–28. [Google Scholar] [CrossRef]
- Fernando, S.; Shaw, L.; Shaw, D.S.; Gallea, M.; vanden Enden, L.; House, R.; Verma, D.K.; Britz McKibbin, P.; McCarry, B.E. Evaluation of Firefighter Exposure to Wood Smoke during Training Exercises at Burn Houses. Environ. Sci. Technol. 2016, 50, 1536–1543. [Google Scholar] [CrossRef]
- Fent, K.W.; Evans, D.E.; Babik, K.; Striley, C.; Bertke, S.; Kerber, S.; Smith, D.; Horn, G.P. Airborne contaminants during controlled residential fires. J. Occup. Environ. Hyg. 2018, 15, 399–412. [Google Scholar] [CrossRef]
- Fent, K.W.; Toennis, C.; Sammons, D.; Robertson, S.; Bertke, S.; Calafat, A.M.; Pleil, J.D.; Wallace, M.A.G.; Kerber, S.; Smith, D.; et al. Firefighters’ absorption of PAHs and VOCs during controlled residential fires by job assignment and fire attack tactic. J. Expo. Sci. Environ. Epid. 2020, 30, 338–349. [Google Scholar] [CrossRef]
- Sjöström, M.; Julander, A.; Strandberg, B.; Lewné, M.; Bigert, C. Airborne and dermal exposure to polycyclic aromatic hydrocarbons, volatile organic compounds, and particles among firefighters and police investigators. Ann. Work Expo. Health 2019, 63, 533–545. [Google Scholar] [CrossRef] [PubMed]
- Keir, J.; Akhtar, U.; Matschke, D.; White, P.; Kirkham, T.; Chan, L.; Blais, J. Polycyclic aromatic hydrocarbon (PAH) and metal contamination of air and surfaces exposed to combustion emissions during emergency fire suppression: Implications for firefighters’ exposures. Sci. Total Environ. 2020, 698, 134211. [Google Scholar] [CrossRef] [PubMed]
- Poutasse, C.M.; Poston, W.S.C.; Jahnke, S.A.; Haddock, C.K.; Tidwell, L.G.; Hoffman, P.D.; Anderson, K.A. Discovery of firefighter chemical exposures using military-style silicone dog tags. Environ. Int. 2020, 142, 105818. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Occupational Safety and Health (NIOSH). Naphthalene. 2019. Available online: https://www.cdc.gov/niosh/npg/npgd0439.html (accessed on 15 December 2024).
- Occupational Safety and Health Administration (OSHA). Permissible Exposure Limits. 2017. Available online: https://www.osha.gov/annotated-pels (accessed on 15 December 2024).
- Han, B.; Liu, Q.; Su, X.; Zhou, L.; Zhang, B.; Kang, H.; Ning, J.; Li, C.; Zhao, B.; Niu, Y.; et al. The role of PP2A/NLRP3 signaling pathway in ambient particulate matter 2.5 induced lung injury. Chemosphere 2022, 307, 135794. [Google Scholar] [CrossRef]
- Santibáñez-Andrade, M.; Sánchez-Pérez, Y.; Chirino, Y.I.; Morales-Bárcenas, R.; Quintana-Belmares, R.; García-Cuellar, C.M. Particulate matter (PM10) destabilizes mitotic spindle through downregulation of SETD2 in A549 lung cancer cells. Chemosphere 2022, 295, 133900. [Google Scholar] [CrossRef]
- Barbosa, J.V.; Farraia, M.; Branco, P.; Alvim-Ferraz, M.C.M.; Martins, F.G.; Annesi-Maesano, I.; Sousa, S.I.V. The Effect of Fire Smoke Exposure on Firefighters’ Lung Function: A Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 16799. [Google Scholar] [CrossRef]
- Sousa, G.; Delerue-Matos, C.; Wang, X.; Rodrigues, F.; Oliveira, M. Potential of Saliva for Biomonitoring of Occupational Exposure: Collection of Evidence from the Literature. In Occupational and Environmental Safety and Health IV; Arezes, P.M., Baptista, J.S., Melo, R.B., Castelo Branco, J., Carneiro, P., Colim, A., Costa, N., Costa, S., Duarte, J., Guedes, J.C., et al., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 587–598. [Google Scholar]
- Sousa, G.; Teixeira, J.; Delerue-Matos, C.; Sarmento, B.; Morais, S.; Wang, X.; Rodrigues, F.; Oliveira, M. Exposure to PAHs during Firefighting Activities: A Review on Skin Levels, In Vitro/In Vivo Bioavailability, and Health Risks. Int. J. Environ. Res. Public Health 2022, 19, 12677. [Google Scholar] [CrossRef]
- Teixeira, J.; Bessa, M.J.; Delerue-Matos, C.; Sarmento, B.; Santos-Silva, A.; Rodrigues, F.; Oliveira, M. Human exposure to polycyclic aromatic hydrocarbons during structure fires: Concentrations outside and inside self-contained breathing apparatus and in vitro respiratory toxicity. Environ. Pollut. 2025, 373, 126112. [Google Scholar] [CrossRef]
- Kim, S.J.; Ham, S. Evaluation of Air Quality inside Self-Contained Breathing Apparatus Used by Firefighters. Fire 2023, 6, 347. [Google Scholar] [CrossRef]
- Jones, L.; Lutz, E.A.; Duncan, M.; Burgess, J.L. Respiratory protection for firefighters—Evaluation of CBRN canisters for use during overhaul. J. Occup. Environ. Hyg. 2015, 12, 314–322. [Google Scholar] [CrossRef]
- World Health Organization (WHO). World Health Survey B—Individual Questionnaire. Evidence and Information Policy; WHO: Geneva, Switzerland, 2002. [Google Scholar]
- Castro, D.; Slezakova, K.; Oliva-Teles, M.T.; Delerue-Matos, C.; Alvim-Ferraz, M.C.; Morais, S.; Carmo Pereira, M. Analysis of polycyclic aromatic hydrocarbons in atmospheric particulate samples by microwave-assisted extraction and liquid chromatography. J. Sep. Sci. 2009, 32, 501–510. [Google Scholar] [CrossRef]
- Teixeira, J.; Sousa, G.; Azevedo, R.; Almeida, A.; Delerue-Matos, C.; Wang, X.; Santos-Silva, A.; Rodrigues, F.; Oliveira, M. Characterization of Wildland Firefighters’ Exposure to Coarse, Fine, and Ultrafine Particles; Polycyclic Aromatic Hydrocarbons; and Metal(loid)s, and Estimation of Associated Health Risks. Toxics 2024, 12, 422. [Google Scholar] [CrossRef]
- Teixeira, J.; Bessa, M.J.; Delerue-Matos, C.; Sarmento, B.; Santos-Silva, A.; Rodrigues, F.; Oliveira, M. Firefighters’ personal exposure to gaseous PAHs during controlled forest fires: A case study with estimation of respiratory health risks and in vitro toxicity. Sci. Total Environ. 2024, 908, 168364. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.; Slezakova, K.; Fernandes, A.; Teixeira, J.P.; Delerue-Matos, C.; Pereira, M.C.; Morais, S. Occupational exposure of firefighters to polycyclic aromatic hydrocarbons in non-fire work environments. Sci. Total Environ. 2017, 592, 277–287. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Human Biomonitoring: Facts and Figures; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2015. [Google Scholar]
- World Health Organization (WHO). Air Quality Guidelines for Europe; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2000. [Google Scholar]
- World Health Organization (WHO). Air Quality Guidelines for Europe; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 1987. [Google Scholar]
- Kalaiarasan, M.; Balasubramanian, R.; Cheong, K.W.D.; Tham, K.W. Traffic-generated airborne particles in naturally ventilated multi-storey residential buildings of Singapore: Vertical distribution and potential health risks. Build. Environ. 2009, 44, 1493–1500. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency (USEPA). Exposure Factors Handbook. Washington, DC. 2011. Available online: https://www.epa.gov/expobox/about-exposure-factors-handbook (accessed on 15 December 2024).
- United States Environmental Protection Agency (USEPA). Regional Screening Level (RSL) Summary Table (TR = 1E-06, HQ = 1); USEPA: Washington, DC, USA, 2023.
- United States Environmental Protection Agency. Mid-Atlantic Risk Assessment. Washington, DC. 2016. Available online: https://archive.epa.gov/region9/superfund/web/html/index-23.html (accessed on 15 December 2024).
- Hornung, R.W.; Reed, L.D. Estimation of Average Concentration in the Presence of Nondetectable Values. Appl.Occup. Environ. Hyg. 1990, 5, 46–51. [Google Scholar] [CrossRef]
- WHO. World Health Organization. Body Mass Index. 2006. Available online: https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/body-mass-index (accessed on 15 December 2024).
- CDC. Centers for Disease Control and Prevention. Assessing Your Weight. 2022. Available online: https://www.cdc.gov/healthyweight/assessing/index.html (accessed on 15 December 2024).
- International Agency for Research on Cancer (IARC). List of Classifications: Agents Classified by the IARC Monographs. In IARC Monographs on the Identification of Carcinogenic Hazards to Humans; IARC: Lyon, France, 2023; Volumes 1–134. [Google Scholar]
- Cattley, R.C.; Kromhout, H.; Sun, M.; Tokar, E.J.; Abdallah, M.A.E.; Bauer, A.K.; Broadwater, K.R.; Campo, L.; Corsini, E.; Houck, K.A.; et al. Carcinogenicity of anthracene, 2-bromopropane, butyl methacrylate, and dimethyl hydrogen phosphite. Lancet Oncol. 2023, 24, 431–432. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency (USEPA). Guidelines for Carcinogen Risk Assessment; EPA/630/P-03/001F; USEPA: Washington, DC, USA, 2005.
- Pleil, J.D.; Stiegel, M.A.; Fent, K.W. Exploratory breath analyses for assessing toxic dermal exposures of firefighters during suppression of structural burns. J. Breath Res. 2014, 8, 037107. [Google Scholar] [CrossRef]
- Gainey, S.J.; Horn, G.P.; Towers, A.E.; Oelschlager, M.L.; Tir, V.L.; Drnevich, J.; Fent, K.W.; Kerber, S.; Smith, D.L.; Freund, G.G. Exposure to a firefighting overhaul environment without respiratory protection increases immune dysregulation and lung disease risk. PLoS ONE 2018, 13, e0201830. [Google Scholar] [CrossRef]
- Fent, K.W.; Alexander, B.M.; Roberts, J.; Robertson, S.; Toennis, C.A.; Sammons, D.L.; Bertke, S.J.; Kerber, S.; Smith, D.L.; Horn, G.P. Contamination of firefighter personal protective equipment and skin and the effectiveness of decontamination procedures. J. Occup. Environ. Hyg. 2017, 14, 801–814. [Google Scholar] [CrossRef] [PubMed]
- Burgess, J.L.; Hoppe-Jones, C.; Griffin, S.C.; Zhou, J.J.; Gulotta, J.J.; Wallentine, D.D.; Moore, P.K.; Valliere, E.A.; Weller, S.R.; Beitel, S.C.; et al. Evaluation of Interventions to Reduce Firefighter Exposures. J. Occup. Environ. Med. 2020, 62, 279–288. [Google Scholar] [CrossRef]
- Kesler, R.M.; Mayer, A.; Fent, K.W.; Chen, I.C.; Deaton, A.S.; Ormond, R.B.; Smith, D.L.; Wilkinson, A.; Kerber, S.; Horn, G.P. Effects of firefighting hood design, laundering and doffing on smoke protection, heat stress and wearability. Ergonomics 2021, 64, 755–767. [Google Scholar] [CrossRef]
- Wang, H.; Wang, J.; Zhao, B.; Hu, S.; Xue, G.; Xia, J. Contamination and removal of polycyclic aromatic hydrocarbons in multilayered assemblies of firefighting protective clothing. J. Ind. Text. 2022, 52, 15280837221130772. [Google Scholar] [CrossRef]
- Wolffe, T.A.M.; Clinton, A.; Robinson, A.; Turrell, L.; Stec, A.A. Contamination of UK firefighters personal protective equipment and workplaces. Sci. Rep. 2023, 13, 65. [Google Scholar] [CrossRef] [PubMed]
- Staack, S.D.; Griffin, S.C.; Lee, V.S.T.; Lutz, E.A.; Burgess, J.L. Evaluation of CBRN Respirator Protection in Simulated Fire Overhaul Settings. Ann. Work Expo. Health 2021, 65, 843–853. [Google Scholar] [CrossRef]
- Wang, S.; Wang, Y. Musculoskeletal Model for Assessing Firefighters’ Internal Forces and Occupational Musculoskeletal Disorders During Self-Contained Breathing Apparatus Carriage. Saf. Health Work. 2022, 13, 315–325. [Google Scholar] [CrossRef]
- Oh, H.E.; Kim, S.J.; Woo, H.; Ham, S. Associations between Awareness of the Risk of Exposure to Pollutants Occurring at Fire Scenes and Health Beliefs among Metropolitan Firefighters in the Republic of Korea. Int. J. Environ. Res. Public Health 2022, 19, 8860. [Google Scholar] [CrossRef]
- Horn, G.P.; Fent, K.W.; Kerber, S.; Smith, D.L. Hierarchy of contamination control in the fire service: Review of exposure control options to reduce cancer risk. J. Occup. Environ. Hyg. 2022, 19, 538–557. [Google Scholar] [CrossRef]
- Fernandez, A.R.; Treichel, A.; Myers, J.B.; Bourn, S.S.; Crowe, R.P.; Gardner, B. Evaluating Firefighter On-Scene Decontamination Practices Using a National Fire Records Management System. J. Occup. Environ. Med. 2023, 65, 931–936. [Google Scholar] [CrossRef]
- Wilkinson, A.F.; Fent, K.W.; Mayer, A.C.; Chen, I.C.; Kesler, R.M.; Kerber, S.; Smith, D.L.; Horn, G.P. Use of Preliminary Exposure Reduction Practices or Laundering to Mitigate Polycyclic Aromatic Hydrocarbon Contamination on Firefighter Personal Protective Equipment Ensembles. Int. J. Environ. Res. Public Health 2023, 20, 2108. [Google Scholar] [CrossRef] [PubMed]
- Bralewska, K.; Bralewski, A.; Wolny, P.; Chiliński, B. Size-resolved particulate matter inside selected fire stations and preliminary evaluation of the effectiveness of washing machines in reducing its concentrations. Sci. Rep. 2024, 14, 18137. [Google Scholar] [CrossRef] [PubMed]
- Banks, A.P.W.; Wang, X.; Engelsman, M.; He, C.; Osorio, A.F.; Mueller, J.F. Assessing decontamination and laundering processes for the removal of polycyclic aromatic hydrocarbons and flame retardants from firefighting uniforms. Environ. Res. 2021, 194, 110616. [Google Scholar] [CrossRef] [PubMed]
- Calvillo, A.; Haynes, E.; Burkle, J.; Schroeder, K.; Calvillo, A.; Reese, J.; Reponen, T. Pilot study on the efficiency of water-only decontamination for firefighters’ turnout gear. J. Occup. Environ. Hyg. 2018, 16, 199–205. [Google Scholar] [CrossRef]
- Yuan, H.; Zhou, Y.; Zhou, F.; Huang, L.; Chen, T. Development and Experimental Study of Mobile Fire Smoke Decontamination System. Fire 2023, 6, 55. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).