Surface Characterisation of PEEK and Dentin, Treated with Atmospheric Non-Thermal PDD Plasma, Applicable for Dental Chair-Side Procedures
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Plasma Treatment
2.2.2. Contact Angle Measurement
2.2.3. Surface Roughness Measurement
2.2.4. SEM Analysis
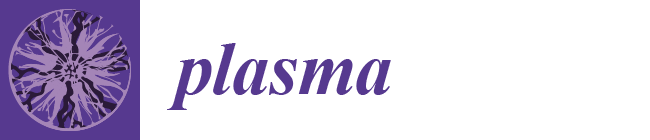
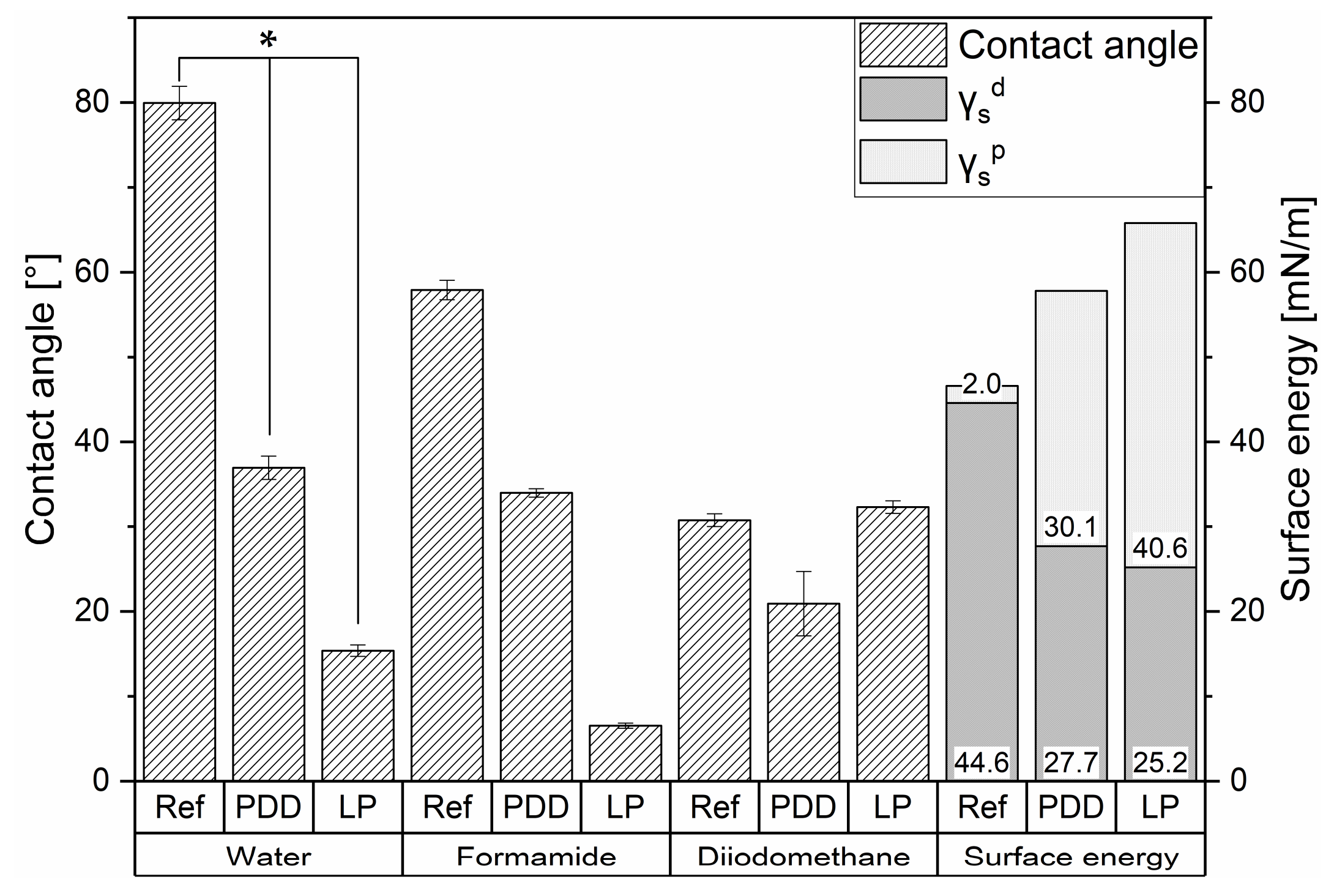
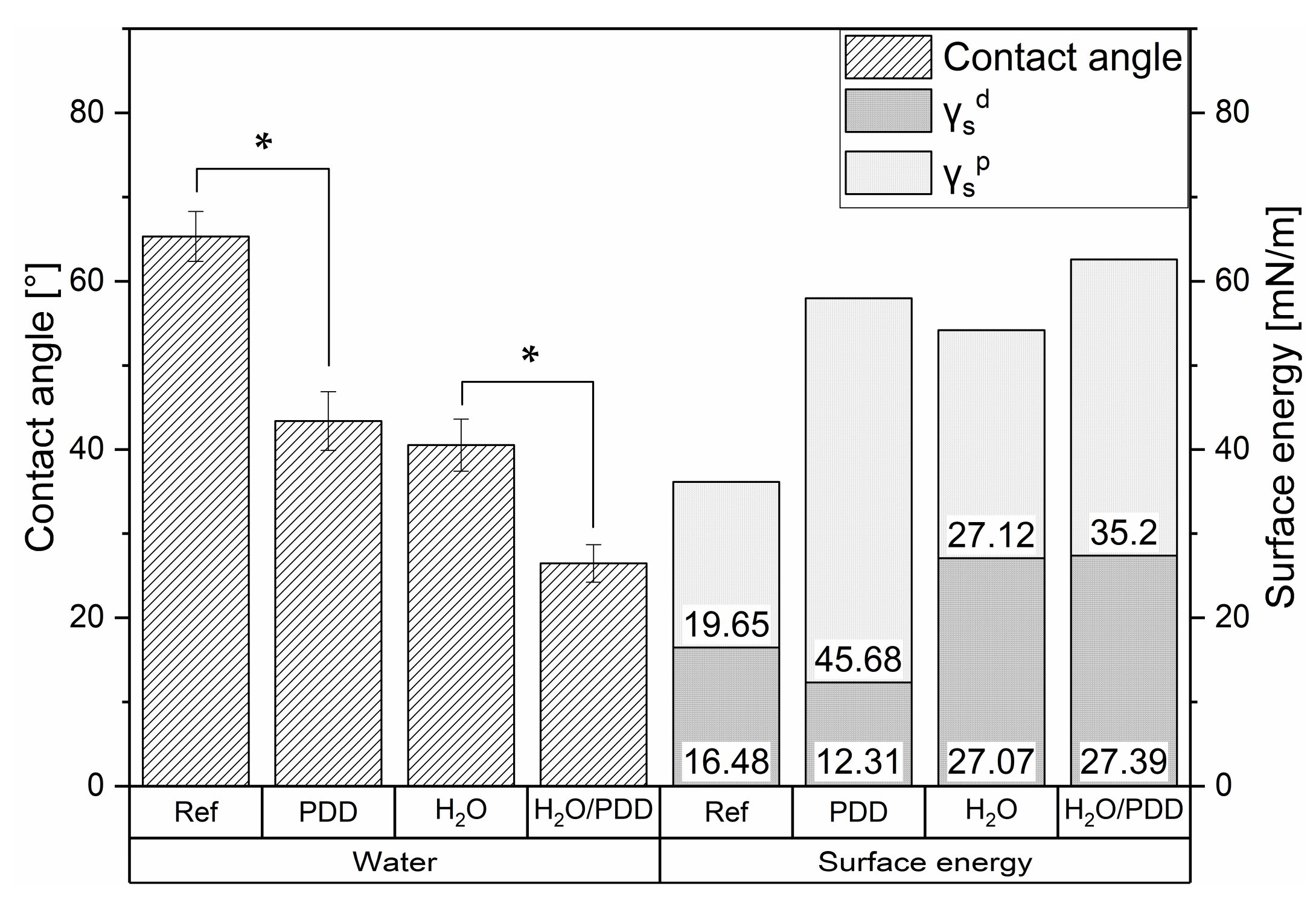
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schütte, U.; Walter, M. Zahnverlust und Zahnersatz vor dem Hintergrund des demographischen Wandels. In Prävention; Springer: Berlin/Heidelberg, Germany, 2006; pp. 575–594. [Google Scholar] [CrossRef]
- Santing, H.J.; Meijer, H.J.A.; Raghoebar, G.M.; Özcan, M. Fracture Strength and Failure Mode of Maxillary Implant-Supported Provisional Single Crowns: A Comparison of Composite Resin Crowns Fabricated Directly Over PEEK Abutments and Solid Titanium Abutments. Clin. Implant. Dent. Relat. Res. 2012, 14, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Escobar, M.; Henriques, B.; Fredel, M.C.; Silva, F.S.; Özcan, M.; Souza, J.C.M. Adhesion of PEEK to resin-matrix composites used in dentistry: A short review on surface modification and bond strength. J. Adhes. Sci. Technol. 2019, 1–12. [Google Scholar] [CrossRef]
- Arjun, B. Comparative Evaluation of the Push-Out Bond Strength of Glass Fiber Reinforced Composite Resin Post and Modified Polyetheretherketone (PEEK) Post Following Surface Treatments: An In Vitro Study. Master’s Thesis, Ragas Dental College and Hospital, Chennai, India, 2019. Available online: http://repository-tnmgrmu.ac.in/10915/ (accessed on 8 July 2021).
- Fricke, K.; Koban, I.; Tresp, H.; Jablonowski, L.; Schröder, K.; Kramer, A.; Weltmann, K.-D.; von Woedtke, T.; Kocher, T. Atmospheric Pressure Plasma: A High-Performance Tool for the Efficient Removal of Biofilms. PLoS ONE 2012, 7, e42539. [Google Scholar] [CrossRef] [PubMed]
- Pashley, D.H.; Tay, F.R.; Breschi, L.; Tjäderhane, L.; Carvalho, R.M.; Carrilho, M.; Tezvergil-Mutluay, A. State of the art etch-and-rinse adhesives. Dent. Mater. 2011, 27, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Nahar, A.B.; Gupta, A. Comparative evaluation of post operative sensitivity in etch and rinse and self etch adhesives: A longitudinal study. Int. Dent. J. Stud. Res. 2019, 7, 35–37. [Google Scholar] [CrossRef]
- Auschill, T.M.; Koch, C.A.; Wolkewitz, M.; Hellwig, E.; Arweiler, N.B. Occurrence and Causing Stimuli of Postoperative Sensitivity in Composite Restorations. Oper. Dent. 2009, 34, 3–10. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Li, C.; Lu, D.; Deng, J.; Zhang, X.; Yang, P. Amyloid-Like Rapid Surface Modification for Antifouling and In-Depth Remineralization of Dentine Tubules to Treat Dental Hypersensitivity. Adv. Mater. 2019, 31, e1903973. [Google Scholar] [CrossRef] [PubMed]
- Law, K.Y.; Zhao, H. Surface Wetting; Springer International Publishing: Cham, Switzerland, 2016. [Google Scholar] [CrossRef]
- Hippler, R. Hrsg. Low Temperature Plasmas; Wiley-VCH: Weinheim, Germany, 2008. [Google Scholar]
- Yang, Y.; Cho, Y.I.; Fridman, A.A. Plasma Discharge in Liquid: Water Treatment and Applications; CRC Press: Boca Raton, FL, USA, 2012; Available online: http://www.crcnetbase.com/isbn/9781439866238 (accessed on 27 April 2021).
- Chen, M.; Zhang, Y.; Driver, M.S.; Caruso, A.N.; Yu, Q.; Wang, Y. Surface modification of several dental substrates by non-thermal, atmospheric plasma brush. Dent. Mater. 2013, 29, 871–880. [Google Scholar] [CrossRef] [PubMed]
- Akkan, C.K.; Hammadeh, M.E.; May, A.; Park, H.-W.; Abdul-Khaliq, H.; Strunskus, T.; Aktas, O.C. Surface topography and wetting modifications of PEEK for implant applications. Lasers Med. Sci. 2014, 29, 1633–1639. [Google Scholar] [CrossRef] [PubMed]
- Przykaza, K.; Jurak, M.; Wiącek, A.; Mroczka, R. Characteristics of hybrid chitosan/phospholipid-sterol, peptide coatings on plasma activated PEEK polymer. Mater. Sci. Eng. C 2021, 120, 111658. [Google Scholar] [CrossRef] [PubMed]
- Cha, S.; Park, Y.-S. Plasma in dentistry. Clin. Plasma Med. 2014, 2, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Han, G.-J.; Kim, J.-H.; Chung, S.-N.; Chun, B.-H.; Kim, C.-K.; Seo, D.-G.; Son, H.-H.; Cho, B.-H. Effects of non-thermal atmospheric pressure pulsed plasma on the adhesion and durability of resin composite to dentin. Eur. J. Oral Sci. 2014, 122, 417–423. [Google Scholar] [CrossRef]
- Jha, S.; Bhowmik, S.; Bhatnagar, N.; Bhattacharya, N.K.; Deka, U.; Iqbal HM, S.; Benedictus, R. Experimental investigation into the effect of adhesion properties of PEEK modified by atmospheric pressure plasma and low pressure plasma. J. Appl. Polym. Sci. 2010, 118, 173–179. [Google Scholar] [CrossRef]
- Koban, I.; Duske, K.; Jablonowski, L.; Schröder, K.; Nebe, B.; Sietmann, R.; Weltmann, K.-D.; Hübner, N.-O.; Kramer, A.; Kocher, T. Atmospheric Plasma Enhances Wettability and Osteoblast Spreading on Dentin In Vitro: Proof-of-Principle. Plasma Process. Polym. 2011, 8, 975–982. [Google Scholar] [CrossRef]
- Judée, F.; Simon, S.; Bailly, C.; Dufour, T. Plasma-activation of tap water using DBD for agronomy applications: Identification and quantification of long lifetime chemical species and production/consumption mechanisms. Water Res. 2018, 133, 47–59. [Google Scholar] [CrossRef] [PubMed]
- Laurita, R.; Barbieri, D.; Gherardi, M.; Colombo, V.; Lukes, P. Chemical analysis of reactive species and antimicrobial activity of water treated by nanosecond pulsed DBD air plasma. Clin. Plasma Med. 2015, 3, 53–61. [Google Scholar] [CrossRef]
- Zhou, R.; Zhou, R.; Wang, P.; Xian, Y.; Mai-Prochnow, A.; Lu, X.; Cullen, P.J.; Ostrikov, K.; Kateryna, B. Plasma-activated water: Generation, origin of reactive species and biological applications. J. Phys. D Appl. Phys. 2020, 53, 303001. [Google Scholar] [CrossRef]
- Dong, X.; Li, H.; Chen, M.; Wang, Y.; Yu, Q. Plasma treatment of dentin surfaces for improving self-etching adhesive/dentin interface bonding. Clin. Plasma Med. 2015, 3, 10–16. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Behnecke, M.; Steinert, V.; Petersen, S. Surface Characterisation of PEEK and Dentin, Treated with Atmospheric Non-Thermal PDD Plasma, Applicable for Dental Chair-Side Procedures. Plasma 2021, 4, 389-398. https://doi.org/10.3390/plasma4030028
Behnecke M, Steinert V, Petersen S. Surface Characterisation of PEEK and Dentin, Treated with Atmospheric Non-Thermal PDD Plasma, Applicable for Dental Chair-Side Procedures. Plasma. 2021; 4(3):389-398. https://doi.org/10.3390/plasma4030028
Chicago/Turabian StyleBehnecke, Marius, Vincent Steinert, and Svea Petersen. 2021. "Surface Characterisation of PEEK and Dentin, Treated with Atmospheric Non-Thermal PDD Plasma, Applicable for Dental Chair-Side Procedures" Plasma 4, no. 3: 389-398. https://doi.org/10.3390/plasma4030028
APA StyleBehnecke, M., Steinert, V., & Petersen, S. (2021). Surface Characterisation of PEEK and Dentin, Treated with Atmospheric Non-Thermal PDD Plasma, Applicable for Dental Chair-Side Procedures. Plasma, 4(3), 389-398. https://doi.org/10.3390/plasma4030028