Effect of Ferrule Design on Stress Distribution of Maxillary Incisor Rehabilitated with Ceramic Crown and PEEK Post–Core Material: A 3D Finite Element Analysis
Abstract
:1. Introduction
2. Materials and Methods
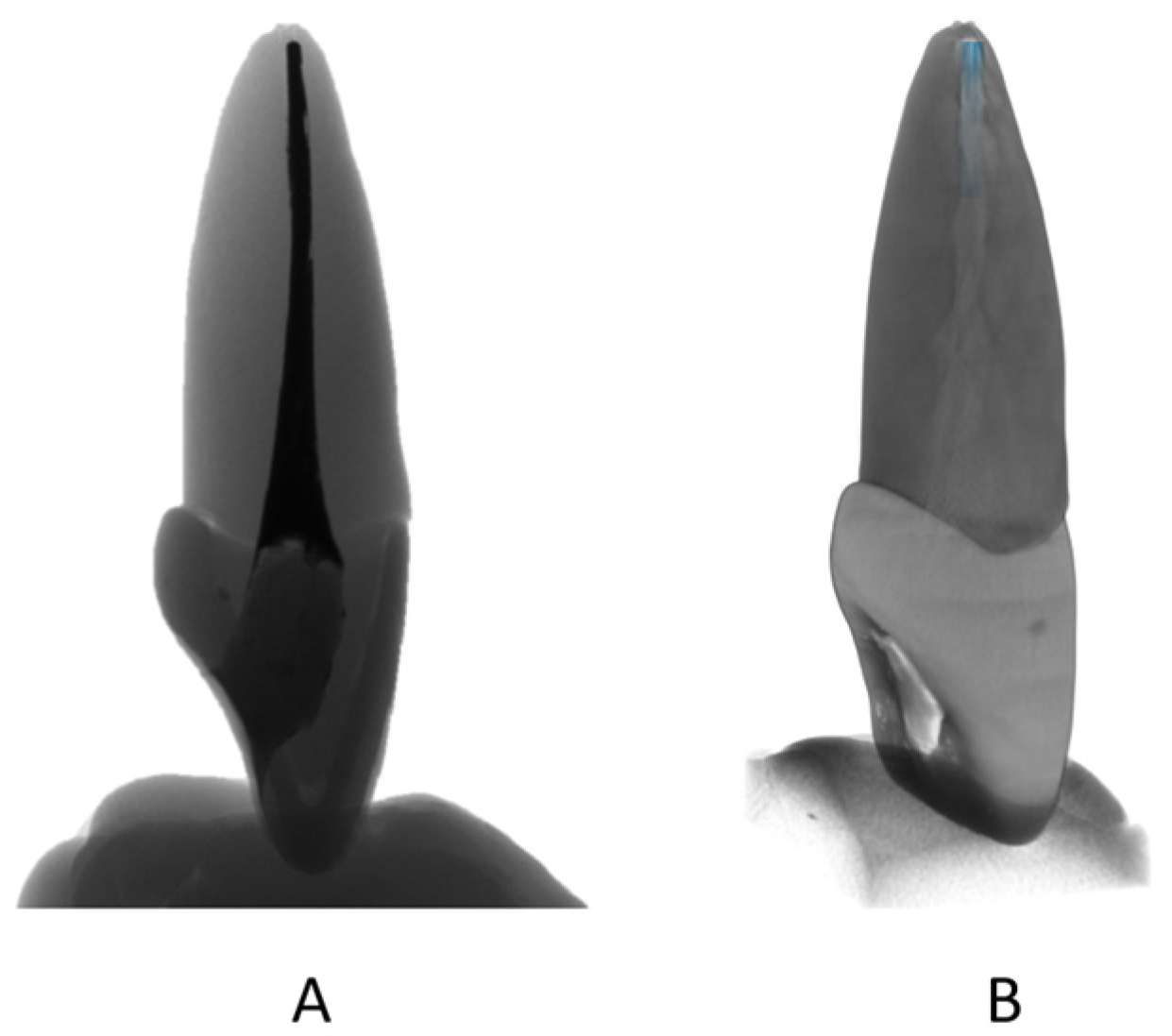
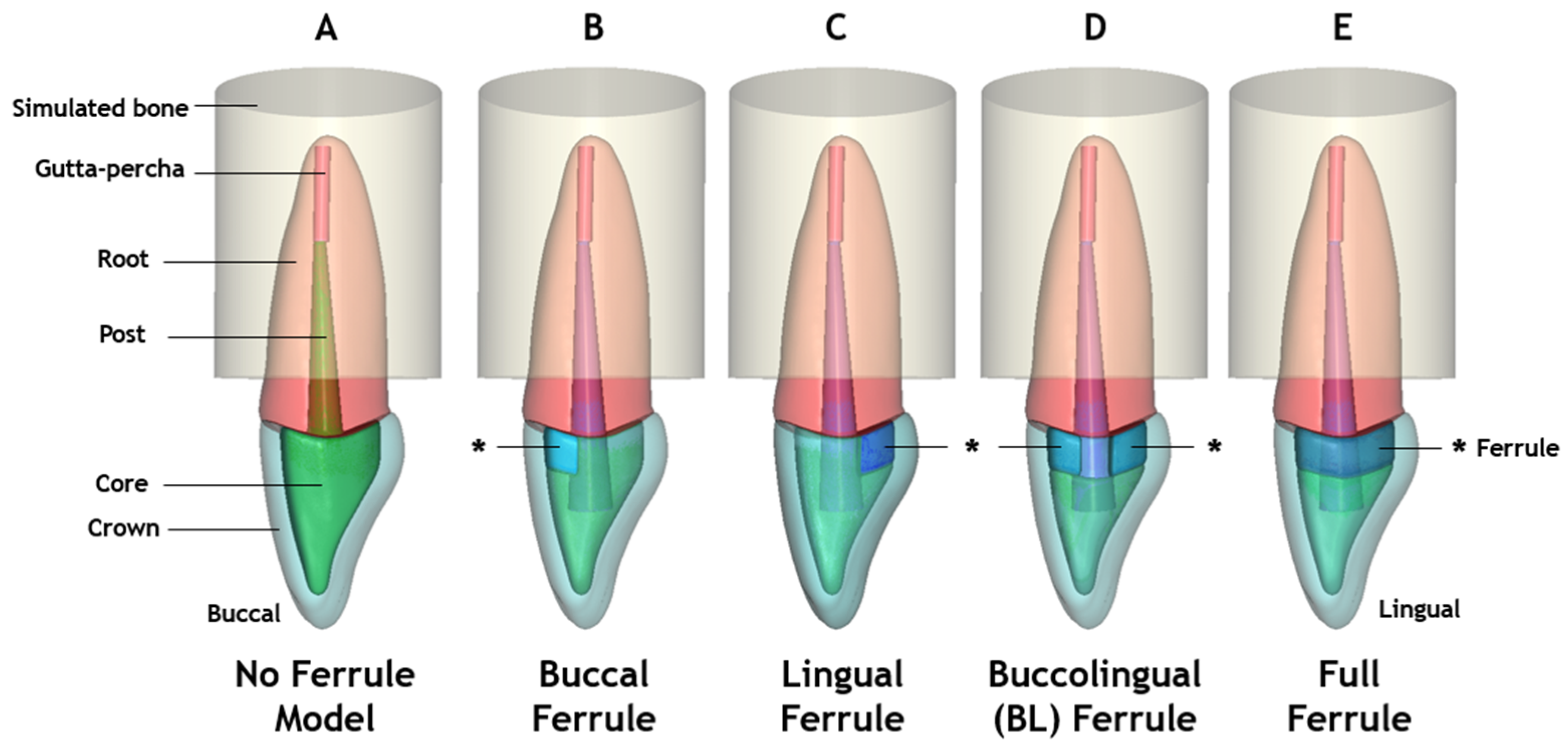
2.1. Three-Dimensional Models
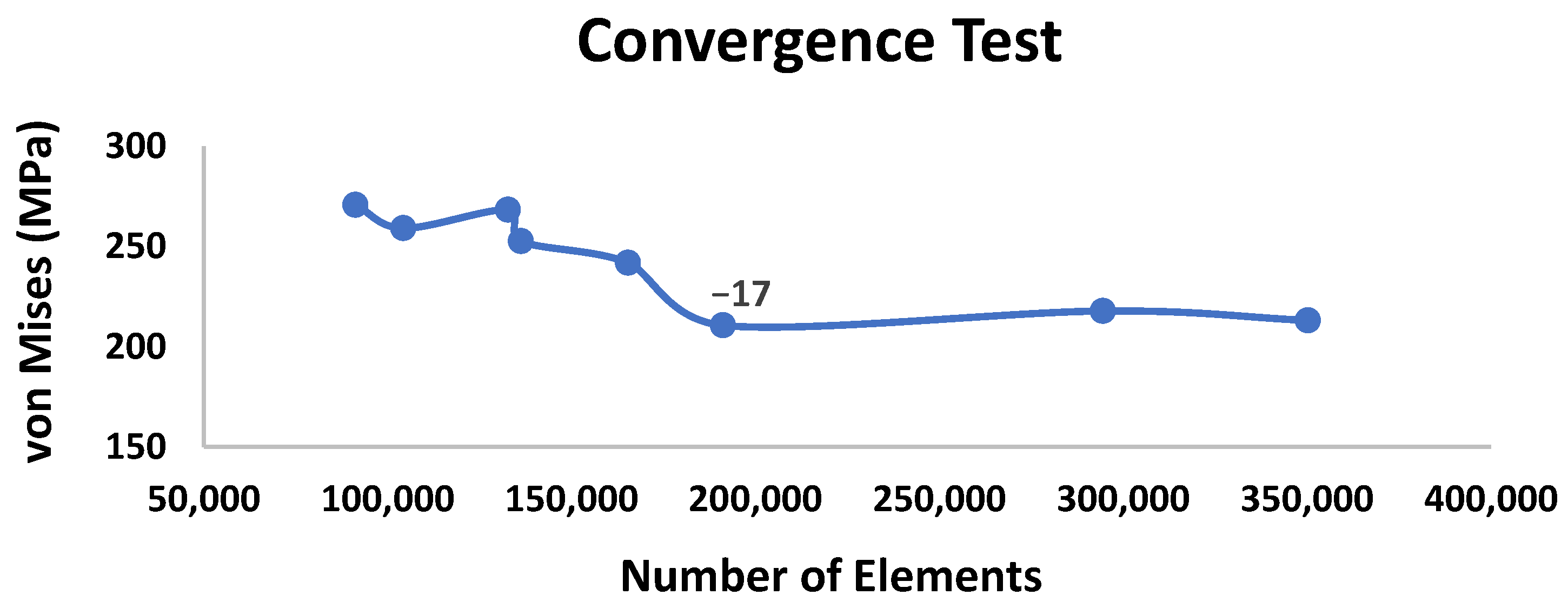
2.2. Finite Element Analysis
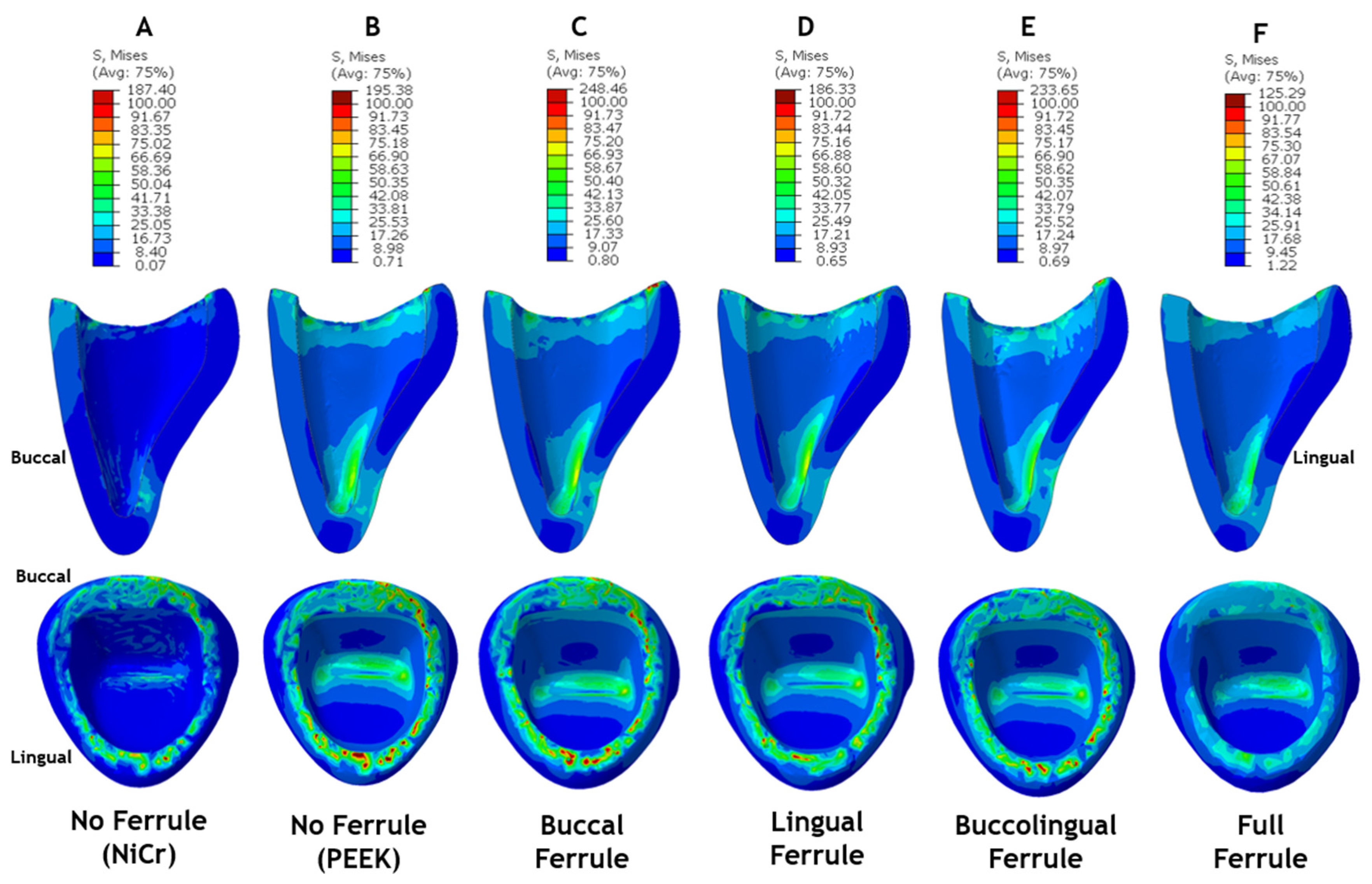
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yu, H.; Feng, Z.; Wang, L.; Mihcin, S.; Kang, J.; Bai, S.; Zhao, Y. Finite Element Study of PEEK Materials Applied in Post-Retained Restorations. Polymers 2022, 14, 3422. [Google Scholar] [CrossRef] [PubMed]
- American Association of Endodontists (AAE). Available online: https://newsroom.aae.org/press-kit/ (accessed on 15 August 2023).
- Hedlund, S.O.; Johansson, N.G.; Sjögren, G. Retention of prefabricated and individually cast root canal posts in vitro. Br. Dent. J. 2003, 195, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Özkurt, Z.; Iseri, U.; Kazazoglu, E. Zirconia ceramic post systems: A literature review and a case report. Dent. Mater. J. 2010, 29, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Callister, W.D.; Rethwisch, D.G. Materials Science and Engineering: An Introduction; John Wiley & Sons: Hoboken, NJ, USA, 2010. [Google Scholar]
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Siddiqui, F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J. Prosthodont. Res. 2016, 60, 12–19. [Google Scholar] [CrossRef] [PubMed]
- De Ruiter, L.; Janssen, D.; Briscoe, A.; Verdonschot, N. The mechanical response of a polyetheretherketone femoral knee implant under a deep squatting loading condition. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2017, 231, 1204–1212. [Google Scholar] [CrossRef]
- Assiri, A.Y.K.; Saafi, J.; Al-Moaleem, M.M.; Mehta, V. Ferrule effect and its importance in restorative dentistry: A literature Review. J. Popul. Ther. Clin. Pharmacol. 2022, 29, e69–e82. [Google Scholar] [CrossRef]
- Khabadze, Z.; Mordanov, O.; Taraki, F.; Magomedov, O.; Kuznetsova, A.; Solimanov, S.; Nazhmudinov, S.; Bokova, R.; Adzhieva, A.; Bakaev, Y. Effects of the Ferrule Design on Fracture Resistance to Endodontically-Treated Teeth Restored with Fiber Posts: A Systematic Review. Open Dent. J. 2019, 13, 493–498. [Google Scholar] [CrossRef]
- Figueiredo, F.E.; Santos, R.C.; Silva, A.S.; Valdívia, A.D.; Oliveira-Neto, L.A.; Griza, S.; Soares, C.J.; Faria, E.S.A.L. Ferrule Design Does Not Affect the Biomechanical Behavior of Anterior Teeth Under Mechanical Fatigue: An In Vitro Evaluation. Oper. Dent. 2019, 44, 273–280. [Google Scholar] [CrossRef]
- Mahdavi Izadi, Z.; Jalalian, E.; Eyvaz Ziaee, A.; Zamani, L.; Javanshir, B. Evaluation of the effect of different ferrule designs on fracture resistance of maxillary incisors restored with bonded posts and cores. J. Dent. 2010, 7, 146–155. [Google Scholar]
- Dikbas, I.; Tanalp, J.; Ozel, E.; Koksal, T.; Ersoy, M. Evaluation of the effect of different ferrule designs on the fracture resistance of endodontically treated maxillary central incisors incorporating fiber posts, composite cores and crown restorations. J. Contemp. Dent. Pract. 2007, 8, 62–69. [Google Scholar]
- Hinckfuss, S.; Wilson, P.R. Effect of Core Material and Restoration Design on Strength of Endodontically Treated Bovine Teeth: A Laboratory Study. J. Prosthodont. 2008, 17, 456–461. [Google Scholar] [CrossRef] [PubMed]
- Al-Hazaimeh, N.; Gutteridge, D.L. An in vitro study into the effect of the ferrule preparation on the fracture resistance of crowned teeth incorporating prefabricated post and composite core restorations. Int. Endod. J. 2001, 34, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Upadhyaya, V.; Bhargava, A.; Parkash, H.; Chittaranjan, B.; Kumar, V. A finite element study of teeth restored with post and core: Effect of design, material, and ferrule. Dent. Res. J. 2016, 13, 233. [Google Scholar] [CrossRef] [PubMed]
- Mosharaf, R.; Abolhasani, M.; Fathi, A.H.; Rajabi, A. The Effect of Ferrule/Crown Ratio and Post Length on the Applied Stress and Strain Distribution to the Endodontically Treated Maxillary Central Teeth: A Finite Element Analysis. Front. Dent. 2023, 20, 16. [Google Scholar] [CrossRef]
- Santos, A.F.; Meira, J.B.; Tanaka, C.B.; Xavier, T.A.; Ballester, R.Y.; Lima, R.G.; Pfeifer, C.S.; Versluis, A. Can fiber posts increase root stresses and reduce fracture? J. Dent. Res. 2010, 89, 587–591. [Google Scholar] [CrossRef]
- Tagahara, A.; Masaki, C.; Nodai, T.; Munemasa, T.; Mukaibo, T.; Kondo, Y.; Hosokawa, R. Stress Distribution in Maxillary Central Incisors without Ferrules: A Finite Element Analysis of Post and Core Systems. Open J. Stomatol. 2021, 11, 251–262. [Google Scholar] [CrossRef]
- Santos, T.D.S.A.; Abu Hasna, A.; Abreu, R.T.; Tribst, J.P.M.; De Andrade, G.S.; Borges, A.L.S.; Torres, C.R.G.; Carvalho, C.A.T. Fracture resistance and stress distribution of weakened teeth reinforced with a bundled glass fiber–reinforced resin post. Clin. Oral. Investig. 2022, 26, 1725–1735. [Google Scholar] [CrossRef]
- Alberto, L.H.J.; Kalluri, L.; Esquivel-Upshaw, J.F.; Duan, Y. Three-Dimensional Finite Element Analysis of Different Connector Designs for All-Ceramic Implant-Supported Fixed Dental Prostheses. Ceramics 2022, 5, 34–43. [Google Scholar] [CrossRef]
- Alberto, L.H.J.; Kalluri, L.; Esquivel-Upshaw, J.F.; Duan, Y. Finite Element Analysis of an Implant-Supported FDP with Different Connector Heights. Symmetry 2022, 14, 2334. [Google Scholar] [CrossRef]
- Meira, J.B.C.; Jikihara, A.N.; Capetillo, P.; Roscoe, M.G.; Cattaneo, P.M.; Ballester, R.Y. Finite Element Analysis in Dentistry. In Dental Biomaterials; World Scientific: Singapore, 2018; Volume 2, pp. 67–89. [Google Scholar]
- Ahmed, W.M.; Abdallah, M.-N.; McCullagh, A.P.; Wyatt, C.C.L.; Troczynski, T.; Carvalho, R.M. Marginal Discrepancies of Monolithic Zirconia Crowns: The Influence of Preparation Designs and Sintering Techniques. J. Prosthodont. 2019, 28, 288–298. [Google Scholar] [CrossRef]
- Bernauer, S.A.; Müller, J.; Zitzmann, N.U.; Joda, T. Influence of Preparation Design, Marginal Gingiva Location, and Tooth Morphology on the Accuracy of Digital Impressions for Full-Crown Restorations: An In Vitro Investigation. J. Clin. Med. 2020, 9, 3984. [Google Scholar] [CrossRef]
- Mehmert, P. Chapter Eleven—Residual stress analysis and geometrical tolerances in powder bed fusion and direct energy deposition processes. In Quality Analysis of Additively Manufactured Metals; Kadkhodapour, J., Schmauder, S., Sajadi, F., Eds.; Elsevier: Amsterdam, The Netherlands, 2023; pp. 429–486. [Google Scholar] [CrossRef]
- Celik, H.K.; Koc, S.; Kustarci, A.; Rennie, A.E.W. A literature review on the linear elastic material properties assigned in finite element analyses in dental research. Mater. Today Commun. 2022, 30, 103087. [Google Scholar] [CrossRef]
- Nokar, S.; Bahrami, M.; Mostafavi, A.S. Comparative Evaluation of the Effect of Different Post and Core Materials on Stress Distribution in Radicular Dentin by Three-Dimensional Finite Element Analysis. J. Dent. 2018, 15, 69–78. [Google Scholar]
- Hallak, A.G.; Caldas, R.A.; Silva, I.D.; Miranda, M.E.; Brandt, W.C.; Vitti, R.P. Stress distribution in restorations with glass fiber and polyetheretherketone intraradicular posts: An in silico analysis. Dent. Mater. J. 2022, 41, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-S.; Shin, J.-H.; Kim, J.-E.; Kim, J.-H.; Lee, W.-C.; Shin, S.-W.; Lee, J.-Y. Biomechanical Evaluation of a Tooth Restored with High Performance Polymer PEKK Post-Core System: A 3D Finite Element Analysis. BioMed Res. Int. 2017, 2017, 1373127. [Google Scholar] [CrossRef]
- Huang, L.; Nemoto, R.; Okada, D.; Shin, C.; Saleh, O.; Oishi, Y.; Takita, M.; Nozaki, K.; Komada, W.; Miura, H. Investigation of stress distribution within an endodontically treated tooth restored with different restorations. J. Dent. Sci. 2022, 17, 1115–1124. [Google Scholar] [CrossRef]
- Adigüzel, Ö.; Kaya, S.; Yiğit Özer, S.; Değer, Y.; Göncü Başaran, E.; Yavuz, İ. Three-dimensional Finite Element Analysis of Endodontically Treated Tooth Restored with Carbon and Titanium Posts. Int. Dent. Res. 2011, 1, 55. [Google Scholar] [CrossRef]
- Alper, B.; Gultekin, P.; Yalci, S. Application of Finite Element Analysis in Implant Dentistry. In Finite Element Analysis: New Trends and Developments; InTech: Rijeka, Croatia, 2012. [Google Scholar] [CrossRef]
- Zhou, T.F.; Zhang, X.H.; Wang, X.Z. Three-dimensional finite element analysis of one-piece computer aided design and computer aided manufacture involved zirconia post and core. Beijing Da Xue Xue Bao Yi Xue Ban 2015, 47, 78–84. [Google Scholar]
- Badami, V.; Ketineni, H.; Pb, S.; Akarapu, S.; Mittapalli, S.P.; Khan, A. Comparative Evaluation of Different Post Materials on Stress Distribution in Endodontically Treated Teeth Using the Finite Element Analysis Method: A Systematic Review. Cureus 2022, 14, e29753. [Google Scholar] [CrossRef]
- Kharboutly, N.A.-D.; Allaf, M.; Kanout, S. Three-Dimensional Finite Element Study of Endodontically Treated Maxillary Central Incisors Restored Using Different Post and Crown Materials. Cureus 2023, 15, e33778. [Google Scholar] [CrossRef]
- Nahar, R.; Mishra, S.K.; Chowdhary, R. Evaluation of stress distribution in an endodontically treated tooth restored with four different post systems and two different crowns- A finite element analysis. J. Oral. Biol. Craniofacial Res. 2020, 10, 719–726. [Google Scholar] [CrossRef] [PubMed]
- Tekin, S.; Adiguzel, O.; Cangul, S.; Atas, O.; Erpacal, B. Evaluation of the use of PEEK material in post-core and crown restorations using finite element analysis. Am. J. Dent. 2020, 33, 251–257. [Google Scholar] [PubMed]
- Nakamura, T.; Ohyama, T.; Waki, T.; Kinuta, S.; Wakabayashi, K.; Mutobe, Y.; Takano, N.; Yatani, H. Stress Analysis of Endodontically Treated Anterior Teeth Restored with Different Types of Post Material. Dent. Mater. J. 2006, 25, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.M.; Dawood, S.N.; Dalloo, G.A.M.; Al-Barazanchi, T.R.H. Evaluation of mechanical properties of different polyetheretherketone endodontic post systems: An in vitro study. BMC Oral Health 2023, 23, 537. [Google Scholar] [CrossRef]
- Sugano, K.; Komada, W.; Okada, D.; Miura, H. Evaluation of composite resin core with prefabricated polyetheretherketone post on fracture resistance in the case of flared root canals. Dent. Mater. J. 2020, 39, 924–932. [Google Scholar] [CrossRef]
- Kasem, A.T.; Shams, M.; Tribst, J.P.M. The Use of Polyetheretherketone (PEEK) as an Alternative Post and Core Material: Five-Year Follow-Up Report. Dent. J. 2022, 10, 237. [Google Scholar] [CrossRef]
- Zoidis, P. The Use of Modified Polyetheretherketone Post and Core for an Esthetic Lithium Disilicate Anterior Ceramic Restoration: A Clinical Report. Int. J. Prosthodont. 2021, 34, 120–125. [Google Scholar] [CrossRef]
- Al-sanabani, F.; Al-Makramani, B.; Alaajam, W.; Al-ak’hali, M.; Alhajj, M.; Nassani, M.Z.; Assad, M.; Al-Maweri, S. Effect of partial ferrule on fracture resistance of endodontically treated teeth: A meta-analysis of in-vitro studies. J. Prosthodont. Res. 2023, 67, 348–359. [Google Scholar] [CrossRef]
- Muangamphan, P.; Sattapan, B.; Kukiattrakoon, B.; Thammasitboon, K. The effect of incomplete crown ferrules on fracture resistance and failure modes of endodontically treated maxillary incisors restored with quartz fiber post, composite core, and crowns. J. Conserv. Dent. 2015, 18, 187–191. [Google Scholar] [CrossRef]
- Naumann, M.; Preuss, A.; Rosentritt, M. Effect of incomplete crown ferrules on load capacity of endodontically treated maxillary incisors restored with fiber posts, composite build-ups, and all-ceramic crowns: An in vitro evaluation after chewing simulation. Acta Odontol. Scand. 2006, 64, 31–36. [Google Scholar] [CrossRef]
- Ng, C.C.; Dumbrigue, H.B.; Al-Bayat, M.I.; Griggs, J.A.; Wakefield, C.W. Influence of remaining coronal tooth structure location on the fracture resistance of restored endodontically treated anterior teeth. J. Prosthet. Dent. 2006, 95, 290–296. [Google Scholar] [CrossRef]



| Model Component | Material | Young’s Modulus (GPa) | Poison’s Ratio | References |
|---|---|---|---|---|
| Bone support | Cancellous bone | 1.37 | 0.30 | [1,28] |
| Filling material | Gutta-percha | 0.69 | 0.45 | [1,31] |
| Root, ferrule | Dentin | 18.60 | 0.31 | [1,29] |
| Post, core | Nickel–chromium (NiCr) | 203.60 | 0.30 | [15] |
| Pure PEEK | 4.10 | 0.40 | [1,30] | |
| Crown | Zirconia | 200.00 | 0.33 | [27,32] |
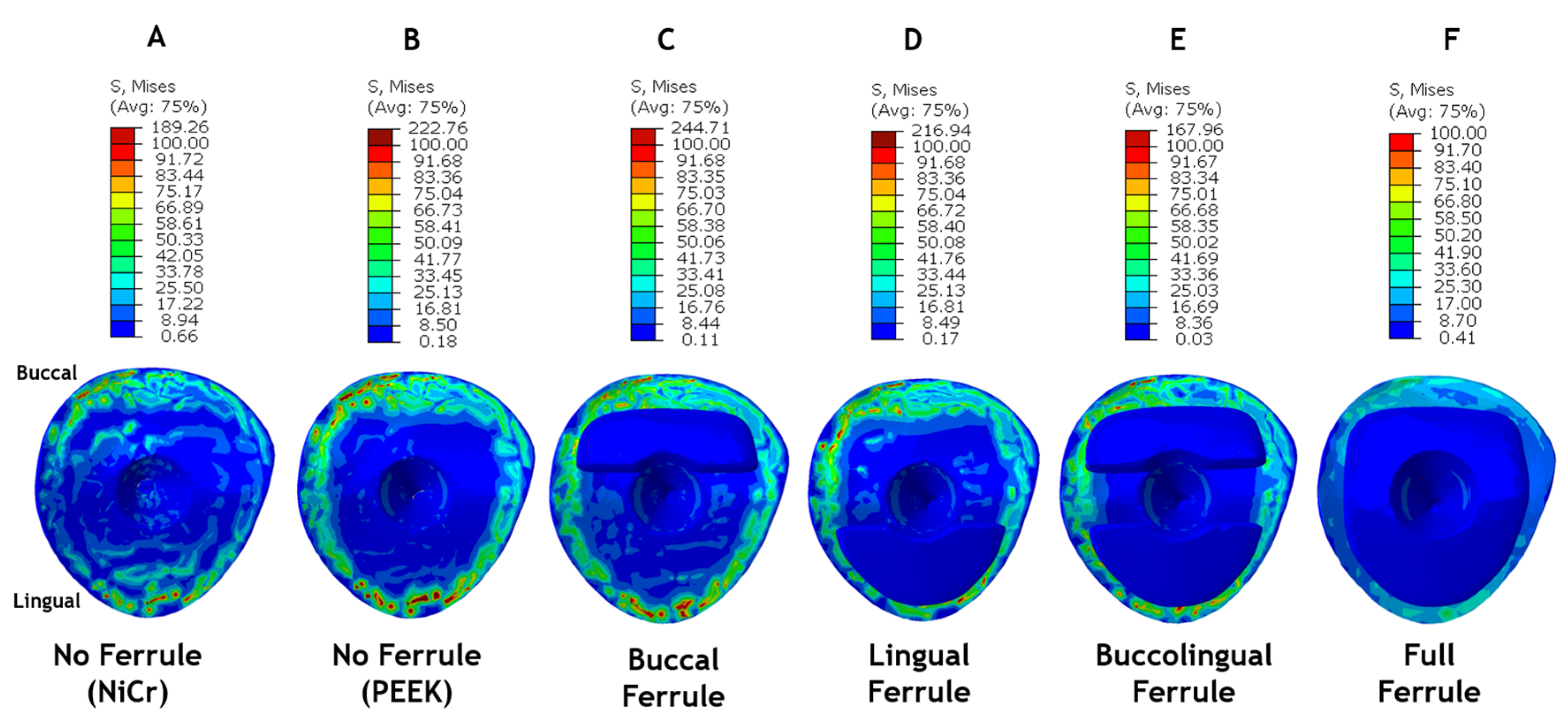
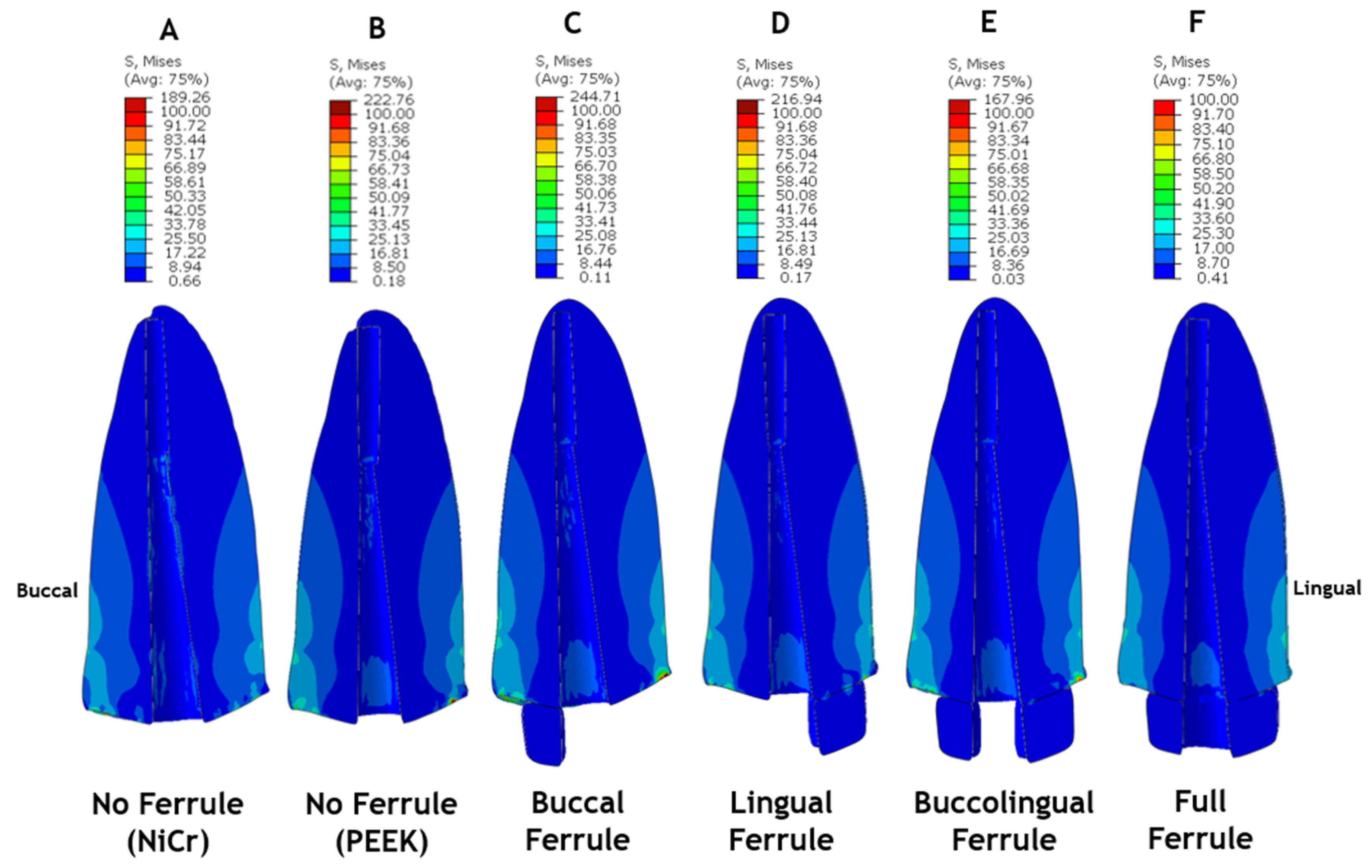
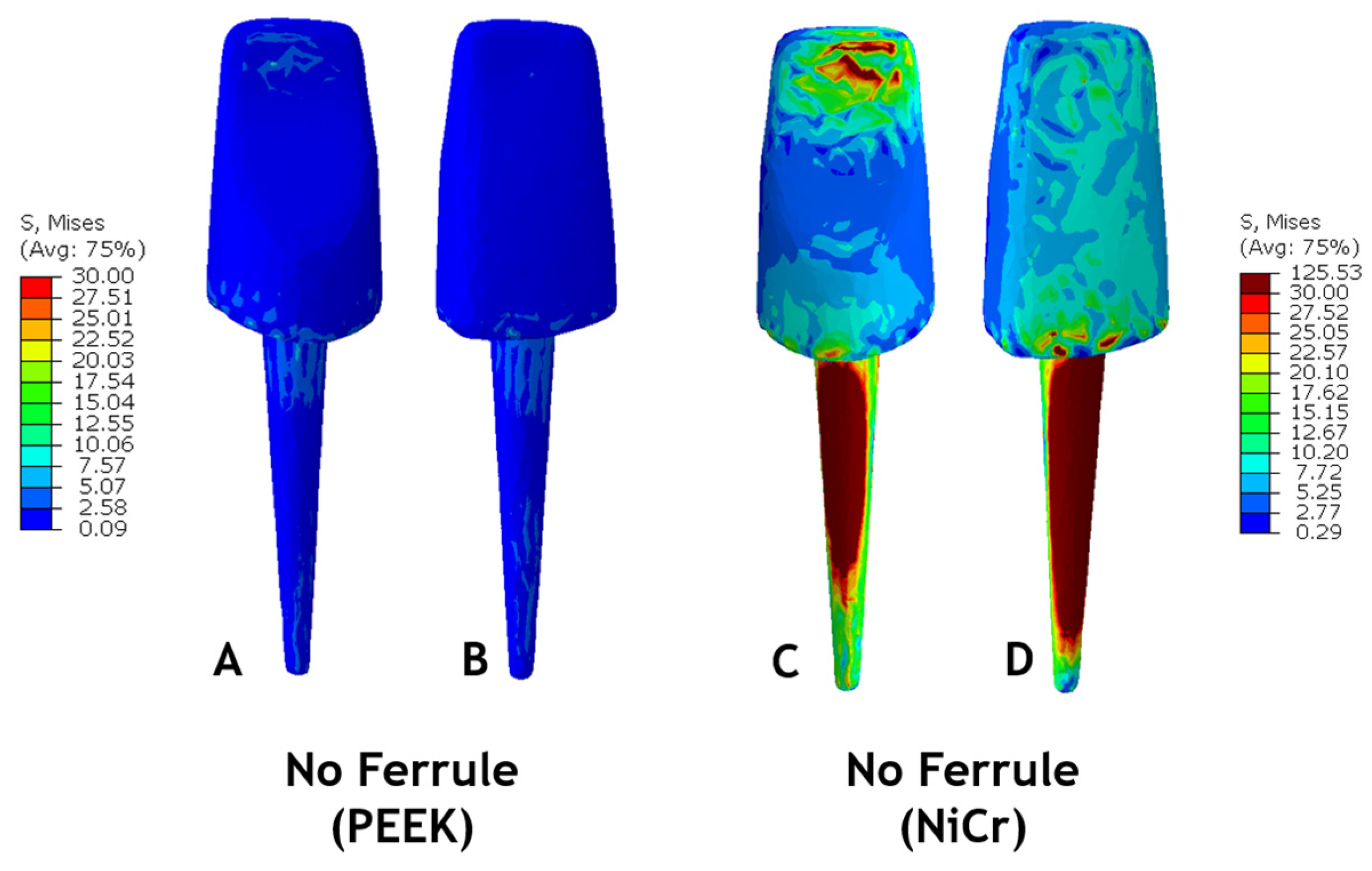
| Assembly Model | Peak Stress (von Mises—MPa) | Location |
|---|---|---|
| No ferrule (NiCr) | 189 | Root (buccal) |
| No ferrule (PEEK) | 223 | Root (buccal) |
| Buccal ferrule | 248 | Crown (buccal) |
| Lingual ferrule | 217 | Root (buccal) |
| Buccalingual ferrule | 234 | Crown (lingual) |
| Full ferrule | 125 | Crown (buccal) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alberto, L.H.J.; Zhang, Z.; Duan, Y. Effect of Ferrule Design on Stress Distribution of Maxillary Incisor Rehabilitated with Ceramic Crown and PEEK Post–Core Material: A 3D Finite Element Analysis. Ceramics 2023, 6, 2256-2268. https://doi.org/10.3390/ceramics6040137
Alberto LHJ, Zhang Z, Duan Y. Effect of Ferrule Design on Stress Distribution of Maxillary Incisor Rehabilitated with Ceramic Crown and PEEK Post–Core Material: A 3D Finite Element Analysis. Ceramics. 2023; 6(4):2256-2268. https://doi.org/10.3390/ceramics6040137
Chicago/Turabian StyleAlberto, Laura H. J., Zhaoxu Zhang, and Yuanyuan Duan. 2023. "Effect of Ferrule Design on Stress Distribution of Maxillary Incisor Rehabilitated with Ceramic Crown and PEEK Post–Core Material: A 3D Finite Element Analysis" Ceramics 6, no. 4: 2256-2268. https://doi.org/10.3390/ceramics6040137
APA StyleAlberto, L. H. J., Zhang, Z., & Duan, Y. (2023). Effect of Ferrule Design on Stress Distribution of Maxillary Incisor Rehabilitated with Ceramic Crown and PEEK Post–Core Material: A 3D Finite Element Analysis. Ceramics, 6(4), 2256-2268. https://doi.org/10.3390/ceramics6040137










