Comparative Fracture Resistance Analysis of Translucent Monolithic Zirconia Dioxide Milled in a CAD/CAM System
Abstract
1. Introduction
- Monolithic Zirconia
1.1. Zirconia Cercon HT Dentsply-Sirona (CDS)
1.2. Zirconia Solid Gen-X Amann Girrbach (ZGX)
2. Materials and Methods
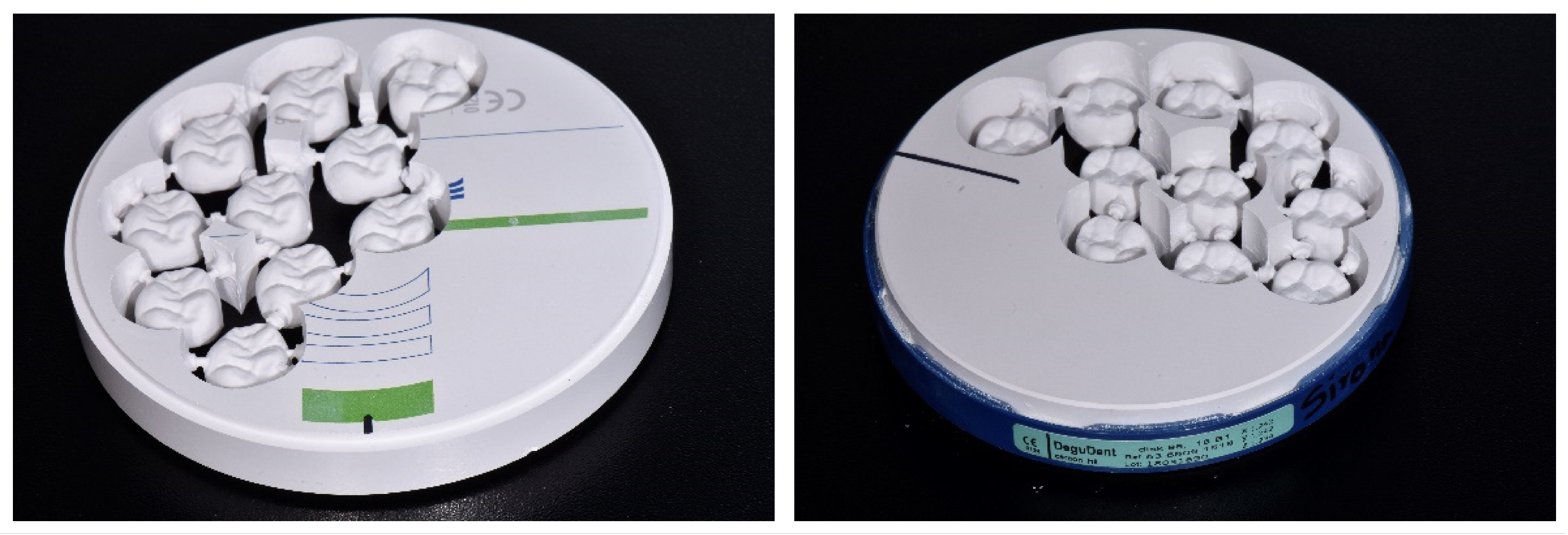
2.1. Materials
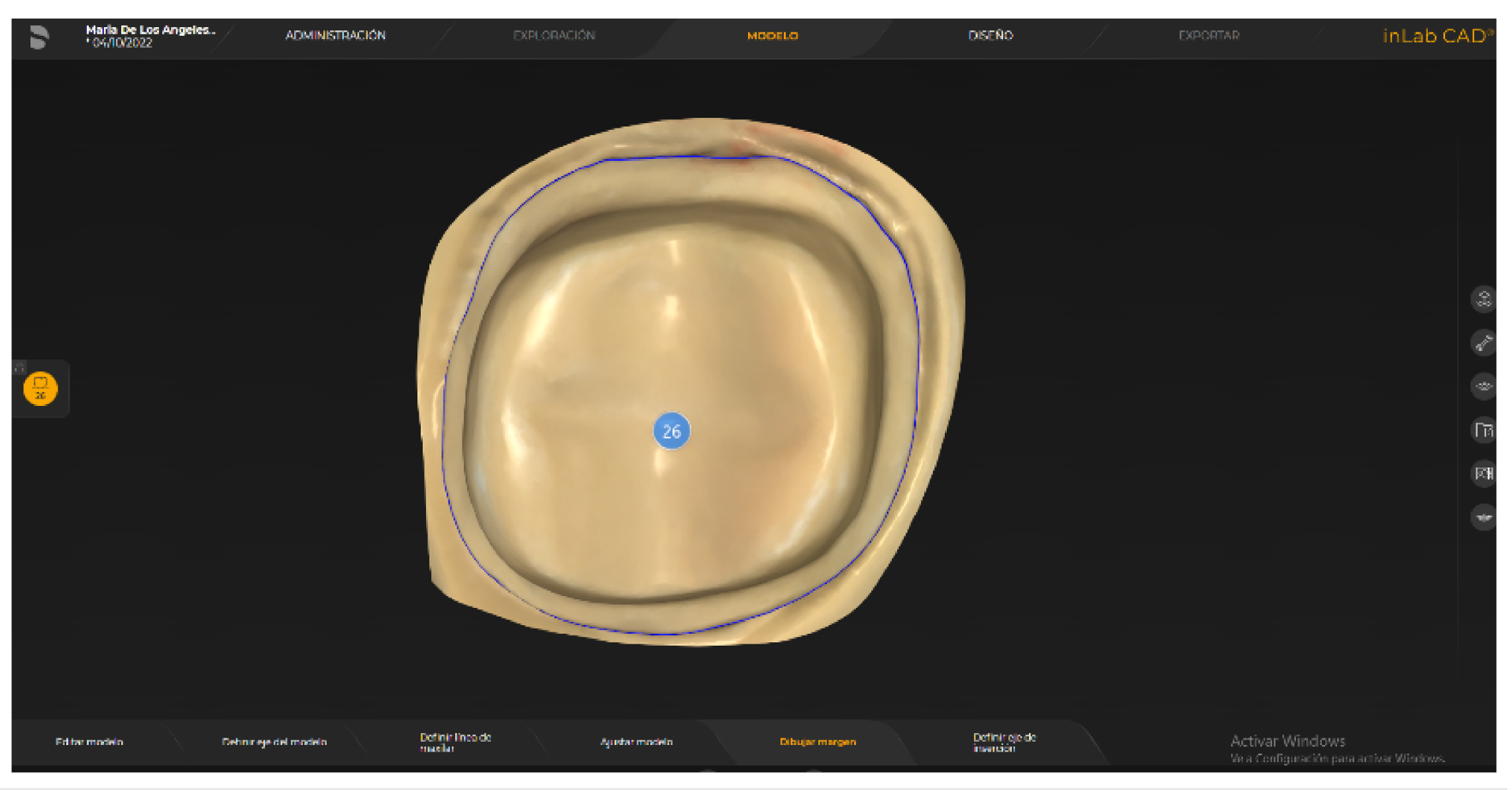
2.2. Digitalization of the Model and Design
2.3. Sinterization
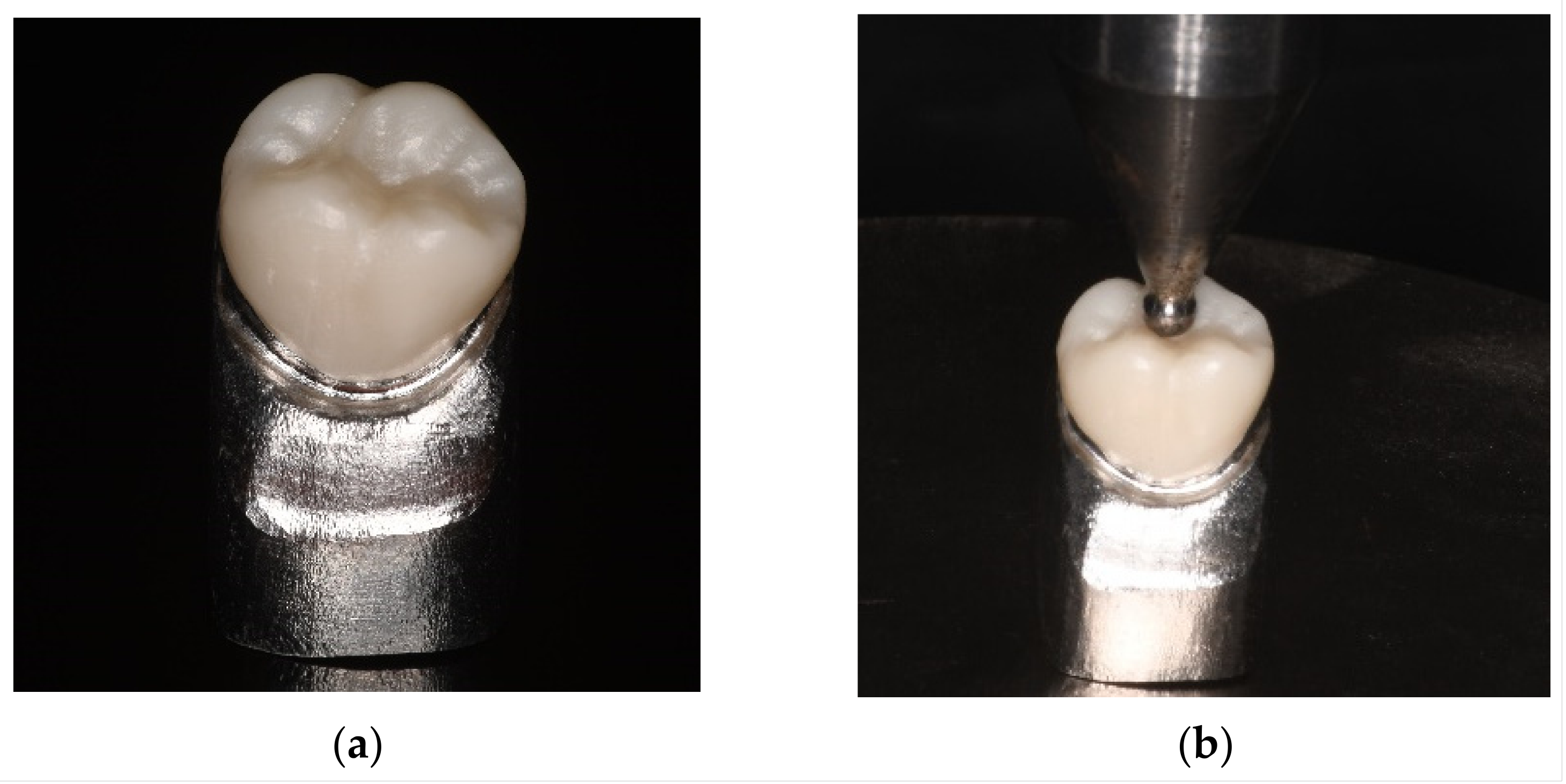
2.4. Fracture Test
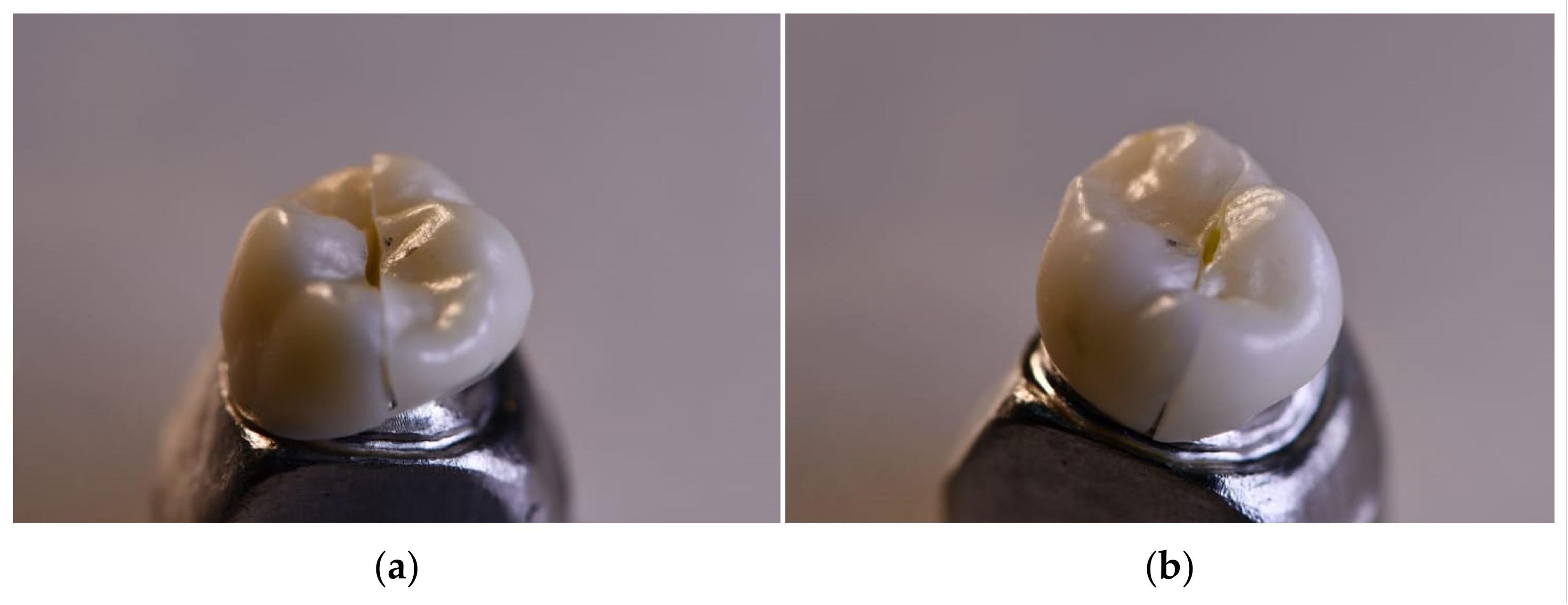
2.5. Evaluation of the Fracture Mode
3. Results
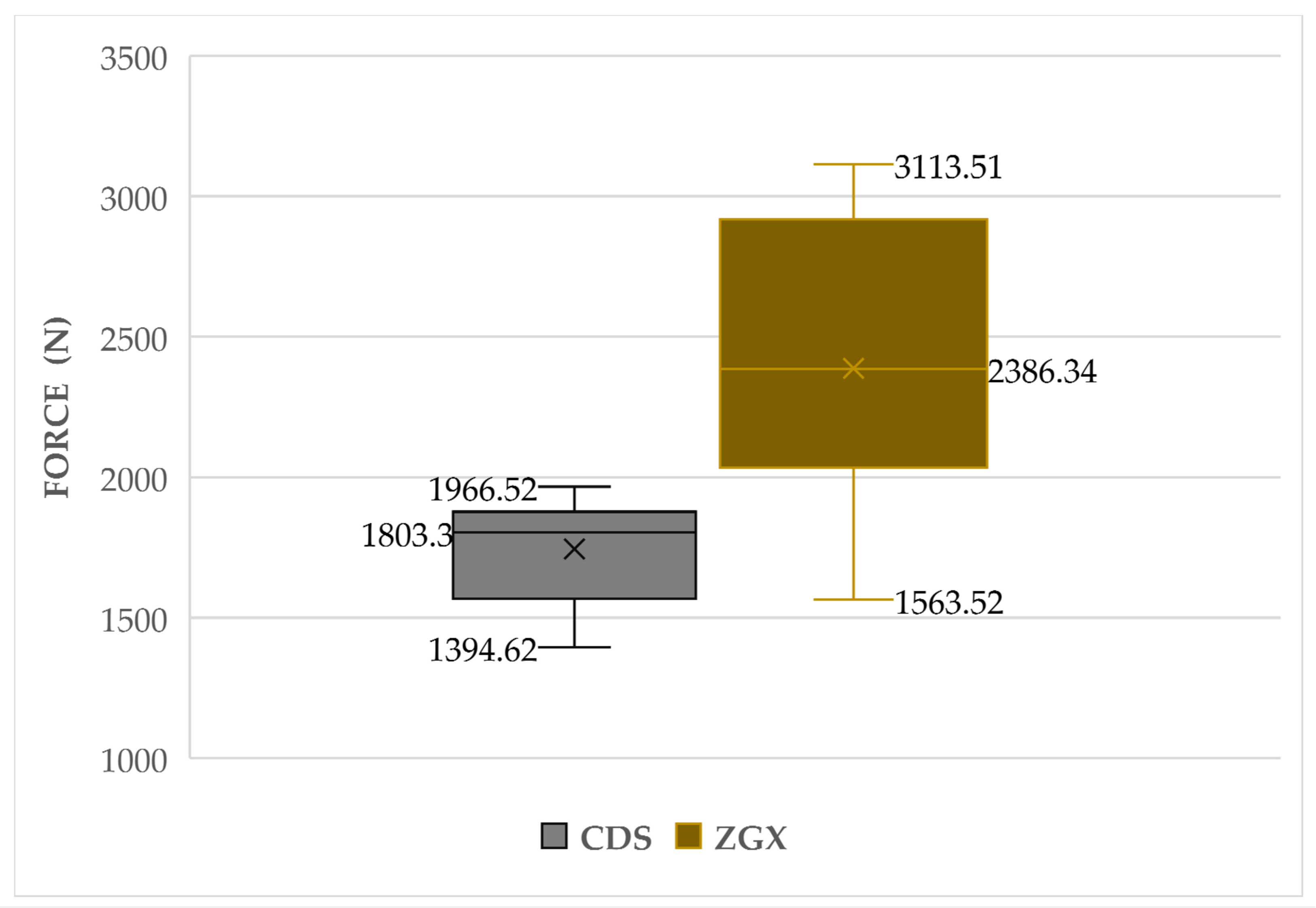
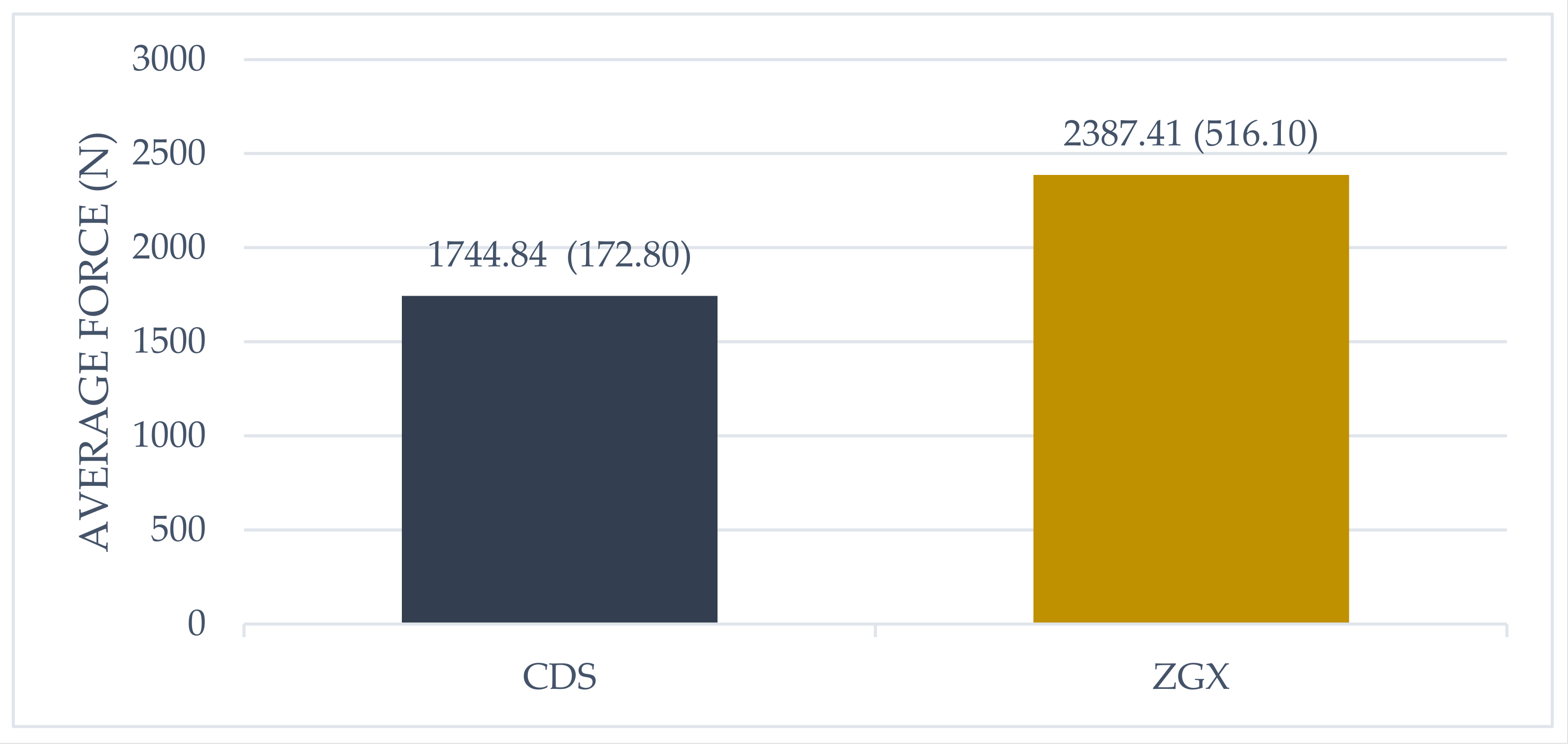
3.1. Descriptive Analysis
3.2. Inferential Analysis
4. Discussion
5. Conclusions
- -
- Although it was found that the ZGX material obtained higher fracture resistance compared with the CDS; the crown fracture loads of the two materials were in the acceptable range.
- -
- The monolithic zirconia CAD-CAM zirconia crowns showed sufficient fracture resistance when used in posterior molar and premolar zones with either material, as they withstood fracture loads greater than the maximum masticatory force.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spitznagel, F.A.; Boldt, J.; Gierthmuehlen, P.C. CAD/CAM Ceramic Restorative Materials for Natural Teeth. J. Dent. Res. 2018, 97, 1082–1091. [Google Scholar] [CrossRef] [PubMed]
- Mörmann, W.H. The evolution of the CEREC system. J. Am. Dent. Assoc. 2006, 137, 7S–13S. [Google Scholar] [CrossRef] [PubMed]
- Luthardt, R.G.; Sandkuhl, O.; Reitz, B. Zirconia-TZP and alumina--advanced technologies for the manufacturing of single crowns. Eur. J. Prosthodont. Restor. Dent. 1999, 7, 113–119. [Google Scholar]
- Stawarczyk, B.; Keul, C.; Eichberger, M.; Figge, D.; Edelhoff, D.; Lümkemann, N. Three generations of zirconia: From veneered to monolithic. Part I. Quintessence Int. 2017, 48, 369–380. [Google Scholar] [CrossRef] [PubMed]
- Čokić, S.M.; Cóndor, M.; Vleugels, J.; Meerbeek, B.V.; Oosterwyck, H.V.; Inokoshi, M.; Zhang, F. Mechanical properties-translucency-microstructure relationships in commercial monolayer and multilayer monolithic zirconia ceramics. Dent. Mater. 2022, 38, 797–810. [Google Scholar] [CrossRef]
- Özkurt-Kayahan, Z. Monolithic zirconia: A review of the literature. Biomed. Res. 2016, 27, 1427–1436. [Google Scholar]
- Stawarczyk, B.; Keul, C.; Eichberger, M.; Figge, D.; Edelhoff, D.; Lümkemann, N. Three generations of zirconia: From veneered to monolithic. Part II. Quintessence Int. 2017, 48, 441–450. [Google Scholar] [CrossRef]
- Güth, J.F.; Stawarczyk, B.; Edelhoff, D.; Liebermann, A. Zirconia and its novel compositions: What do clinicians need to know? Quintessence Int. 2019, 50, 512–520. [Google Scholar] [CrossRef]
- Ghodsi, S.; Jafarian, Z. A Review on Translucent Zirconia. Eur. J. Prosthodont. Restor. Dent. 2018, 26, 62–74. [Google Scholar] [CrossRef]
- Zhang, Y.; Lawn, B.R. Novel Zirconia Materials in Dentistry. J. Dent. Res. 2018, 97, 140–147. [Google Scholar] [CrossRef]
- Kwon, S.J.; Lawson, N.C.; McLaren, E.E.; Nejat, A.H.; Burgess, J.O. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J. Prosthet. Dent. 2018, 120, 132–137. [Google Scholar] [CrossRef]
- Rinke, S.; Metzger, A.; Ziebolz, H. Multilayer Super-Translucent Zirconia for Chairside Fabrication of a Monolithic Posterior Crown. Case Rep. Dent. 2022, 2022, 4474227. [Google Scholar] [CrossRef]
- Lan, T.H.; Chen, Y.F.; Wang, Y.Y.; Chou, M.M.C. Evaluation of the Feasibility of NaCaPO4-Blended Zirconia as a New CAD/CAM Material for Dental Restoration. Materials 2021, 14, 3819. [Google Scholar] [CrossRef] [PubMed]
- Flinn, B.D.; Raigrodski, A.J.; Mancl, L.A.; Toivola, R.; Kuykendall, T. Influence of aging on flexural strength of translucent zirconia for monolithic restorations. J. Prosthet. Dent. 2017, 117, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Alghazzawi, T.F. The effect of extended aging on the optical properties of different zirconia materials. J. Prosthodont. Res. 2017, 61, 305–314. [Google Scholar] [CrossRef]
- Silva, L.H.D.; Lima, E.; Miranda, R.B.P.; Favero, S.S.; Lohbauer, U.; Cesar, P.F. Dental ceramics: A review of new materials and processing methods. Braz. Oral Res. 2017, 31 (Suppl. S1), e58. [Google Scholar] [CrossRef]
- Lameira, D.P.; Buarque e Silva, W.A.; Andrade e Silva, F.; De Souza, G.M. Fracture Strength of Aged Monolithic and Bilayer Zirconia-Based Crowns. Biomed. Res. Int. 2015, 2015, 418641. [Google Scholar] [CrossRef]
- Johansson, C.; Kmet, G.; Rivera, J.; Larsson, C.; Vult Von Steyern, P. Fracture strength of monolithic all-ceramic crowns made of high translucent yttrium oxide-stabilized zirconium dioxide compared to porcelain-veneered crowns and lithium disilicate crowns. Acta Odontol. Scand. 2014, 72, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Jansen, J.U.; Lümkemann, N.; Letz, I.; Pfefferle, R.; Sener, B.; Stawarczyk, B. Impact of high-speed sintering on translucency, phase content, grain sizes, and flexural strength of 3Y-TZP and 4Y-TZP zirconia materials. J. Prosthet. Dent. 2019, 122, 396–403. [Google Scholar] [CrossRef]
- Ahmed, W.M.; Troczynski, T.; McCullagh, A.P.; Wyatt, C.C.L.; Carvalho, R.M. The influence of altering sintering protocols on the optical and mechanical properties of zirconia: A review. J. Esthet. Restor. Dent. 2019, 31, 423–430. [Google Scholar] [CrossRef]
- Kolakarnprasert, N.; Kaizer, M.R.; Kim, D.K.; Zhang, Y. New multi-layered zirconias: Composition, microstructure and translucency. Dent. Mater. 2019, 35, 797–806. [Google Scholar] [CrossRef]
- Cardoso, K.V.; Adabo, G.L.; Mariscal-Muñoz, E.; Antonio, S.G.; Arioli Filho, J.N. Effect of sintering temperature on microstructure, flexural strength, and optical properties of a fully stabilized monolithic zirconia. J. Prosthet. Dent. 2020, 124, 594–598. [Google Scholar] [CrossRef] [PubMed]
- Tabatabaian, F. Color Aspect of Monolithic Zirconia Restorations: A Review of the Literature. J. Prosthodont. 2019, 28, 276–287. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Suarez, C.; Rodriguez, V.; Pelaez, J.; Agustin-Panadero, R.; Suarez, M.J. Comparative fracture behavior of monolithic and veneered zirconia posterior fixed dental prostheses. Dent. Mater. J. 2017, 36, 816–821. [Google Scholar] [CrossRef]
- Sarıkaya, I.; Hayran, Y. Effects of dynamic aging on the wear and fracture strength of monolithic zirconia restorations. BMC Oral Health 2018, 18, 146. [Google Scholar] [CrossRef]
- Habibi, Y.; Dawid, M.T.; Waldecker, M.; Rammelsberg, P.; Bömicke, W. Three-year clinical performance of monolithic and partially veneered zirconia ceramic fixed partial dentures. J. Esthet. Restor. Dent. 2020, 32, 395–402. [Google Scholar] [CrossRef]
- El Shahawy, O.I.; Azab, M.M. Fracture resistance of prefabricated versus custom-made zirconia crowns after thermo-mechanical aging: An in-vitro study. BMC Oral Health 2022, 22, 587. [Google Scholar] [CrossRef]
- Porcelain-Fused-to-Metal Crowns versus All-Ceramic Crowns: A Review of the Clinical and Cost-Effectiveness [Internet]; Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2015.
- Barão, V.A.; Gennari-Filho, H.; Goiato, M.C.; dos Santos, D.M.; Pesqueira, A.A. Factors to achieve aesthetics in all-ceramic restorations. J. Craniofac. Surg. 2010, 21, 2007–2012. [Google Scholar] [CrossRef] [PubMed]
- Harada, K.; Shinya, A.; Gomi, H.; Hatano, Y.; Shinya, A.; Raigrodski, A.J. Effect of accelerated aging on the fracture toughness of zirconias. J. Prosthet. Dent. 2016, 115, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Konstantinidis, I.; Trikka, D.; Gasparatos, S.; Mitsias, M.E. Clinical Outcomes of Monolithic Zirconia Crowns with CAD/CAM Technology. A 1-Year Follow-Up Prospective Clinical Study of 65 Patients. Int. J. Environ. Res. Public Health 2018, 15, 2523. [Google Scholar] [CrossRef]
- Yang, S.W.; Kim, J.E.; Shin, Y.; Shim, J.S.; Kim, J.H. Enamel wear and aging of translucent zirconias: In vitro and clinical studies. J. Prosthet. Dent. 2019, 121, 417–425. [Google Scholar] [CrossRef]
- Candido, L.M.; Miotto, L.N.; Fais, L.; Cesar, P.F.; Pinelli, L. Mechanical and Surface Properties of Monolithic Zirconia. Oper. Dent. 2018, 43, E119–E128. [Google Scholar] [CrossRef]
- Scherrer, S.S.; Lohbauer, U.; Della Bona, A.; Vichi, A.; Tholey, M.J.; Kelly, J.R.; van Noort, R.; Cesar, P.F. ADM guidance-Ceramics: Guidance to the use of fractography in failure analysis of brittle materials. Dent. Mater. 2017, 33, 599–620. [Google Scholar] [CrossRef]
- Kongkiatkamon, S.; Booranasophone, K.; Tongtaksin, A.; Kiatthanakorn, V.; Rokaya, D. Comparison of Fracture Load of the Four Translucent Zirconia Crowns. Molecules 2021, 26, 5308. [Google Scholar] [CrossRef]
- Sorrentino, R.; Triulzio, C.; Tricarico, M.G.; Bonadeo, G.; Gherlone, E.F.; Ferrari, M. In vitro analysis of the fracture resistance of CAD-CAM monolithic zirconia molar crowns with different occlusal thickness. J. Mech. Behav. Biomed. Mater. 2016, 61, 328–333. [Google Scholar] [CrossRef]
- Bulut, A.C.; Atsü, S.S. Occlusal Thickness and Cement-Type Effects on Fracture Resistance of Implant-Supported Posterior Monolithic Zirconia Crowns. Int. J. Oral Maxillofac. Implants 2021, 36, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Tekin, Y.H.; Hayran, Y. Fracture resistance and marginal fit of the zirconia crowns with varied occlusal thickness. J. Adv. Prosthodont. 2020, 12, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Denry, I. How and when does fabrication damage adversely affect the clinical performance of ceramic restorations? Dent. Mater. 2013, 29, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Hallmann, L.; Mehl, A.; Ulmer, P.; Reusser, E.; Stadler, J.; Zenobi, R.; Stawarczyk, B.; Özcan, M.; Hämmerle, C.H. The influence of grain size on low-temperature degradation of dental zirconia. J. Biomed. Mater. Res. B Appl. Biomater. 2012, 100, 447–456. [Google Scholar] [CrossRef]
- Pereira, G.K.R.; Guilardi, L.F.; Dapieve, K.S.; Kleverlaan, C.J.; Rippe, M.P.; Valandro, L.F. Mechanical reliability, fatigue strength and survival analysis of new polycrystalline translucent zirconia ceramics for monolithic restorations. J. Mech. Behav. Biomed. Mater. 2018, 85, 57–65. [Google Scholar] [CrossRef]
- Kim, H.K.; Kim, S.H.; Lee, J.B.; Han, J.S.; Yeo, I.S. Effect of polishing and glazing on the color and spectral distribution of monolithic zirconia. J. Adv. Prosthodont. 2013, 5, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Elisa Kauling, A.; Güth, J.F.; Erdelt, K.; Edelhoff, D.; Keul, C. Influence of speed sintering on the fit and fracture strength of 3-unit monolithic zirconia fixed partial dentures. J. Prosthet. Dent. 2020, 124, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Ordoñez Balladares, A.; Abad-Coronel, C.; Ramos, J.C.; Martín Biedma, B.J. Fracture Resistance of Sintered Monolithic Zirconia Dioxide in Different Thermal Units. Materials 2022, 15, 2478. [Google Scholar] [CrossRef]
- Kaizer, M.R.; Kolakarnprasert, N.; Rodrigues, C.; Chai, H.; Zhang, Y. Probing the interfacial strength of novel multi-layer zirconias. Dent. Mater. 2020, 36, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Giner, S.; Bartolomé, J.F.; Gomez-Cogolludo, P.; Castellote, C.; Pradíes, G. Fatigue fracture resistance of titanium and chairside CAD-CAM zirconia implant abutments supporting zirconia crowns: An in vitro comparative and finite element analysis study. J. Prosthet. Dent. 2021, 125, e1–e503. [Google Scholar] [CrossRef] [PubMed]
- Badawy, R.; El-Mowafy, O.; Tam, L.E. Fracture toughness of chairside CAD/CAM materials—Alternative loading approach for compact tension test. Dent. Mater. 2016, 32, 847–852. [Google Scholar] [CrossRef]
| Materials | Components | % |
|---|---|---|
| CDS | ZrO2 + HfO2 + Y2O3 | ≥94.0% |
| Y2O3 | 5% | |
| Al2O3 | ≤1% | |
| Fe2O3 | ≤0.01% | |
| Other oxides | ≤0.2% | |
| ZGX | ZrO2 + HfO2 + Y2O3 | ≥99.0% |
| Y2O3 | 6–7% | |
| Al2O3 | ≤0.5% | |
| Fe2O3 | ≤0.5% | |
| Other oxides | ≤0.1% |
| CAD/CAM Material | Media (SD) | CI 95% | CV | Minimum | Maximum |
|---|---|---|---|---|---|
| CDS | 1744.84 (172.80) | (1628.75;1860.93) | 9.9% | 1394.60 | 1563.50 |
| ZGX | 2387.41 (516.10) | (2018.23;2756.59) | 21.6% | 1966.50 | 3113.50 |
| CAD/CAM Material | Shapiro–Wilk | Levene | |||
|---|---|---|---|---|---|
| Statistic | gl | p-Value | F | p-Value | |
| CDS | 0.92 | 10 | 0.33 | 7.15 | 0.02 |
| ZGX | 0.95 | 9 | 0.71 | ||
| CAD/CAM Material | Media (DE) | Statistical T-de Student | p-Value |
|---|---|---|---|
| CDS | 1744.84 (172.80) | −3.75 | 0.003 < 0.05 |
| ZGX | 2387.41 (516.10) |
| Materials | Results | |
|---|---|---|
| CDS | Abad C. 1744.84 ± 172.80 N | Kongkiatkamon S. 1987.38 ± 414.88 N |
| ZGX | Abad C. 2387.41 ± 516.10 N | Ottawa 2634 ± 106.20 N |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abad-Coronel, C.; Paladines, Á.; Ulloa, A.L.; Paltán, C.A.; Fajardo, J.I. Comparative Fracture Resistance Analysis of Translucent Monolithic Zirconia Dioxide Milled in a CAD/CAM System. Ceramics 2023, 6, 1179-1190. https://doi.org/10.3390/ceramics6020071
Abad-Coronel C, Paladines Á, Ulloa AL, Paltán CA, Fajardo JI. Comparative Fracture Resistance Analysis of Translucent Monolithic Zirconia Dioxide Milled in a CAD/CAM System. Ceramics. 2023; 6(2):1179-1190. https://doi.org/10.3390/ceramics6020071
Chicago/Turabian StyleAbad-Coronel, Cristian, Ángeles Paladines, Ana Liz Ulloa, César A. Paltán, and Jorge I. Fajardo. 2023. "Comparative Fracture Resistance Analysis of Translucent Monolithic Zirconia Dioxide Milled in a CAD/CAM System" Ceramics 6, no. 2: 1179-1190. https://doi.org/10.3390/ceramics6020071
APA StyleAbad-Coronel, C., Paladines, Á., Ulloa, A. L., Paltán, C. A., & Fajardo, J. I. (2023). Comparative Fracture Resistance Analysis of Translucent Monolithic Zirconia Dioxide Milled in a CAD/CAM System. Ceramics, 6(2), 1179-1190. https://doi.org/10.3390/ceramics6020071










