Benefits from Incorporating Virtual Reality in Pulmonary Rehabilitation of COPD Patients: A Systematic Review and Meta-Analysis
Abstract
Highlights
- VR programs could be used to augment the therapeutic effect of PR in COPD patients.
- VR rehabilitation programs could be used for home based programs as they are safe and feasible.
- Different games and environments offer the ability to tailor the exercise regimen to patients’ needs and ability providing a personalized rehabilitation.
- Gamification features could increase adherence and participation of COPD patients.
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Eligibility Criteria
2.3. Data Extraction and Quality Assessment
2.4. Data Synthesis and Analysis
3. Results
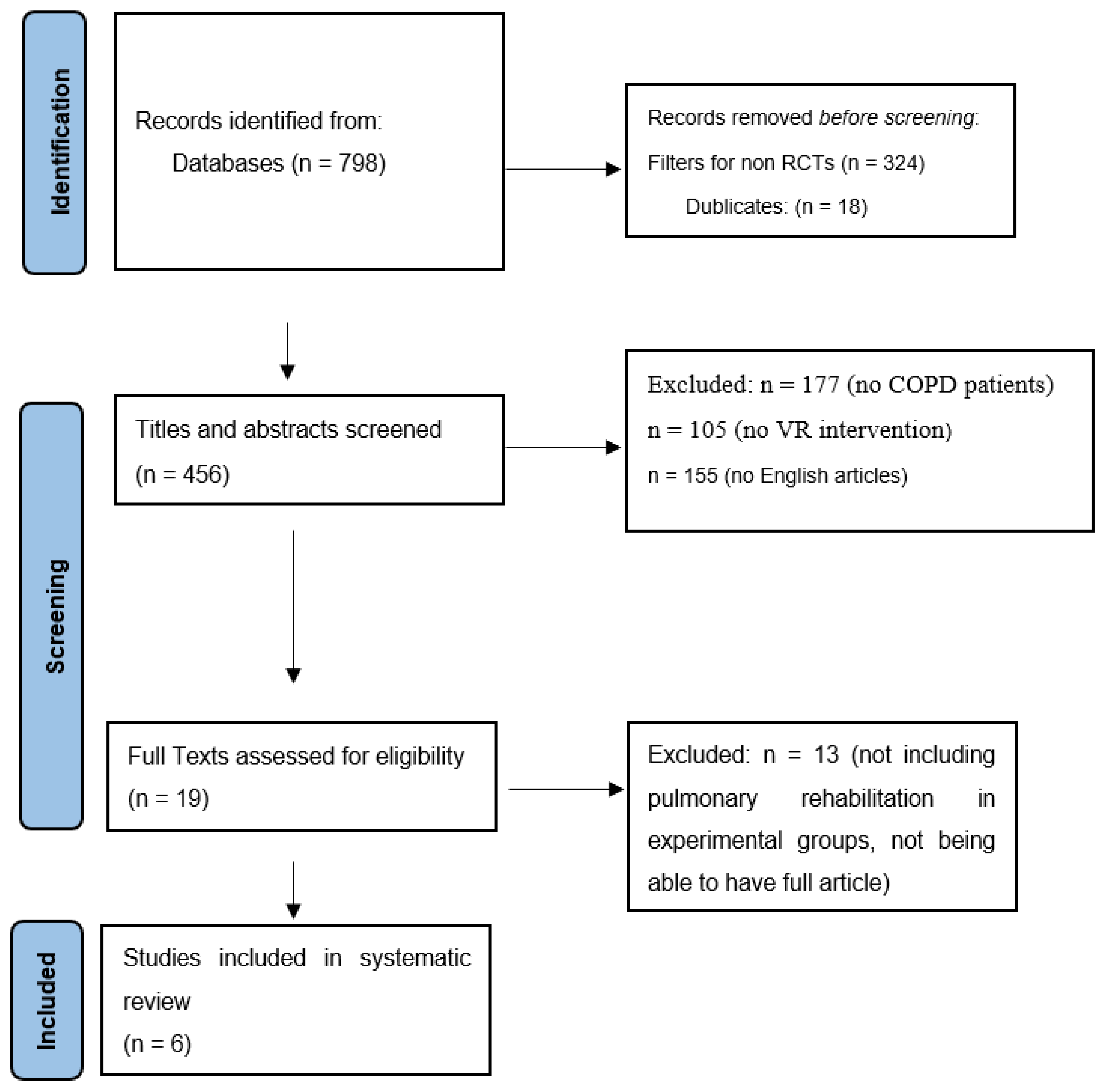
3.1. Identification of Studies
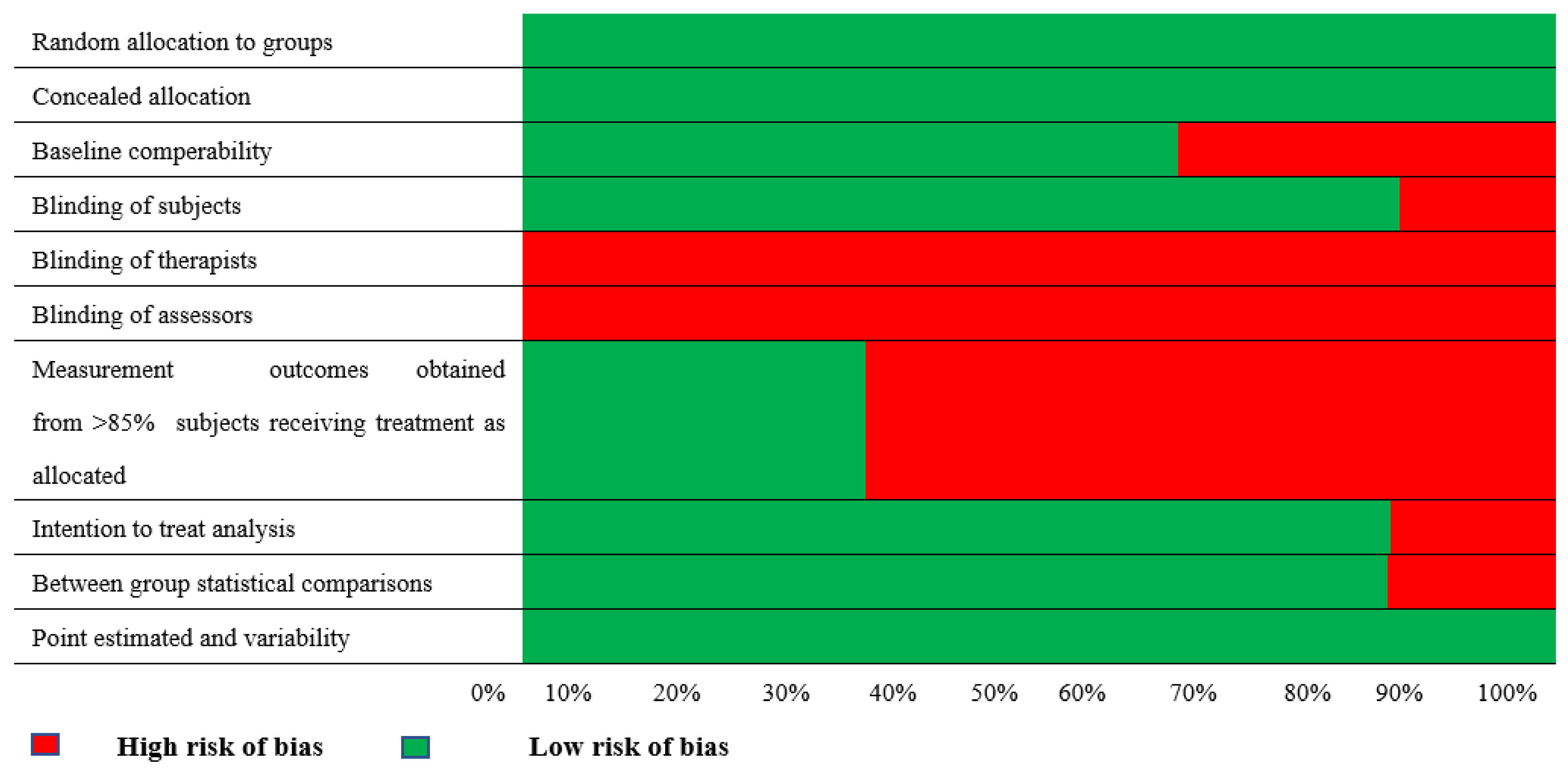
3.2. Methodological Quality
| Criteria Studies | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Score | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mazzoleni et al. (2014) [24] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6/10 | Good |
| Sutanto et al. (2019) [25] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4/10 | Fair |
| Xie et al. (2021) [26] | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6/10 | Good |
| Rutkowski et al. (2019) [27] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7/10 | Good |
| Rutkowski et al. (2020) [28] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/10 | Good |
| Rutkowski et al. (2021) [15] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/10 | Good |
3.3. Description of Studies
3.4. Intervention Comparability
3.5. Effects of Interventions
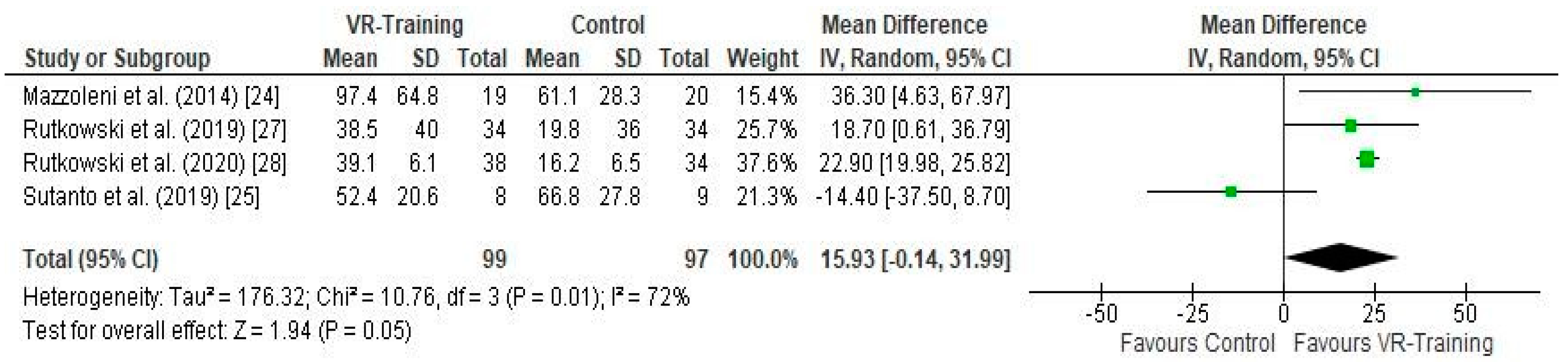
3.5.1. Effect of VR Training on Exercise Capacity (Figure 3)
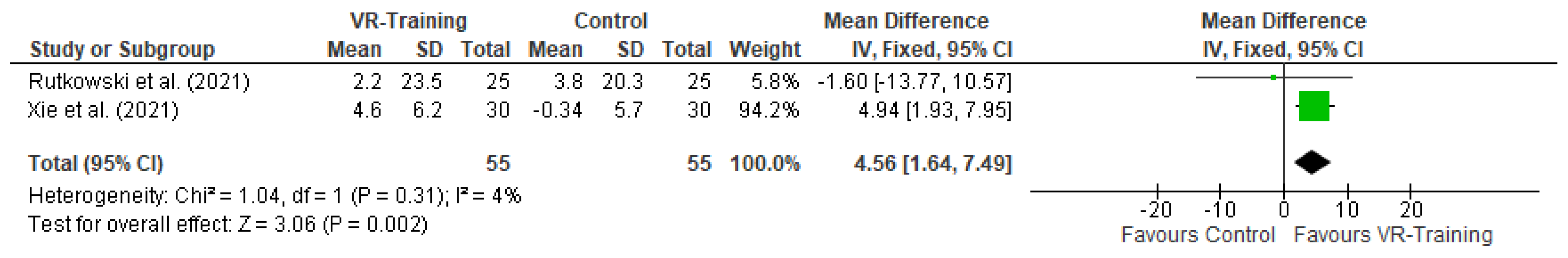
3.5.2. Effect of VR Training on Pulmonary Function (Figure 4)
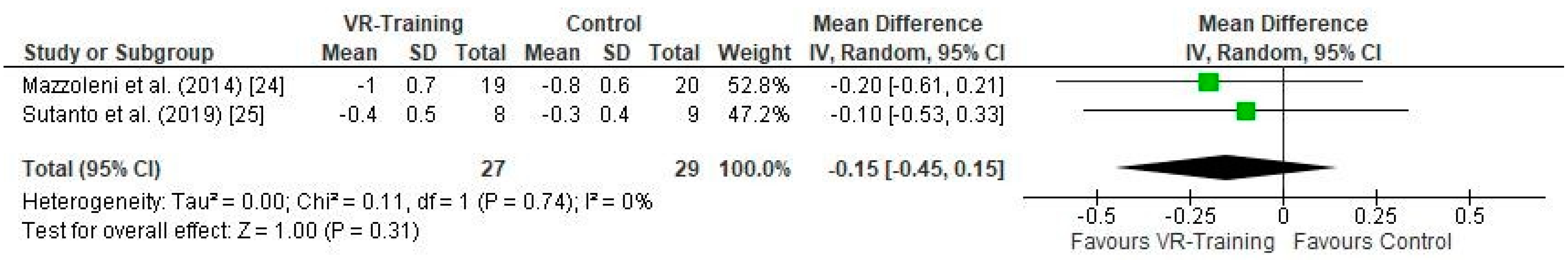
3.5.3. Effect of VR Training on Subjective Dyspnea (Figure 5)
3.5.4. Psychological Status
4. Discussion
5. Future Studies
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Celli, B.R.; Decramer, M.; Wedzicha, J.A.; Wilson, K.C.; Agustí, A.A.; Criner, G.J.; MacNee, W.; Make, B.J.; Rennard, S.I.; Stockley, R.A.; et al. An official American Thoracic Society/European Respiratory Society statement: Research questions in COPD. Eur. Respir. J. 2015, 45, 879–905. [Google Scholar] [CrossRef]
- Hanania, N.A.; O’Donnell, D.E. Activity-related dyspnea in chronic obstructive pulmonary disease: Physical and psychological consequences, unmet needs, and future directions. Int. J. Chron. Obstruct. Pulmon. Dis. 2019, 14, 1127–1138. [Google Scholar] [CrossRef]
- Fazekas-Pongor, V.; Fekete, M.; Balazs, P.; Árva, D.; Pénzes, M.; Tarantini, S.; Urbán, R.; Varga, J.T. Health-related quality of life of COPD patients aged over 40 years. Physiol. Int. 2021, 108, 261–273. [Google Scholar] [CrossRef]
- Safiri, S.; Carson-Chahhoud, K.; Noori, M.; Nejadghaderi, S.A.; Sullman, M.J.M.; Ahmadian Heris, J.; Ansarin, K.; Mansournia, M.A.; Collins, G.S.; Kolahi, A.A.; et al. Burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990–2019: Results from the Global Burden of Disease Study 2019. BMJ 2022, 378, e069679. [Google Scholar] [CrossRef]
- Paneroni, M.; Simonelli, C.; Vitacca, M.; Ambrosino, N. Aerobic Exercise Training in Very Severe Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis. Am. J. Phys. Med. Rehabil. 2017, 96, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Keating, A.; Lee, A.; Holland, A.E. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chronic Respir. Dis. 2011, 8, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Holland, A.E.; Mahal, A.; Hill, C.J.; Lee, A.L.; Burge, A.T.; Cox, N.S.; Moore, R.; Nicolson, C.; O’Halloran, P.; Lahham, A.; et al. Home-based rehabilitation for COPD using minimal resources: A randomised, controlled equivalence trial. Thorax 2017, 72, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Fekete, M.; Fazekas-Pongor, V.; Balazs, P.; Tarantini, S.; Nemeth, A.N.; Varga, J.T. Role of new digital technologies and telemedicine in pulmonary rehabilitation. Wien. Klin. Wochenschr. 2021, 133, 1201–1207. [Google Scholar] [CrossRef]
- Colombo, V.; Aliverti, A.; Sacco, M. Virtual reality for COPD rehabilitation: A technological perspective. Pulmonology 2022, 28, 119–133. [Google Scholar] [CrossRef]
- del Corral, T.; Percegona, J.; Seborga, M.; Rabinovich, R.A.; Vilaró, J. Physiological response during activity programs using Wii-based video games in patients with cystic fibrosis (CF). J. Cyst. Fibros. Off. J. Eur. Cyst. Fibros. Soc. 2014, 13, 706–711. [Google Scholar] [CrossRef]
- Damaševičius, R.; Maskeliūnas, R.; Blažauskas, T. Serious Games and Gamification in Healthcare: A Meta-Review. Information 2023, 14, 105. [Google Scholar] [CrossRef]
- Lavoue, E.; Monterrat, B.; Desmarais, M.; George, S. Adaptive Gamification for Learning Environments. IEEE Trans. Learn. Technol. 2019, 12, 16–28. [Google Scholar] [CrossRef]
- Nor, N.; Sunar, M.; Kapi, A. A Review of Gamification in Virtual Reality (VR) Sport. EAI Endorsed Trans. Creat. Technol. 2020, 6, 163212. [Google Scholar] [CrossRef]
- Nedel, L.; de Souza, V.C.; Menin, A.; Sebben, L.; Oliveira, J.; Faria, F.; Maciel, A. Using Immersive Virtual Reality to Reduce Work Accidents in Developing Countries. IEEE Comput. Graph. Appl. 2016, 36, 36–46. [Google Scholar] [CrossRef]
- Rutkowski, S.; Szczegielniak, J.; Szczepanska-Gieracha, J. Evaluation of the efficacy of immersive virtual reality therapy as a method supporting pulmonary rehabilitation: A randomized controlled trial. J. Clin. Med. 2021, 10, 352. [Google Scholar] [CrossRef] [PubMed]
- Chandrasiri, A.; Collett, J.; Fassbender, E.; de Foe, A. A virtual reality approach to mindfulness skills training. Virtual Real. 2020, 24, 143–149. [Google Scholar] [CrossRef]
- Silva, L.; Maricoto, T.; Costa, P.; Berger-Estilita, J.; Padilha, J.M. A meta-analysis on the structure of pulmonary rehabilitation maintenance programmes on COPD patients’ functional capacity. NPJ Prim. Care Respir. Med. 2022, 32, 38. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Foley, N.C.; Bhogal, S.K.; Teasell, R.W.; Bureau, Y.; Speechley, M.R. Estimates of quality and reliability with the physiotherapy evidence-based database scale to assess the methodology of randomized controlled trials of pharmacological and nonpharmacological interventions. Phys. Ther. 2006, 86, 817–824. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions Version 6.3; updated February 2022; Cochrane: Chichester, UK, 2022; Available online: www.training.cochrane.org/handbook (accessed on 1 January 2022).
- Deeks, J.J.; Higgins, J.P.T.; Altman, D.G. Chapter 10: Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Version 6.3 (updated February 2022); Cochrane: Chichester, UK, 2022. [Google Scholar]
- Moseley, A.M.; Rahman, P.; Wells, G.A.; Zadro, J.R.; Sherrington, C.; Toupin-April, K.; Brosseau, L. Agreement between the Cochrane risk of bias tool and Physiotherapy Evidence Database (PEDro) scale: A meta-epidemiological study of randomized controlled trials of physical therapy interventions. PLoS ONE 2019, 14, e0222770. [Google Scholar] [CrossRef] [PubMed]
- Mazzoleni, S.; Montagnani, G.; Vagheggini, G.; Buono, L.; Moretti, F.; Dario, P.; Ambrosino, N. Interactive videogame as rehabilitation tool of patients with chronic respiratory diseases: Preliminary results of feasibility study. Respir. Med. 2014, 108, 1516–1524. [Google Scholar] [CrossRef]
- Sutanto, Y.S.; Makhabah, D.N.; Aphridasari, J.; Doewes, M.; Suradi; Ambrosino, N. Vidaogames assisted exercise training in patients with chronic obstructive pulmonary disease: A preliminary study. Pulmonology 2019, 25, 275–282. [Google Scholar] [CrossRef]
- Xie, X.; Fan, J.; Chen, H.; Zhu, L.; Wan, T.; Zhou, J.; Fan, D.; Hu, X. Virtual reality technology combined with comprehensive pulmonary rehabilitation on patients with stable chronic obstructive pulmonary disease. J. Healthc. Eng. 2021, 2021, 9987200. [Google Scholar] [CrossRef] [PubMed]
- Rutkowski, S.; Rutkowska, A.; Jastrzębski, D.; Racheniuk, H.; Pawełczyk, W.; Szczegielniak, J. Effect of virtual reality-based rehabilitation on physical fitness in patients with chronic obstructive pulmonary disease. J. Hum. Kinet. 2019, 69, 149–157. [Google Scholar] [CrossRef]
- Rutkowski, S.; Rutkowska, A.; Kiper, P.; Jastrzebski, D.; Racheniuk, H.; Turolla, A.; Szczegielniak, J.; Casaburi, R. Virtual reality rehabilitation in patients with chronic obstructive pulmonary disease: A randomized controlled trial. Int. J. Chron. Obstruct. Pulmon. Dis. 2020, 15, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Patsaki, I.; Dimitriadi, N.; Despoti, A.; Tzoumi, D.; Leventakis, N.; Roussou, G.; Papathanasiou, A.; Nanas, S.; Karatzanos, E. The effectiveness of immersive virtual reality in physical recovery of stroke patients: A systematic review. Front. Syst. Neurosci. 2022, 16, 880447. [Google Scholar] [CrossRef]
- Miller, K.J.; Adair, B.S.; Pearce, A.J.; Said, C.M.; Ozanne, E.; Morris, M.M. Effectiveness and feasibility of virtual reality and gaming system use at home by older adults for enabling physical activity to improve health-related domains: A systematic review. Age Ageing 2014, 43, 188–195. [Google Scholar] [CrossRef]
- Kuys, S.S.; Hall, K.; Peasey, M.; Wood, M.; Cobb, R.; Bell, S.C. Gaming console exercise and cycle or treadmill exercise provide similar cardiovascular demand in adults with cystic fibrosis: A randomised cross-over trial. J. Physiother. 2011, 57, 35–40. [Google Scholar] [CrossRef]
- Spruit, M.A.; Singh, S.J.; Garvey, C.; ZuWallack, R.; Nici, L.; Rochester, C.; Hill, K.; Holland, A.E.; Lareau, S.C.; Man, W.D.; et al. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 2014, 189, 1570. [Google Scholar] [CrossRef]
- LeGear, T.; LeGear, M.; Preradovic, D.; Wilson, G.; Kirkham, A.; Camp, P.G. Does a Nintendo Wii exercise program provide similar exercise demands as a traditional pulmonary rehabilitation program in adults with COPD? Clin. Respir. J. 2016, 10, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Augustine, A.; Bhat, A.; Vaishali, K.; Magazine, R. Barriers to pulmonary rehabilitation—A narrative review and perspectives from a few stakeholders. Lung India 2021, 38, 59–63. [Google Scholar] [PubMed]
- Wang, Y.Q.; Liu, X.; Ma, R.C.; Yin, Y.Y.; Yang, Z.; Cao, H.P.; Xie, J. Active Video Games as an Adjunct to Pulmonary Rehabilitation of Patients with Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis. Am. J. Phys. Med. Rehabil. 2020, 99, 372–380. [Google Scholar] [CrossRef]
- Debigaré, R.; Maltais, F. The major limitation to exercise performance in COPD is lower limb muscle dysfunction. J. Appl. Physiol. 2008, 105, 751–753. [Google Scholar] [CrossRef]
- Jung, T.; Moorhouse, N.; Shi, X.; Amin, M.F. A Virtual Reality-Supported Intervention for Pulmonary Rehabilitation of Patients with Chronic Obstructive Pulmonary Disease: Mixed Methods Study. J. Med. Internet Res. 2020, 22, e14178. [Google Scholar] [CrossRef] [PubMed]
- Ries, A.L.; Kaplan, R.M.; Myers, R.; Prewitt, L.M. Maintenance after pulmonary rehabilitation in chronic lung disease. Am. J. Respir. Crit. Care 2003, 167, 880–888. [Google Scholar] [CrossRef]
- Corhay, J.L.; Dang, D.N.; Van Cauwenberge, H.; Louis, R. Pulmonary rehabilitation and COPD: Providing patients a good environment for optimizing therapy. Int. J. Chron. Obstruct. Pulmon. Dis. 2014, 9, 27–39. [Google Scholar] [CrossRef]
- Spielmanns, M.; Gloeckl, R.; Jarosch, I.; Leitl, D.; Schneeberger, T.; Boeselt, T.; Huber, S.; Kaur-Bollinger, P.; Ulm, B.; Mueller, C.; et al. Using a smartphone application maintains physical activity following pulmonary rehabilitation in patients with COPD: A randomised controlled trial. Thorax 2023, 78, 442–450. [Google Scholar] [CrossRef]
- Kolbe, L.; Jaywant, A.; Gupta, A.; Vanderlind, W.M.; Jabbour, G. Use of virtual reality in the inpatient rehabilitation of COVID-19 patients. Gen. Hosp. Psychiatry 2021, 71, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Wardini, R.; Dajczman, E.; Yang, N.; Baltzan, M.; Préfontaine, D.; Stathatos, M.; Marciano, H.; Watson, S.; Wolkove, N. Using a virtual game system to innovate pulmonary rehabilitation: Safety, adherence and enjoyment in severe chronic obstructive pulmonary disease. Can. Respir. J. 2013, 20, 357–361. [Google Scholar] [CrossRef]
- Parent, A.A.; Gosselin-Boucher, V.; Houle-Peloquin, M.; Poirier, C.; Comtois, A.S. Pilot project: Physiologic responses to a high-intensity active video game with COPD patients-Tools for home rehabilitation. Clin. Respir. J. 2018, 12, 1927–1936. [Google Scholar] [CrossRef] [PubMed]
- Albores, J.; Marolda, C.; Haggerty, M.; Gerstenhaber, B.; ZuWallack, R. The Use of a Home Exercise Program Based on a Computer System in Patients with Chronic Obstructive Pulmonary Disease. J. Cardiopulm. Rehabil. Prev. 2013, 33, 47–52. [Google Scholar] [CrossRef] [PubMed]
| Studies | Sample | Interventions | Control Group | Results |
|---|---|---|---|---|
| Mazzoleni et al. (2014) [24] | 39 CG: 19 EG: 20 | Wii Fit Plus System + PR | PR | 6MWT: EG vs. CG (p = 0.028) MRC dyspnea: EG vs. CG (p = 0.488) SGRQ: EG vs. CG (p = 0.657) BDEI: EG vs. CG (p = 0.724) STAI: EG vs. CG (p = 0.788) |
| Rutkowski et al. (2019) [27] | 68 CG: 34 EG: 34 | Kinect training + PR | PR | 6MWT: CG vs. EG (p > 0.05) |
| Rutkowski et al. (2020) [28] | 106 CG: 34 EG1: 38 EG2: 34 | EG1: Kinect training + PR + Stationary cycle ergometer EG2: Kinect training + PR | PR + Static cycle ergometer | 6MWT: EG1 vs. CG (p = 0.011) EG2 vs. CG (p = 0.031) |
| Rutkowski et al. (2021) [15] | 50 CG: 25 EG: 25 | Immersive VR + PR | PR + Schultz autogenic training | 6MWT: EG vs. CG (d = −0.074) FEV1% pred: EG vs. CG (d = −0.066) HADS: EG vs. CG (d = −1.175) |
| Sutanto et al. (2019) [25] | 23 CG: 11 EG: 12 | Wii Fit System + Cycle Ergometer | Cycle Ergometer | 6MWT: EG vs. CG (p = 0.226) SGRQ: EG vs. CG (p = 0.523) MRC dyspnea: EG vs. CG (p = 0.036) |
| Xie et al. (2021) [26] | 60 CG: 30 EG: 30 | VR + PR | PR | Self efficacy score (p < 0.05) mMRC (p > 0.05) FEV1%pred (p > 0.05) |
| Study | Intervention | Program Duration | Frequency | Session Duration |
|---|---|---|---|---|
| Mazzoleni et al. (2014) [24] |
| 2 weeks PR + 1 week PR and Wii fit plus | Daily | (1) 30 min (2) 1 h |
| Sutanto et al. (2019) [25] |
| 6 weeks | 3 times per week | (1) 30 min (2) 30 min |
| Rutkowski et al. (2019) [27] |
| 2 weeks | 1 time per week | -- |
| Rutkowski et al. (2020) [28] |
| 2 weeks | 5 times per week | (1) 15–30 min each exercise (2) 20 min (3) 20–30 min |
| Rutkowski et al. (2021) [15] |
| 2 weeks | 5 times per week | (1) 15–30 min each exercise (2) 20 min |
| Xie et al. (2021) [26] |
| 8 weeks | -- | (1) 35 min (2) 20 min |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patsaki, I.; Avgeri, V.; Rigoulia, T.; Zekis, T.; Koumantakis, G.A.; Grammatopoulou, E. Benefits from Incorporating Virtual Reality in Pulmonary Rehabilitation of COPD Patients: A Systematic Review and Meta-Analysis. Adv. Respir. Med. 2023, 91, 324-336. https://doi.org/10.3390/arm91040026
Patsaki I, Avgeri V, Rigoulia T, Zekis T, Koumantakis GA, Grammatopoulou E. Benefits from Incorporating Virtual Reality in Pulmonary Rehabilitation of COPD Patients: A Systematic Review and Meta-Analysis. Advances in Respiratory Medicine. 2023; 91(4):324-336. https://doi.org/10.3390/arm91040026
Chicago/Turabian StylePatsaki, Irini, Vasiliki Avgeri, Theodora Rigoulia, Theodoros Zekis, George A. Koumantakis, and Eirini Grammatopoulou. 2023. "Benefits from Incorporating Virtual Reality in Pulmonary Rehabilitation of COPD Patients: A Systematic Review and Meta-Analysis" Advances in Respiratory Medicine 91, no. 4: 324-336. https://doi.org/10.3390/arm91040026
APA StylePatsaki, I., Avgeri, V., Rigoulia, T., Zekis, T., Koumantakis, G. A., & Grammatopoulou, E. (2023). Benefits from Incorporating Virtual Reality in Pulmonary Rehabilitation of COPD Patients: A Systematic Review and Meta-Analysis. Advances in Respiratory Medicine, 91(4), 324-336. https://doi.org/10.3390/arm91040026