Application and Technical Principles of Catheter High-Frequency Jet Ventilation
Abstract
Highlights
- Explanation of potentially optimal techniques for catheter high-frequency jet ventilation (C-HFJV) applications.
- Assessment and clarification of application methodologies of C-HFJV ventilation, its biophysical principles of function, and solutions to prevent volutrauma and barotrauma.
- The positive effects of C-HFJV, even with complications, such as bacterial or viral pneumonia, including COVID-19.
- The method of double-lumen catheter ventilation significantly contributes to clinical practice.
Abstract
1. Introduction
2. High-Frequency Jet Ventilation
- HFPPV (high-frequency positive pressure ventilation)–high-frequency ventilation with positive pressure using a frequency of up to 200 cycles/min;
- HFJV (high-frequency jet ventilation)–high-frequency ventilation using a nozzle to generate a jet stream with a frequency of up to 600 cycles/min;
- HFFI (high-frequency flow interruption)–also known as HFPV (high-frequency percussive ventilation) is characterized by short bursts of gas delivered directly into the ventilator circuit without the injector cannula used in HFJV [5];
- HFO (high-frequency oscillation)–high-frequency ventilation that uses very small tidal volumes often lower than the dead space, with a frequency normally above 400 cycles/min, often reaching as much as 600–900 cycles/min [6].
- (a)
- classic ventilator with a higher breathing frequency (HFPPV);
- (b)
- ventilator with nozzle-type injector and receiving channel (HFJV);
- (c)
- special HF ventilators using piston, bubble, and membrane, to generate oscillation (HFO).
- with an MNJI connected to an endotracheal tube or laryngeal mask, tight or open;
- with a transtracheal needle or catheter;
- with a catheter inserted into the trachea (bronchus) to monitor the airway pressure;
- with a bi-nasal cannula;
- with a face mask.
| Advantages | Disadvantages | |
|---|---|---|
| Physiological | ↓ the peak pressure in airways | Risk of volutrauma and barotrauma |
| ↑ cardiac output | Inspired FiO2 inaccurate | |
| ↓ ADH, fluid retention | Gas exchange efficiency is less predictable in obesity or chronic obstructive pulmonary disease (COPD) | |
| Surgical | Minimal movement of the vocal cords | Possibility of lower airways contamination during ORL surgery |
| Improving access to the surgical field | ||
| Lowering risk during laser surgery | Contamination of expired air with operational debris | |
| Minimizing the excursions of the respiratory system | ||
| Anesthesia | Advantageous during respiratory tract operations and bronchoscopy | Impossibility of inhalation anesthesia |
| Intermittent measurement of ETCO2 | ||
| Useful in emergencies; transtracheal approach | Necessary humidification | |
| Minor gas leak at broncho-pleural fistula surgery | High gas flow | |
| Measured airway pressure inaccurate |
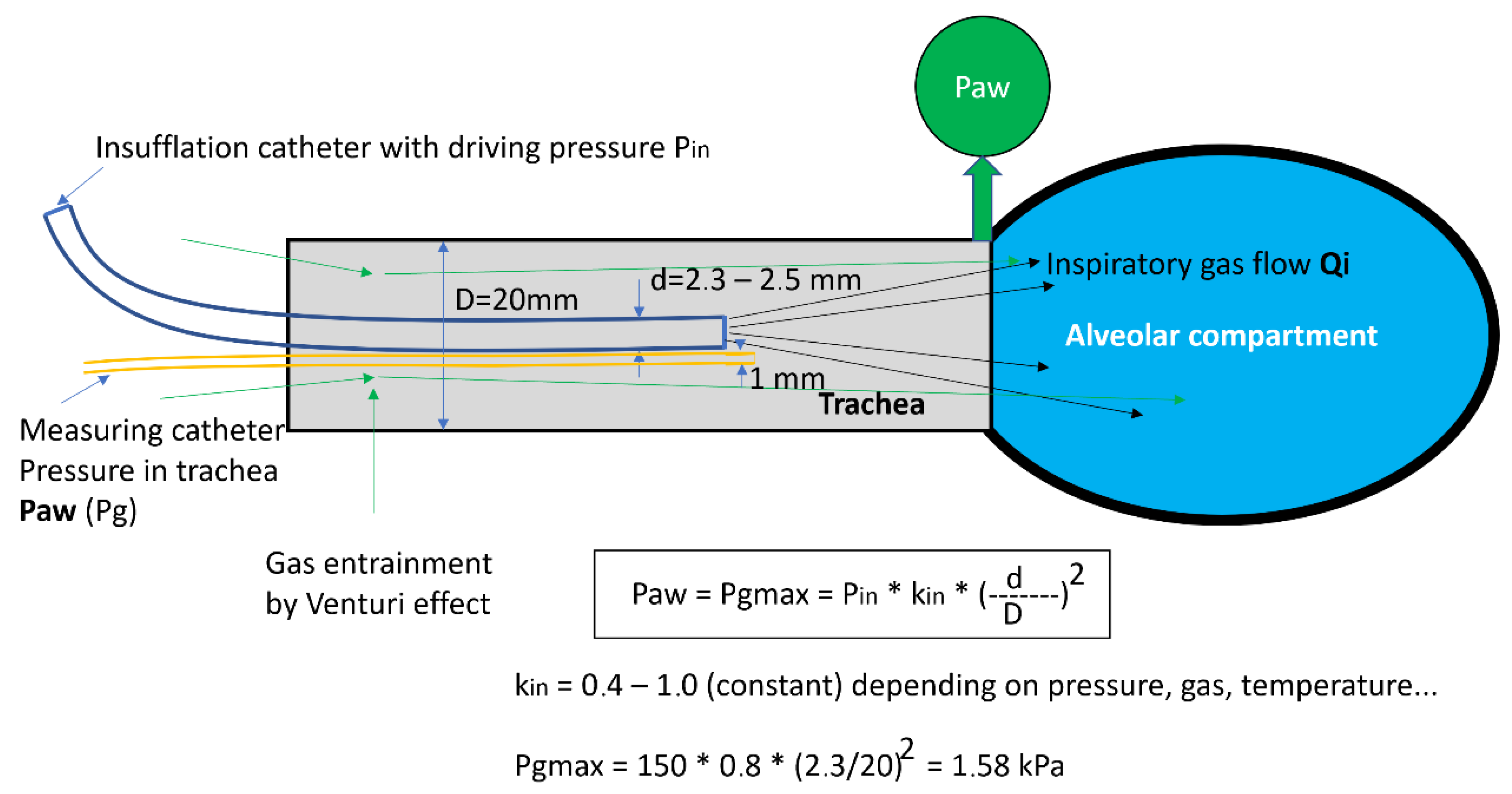
2.1. Basic Physical Principles of HFJV Function
2.2. Catheter form of HFJV with the Original Jet Catheter
2.3. Advantages of Catheter HFJV
- Ensures the adequate exchange of blood gases
- Achieves a free operating field or bronchoscope view
- Prevents aspiration—the Klein effect. Positive pressure in the space under the tip of the catheter and the flow of gases is continuous during expiration and inspiration from the airways to the atmosphere
2.4. Placement of Ventilation Catheter
- (a)
- Supraglottic—during surgery in the area above the vocal cords
- (b)
- Transtracheal (very rare, usually as a life-saving procedure
- (c)
- Subglottic (Figure 4.)—introduced to a depth of 6–8 cm below the vocal cords or 3–4 cm above the carina
2.5. Contraindications for the Use of C-HFJV
2.6. Ventilator Settings
3. Recommendations for the Practice
- The C-HFJV method is safe and preferred by surgeons, even in the case of airway obstruction of various degrees and locations.
- The insufflation catheter must be inserted deep enough (6–7 cm below the vocal cords) and well fixed, usually in the corner of the mouth.
- It is necessary to maintain a sufficient depth of anesthesia and sufficient relaxation to prevent cough and laryngospasm.
- Catheter insertion must take place under visual control, as blind insertion can result in dislocation into the esophagus.
- The position of the catheter should be checked regularly, especially when handling surgical instruments.
- Before the insertion, in the period in which there is no diagnostic or surgical instrument present, it is necessary to ensure the free passage of expired gases by using an airline.
- The catheter must contain a measurement channel for measuring airway pressure, as well as a “total stop” system.
- The methodology requires the cooperation of an experienced anesthesiologist and surgeon.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Paulíková, M. Catheter high-frequency nozzle lung ventilation and its use in ORL surgery/Katétrová vysokofrekvenčná dýzová ventilácia pľúc a jej použitie v ORL chirurgii. Anestéziologia Intenzívna Med. 2017, 6, 46–49. [Google Scholar]
- Klain, M.; Smith, R.B. High frequency percutaneous transtracheal jet ventilation. Crit. Care Med. 1977, 6, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Brychta, O. High Frequency Ventilation Research Final Report; Konštrukta Trenčín: Trenčín, Slovakia, 1985. [Google Scholar]
- Biro, P. Carbon dioxide elimination during high-frequency jet ventilation for rigid bronchoscopy. Br. J. Anaesth. 2000, 84, 635–637. [Google Scholar] [CrossRef] [PubMed]
- Peták, F.; Fodor, G.H.; Schranc, Á.; Südy, R.; Balogh, Á.L.; Babik, B.; Dos Santos Rocha, A.; Bayat, S.; Bizzotto, D.; Dellacà, R.L.; et al. Expiratory High-Frequency Percussive Ventilation: A Novel Concept for Improving Gas Exchange. Respir. Res. 2022, 23, 283. [Google Scholar] [CrossRef] [PubMed]
- Török, P.; Kol, A. Theoretical and Clinical Foundations of High-Frequency Nozzle Ventilation of the Czech-Slovak Type and Methods and Techniques of Artificial Lung Ventilation Derived from It; Osveta: Martin, Slovakia, 2013. [Google Scholar]
- Török, P.; Hermely, A.; Cík, P.; Jakubová, M.; Sopko, I.; Rybár, D.; Saladiak, S.; Doni, V.; Beníkvá, E. Fantoni’s Tracheostomy using Catheter High Frequency Jet Ventilation. Gen. Reanimatol. 2012, 8, 52. [Google Scholar] [CrossRef]
- Sanders, R.D. Two ventilating Attachments for Bronchoscopes. Del. Med. J. 1967, 39, 178–180. [Google Scholar]
- Davies, J.M.; Hillel, A.D.; Maronian, N.C. The Hunsaker Mon-Jet tube with jet ventilation is effective for microlaryngeal surgery. Can. J. Anest. 2009, 56, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Quintel, M.; Marini, J.J. Volutrauma and Atelectrauma: Which Is Worse? Crit. Care 2018, 22, 264. [Google Scholar] [CrossRef] [PubMed]
- Patel, C.; Diba, A. Measuring tracheal airway pressures during transtracheal jet ventilation: An observational study. Anaesthesia 2004, 59, 248–251. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Rubin, J.S. The difficult airway: The use of subglottic jet ventilation for larynge-al surgery. Logoped Phoniatr. Vocol. 2008, 33, 22–24. [Google Scholar] [CrossRef] [PubMed]
- Biro, P. Jet ventilation for surgical interventions in the upper airway. Anesthesiol. Clin. 2010, 28, 397–409. [Google Scholar] [CrossRef] [PubMed]
- Rybár, D. Lactate and its clearance as a marker of shock after cardiac surgery. Anestéziol. Intenzív. Med. 2016, 2, 62–66. [Google Scholar]
- Al Otair, H.A.; BaHammam, A.S. Ventilator- and Interface-Related Factors Influencing Patient-Ventilator Asynchrony during Noninvasive Ventilation. Ann. Thorac. Med. 2020, 15, 1. [Google Scholar] [CrossRef] [PubMed]
- Galmén, K.; Harbut, P.; Freedman, J.; Jakobsson, J.G. The use of high-frequency ventilation during general anaesthesia: An update. F1000Research 2017, 6, 756. [Google Scholar] [CrossRef] [PubMed]
- Alp, E.; Voss, A. Ventilator Associated Pneumonia and Infection Control. Ann. Clin. Microbiol. Antimicrob. 2006, 5, 7. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Musil, P.; Harsanyi, S.; Torok, P.; Paulikova, M.; Moens, D.; Kalas, L.; Kalas, P. Application and Technical Principles of Catheter High-Frequency Jet Ventilation. Adv. Respir. Med. 2023, 91, 278-287. https://doi.org/10.3390/arm91040022
Musil P, Harsanyi S, Torok P, Paulikova M, Moens D, Kalas L, Kalas P. Application and Technical Principles of Catheter High-Frequency Jet Ventilation. Advances in Respiratory Medicine. 2023; 91(4):278-287. https://doi.org/10.3390/arm91040022
Chicago/Turabian StyleMusil, Peter, Stefan Harsanyi, Pavol Torok, Monika Paulikova, Didier Moens, Ladislav Kalas, and Peter Kalas. 2023. "Application and Technical Principles of Catheter High-Frequency Jet Ventilation" Advances in Respiratory Medicine 91, no. 4: 278-287. https://doi.org/10.3390/arm91040022
APA StyleMusil, P., Harsanyi, S., Torok, P., Paulikova, M., Moens, D., Kalas, L., & Kalas, P. (2023). Application and Technical Principles of Catheter High-Frequency Jet Ventilation. Advances in Respiratory Medicine, 91(4), 278-287. https://doi.org/10.3390/arm91040022






