Abstract
This study aimed to develop experimental filler-reinforced resin composites for vat-photopolymerization 3D printing and to evaluate the effects of filler addition on their mechanical, physicochemical, and bonding properties for dental restorative applications. Silanized nano- and/or micro-fillers were incorporated into acrylic resin monomers to formulate photocurable resins suitable for vat-photopolymerization. The rheological behavior of these liquid-state resins was assessed through viscosity measurements. Printed resin composites were fabricated and characterized for mechanical properties—including flexural strength, flexural modulus, and Vickers hardness—both before and after 8 weeks of water immersion. Physicochemical properties, such as water sorption, water solubility, and degree of conversion, were also evaluated. Additionally, shear bond strength to a resin-based luting agent was measured before and after artificial aging via thermocycling. A commercial dental CAD-CAM resin composite served as a reference material. Filler incorporation significantly improved the mechanical properties of the printed composites. The highest performance was observed in the composite containing 60 wt% micro-fillers, with a flexural strength of 168 ± 10 MPa, flexural modulus of 6.3 ± 0.4 GPa, and Vickers hardness of 63 ± 1 VHN, while the commercial CAD-CAM composite showed values of 152 ± 8 MPa, 7.9 ± 0.3 GPa, and 66 ± 2 VHN, respectively. Filler addition did not adversely affect the degree of conversion, although the relatively low conversion led to the elution of unpolymerized monomers and increased water solubility. The shear bond strength of the optimal printed composite remained stable after aging without silanization, demonstrating superior bonding performance compared with the CAD-CAM composite. These findings suggest that the developed 3D-printed resin composite is a promising candidate for dental restorative materials.
1. Introduction
Additive manufacturing (3D printing) has become an essential technology in dentistry, driven by advancements in computer-aided design and computer-aided manufacturing (CAD-CAM) systems [1]. Among the various 3D printing techniques, vat-photopolymerization, including stereolithography (SLA), digital light processing (DLP), and liquid crystal display (LCD), has gained prominence due to its high precision and ability to fabricate complex structures through layer-by-layer polymerization of photocurable resins [2]. Vat-photopolymerization 3D printing has been employed to manufacture both resin-based [3,4,5] and ceramic-based materials [6,7,8] for a wide range of dental applications, including dental models, impression trays, orthodontic appliances (e.g., retainers and aligners), and dental prostheses, such as dentures and fixed partial dentures [9,10,11,12,13,14]. This technology offers several advantages, including reduced material waste, enhanced design flexibility, and improved production efficiency. Recent research has suggested that resin-based materials fabricated using vat-photopolymerization have the potential to achieve accuracy comparable to or even exceeding that of subtractive manufacturing processes used in CAD-CAM systems [15,16,17,18].
Despite these advantages, significant challenges limit the clinical application of vat-photopolymerization 3D-printed dental resins. One of the primary limitations is the restricted variety and composition of resin-based materials available for vat-photopolymerization 3D printing. Contemporary 3D-printed resins often exhibit inferior mechanical and physicochemical properties compared with CAD-CAM resin composite blocks used in subtractive manufacturing [19,20]. This deficiency compromises the durability of 3D-printed fixed partial dentures, making them unsuitable for long-term clinical applications exceeding one year. Consequently, most 3D-printed resins are limited to use in temporary or provisional restorations [21,22], and their use in posterior tooth restorations remains particularly challenging due to the high masticatory forces in these regions. Overcoming these clinical limitations requires further advancements in the mechanical and physicochemical properties of 3D-printed resins to improve their long-term performance in the oral environment [23].
One promising approach to improving the mechanical properties of 3D-printed resins is the incorporation of fillers into the resin matrix [24,25]. Conventional direct and indirect resin-based materials have been reinforced with various inorganic fillers to enhance mechanical properties such as strength, hardness, and wear resistance [26,27]. High filler content has been a key factor in the superior properties of CAD-CAM composites compared with those of conventional composites [28]. While extensive research has been conducted on filler-reinforced composites in conventional resin composites for dental restorative materials, the effects of filler size and content on the mechanical properties of 3D-printed resins remain insufficiently explored.
For dental restorative materials, bonding characteristics also play a crucial role in the long-term clinical success of 3D-printed restorations as well as mechanical properties. A common cause of failure in tooth restorations is the debonding or fracture of restorative materials from the abutment tooth. Fixed partial dentures rely on strong adhesion to the abutment tooth using dental adhesives such as resin-based luting agents [29,30]. Achieving a durable bond is essential to preventing clinical failure, including unintended debonding and catastrophic fractures. Secure bonding between the abutment tooth and the restorative material helps to evenly distribute occlusal forces, thereby reducing stress concentration and enhancing the longevity of restorations [31,32]. The bonding performance of 3D-printed resins is influenced by multiple factors, including surface characteristics and composition. However, the impact of filler addition on the bonding properties of 3D-printed composites remains unclear.
This study aimed to develop novel 3D-printing resins for vat-photopolymerization 3D printing by incorporating fillers and to investigate the effects of filler addition on the mechanical, physicochemical, and bonding properties of printed composites. Amorphous silica fillers of two different sizes—nano-fillers and micro-fillers—were incorporated into an acrylic resin matrix to formulate photocurable resins, which served as printing inks for vat-photopolymerization 3D printing. The printed composites were evaluated for mechanical properties, including flexural strength, flexural modulus, and Vickers hardness, as well as physicochemical properties, such as water sorption, water solubility, and degree of conversion. Their bonding performance with a resin-based luting agent was assessed using a conventional shear bond strength test, both without and with artificial aging. This comprehensive evaluation aimed to demonstrate the potential of 3D-printed composites as viable materials for dental restorations.
2. Materials and Methods
The present experimental procedure is illustrated in Figure 1.
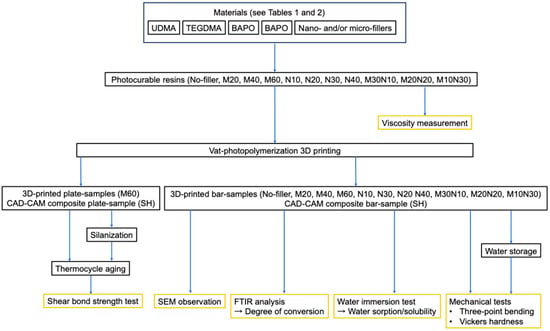
Figure 1.
Schematic flowchart of the experimental procedure. Note that the CAD-CAM composite samples were prepared by cutting from a commercial block, not fabricated by 3D printing.
2.1. Materials
The materials used for preparing the photocurable resin are listed in Table 1. A commercial CAD-CAM composite block (Shofu HC Block, Shofu, Kyoto, Japan) was used as the control sample for each evaluation.

Table 1.
Materials used for the formulation of photocurable resins for vat-photopolymerization 3D printing.
2.2. Preparation of Experimental Photocurable Resin for 3D Printing
Eleven types of experimental photocurable resin were prepared by combining appropriate amounts of resin monomers, silica fillers, and a photoinitiator, as listed in Table 2. Silanized nano-sized and submicron-sized amorphous silica particles were used as fillers for the composites. The compositions of the photocurable resin are shown in Table 2. The upper limits of total filler amounts for micro-fillers, nano-fillers, and mixed fillers were determined based on preliminary experiments. Excessive filler addition led to aggregation in the photocurable resin and significantly increased its viscosity, rendering it unsuitable for 3D printing. Resin monomers were mixed with micro-fillers and/or nano-fillers using a planetary centrifugal mixer (ARE-310, THINKY Corp., Tokyo, Japan) at 2000 rpm for 2 min in the mix mode, followed by centrifugation at 2200 rpm for 1 min in the defoamed mode. Subsequently, a photoinitiator was added to the mixture and mixed again under the same conditions. This preparation process produced a liquid-state photocurable resin for vat-photopolymerization 3D printing.

Table 2.
Chemical composition of the photocurable resins used for vat-photopolymerization 3D printing. Total filler (wt%) represents the weight percentage of fillers relative to the total weight of resin and fillers combined.
2.3. Viscosity Measurement for the Photocurable Resin
The viscosity of each photocurable resin was measured using a B-type viscometer (ROTAVISC me-vi Complete, IKA-Werke GmbH & Co. KG, Staufen, Germany). Viscosity measurements were conducted at seven different temperatures ranging from 10 °C to 40 °C at 5 °C intervals.
2.4. Data Fabrication for 3D Printing
Standard triangulated language (STL) data for 3D printing were created using Fusion 360 (Tinkercad, Autodesk Inc., San Francisco, CA, USA). A bar-shaped design (14.5 × 4.5 × 1.3 mm) was used for flexural strength, flexural modulus, Vickers hardness, water sorption, water solubility, SEM evaluation, and degree of conversion tests. A plate-shaped design (14.5 × 14.5 × 1.3 mm) was used for shear bond strength test samples. The STL files were processed using CHITUBOX Basic V2.1.0 (CBD-Tech, Shenzhen, China) to generate slice model data for 3D printing.
2.5. Vat-Photopolymerization 3D Printing
A commercial liquid crystal display (LCD) 3D printer (Spark Maker, WOW Innovation, Shenzhen, China) equipped with a UV-LED (400–410 nm, 24 W intensity) was used for vat photopolymerization 3D printing. The printing parameters included a layer thickness of 50 µm and a light irradiation time of 10 s per layer. The printed samples were ultrasonically cleaned in isopropanol for 5 min to remove unpolymerized resin. Post-curing was performed using a laboratory light-curing unit (α Light II N, J. Morita, Tokyo, Japan) for 5 min per side. The post-cured samples were sequentially polished using silicon carbide papers (#400 to #2000), followed by ultrasonic cleaning in deionized water for 5 min. The experimental conditions for 3D printing and post-curing were determined based on preliminary experiments conducted in our laboratory. Bar samples were finalized with dimensions of 14.0 ± 0.2 × 4.0 ± 0.2 × 1.2 ± 0.2 mm, confirmed with a digital vernier caliper, and chamfered along the edges (0.2–0.3 mm) to reduce edge failure. Similarly, plate samples were prepared to final dimensions of 14.0 ± 0.2 × 14.0 ± 0.2 × 1.0 ± 0.2 mm. The CAD-CAM composite blocks were cut and polished following the same procedure for comparison.
2.6. SEM Observation
The samples were mounted on aluminum stubs and sputter-coated with platinum. Surface morphology was examined using field-emission scanning electron microscopy (FE-SEM; S-4300, Hitachi High-Tech Corp., Tokyo, Japan) at 5000× magnification with an accelerating voltage of 10 kV.
2.7. Three-Point Bending Test
Bar samples were either aged by immersion in distilled water at 37 °C for two months before the three-point bending test or tested immediately without aging. Both aged and unaged samples were evaluated for flexural strength and flexural modulus following ISO 6872:2024 [33]. The three-point bending test was performed using a jig with a supporting span of 12 mm and a crosshead speed of 1 mm/min on a universal testing machine (AG-X, Shimadzu Corp., Kyoto, Japan). The flexural strength (σ) was calculated in megapascals (MPa), and the flexural modulus (E) was calculated in gigapascals (GPa) using the following equations:
where F is the maximum load, L is the supporting span, b is the width of the sample, h is the thickness of the sample, and m is the gradient of the initial linear portion of the load–deflection curve.
σ = (3FL)/(2bh2)
E = (mL3)/(4bh3)
2.8. Vickers Hardness Test
Following the three-point bending test, the fractured samples were utilized for hardness evaluation. The micro-Vickers hardness was measured using a micro-Vickers hardness tester (HMV-G, Shimadzu Corp., Kyoto, Japan) by applying a 200 g load for 15 s. The measurements followed the standard procedures outlined in ISO 6872:2024.
2.9. Water Sorption/Water Solubility Test
The physicochemical properties of the samples were assessed using water sorption and solubility tests. Before testing, the dimensions of each bar sample were individually measured to calculate the sample volume (V). The samples were then dehydrated in a desiccator until they reached a constant weight, recorded as S0. Subsequently, the samples were immersed in deionized water and stored in an incubator at 37 °C for eight weeks. After water storage, the sample weight was recorded as S1. The samples were then returned to the desiccator until their weight stabilized, recorded as S2. Water sorption (WS) and water solubility (WL) were calculated using the following equations:
where V is the sample volume.
WS = (S1 − S2)/V
WL = (S0 − S1)/V
2.10. Degree of Conversion
Fourier-transform infrared spectroscopy (FTIR) analysis was performed on both unpolymerized photocurable resin and the printed composite after post-polymerization using an IRSpirit spectrometer (Shimadzu Corp., Kyoto, Japan). The degree of conversion was determined by measuring the absorption intensities of the characteristic functional groups: the C = C band at 1637 cm−1 and the C = O band at 1720 cm−1. The degree of conversion was calculated using the following equation [34,35]:
Degree of conversion (%) =
where A(C = C) and A(C = O) are the respective band intensities before and after polymerization.
(1 − [A(C = C)/A(C = O)]before polymerization/[A(C = C)/A(C = O)]after polymerization) × 100
2.11. Shear Bond Strength Test
The shear bond strength (SBS) between the sample and a commercial dental resin-based luting agent (ResiCem-Opaque, Shofu Inc., Kyoto, Japan) was evaluated using a standardized SBS test protocol [36]. The plate samples were embedded in acrylic rings using a self-cured acrylic resin. A commercial porcelain primer (Shofu Inc., Kyoto, Japan) containing a silane coupling agent was either applied to the sample surface or omitted, then dried with compressed air. The luting agent was then loaded onto the sample surface through a Teflon tube (inner diameter: 5 mm) and light-cured for 10 s using a handheld curing unit, followed by additional polymerization with the laboratory curing unit for 5 min. The samples were stored in water at 37 °C for 24 h, then subjected to thermocycling (5 °C and 55 °C, 20,000 cycles, 60 s dwell time) or not subjected to thermocycling. The SBS test was performed using a universal testing machine (AGS-H, Shimadzu Corp., Kyoto, Japan) at a crosshead speed of 1.0 mm/min (n = 12). After the SBS test, the fractured sample surface was observed and the failure mode was categorized into three groups; cohesive failure within the sample, adhesive failure at the sample and the luting agent interface, and mixed failure consisting of both cohesive and adhesive failures.
2.12. Statistical Analysis
Statistical analysis was conducted using EZR software version 1.38 (Saitama Medical Center, Jichi Medical University, Saitama, Japan). Multiple comparisons were performed using one-way analysis of variance (ANOVA) followed by Tukey’s post hoc test to determine statistically significant differences between groups (p < 0.05). Pairwise comparisons were performed using Student’s t-test (p < 0.05).
3. Results
3.1. Viscosity of the Photocurable Resins
Figure 2 shows the viscosities of the photocurable resins across a temperature range of 10–40 °C. The viscosity of all resins decreased as the temperature increased. At room temperature (25 °C), which was used for 3D printing, N40 exhibited the highest viscosity (466 mPa∙s), followed by M10N30 (422 mPa∙s), N30 (370 mPa∙s), M20N20 (209 mPa∙s), and N20 (170 mPa∙s). Micro-filler-containing photocurable resins generally demonstrated lower viscosity compared with nano-filler-containing resins. The photocurable resins with micro-filler content ≥ 60 wt%, nano-filler content ≥ 50 wt%, or mixed filler content > 50 wt% had viscosities too high to be measured using the viscometer. Due to their excessive viscosity, these resins could not be processed for 3D printing. As a result, these formulations (M70, N50, M30N20, and M20N30) were excluded from further experiments.
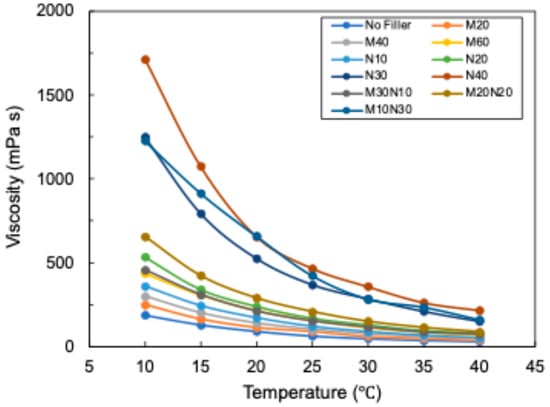
Figure 2.
Viscosity of the photocurable resins with different filler sizes and contents. Photoinitiators were excluded to prevent unintentional curing due to ambient light during the experiment.
3.2. Microstructures
Figure 3 presents SEM images of the printed composites and the commercial CAD-CAM composite (SH), highlighting filler shape, size, density, and distribution. SEM images of micro-filler-containing composites revealed filler sizes ranging from submicron sizes to several microns, whereas nano-filler-containing composites displayed significantly smaller fillers. The commercial CAD-CAM composite contained a variety of filler sizes, from submicron sizes to several microns. All images showed uniformly distributed fillers without observable aggregation across the analyzed areas.
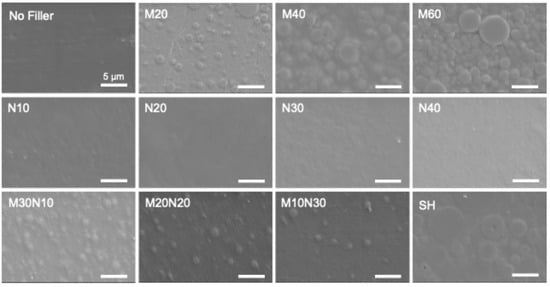
Figure 3.
SEM images of the printed resin composites and the commercial CAD-CAM composite (SH). All scale bars represent 5 µm.
3.3. Mechanical Properties
Figure 4 presents the mechanical properties of the printed composites, including flexural strength, flexural modulus, and Vickers hardness. The results indicate a clear improvement in mechanical properties with increasing filler content. At the same filler percentage, micro-filler-containing resins exhibited mechanical properties comparable to those of nano-filler- and mixed-filler-containing composites. Among the experimental composites, M60 composite demonstrated the best mechanical properties. Compared with the commercial CAD-CAM composite, the M60 composite exhibited a significantly higher flexural strength (168 ± 10 MPa vs. 152 ± 8 MPa). However, its flexural modulus (6.4 ± 0.4 GPa) and Vickers hardness (63 ± 1 VHN) were significantly lower than those of the CAD-CAM composite (7.9 ± 0.3 GPa and 66 ± 2 VHN, respectively). Following eight weeks of water storage, the mechanical properties of all examined samples decreased, indicating the influence of aging on material performance.
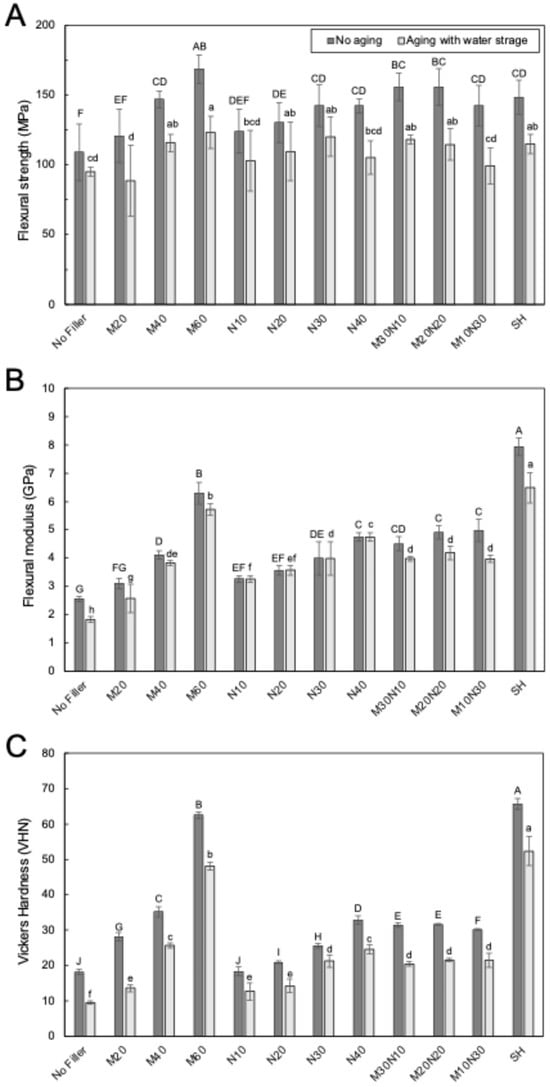
Figure 4.
Mechanical properties of the printed resin composites and the commercial CAD-CAM composite (SH); (A) Flexural strength, (B) Flexural modulus, and (C) Vickers hardness. Different uppercase letters in the figures indicate significant differences between groups under the no-aging condition, while different lowercase letters denote significant differences after 8 weeks of water storage aging (p < 0.05, Tukey’s test, n = 12).
3.4. Water Sorption/Solubility
Figure 5 illustrates the water sorption and solubility of the samples. Water sorption exhibited an inverse correlation with filler content for both micro-filler- and nano-filler-containing composites (Figure 5A). Among the experimental composites, the M60 composite demonstrated the lowest water sorption (30.7 ± 1.1 µg/mm3), which was significantly lower than that of the CAD-CAM composite (42.6 ± 0.9 µg/mm3). A similar trend was observed for water solubility, which decreased with increasing filler content (Figure 5B). However, the water solubility of the M60 composite (3.9 ± 0.8 µg/mm3) was significantly higher than that of the CAD-CAM composite (1.2 ± 0.9 µg/mm3).
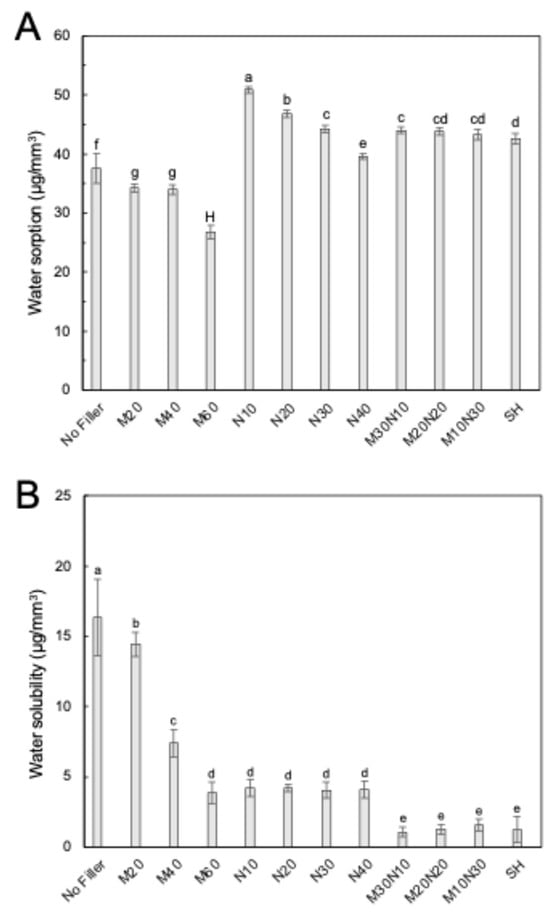
Figure 5.
Physicochemical properties of the printed resin composites and the commercial CAD-CAM composite (SH); (A) Water sorption, (B) Water solubility. Different uppercase and lowercase letters indicate significant differences between groups (p < 0.05, Tukey’s test, n = 12).
Considering the combined results for mechanical properties, water sorption, and water solubility, M60 was identified as the best-performing experimental printed composite. Consequently, further investigations were focused on this formulation.
3.5. Degree of Conversion for the 3D-Printed Composites
Figure 6 compares the degree of conversion between the no-filler resin and the filler-reinforced composite (M60) to assess the impact of filler addition on polymerization behavior. The results indicate no significant difference in the degree of conversion between the no-filler resin (50 ± 4%) and M60 composite (51 ± 2%), suggesting that filler incorporation did not adversely affect the polymerization efficiency of the experimental 3D-printed composite.
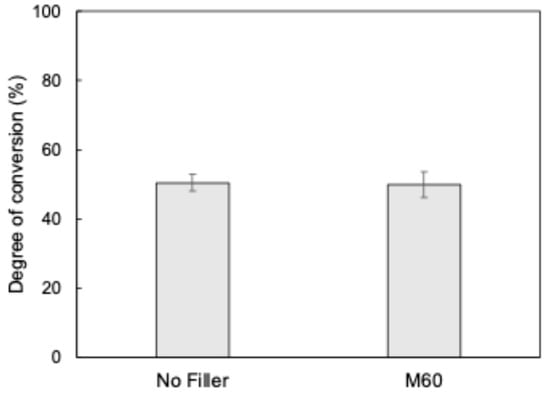
Figure 6.
Degree of conversion for the printed no-filler resin and the printed resin composite containing 60 wt% micro-fillers (M60). No significant difference was observed between the groups (Student’s t-test, p < 0.05, n = 5).
3.6. Shear Bond Strength to Resin-Based Luting Agent
Figure 7 shows the SBS between each sample and the commercial resin-based luting agent. Table 3 summarizes the failure modes observed in the SBS test. The M60 composite exhibited significantly higher SBS values both without and with silanization (59.1 ± 24.4 MPa and 69.4 ± 25.1 MPa, respectively) compared with the CAD-CAM composite (22.4 ± 7.8 MPa and 34.0 ± 10.7 MPa, respectively). Notably, the SBS values of M60 composite, regardless of silanization, remained unaffected by thermocycling-induced aging. In contrast, the SBS values of the CAD-CAM composite significantly decreased following aging, irrespective of the silanization treatment. In terms of failure mode, adhesive failure was predominant in both untreated and silanized CAD-CAM composite samples, whereas cohesive failure was predominant in both untreated and silanized M60 composite samples. This correlation between SBS values and failure modes indicates that the M60 composite possesses superior bonding properties compared with the CAD-CAM composite, suggesting its potential for enhanced long-term adhesion to resin-based luting agents.
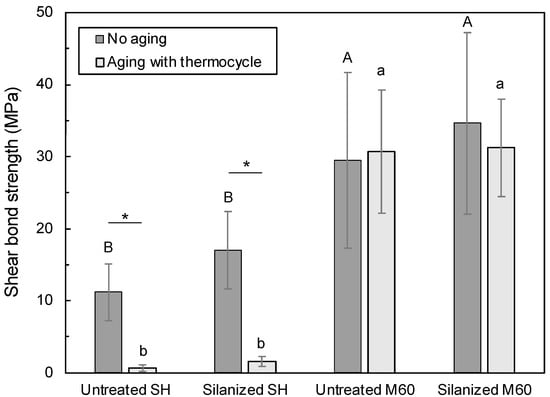
Figure 7.
Shear bond strength between each sample and the commercial resin-based luting agent with/without silanization. Different uppercase and lowercase letters indicate significant differences between groups under no-aging and aging conditions, respectively (p < 0.05, Tukey’s test, n = 12). The asterisk indicates a significant difference between groups with/without aging (p < 0.05, Student’s t-test, n = 12). SH: commercial CAD-CAM composite, M60: the printed resin composite containing 60 wt% micro-fillers.

Table 3.
Failure modes observed in the shear bond strength test. SH: Commercial CAD-CAM composite, M60 composite: Printed resin composite containing 60 wt% micro-fillers. Each group consisted of 12 samples. The failure mode of each sample was categorized as cohesive, mixed, or adhesive, with the respective number of occurrences recorded in the table.
4. Discussion
This study successfully developed filler-reinforced resin composites for vat-photopolymerization 3D printing by incorporating silanized nano-fillers, micro-fillers, or a combination of both. The mechanical and physicochemical properties of the printed composites improved with increasing filler content, reaching optimal performance at 60 wt% micro-filler addition. The optimal composite exhibited mechanical and physicochemical properties similar to those of commercial CAD-CAM composites. Notably, the bonding properties of the printed composite surpassed those of the commercial CAD-CAM composite, highlighting a significant advantage of the printed composite.
Vat-photopolymerization 3D printing constructs structures layer by layer through a repetitive process, involving three key steps: the photocurable resin in the vat is cured onto the platform by light irradiation, uncured resin flows between the platform and vat, and the resin is cured again in this space. The rheological behavior of the photocurable resin plays a crucial role in ensuring successful printing, as it directly influences material flow, layer adhesion, and overall printability. In this study, viscosity measurements were used to characterize the rheological properties of the photocurable resins. All printable resins at 25 °C exhibited viscosities below 500 mPa∙s, which is within the acceptable range for 3D printing and aligns with previously reported values for dental photocurable resins [37,38,39]. The viscosity of the photocurable resin increased with higher filler loading, with nano-fillers causing a more significant increase than micro-fillers due to their strong tendency to aggregate. Consequently, nano-fillers could not be incorporated in as high amounts as micro-fillers without compromising printability. This limitation is primarily attributed to the larger surface area of nano-fillers (20–50 m2/g) compared with micro-fillers (approximately 4–7 m2/g), which leads to greater interparticle interactions and hinders uniform dispersion within the resin matrix. Previous studies on conventional composites have also reported that nano-fillers with large surface areas tend to form aggregates [40,41], making uniform dispersion difficult, even when treated with a silane coupling agent. These findings emphasize the importance of optimizing both filler content and particle size when designing printable composites for vat-photopolymerization 3D printing to achieve the desired balance between viscosity, printability, and mechanical performance.
The mechanical properties of the printed composites improved with increasing filler content, a trend consistent with that in a previous study on conventional dispersed-filler resin composites [42]. Studies have shown that filler incorporation enhances mechanical performance by reinforcing the resin matrix through covalent or hydrogen bonding at the filler–resin interface, facilitated by silane coupling agents [43,44,45]. In the present study, both nano- and micro-fillers were not only dispersed, but also chemically integrated into the resin matrix, contributing to increased strength and durability. The well-incorporated fillers effectively enhanced the mechanical properties, resulting in printed composites with performance comparable to that of the CAD-CAM composite. However, certain commercial high-performance CAD-CAM composites contain over 70 wt% fillers, achieving significantly greater mechanical properties, including flexural strengths exceeding 200 MPa [46,47,48]. These high-strength CAD-CAM composites are particularly well-suited for posterior tooth restorations, where materials must endure substantial occlusal forces [49,50]. In contrast, the printed composites in this study exhibited lower mechanical properties, which may restrict their application in high-load-bearing restorations. To improve the clinical viability of printed composites for molar restorations, further advancements in mechanical performance are necessary, including optimized filler content and enhanced polymer matrix formulations.
The degree of conversion for the printed composite containing 60 wt% micro-fillers was comparable to that of the filler-free printed resin, indicating that filler incorporation did not inhibit polymerization of the resin matrix. This suggests that the irradiated light used for polymerization was able to penetrate the printed resin effectively without significant scattering at the resin matrix–filler interface. The filler composition used in this experiment consisted of amorphous silica, which has a refractive index of 1.46, closely matching that of the resin matrix (UDMA: 1.48, TEGDMA: 1.46). This minimal refractive index mismatch reduced light scattering at the filler–resin interfaces, allowing for efficient light transmission and polymerization. These findings confirm that amorphous silica fillers do not interfere with the curing process of printed composites and suggest that high filler loading can be achieved without compromising polymerization efficiency.
The water solubility of the printed resin indicates that unpolymerized resin monomers were leached from the material during water immersion. This phenomenon is directly related to the degree of conversion, which remained at approximately 50% even after photopolymerization, confirming the presence of residual monomers. Vat-photopolymerization 3D printing relies on layer-by-layer curing using relatively low-intensity and short-duration light irradiation without additional thermal treatment, resulting in a lower degree of conversion despite post-polymerization [37]. In contrast, the commercial CAD-CAM composite undergoes polymerization under controlled factory conditions involving high temperature and pressure, leading to a significantly higher degree of conversion and lower unpolymerized resin content [51]. This difference in polymerization conditions explains why printed resins exhibit higher water solubility than CAD-CAM composites. Although the incorporation of fillers improved the water resistance of the printed composite, its overall performance remained inferior to that of commercial CAD-CAM composites. These findings suggest that printed composites may have limitations in physicochemical stability compared with CAD-CAM composites. To address this issue, future research should focus on optimizing the chemical composition of the matrix resin and refining the polymerization process to enhance the degree of conversion, thereby reducing monomer leaching and improving long-term durability.
The shear bond strengths of the printed composite, both before and after aging, were significantly higher than those of the CAD-CAM composite, indicating superior bonding performance. Moreover, the bond strength of the printed resin remained stable regardless of silanization treatment, suggesting that bonding would occur primarily through covalent interactions between the resin matrix of the luting agent and the printed resin, rather than relying on siloxane bonds. These findings highlight the potential of the printed composites as a significant advancement in bonding performance, offering improved long-term stability without the need for additional surface treatments, such as silanization. The superior bonding properties of the printed resin are likely due to the presence of unpolymerized resin monomers or unreacted C = C bonds, which chemically interact with the resin-based luting agent, forming strong chemical bonds between the printed composite and the luting agent. In contrast, CAD-CAM composites exhibit a high degree of conversion with minimal unpolymerized monomers, leaving little potential for chemical interaction with the luting agents through covalent bonds between resins [52,53,54]. Previous studies on the bonding properties of CAD-CAM composites have shown that silane coupling treatment is necessary to improve bonding by facilitating the formation of siloxane bonds between the fillers in the CAD-CAM composite and the resin in the luting agent [55,56]. However, these siloxane bonds are susceptible to hydrolysis in the presence of water, leading to gradual bond strength degradation over time [57,58]. As a result, the shear bond strength of CAD-CAM composites decreases with aging, whereas the printed composites maintain more stable bonding characteristics.
Previous studies on dental 3D printing resins have largely focused on commercially available materials, investigating their mechanical and physicochemical properties or their clinical outcomes [59,60,61]. However, the influence of filler characteristics such as particle size and loading content on the performance of 3D-printed resin composites remains insufficiently explored. The present study systematically evaluates these parameters using nano-, micro-, and mixed-filler formulations, thereby providing new insights into optimizing material composition for improved clinical performance. The highest flexural strength of the printed composites was approximately 170 MPa, surpassing that of previously reported experimental 3D-printed resins (approximately 100 MPa) [62] and commercial printed resins (approximately 100–130 MPa) [63]. However, the degree of conversion remained lower than those of the printed resins [62,63]. While this lower degree of conversion contributed to enhanced bonding properties, it also raised concerns about the elution of unpolymerized monomers. Residual monomers may affect biocompatibility, potentially leading to allergic reactions or other adverse effects. Reducing the presence of unpolymerized components is essential to ensuring the safety and long-term clinical success of printed composites. Further research is necessary to evaluate the long-term physicochemical stability of printed resins, particularly their color stability in aqueous environments and exposure to common beverages, such as cola and wine. For biocompatibility, previous studies have shown that commercial 3D printing resins release residual monomers, which may cause cytotoxicity in vitro [63,64]. However, clinical data suggest that these materials are well-tolerated in practice [61,65]. The present resin likely shows similar behavior. Nevertheless, future studies will be needed to verify biocompatibility. Additionally, the potential for dental plaque accumulation and bacterial adhesion on printed resin surfaces must be investigated, as these factors could contribute to oral health complications. Assessing these biological properties is crucial for determining the long-term clinical viability of printed composites. To address these challenges, future studies should include both in vitro and in vivo evaluations to optimize material formulations, enhance polymerization efficiency, and improve the biological compatibility of 3D-printed dental resins. By overcoming these limitations, printed composites could evolve into a viable alternative to conventional restorative materials, offering customizable, efficient, and clinically reliable solutions for dental applications.
5. Conclusions
This study aimed to develop 3D-printable composites using filler-reinforced photocurable resins for vat-photopolymerization. The optimal composition (M60) showed a flexural strength of 168 ± 10 MPa, modulus of 6.3 ± 0.4 GPa, and hardness of 63 ± 1 VHN. Compared with the commercial CAD-CAM composite, M60 had a lower modulus and hardness, but superior bonding performance. Future research should focus on optimizing filler shape and resin chemistry to improve clinical durability. These findings support the potential for the long-term use of 3D-printed composites in dental restorations.
Author Contributions
Conceptualization, H.I.; methodology, P.K. and H.I.; software, P.K. and Y.N.; validation, P.K., H.I., and H.S.; formal analysis, Y.N.; investigation, P.K.; writing—original draft preparation, P.K. and H.I.; writing—review and editing, Y.N. and H.S.; visualization, Y.N.; supervision, H.I. and H.S.; project administration, H.I. and H.S.; funding acquisition, H.I. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by JSPS KAKENHI (grant number 23K09236).
Data Availability Statement
Data are contained within article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chaudhary, S.; Avinashi, S.K.; Rao, J.; Gautam, C. Recent Advances in Additive Manufacturing, Applications and Challenges for Dentistry: A Review. ACS Biomater. Sci. Eng. 2023, 9, 3987–4019. [Google Scholar] [CrossRef]
- Andjela, L.; Abdurahmanovich, V.M.; Vladimirovna, S.N.; Mikhailovna, G.I.; Yurievich, D.D.; Alekseevna, M.Y. A review on Vat Photopolymerization 3D-printing processes for dental application. Dent. Mater. 2022, 38, e284–e296. [Google Scholar] [CrossRef]
- Al-Qarni, F.D.; Gad, M.M. Printing Accuracy and Flexural Properties of Different 3D-Printed Denture Base Resins. Materials 2022, 15, 2410. [Google Scholar] [CrossRef]
- Pantea, M.; Ciocoiu, R.C.; Greabu, M.; Ripszky Totan, A.; Imre, M.; Tancu, A.M.C.; Sfeatcu, R.; Spinu, T.C.; Ilinca, R.; Petre, A.E. Compressive and Flexural Strength of 3D-Printed and Conventional Resins Designated for Interim Fixed Dental Prostheses: An In Vitro Comparison. Materials 2022, 15, 3075. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Al-Shahrani, F.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Ateeq, I.S.; Helal, M.A.; Al-Harbi, F.A. Strength and Surface Properties of a 3D-Printed Denture Base Polymer. J. Prosthodont. 2021, 31, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Baysal, N.; Tugba Kalyoncuoglu, U.; Ayyildiz, S. Mechanical Properties and Bond Strength of Additively Manufactured and Milled Dental Zirconia: A Pilot Study. J. Prosthodont. 2022, 31, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Marsico, C.; Carpenter, I.; Kutsch, J.; Fehrenbacher, L.; Arola, D. Additive manufacturing of lithium disilicate glass-ceramic by vat polymerization for dental appliances. Dent. Mater. 2022, 38, 2030–2040. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Jiang, J.; Wang, Y.; Wang, S.; He, Y.; He, F. Additive manufacturing of dental ceramics in prosthodontics: The status quo and the future. J. Prosthodont. Res. 2024, 68, 380–399. [Google Scholar] [CrossRef]
- Xu, Y.; Huettig, F.; Schille, C.; Schweizer, E.; Geis-Gerstorfer, J.; Spintzyk, S. Peel bond strength between 3D printing tray materials and elastomeric impression/adhesive systems: A laboratory study. Dent. Mater. 2020, 36, e241–e254. [Google Scholar] [CrossRef]
- Gad, M.M.; Alghamdi, R.; Al-Ghamdi, R.; Al-Jefri, A.; Akhtar, S.; Khan, S.Q.; Alalawi, H.; Al-Qarni, F.D. Wear and Fracture Resistance of 3D-Printed Denture Teeth: An In Vitro Comparative Study. J. Prosthodont. 2023, 32, 170–177. [Google Scholar] [CrossRef]
- Tartaglia, G.M.; Mapelli, A.; Maspero, C.; Santaniello, T.; Serafin, M.; Farronato, M.; Caprioglio, A. Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials 2021, 14, 1799. [Google Scholar] [CrossRef] [PubMed]
- Karasan, D.; Legaz, J.; Boitelle, P.; Mojon, P.; Fehmer, V.; Sailer, I. Accuracy of Additively Manufactured and Milled Interim 3-Unit Fixed Dental Prostheses. J. Prosthodont. 2022, 31, 58–69. [Google Scholar] [CrossRef] [PubMed]
- Wulff, J.; Schweikl, H.; Rosentritt, M. Cytotoxicity of printed resin-based splint materials. J. Dent. 2022, 120, 104097. [Google Scholar] [CrossRef] [PubMed]
- Al Hamad, K.Q.; Al-Rashdan, B.A.; Ayyad, J.Q.; Al Omrani, L.M.; Sharoh, A.M.; Al Nimri, A.M.; Al-Kaff, F.T. Additive Manufacturing of Dental Ceramics: A Systematic Review and Meta-Analysis. J. Prosthodont. 2022, 31, e67–e86. [Google Scholar] [CrossRef]
- Son, K.; Lee, J.H.; Lee, K.B. Comparison of Intaglio Surface Trueness of Interim Dental Crowns Fabricated with SLA 3D Printing, DLP 3D Printing, and Milling Technologies. Healthcare 2021, 9, 983. [Google Scholar] [CrossRef]
- Mukai, S.; Mukai, E.; Santos-Junior, J.A.; Shibli, J.A.; Faveri, M.; Giro, G. Assessment of the reproducibility and precision of milling and 3D printing surgical guides. BMC Oral Health 2021, 21, 1. [Google Scholar] [CrossRef]
- Kakinuma, H.; Izumita, K.; Yoda, N.; Egusa, H.; Sasaki, K. Comparison of the accuracy of resin-composite crowns fabricated by three-dimensional printing and milling methods. Dent. Mater. J. 2022, 41, 808–815. [Google Scholar] [CrossRef]
- Lim, Y.A.; Kim, J.M.; Choi, Y.; Park, S. Evaluation of Fitness and Accuracy of Milled and Three-Dimensionally Printed Inlays. Eur. J. Dent. 2023, 17, 1029–1036. [Google Scholar] [CrossRef]
- Legaz, J.; Sailer, I.; Mojon, P.; Lee, H.; Karasan, D. Mechanical Properties of Additively Manufactured and Milled Interim 3-Unit Fixed Dental Prostheses. J. Prosthodont. 2023, 32, 234–243. [Google Scholar] [CrossRef]
- Sartori, N.; Sanchez, S.A.; Oliveira, D.; Hosney, S.; Zoidis, P.; Martin, W.; Gonzaga, L.; Rocha, M.G. Flexural properties and fatigue limit of 3D-printed and milled resin-based materials. J. Prosthodont. 2024, 34, 626–634. [Google Scholar] [CrossRef] [PubMed]
- Frasheri, I.; Aumer, K.; Kessler, A.; Miosge, N.; Folwaczny, M. Effects of resin materials dedicated for additive manufacturing of temporary dental restorations on human gingival keratinocytes. J. Esthet. Restor. Dent. 2022, 34, 1105–1112. [Google Scholar] [CrossRef]
- Atria, P.J.; Bordin, D.; Marti, F.; Nayak, V.V.; Conejo, J.; Benalcazar Jalkh, E.; Witek, L.; Sampaio, C.S. 3D-printed resins for provisional dental restorations: Comparison of mechanical and biological properties. J. Esthet. Restor. Dent. 2022, 34, 804–815. [Google Scholar] [CrossRef]
- Pot, G.J.; Van Overschelde, P.A.; Keulemans, F.; Kleverlaan, C.J.; Tribst, J.P.M. Mechanical Properties of Additive-Manufactured Composite-Based Resins for Permanent Indirect Restorations: A Scoping Review. Materials 2024, 17, 3951. [Google Scholar] [CrossRef]
- Rastelli, A.N.; Jacomassi, D.P.; Faloni, A.P.; Queiroz, T.P.; Rojas, S.S.; Bernardi, M.I.; Bagnato, V.S.; Hernandes, A.C. The filler content of the dental composite resins and their influence on different properties. Microsc. Res. Tech. 2012, 75, 758–765. [Google Scholar] [CrossRef]
- Randolph, L.D.; Palin, W.M.; Leloup, G.; Leprince, J.G. Filler characteristics of modern dental resin composites and their influence on physico-mechanical properties. Dent. Mater. 2016, 32, 1586–1599. [Google Scholar] [CrossRef]
- Lohbauer, U.; Belli, R.; Ferracane, J.L. Factors involved in mechanical fatigue degradation of dental resin composites. J. Dent. Res. 2013, 92, 584–591. [Google Scholar] [CrossRef]
- Rodriguez, H.A.; Kriven, W.M.; Casanova, H. Development of mechanical properties in dental resin composite: Effect of filler size and filler aggregation state. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 101, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Ruse, N.D.; Sadoun, M.J. Resin-composite blocks for dental CAD/CAM applications. J. Dent. Res. 2014, 93, 1232–1234. [Google Scholar] [CrossRef] [PubMed]
- Machry, R.V.; Bergoli, C.D.; Schwantz, J.K.; Brondani, L.P.; Pereira-Cenci, T.; Pereira, G.K.R.; Valandro, L.F. Longevity of metal-ceramic single crowns cemented onto resin composite prosthetic cores with self-adhesive resin cement: An update of a prospective analysis with up to 106 months of follow-up. Clin. Oral Investig. 2023, 27, 1071–1078. [Google Scholar] [CrossRef]
- Maletin, A.; Knezevic, M.J.; Koprivica, D.D.; Veljovic, T.; Puskar, T.; Milekic, B.; Ristic, I. Dental Resin-Based Luting Materials-Review. Polymers 2023, 15, 4156. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Wang, R.; Mao, S.; Arola, D.; Zhang, D. Reduction of load-bearing capacity of all-ceramic crowns due to cement aging. J. Mech. Behav. Biomed. Mater. 2013, 17, 56–65. [Google Scholar] [CrossRef]
- da Rosa, L.S.; Velho, H.C.; Tribst, J.P.M.; Valandro, L.F.; Kleverlaan, C.J.; Pereira, G.K.R. Weak adhesion between ceramic and resin cement impairs the load-bearing capacity under fatigue of lithium disilicate glass-ceramic crowns. J. Mech. Behav. Biomed. Mater. 2023, 138, 105604. [Google Scholar] [CrossRef]
- ISO 6872:2024; Dentistry—Ceramic Materials. International Organization for Standardization: Geneva, Switzerland, 2024.
- Viljanen, E.K.; Skrifvars, M.; Vallittu, P.K. Degree of conversion of a copolymer of an experimental monomer and methyl methacrylate for dental applications. J. Appl. Polym. Sci. 2004, 93, 1908–1912. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Gibreel, M.; Garoushi, S.; Vallittu, P.; Lassila, L. Evaluation of flexible three-dimensionally printed occlusal splint materials: An in vitro study. Dent. Mater. 2023, 39, 957–963. [Google Scholar] [CrossRef]
- Yano, H.T.; Ikeda, H.; Nagamatsu, Y.; Masaki, C.; Hosokawa, R.; Shimizu, H. Correlation between microstructure of CAD/CAM composites and the silanization effect on adhesive bonding. J. Mech. Behav. Biomed. Mater. 2020, 101, 103441. [Google Scholar] [CrossRef]
- Lin, C.H.; Lin, Y.M.; Lai, Y.L.; Lee, S.Y. Mechanical properties, accuracy, and cytotoxicity of UV-polymerized 3D printing resins composed of Bis-EMA, UDMA, and TEGDMA. J. Prosthet. Dent. 2020, 123, 349–354. [Google Scholar] [CrossRef]
- Hata, K.; Ikeda, H.; Nagamatsu, Y.; Masaki, C.; Hosokawa, R.; Shimizu, H. Development of dental poly(methyl methacrylate)-based resin for stereolithography additive manufacturing. Polymers 2021, 13, 4435. [Google Scholar] [CrossRef]
- Kim, J.E.; Mangal, U.; Yu, J.H.; Kim, G.T.; Kim, H.; Seo, J.Y.; Cha, J.Y.; Lee, K.J.; Kwon, J.S.; Choi, S.H. Evaluation of the effects of temperature and centrifugation time on elimination of uncured resin from 3D-printed dental aligners. Sci. Rep. 2024, 14, 15206. [Google Scholar] [CrossRef]
- Cassagnau, P. Melt rheology of organoclay and fumed silica nanocomposites. Polymer 2008, 49, 2183–2196. [Google Scholar] [CrossRef]
- Dorigato, A.; Dzenis, Y.; Pegoretti, A. Filler aggregation as a reinforcement mechanism in polymer nanocomposites. Mech. Mater. 2013, 61, 79–90. [Google Scholar] [CrossRef]
- Jun, S.K.; Kim, D.A.; Goo, H.J.; Lee, H.H. Investigation of the correlation between the different mechanical properties of resin composites. Dent. Mater. J. 2013, 32, 48–57. [Google Scholar] [CrossRef]
- Arksornnukit, M.; Takahashi, H.; Nishiyama, N. Effects of silane coupling agent amount on mechanical properties and hydrolytic durability of composite resin after hot water storage. Dent. Mater. J. 2004, 23, 31–36. [Google Scholar] [CrossRef]
- Sideridou, I.D.; Karabela, M.M. Effect of the structure of silane-coupling agent on dynamic mechanical properties of dental resin-nanocomposites. J. Appl. Polym. Sci. 2008, 110, 507–516. [Google Scholar] [CrossRef]
- Aydinoglu, A.; Yoruc, A.B.H. Effects of silane-modified fillers on properties of dental composite resin. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 79, 382–389. [Google Scholar] [CrossRef]
- Ikeda, H.; Nagamatsu, Y.; Shimizu, H. Data on changes in flexural strength and elastic modulus of dental CAD/CAM composites after deterioration tests. Data Brief. 2019, 24, 103889. [Google Scholar] [CrossRef] [PubMed]
- Venturini, A.B.; Dapieve, K.S.; de Kok, P.; Pereira, G.K.R.; Valandro, L.F.; Kleverlaan, C.J. Effect of the region of the CAD/CAM block on the flexural strength and structural reliability of restorative materials. J. Mech. Behav. Biomed. Mater. 2023, 138, 105597. [Google Scholar] [CrossRef]
- Ling, L.; Ma, Y.; Malyala, R. A novel CAD/CAM resin composite block with high mechanical properties. Dent. Mater. 2021, 37, 1150–1155. [Google Scholar] [CrossRef]
- Komine, F.; Honda, J.; Kusaba, K.; Kubochi, K.; Takata, H.; Fujisawa, M. Clinical outcomes of single crown restorations fabricated with resin-based CAD/CAM materials. J. Oral Sci. 2020, 62, 353–355. [Google Scholar] [CrossRef]
- Miura, S.; Fujisawa, M. Current status and perspective of CAD/CAM-produced resin composite crowns: A review of clinical effectiveness. Jpn. Dent. Sci. Rev. 2020, 56, 184–189. [Google Scholar] [CrossRef]
- Bompolaki, D.; Lubisich, E.B.; Fugolin, A.P. Resin-Based Composites for Direct and Indirect Restorations: Clinical Applications, Recent Advances, and Future Trends. Dent. Clin. N. Am. 2022, 66, 517–536. [Google Scholar] [CrossRef]
- Mainjot, A.K.; Dupont, N.M.; Oudkerk, J.C.; Dewael, T.Y.; Sadoun, M.J. From artisanal to CAD-CAM blocks: State of the art of indirect composites. J. Dent. Res. 2016, 95, 487–495. [Google Scholar] [CrossRef]
- Reymus, M.; Roos, M.; Eichberger, M.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Bonding to new CAD/CAM resin composites: Influence of air abrasion and conditioning agents as pretreatment strategy. Clin. Oral Investig. 2019, 23, 529–538. [Google Scholar] [CrossRef]
- Eggmann, F.; Mante, F.K.; Ayub, J.M.; Conejo, J.; Ozer, F.; Blatz, M.B. Influence of universal adhesives and silane coupling primer on bonding performance to CAD-CAM resin-based composites: A laboratory investigation. J. Esthet. Restor. Dent. 2024, 36, 620–631. [Google Scholar] [CrossRef]
- Eldafrawy, M.; Greimers, L.; Bekaert, S.; Gailly, P.; Lenaerts, C.; Nguyen, J.F.; Sadoun, M.; Mainjot, A. Silane influence on bonding to CAD-CAM composites: An interfacial fracture toughness study. Dent. Mater. 2019, 35, 1279–1290. [Google Scholar] [CrossRef]
- Sismanoglu, S.; Yildirim-Bilmez, Z.; Erten-Taysi, A.; Ercal, P. Influence of different surface treatments and universal adhesives on the repair of CAD-CAM composite resins: An in vitro study. J. Prosthet. Dent. 2020, 124, 238.e1–238.e9. [Google Scholar] [CrossRef]
- Komagata, Y.; Nagamatsu, Y.; Ikeda, H. Comparative Bonding Analysis of Computer-Aided Design/Computer-Aided Manufacturing Dental Resin Composites with Various Resin Cements. J. Compos. Sci. 2023, 7, 418. [Google Scholar] [CrossRef]
- Lee, C.; Yamaguchi, S.; Imazato, S. Quantitative evaluation of the degradation amount of the silane coupling layer of CAD/CAM resin composites by water absorption. J. Prosthodont. Res. 2023, 67, 55–61. [Google Scholar] [CrossRef]
- de Castro, E.F.; Nima, G.; Rueggeberg, F.A.; Giannini, M. Effect of build orientation in accuracy, flexural modulus, flexural strength, and microhardness of 3D-Printed resins for provisional restorations. J. Mech. Behav. Biomed. Mater. 2022, 136, 105479. [Google Scholar] [CrossRef]
- Hobbi, P.; Ordueri, T.M.; Ozturk-Bozkurt, F.; Toz-Akalin, T.; Ates, M.; Ozcan, M. 3D-printed resin composite posterior fixed dental prosthesis: A prospective clinical trial up to 1 year. Front. Dent. Med. 2024, 5, 1390600. [Google Scholar] [CrossRef]
- Liang, X.; Yu, B.; Dai, Y.; Wang, Y.; Hu, M.; Zhong, H.J.; He, J. Three-Dimensional Printing Resin-Based Dental Provisional Crowns and Bridges: Recent Progress in Properties, Applications, and Perspectives. Materials 2025, 18, 2022. [Google Scholar] [CrossRef]
- Zattera, A.C.A.; Morganti, F.A.; de Souza Balbinot, G.; Della Bona, A.; Collares, F.M. The influence of filler load in 3D printing resin-based composites. Dent. Mater. 2024, 40, 1041–1046. [Google Scholar] [CrossRef] [PubMed]
- Jin, G.; Gu, H.; Jang, M.; Bayarsaikhan, E.; Lim, J.H.; Shim, J.S.; Lee, K.W.; Kim, J.E. Influence of postwashing process on the elution of residual monomers, degree of conversion, and mechanical properties of a 3D printed crown and bridge materials. Dent. Mater. 2022, 38, 1812–1825. [Google Scholar] [CrossRef]
- Wedekind, L.; Guth, J.F.; Schweiger, J.; Kollmuss, M.; Reichl, F.X.; Edelhoff, D.; Hogg, C. Elution behavior of a 3D-printed, milled and conventional resin-based occlusal splint material. Dent. Mater. 2021, 37, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Anadioti, E.; Odaimi, T.; O’Toole, S. Clinical Applications of 3D-Printed Polymers in Dentistry: A Scoping Review. Int. J. Prosthodont. 2024, 37, 209–219. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).