Applications and Clinical Behavior of BioHPP in Prosthetic Dentistry: A Short Review
Abstract
:1. Introduction
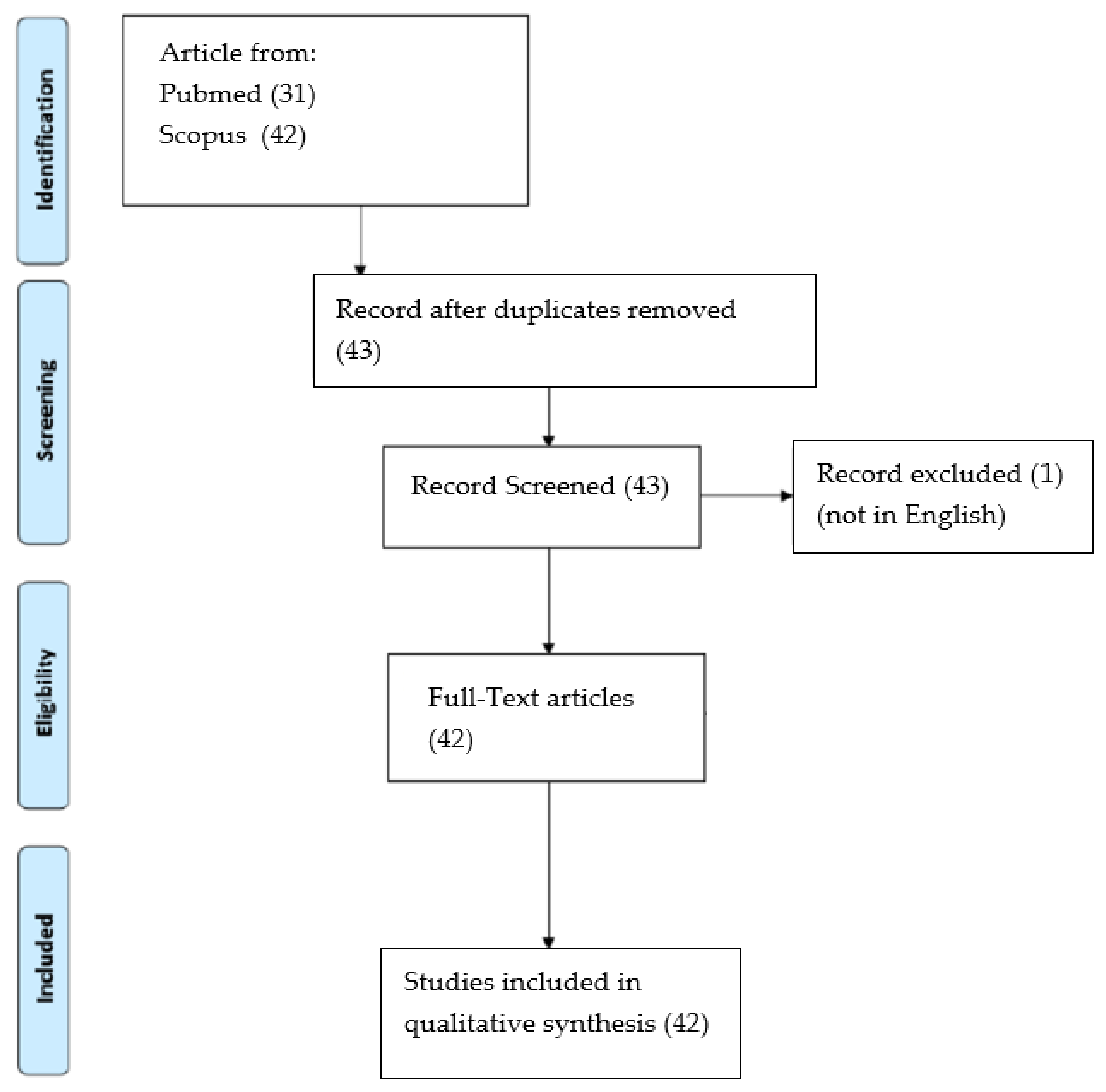
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- single crowns
- endocrowns
- bridges with up to two pontics
- bonded bridges (Maryland bridges)
- superstructures with or without friction elements
- secondary parts in the presence of bars
- individual abutments
- Toronto Bridge
Author Contributions
Funding
Conflicts of Interest
References
- De Bruyn, H.; Raes, S.; Östman, P.-O.; Cosyn, J. Immediate loading in partially and completely edentulous jaws: A review of the literature with clinical guidelines. Periodontology 2000 2014, 66, 153–187. [Google Scholar] [CrossRef] [PubMed]
- Panayotov, I.V.; Orti, V.; Cuisinier, F.; Yachouh, J. Polyetheretherketone (PEEK) for medical applications. J. Mater. Sci. Mater. Med. 2016, 27, 118. [Google Scholar] [CrossRef]
- Zoidis, P.; Papathanasiou, I.; Polyzois, G. The Use of a Modified Poly-Ether-Ether-Ketone (PEEK) as an Alternative Framework Material for Removable Dental Prostheses. A Clinical Report. J. Prosthodont. 2015, 25, 580–584. [Google Scholar] [CrossRef]
- Jin, H.-Y.; Teng, M.-H.; Wang, Z.-J.; Li, X.; Liang, J.-Y.; Wang, W.-X.; Jiang, S.; Zhao, B.-D. Comparative evaluation of BioHPP and titanium as a framework veneered with composite resin for implant-supported fixed dental prostheses. J. Prosthet. Dent. 2019, 122, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Azcarate-Velázquez, F.; Castillo-Oyagüe, R.; Oliveros-López, L.G.; Torres-Lagares, D.; Martínez-González, Á.J.; Pérez-Velasco, A.; Lynch, C.D.; Gutiérrez-Pérez, J.L.; Serrera-Figallo, M.Á. Influence of bone quality on the mechanical interaction between implant and bone: A finite element analysis. J. Dent. 2019, 88, 103161. [Google Scholar] [CrossRef] [PubMed]
- Jovanović, M.; Živić, M.; Milosavljević, M. A Potential Application of Materials Based on a Polymer and CAD/CAM Composite Resins in Prosthetic Dentistry. J. Prosthodont. Res. 2021, 65, 137–147. [Google Scholar] [CrossRef]
- Alhammadi, M.; Al-Mashraqi, A.; Alnami, R.; Ashqar, N.; Alamir, O.; Halboub, E.; Reda, R.; Testarelli, L.; Patil, S. Accuracy and Reproducibility of Facial Measurements of Digital Photographs and Wrapped Cone Beam Computed Tomography (CBCT) Photographs. Diagnostics 2021, 11, 757. [Google Scholar] [CrossRef]
- Perrotti, G.; Baccaglione, G.; Clauser, T.; Scaini, R.; Grassi, R.; Testarelli, L.; Reda, R.; Testori, T.; Del Fabbro, M. Total Face Approach (TFA) 3D Cephalometry and Superimposition in Orthognathic Surgery: Evaluation of the Vertical Dimensions in a Consecutive Series. Methods Protoc. 2021, 4, 36. [Google Scholar] [CrossRef]
- Reda, R.; Zanza, A.; Mazzoni, A.; Cicconetti, A.; Testarelli, L.; Di Nardo, D. An Update of the Possible Applications of Magnetic Resonance Imaging (MRI) in Dentistry: A Literature Review. J. Imaging 2021, 7, 75. [Google Scholar] [CrossRef]
- Patil, S.; Alkahtani, A.; Bhandi, S.; Mashyakhy, M.; Alvarez, M.; Alroomy, R.; Hendi, A.; Varadarajan, S.; Reda, R.; Raj, A.; et al. Ultrasound Imaging versus Radiographs in Differentiating Periapical Lesions: A Systematic Review. Diagnostics 2021, 11, 1208. [Google Scholar] [CrossRef]
- Reda, R.; Zanza, A.; Cicconetti, A.; Bhandi, S.; Miccoli, G.; Gambarini, G.; Di Nardo, D. Ultrasound Imaging in Dentistry: A Literature Overview. J. Imaging 2021, 7, 238. [Google Scholar] [CrossRef] [PubMed]
- Spyropoulos, D.; Kamposiora, P.; Zoidis, P. The Effect of Surface Pretreatment and Water Storage on the Bonding Strength of a Resin Composite Cement to Modified PEEK. Eur. J. Prosthodont. Restor. Dent. 2020, 28, 121–127. [Google Scholar] [PubMed]
- Reda, R.; Zanza, A.; Cicconetti, A.; Bhandi, S.; Guarnieri, R.; Testarelli, L.; Di Nardo, D. A Systematic Review of Cementation Techniques to Minimize Cement Excess in Cement-Retained Implant Restorations. Methods Protoc. 2022, 5, 9. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [Green Version]
- Andrikopoulou, E.; Zoidis, P.; Artopoulou, I.-I.; Doukoudakis, A. Modified PEEK Resin Bonded Fixed Dental Prosthesis for a Young Cleft Lip and Palate Patient. J. Esthet. Restor. Dent. 2016, 28, 201–207. [Google Scholar] [CrossRef]
- Micovic, D.; Mayinger, F.; Bauer, S.; Roos, M.; Eichberger, M.; Stawarczyk, B. Is the high-performance thermoplastic polyetheretherketone indicated as a clasp material for removable dental prostheses? Clin. Oral Investig. 2020, 25, 2859–2866. [Google Scholar] [CrossRef]
- Guo, L.; Smeets, R.; Kluwe, L.; Hartjen, P.; Barbeck, M.; Cacaci, C.; Gosau, M.; Henningsen, A. Cytocompatibility of Titanium, Zirconia and Modified PEEK after Surface Treatment Using UV Light or Non-Thermal Plasma. Int. J. Mol. Sci. 2019, 20, 5596. [Google Scholar] [CrossRef] [Green Version]
- Atsü, S.; Aksan, M.; Bulut, A. Fracture Resistance of Titanium, Zirconia, and Ceramic-Reinforced Polyetheretherketone Implant Abutments Supporting CAD/CAM Monolithic Lithium Disilicate Ceramic Crowns After Aging. Int. J. Oral Maxillofac. Implant. 2019, 34, 622–630. [Google Scholar] [CrossRef]
- Elashmawy, Y.; Elshahawy, W.; Seddik, M.; Aboushelib, M. Influence of fatigue loading on fracture resistance of endodontically treated teeth restored with endocrowns. J. Prosthodont. Res. 2021, 65, 78–85. [Google Scholar] [CrossRef]
- Ramadan, R.; Elsherbeeny, Y.; Ghali, R.; Thabet, Y.; Kandil, B. Retention of a telescopic overdenture on customized abutments after the simulation of 1 year in function. Dent. Med. Probl. 2021, 58, 201–206. [Google Scholar] [CrossRef]
- Ardakani, Z.H.; Giti, R.; Dabiri, S.; Hosseini, A.H.; Moayedi, M. Flexural strength of polymethyl methacrylate reinforced with high-performance polymer and metal mesh. Dent. Res. J. 2021, 18, 30. [Google Scholar]
- Kazi, A.I.; Godil, A.Z.; Wadwan, S.A.; Gandhi, K.Y.; Dugal, R.J.S. Comparative evaluation of marginal and internal fit of endocrowns using lithium disilicate and polyetheretherketone computer-aided design—Computer-aided manufacturing (CAD-CAM) materials: An in vitro study. J. Conserv. Dent. 2021, 24, 198. [Google Scholar] [CrossRef] [PubMed]
- Turksayar, A.A.D.; Hisarbeyli, D.; Kelten, S.; Bulucu, N.B. Wear behavior of current computer-aided design and computer-aided manufacturing composites and reinforced high performance polymers: An in vitro study. J. Esthet. Restor. Dent. 2021. [Google Scholar] [CrossRef]
- Blanch-Martínez, N.; Arias-Herrera, S.; Martínez-González, A. Behavior of polyether-ether-ketone (PEEK) in prostheses on dental implants. A review. J. Clin. Exp. Dent. 2021, 13, e520–e526. [Google Scholar] [CrossRef]
- Reyal, S.S.; Rajamani, V.K.; Gowda, E.M.; Shashidhar, M.P. Comparative prospective clinical evaluation of computer aided design/ computer aided manufacturing milled BioHPP PEEK inlays and Zirconia inlays. J. Indian Prosthodont. Soc. 2021, 21, 240. [Google Scholar] [CrossRef] [PubMed]
- Lalama, M.; Rocha, M.G.; Neill, E.O.; Zoidis, P. Polyetheretherketone (PEEK) Post and Core Restorations: A 3D Accuracy Analysis between Heat-Pressed and CAD-CAM Fabrication Methods. J. Prosthodont. 2021, 1–6. [Google Scholar] [CrossRef]
- Rasheed, M.N.; Sarfaraz, H.; Shetty, S.K.; Prabhu, U.M.; Fernandes, K.; Mohandas, S. Comparison of the bond strength of composite resin to zirconia and composite resin to polyether ether ketone: An in vitro study. J. Pharm. Bioallied Sci. 2020, 12, S504–S509. [Google Scholar] [CrossRef]
- Mayinger, F.; Micovic, D.; Schleich, A.; Roos, M.; Eichberger, M.; Stawarczyk, B. Retention force of polyetheretherketone and cobalt-chrome-molybdenum removable dental prosthesis clasps after artificial aging. Clin. Oral Investig. 2020, 25, 3141–3149. [Google Scholar] [CrossRef]
- Merk, S.; Wagner, C.; Stock, V.; Eichberger, M.; Schmidlin, P.R.; Roos, M.; Stawarczyk, B. Suitability of Secondary PEEK Telescopic Crowns on Zirconia Primary Crowns: The Influence of Fabrication Method and Taper. Materials 2016, 9, 908. [Google Scholar] [CrossRef]
- Abhay, S.S.; Ganapathy, D.; Veeraiyan, D.N.; Ariga, P.; Heboyan, A.; Amornvit, P.; Rokaya, D.; Srimaneepong, V. Wear Resistance, Color Stability and Displacement Resistance of Milled PEEK Crowns Compared to Zirconia Crowns under Stimulated Chewing and High-Performance Aging. Polymers 2021, 13, 3761. [Google Scholar] [CrossRef]
- Porojan, L.; Toma, F.R.; Vasiliu, R.D.; Topală, F.-I.; Porojan, S.D.; Matichescu, A. Optical Properties and Color Stability of Dental PEEK Related to Artificial Ageing and Staining. Polymers 2021, 13, 4102. [Google Scholar] [CrossRef] [PubMed]
- Prechtel, A.; Reymus, M.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Comparison of various 3D printed and milled PAEK materials: Effect of printing direction and artificial aging on Martens parameters. Dent. Mater. 2019, 36, 197–209. [Google Scholar] [CrossRef] [PubMed]
- Preis, V.; Hahnel, S.; Behr, M.; Bein, L.; Rosentritt, M. In-Vitro fatigue and fracture testing of CAD/CAM-materials in implant-supported molar crowns. Dent. Mater. 2017, 33, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Abdelrehim, A.; Abdelhakim, A.; El Dakkak, S. Influence of different materials on retention behavior of CAD-CAM fabricated bar attachments. J. Prosthet. Dent. 2021. [Google Scholar] [CrossRef]
- Stock, V.; Wagner, C.; Merk, S.; Roos, M.; Schmidlin, P.R.; Eichberger, M.; Stawarczyk, B. Retention force of differently fabricated telescopic PEEK crowns with different tapers. Dent. Mater. J. 2016, 35, 594–600. [Google Scholar] [CrossRef] [Green Version]
- Zoidis, P.; Papathanasiou, I. Modified PEEK resin-bonded fixed dental prosthesis as an interim restoration after implant placement. J. Prosthet. Dent. 2016, 116, 637–641. [Google Scholar] [CrossRef]
- Emera, R.M.K.; Abdallah, R.M. Denture base adaptation, retention, and mechanical properties of BioHPP versus nano-alumina-modified polyamide resins. J. Dent. Res. Dent. Clin. Dent. Prospect. 2021, 15, 239–246. [Google Scholar] [CrossRef]
- Omaish, H.H.M.; Abdelhamid, A.M.; Neena, A.F. Comparison of the strain developed around implants with angled abutments with two reinforced polymeric CAD-CAM superstructure materials: An in vitro comparative study. J. Prosthet. Dent. 2022. [Google Scholar] [CrossRef]
- Popa, D.; Constantiniuc, M.; Earar, K.; Mercut, V.; Scrieciu, M.; Buduru, S.; Luca, E.; Negucioiu, M. Review of Different Materials that can be CAD/CAM Processed Description, chemical composition, indications in dentistry areas. Rev. Chim. 2019, 70, 4029–4034. [Google Scholar] [CrossRef]
- Baciu, S.; Berece, C.; Florea, A.; Tonea, A.V.; Lucaciu, O.; Burde, A.V.; Rusnac, M.; Manole, M.; Saceleanu, A.; Mohan, A.; et al. Comparison of Two Evaluating Methods for Establishing the Marginal Fit on Four Heat—Pressed Resin Inlays. Rev. Chim. 2018, 69, 890–893. [Google Scholar] [CrossRef]
- Biris, C.; Bechir, E.S.; Bechir, A.; Mola, F.C.; Badiu, A.V.; Oltean, C.; Andreescu, C.; Gioga, C. Evaluations of Two Reinforced Polymers Used as Metal-FreeSubstructures in Fixed Dental Restoration. Mater. Plast. 2018, 55, 33–37. [Google Scholar] [CrossRef]
- Baciu, S.; Berece, C.; Florea, A.; Burde, A.V.; Munteanu, A.; Cigu, T.A.; Hosszu, T.; Szuhanek, C.; Manole, M.; Sinescu, C. Three-dimensional Marginal Evaluation of Two Pressed Materials Using Micro-CT Technology. Rev. Chim. 2017, 68, 615–618. [Google Scholar] [CrossRef]
- Pacurar, M.; Bechir, E.S.; Suciu, M.; Bechir, A.; Biris, C.I.; Curt-Mola, F.; Cherana, G.; Dascalu, T.I.; Ormenisan, A. The Benefits of Polyether-Ether-Ketone Polymers in Partial Edentulous Patients. Rev. Chim. 2016, 53, 657–660. [Google Scholar]
- Bechir, S.E.; Bechir, A.; Gioga, C.; Manu, R.; Burcea, A.; Dscalu, I.T. The Advantages of BioHPP Polymer as Superstructure Material in Oral Implantology. Rev. Chim. 2016, 53, 394–398. [Google Scholar]
- Di Iorio, E.; Berardini, M. A new material for fixed implant-supported rehabilitations. Dent. Cadmos 2016, 84, 320–325. [Google Scholar] [CrossRef]
- Amer, M.M.; Elsheikh, M.M.; Haleem, M.M.; Ghoraba, S.F.; Salem, A.A. Short-term comparative evaluation of BioHPP and cast cobalt–chromium as framework for implant supported prostheses: A split mouth clinical randomized trial. J. Int. Oral Health 2021, 13, 564–570. [Google Scholar]
- Odeh, E.; Alansary, H.; Naguib, A.; Taymour, M. Evaluation of biocompatibility of veneered Bio HPP and veneered lithium disilicate crowns in anterior zone (Randomized controlled clinical trial). Braz. Dent. Sci. 2021, 24. [Google Scholar] [CrossRef]
- Kwan, J.; Kwan, N. Clinical Application of PEEK as a Provisional Fixed Dental Prosthesis Retained by Reciprocated Guide Surfaces of Healing Abutments During Dental Implant Treatment. Int. J. Oral Maxillofac. Implant. 2021, 36, 581–586. [Google Scholar] [CrossRef]
- Guarnieri, R.; Zanza, A.; D’Angelo, M.; Di Nardo, D.; Del Giudice, A.; Mazzoni, A.; Reda, R.; Testarelli, L. Correlation between Peri-Implant Marginal Bone Loss Progression and Peri-Implant Sulcular Fluid Levels of Metalloproteinase-8. J. Pers. Med. 2022, 12, 58. [Google Scholar] [CrossRef]
- Sadek, S.A. Comparative Study Clarifying the Usage of PEEK as Suitable Material to Be Used as Partial Denture Attachment and Framework. Open Access Maced. J. Med. Sci. 2019, 7, 1193–1197. [Google Scholar] [CrossRef] [Green Version]
- Bolat, M.; Bosinceanu, D.G.; Sandu, I.G.; Bosinceanu, D.N.; Surlari, Z.; Balcos, C.; Solomon, O.; Vitalariu, A. Comparative Study on the Degree of Bacterial Biofilm Formation of Dental Bridges Made from Three Types of Materials. Mater. Plast. 2019, 56, 144–147. [Google Scholar] [CrossRef]
- Guarnieri, R.; Miccoli, G.; Reda, R.; Mazzoni, A.; Di Nardo, D.; Testarelli, L. Laser microgrooved vs. machined healing abutment disconnection/reconnection: A comparative clinical, radiographical and biochemical study with split-mouth design. Int. J. Implant Dent. 2021, 7, 19. [Google Scholar] [CrossRef]
- Guarnieri, R.; Reda, R.; Di Nardo, D.; Miccoli, G.; Zanza, A.; Testarelli, L. In Vitro Direct and Indirect Cytotoxicity Comparative Analysis of One Pre-Hydrated versus One Dried Acellular Porcine Dermal Matrix. Materials 2022, 15, 1937. [Google Scholar] [CrossRef] [PubMed]
- Guarnieri, R.; Miccoli, G.; Reda, R.; Mazzoni, A.; Di Nardo, D.; Testarelli, L. Sulcus fluid volume, IL-6, and Il-1b concentrations in periodontal and peri-implant tissues comparing machined and laser-microtextured collar/abutment surfaces during 12 weeks of healing: A split-mouth RCT. Clin. Oral Implant. Res. 2022, 33, 94–104. [Google Scholar] [CrossRef]
- Huang, Z.-L.; Shi, J.-Y.; Zhang, X.; Gu, Y.-X.; Lai, H.-C. The influence of the shock-absorbing restorative materials on the stress distributions of short dental implant rehabilitations. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 24–34. [Google Scholar] [PubMed]
| Title and First Author | Objective | Year | Conclusions |
|---|---|---|---|
| Is the high-performance thermoplastic polyetheretherketone indicated as a clasp material for removable dental prostheses? Micovic D. et al. | To investigate the retention force of polyetheretherketone (PEEK) removable dental prosthesis clasps in comparison with a cobalt-chrome-molybdenum control group after storage in artificial saliva. | 2020 [16] | The retention force values observed for PEEK materials indicate a potential clinical application, not influenced by manufacturing process. PEEK materials presented constant results also after artificial aging. |
| Comparative evaluation of BioHPP and titanium as a framework veneered with composite resin for implant-supported fixed dental prostheses Jin H.Y. et al. | The aim was to evaluate and compare the bond strength of modified PEEK (BioHHP) and titanium with a veneering composite resin and compare the marginal fit and fracture resistance of implant-supported screw-retained FDPs fabricated by using computer-aided design and computer-aided manufacturing (CAD/CAM) frameworks veneered with composite resin. | 2019 [4] | The bond strength of BioHPP to composite resin was greater than that of titanium. CAD/CAM BioHPP frameworks exhibited good marginal fit and fracture resistance, it represent a suitable alternative to metal restoration. |
| Cytocompatibility of Titanium, Zirconia and Modified PEEK after Surface Treatment Using UV Light or Non-Thermal Plasma Guo L. et al. | The objective of this study was to compare the effects of UV light and NTP on machined titanium, zirconia and modified polyetheretherketone (PEEK, BioHPP) surfaces in vitro. | 2019 [17] | UV light and oxygen plasma treatments may improve the attachment, proliferation and viability of soft tissue cells on machined titanium, zirconia and ceramic reinforced PEEK surfaces. These materials they offer excellent biocompatibility characteristics. |
| Fracture Resistance of Titanium, Zirconia, and Ceramic-Reinforced Polyetheretherketone Implant Abutments Supporting CAD/CAM Monolithic Lithium Disilicate Ceramic Crowns After Aging Atsü S.S. et al. | The aim of this study was to compare the effects of UV light and NTP on machined titanium, zirconia and modified polyetheretherketone (PEEK, BioHPP) surfaces in vitro. | 2019 [18] | Promising fracture strengths and fracture types were found for the ceramic reinforced PEEK abutments with titanium base |
| A potential application of materials based on a polymer and CAD/CAM composite resins in prosthetic dentistry Jovanović M. et al. | A bioactive high performance polymer (BioHPP) and computer-aided design/computer-aided manufacturing (CAD/CAM) composite resin materials are a relatively new class of dental biomaterials, that are biocompatible and have good aesthetic features. | 2021 [6] | These materials offer many advantages over traditional metal-ceramic materials, such as better aesthetics properties, biocompatibility, and less brittleness. Summing up the available literature and publications we concluded that the best indication for using BioHPP and Trinia in prosthetics is making a framework for superstructure on implants. |
| Influence of fatigue loading on fracture resistance of endodontically treated teeth restored with endocrowns. Elashmawy Y. et al. | This in vitro study aimed to evaluate the influence of fatigue loading on fracture resistance of endodontically treated molars restored with endocrowns using different machinable blocks. | 2021 [19] | Poly infiltrated ceramics should be considered as a proper material to be used as an endocrown material, also because of its ability to be restorable if failure occurs. |
| Retention of a telescopic overdenture on customized abutments after the simulation of 1 year in function Ramadan R. et al. | The aim of the study was to evaluate the retention of a BioHPP (biocompatible highperformance polymer) telescopic overdenture supported by customized abutments made from 2 different materials after the simulation of 1 year in function. | 2021 [20] | BioHPP and titanium are both considered suitable materials for customized abutments to retain BioHPP telescopic implant overdentures. |
| Modified PEEK Resin Bonded Fixed Dental Prosthesis for a Young Cleft Lip and Palate Patient Andrikopoulou E. et al. | This clinical report presents the use of a modified poly etheretherketone material as an alternativematerial for the fabrication of resin-bonded fixed dentalprosthesis (RBFDP) framework. | 2016 [15] | Due to lack of clinical evidence, BioHPP cannot substitute the conventional metal ceramic or all ceramic materials; however it can be used as an alternative treatment option. |
| Flexural strength of polymethyl methacrylate reinforced with high-performance polymer and metal mesh Ardakani Z.H. et al. | The present study aimed to evaluate the effect of high-performance polymer (BioHPP) and metal mesh reinforcement on the FS of a heat-cured poly methyl methacrylate (PMMA) acrylic resin. | 2021 [21] | Accordingly, BioHPP is not a suitable substitute for metal reinforce to enhance the Fracture Strenght of PMMA denture base material. |
| Comparative evaluation of marginal and internal fit of endocrowns using lithium disilicate and polyetheretherketone computer-aided design—computer-aided manufacturing (CAD-CAM) materials: An in vitro study Godil A.Z. et al. | The primary research question was to investigate any statistically significant differences in the marginal and internal gap of endocrowns using PEEK or Lithium Disilicate for endocrowns. | 2021 [22] | The current study shows a statistically significant difference in which lithium disilicate showed a better marginal and internal fit compared to PEEK. However, the marginal fit of both materials is within the clinical acceptable range. Hence, both the materials can be used as endocrown materials. |
| Wear behavior of current computer-aided design and computer-aided manufacturing composites and reinforced high performance polymers: An in vitro study Diken Turksayar A.A. et al. | To analyze the wear rate of computer-aided design and computer-aided manufacturing (CAD/CAM) composites, polyetheretherketones and glass ceramics. | 2021 [23] | High performance polymers show less wear against natural enamel than ceramic and composite materials. The wear type of polyetheretherketone, which has high wear resistance and low elastic modulus, is also different from ceramic and composite materials. |
| Behavior of polyether-ether-ketone (PEEK) in prostheses on dental implants. A review. Blanch-Martínez N. et al. | The objective of this review is to know the characteristics of this material and thus assess its advantages and disadvantages in its possible applications in prostheses on dental implants. | 2021 [24] | The main PEEK characteristics are due to its low elastic modulus, similar to that of bone, its low hardness, which will not cause an abrasion of the opposing tooth as occurs with the ceramic. We cannot conclude anything on the survival of prostheses made with PEEK after a time in the mouth. |
| Comparative prospective clinical evaluation of computer aided design/computer aided manufacturing milled BioHPP PEEK inlays and Zirconia inlays. Rajamani V.K. et al. | The aim of the present study was to clinically assess the performance of BioHPP PEEK material when used for inlay restoration and to compare it with widely used zirconia inlays. | 2021 [25] | High level of accuracy of fit can be achieved in inlay restorations with use of BioHPP PEEK materials. |
| Retention of different CAD/CAM endocrowns bonded to severely damaged endodontically treated teeth: An in vitro study. Elashmawy Y. et al. | The aim of the present study was to assess the retention of endocrowns fabricated of different CAD/CAM materials. | 2021 [19] | Within the limitations of this study, using lithium disilicate glass ceramics and resin-infiltrated ceramics as restorative materials to fabricate endocrowns to restore severely damaged endodontically treated teeth recorded significantly higher retention values. |
| Polyetheretherketone (PEEK) Post and Core Restorations: A 3D Accuracy Analysis between Heat-Pressed and CAD/CAM Fabrication Methods. Lalama M. et al. | The purpose of this study was to evaluate the accuracy of polyetheretherketone (PEEK) based post and core restorations using heat-pressed and computer-aided design and computer-aided manufacturing (CAD/CAM) methods. | 2021 [26] | This study showed that heat-pressed PEEK post and core restorations resulted in higher accuracy when compared to the CAD/CAM method. |
| Comparison of the Bond Strength of Composite Resin to Zirconia and Composite Resin to Polyether Ether Ketone: An In Vitro Study Sarfaraz H. et al. | The aim of the study was to compare the shear bond strength of composite resin bonded to polyether ether ketone (PEEK) and zirconia, and also to evaluate the effect of thermocycling on the shear bond strength. | 2020 [27] | The shear bond strength of PEEK is similar to that of zirconia. As an alternative to metal, BioHPP can thus be recommended as a framework to be veneered with composite resin. |
| The Effect of Surface Pretreatment and Water Storage on the Bonding Strength of a Resin Composite Cement to Modified PEEK. Spyropoulos D. et al. | The aim was to evaluate the bonding quality of bonding to polyether ether ketone (PEEK) after different surface treatments. | 2020 [12] | Use of different conditioning protocols had a significant effect on the final bond strength of composite resin cement to PEEK surface |
| Retention force of polyetheretherketone and cobalt-chrome-molybdenum removable dental prosthesis clasps after artificial aging. Mayinger F. et al. | The aim is to examine the retention force of removable dental prosthesis (RDP) clasps made from polyetheretherketone (PEEK) and cobalt-chrome-molybdenum (CoCrMo, control group) after storage in water and artificial aging. | 2021 [28] | Within the tested PEEK materials, PEEKmilled2 presented superior results than PEEK pressed. Artificial aging led to a significant decline in retention force for all PEEK-based materials |
| Suitability of Secondary PEEK Telescopic Crowns on Zirconia Primary Crowns: The Influence of Fabrication Method and Taper Merk S. et al. | The aim is to investigates the retention load (RL) between ZrO2 primary crowns and secondary polyetheretherketone (PEEK) crowns made by different fabrication methods with three different tapers. | 2016 [29] | PEEK may be a suitable material for removable prosthesis and a telescopic crown technique when used on zirconia crowns. |
| Wear Resistance, Color Stability and Displacement Resistance of Milled PEEK Crowns Compared to Zirconia Crowns under stimulated Chewing and High-Performance Aging Abhay S. et al. | This study aimed to compare the wear resistance, abrasiveness, color stability, and displacement resistance of zirconia and PEEK milled crowns. | 2021 [30] | The PEEK crowns showed minimal abrasion, better stress modulation through plastic deformation, and good color stability, which makes it a promising alternative to zirconia for fabrication of the crown. |
| Optical Properties and Color Stability of Dental PEEK Related to Artificial Ageing and Staining Porojan L. et al. | The aim of this study was to investigate the long-term effect of the combined action of ageing and immersing solutions on the optical properties and color stability of PEEK material, related to surface processing (polishing or glazing). | 2021 [31] | PEEK glazing has a favorable effect on surface roughness and opalescence, irrespective of the artificial ageing or staining protocols. Artificial ageing damages the color stability and roughness of PEEK. |
| Comparison of various 3D printed and milled PAEK materials: Effect of printing direction and artificial aging on Martens parameters. Prechtel A. et al. | The aim of this study was to investigate the effect of artificial aging on the Martens parameters of different 3D printed and milled polyaryletherketon (PAEK) materials. | 2020 [32] | Additive manufacturing of PEEK for dental application sseems promising, but still needs further investigation to understand material and process influences better. |
| In-vitro fatigue and fracture testing of CAD/CAM-materials in implant-supported molar crowns. Preis V. et al. | The aim of the study is to investigate the fatigue and fracture resistance of different CAD/CAM-materialsas implant- or tooth-supported molar crowns with respect to the clinical procedure(screwed/bonded restoration). | 2017 [33] | Conclusion based on the present in vitro results, most CAD/CAM materials, except for polyether ether ketone with composite pasteveneers, may be applied in implant-supported crowns with-out restrictions. The insertion of a screw channel resulted in a total failurerate of polyether ether ketone crowns with composite pasteveneers, and reduced fracture resistance for two compositematerials (COB, COH). |
| Influence of different materials on retention behavior of CAD/CAM fabricated bar attachments. Abdelrehim A. et al. | The aim was was to assess the retentive behavior of implant overdentures and the loss of retention from clip wear when used with computer-aided design and computer-aided manufacturing (CAD/CAM) fabricated bar attachments from cobaltchromium (Co-Cr), zirconia (ZrO2), and BioHPP to identify the optimal material in terms of minimal loss of retention and minimal wear. | 2021 [34] | BioHPP is a candidate for replacing Co-Cr and ZrO2 for fabricating bar attachments. |
| Retention force of differently fabricated telescopic PEEK crowns with different tapers. Stock V. et al. | The aim of this study was To assess the retention force between primary and secondary PEEK crowns made by different fabrication methods. | 2016 [35] | Milled PEEK crowns with a 0° taper showed the lowest retention force values, whereas milled PEEK crowns with a 2° taper showed the highest retention force values. For pressed PEEK crowns the taper angle had no impact on retention force. |
| The Use of a Modified Poly-Ether-Ether-Ketone (PEEK) as an Alternative Framework Material for Removable Dental Prostheses. A Clinical Report Zoidis P. et al. | The aim of this study eas to evaluate fot the first time BioHPP as an alternative framework material for removable dental prostheses. | 2016 [3] | Due to the lack of solid clinical evidence, BioHPP should not be considered as a substitute framework material for a well-designed Cr-Co RDP. |
| Modified PEEK resin-bonded fixed dental prosthesis as an interim restoration after implant placemen Zoidis P. et al. | The aim of this study was to evaluate modified PEEK resin-bonded fixed dental prosthesis as an interim restoration after implant placement | 2016 [36] | PEEK has a low specific weight that permits the fabrication of lighter prostheses, providing high patient satisfaction and comfort during function. |
| Denture base adaptation, retention, and mechanical properties of BioHPP versus nano-alumina-modified polyamide resins Emera R.M.K. et al. | The present study aimed to evaluate the mechanical properties, adaptation, and retention of alumina nanoparticles (Al2O3 NPs) modified polyamide resin versus BioHPP (high-performance polymer) denture base materials. | 2021 [37] | BioHPP and Al2O3 NP-modified polyamide resin could be used as a promising alternative denture base material with good adaptation, retention, and mechanical properties. |
| Comparison of the strain developed around implants with angled abutments with two reinforced polymeric CAD/CAM superstructure materials: An in vitro comparative study Omaish H.H.M. et al. | The aim is to assess the strain developed around implants with angled abutments (15 and 25 degrees) of biocompatible high-performance polymer (BioHPP) and reinforced nanohybrid polymer with a multilayered glass fiber (TRINIA) superstructure under axial and oblique loading | 2022 [38] | The strain developed around dental implants was significantly affected by the superstructure material. The microstrain was considerably higher when the implant abutment angulation increased. When a 45-degree loading direction was used, this tendency became more pronounced. |
| Review of Different Materials that can be CAD/CAM Processed Description, chemical composition, indications in dentistry areas Popa D. et al. | The objective of this paper is to inform on the indications, appearance and advantages offered by each category of materials used in CAD/CAM technique for different prosthetic restorations. We can choose from available materiales including glass ceramics, nano ceramics, zirconia, hybrid ceramics, BioHPP, in blocks or disks form. | 2019 [39] | BioHPP is a high performance polymer developed especially for intra-oral use. Indications in dentistry areas: single crowns, bridges (maximum 2 pontics), adhesive bridges (Maryland), suprastructures with or without frictional elements, secondary parts for telescopic crown technique and bar suprastructures, supraimplant restorations, crowns and bridges (cemented or screwed), primary crowns, removable suprastructures, Toronto bridge. |
| Comparison of Two Evaluating Methods for Establishing the Marginal Fit on Four Heat—Pressed Resin Inlays. Baciu S. et al. | The aim is to compare two investigation methods, a bi-dimensional and a three-dimensional technique, by examining the marginal fit of pressed resin (BioHPP) inlays. | 2018 [40] | Composite inlays are an alternative with superior results offering good esthetic results and longevity compared to Fillings. BioHPP provides very good clinical results due to of the structure but also due to of the polymerization method, namely heat pressing. It has no abrasive effect on the remaining teeth, it has white color suitable for fully anatomical use, and it insures no ion exchange in the mouth, no discoloration along with excellent stability and optimal polishable properties. |
| Evaluations of Two Reinforced Polymers Used as Metal-FreeSubstructures in Fixed Dental Restorations Biris C. et al. | The purpose of the study was to present the results of the comparative clinical trials referring to the use of BioHPP and Trinia resins as core in fixed prosthetic rehabilitation. | 2018 [41] | Both types of these materials exhibit a certain degree of elasticity and have numerous advantages. |
| Three-dimensional Marginal Evaluation of Two Pressed Materials Using Micro-CT Technology Baciu S. et al. | The aim of this study is to compare themarginal fit of two different kind of pressed materials: a partially crystalline thermoplastic resin reinforced with ceramic particles (BioHPP) and lithium disilicate (Max), through the use of the microCT technique. | 2017 [42] | A significant statistical difference was found between the marginal gap size obtained for BioHPP and Emax inlays (p < 0.001). For the Emax inlays the marginal gap had an average of 72 μm, while for BioHPP the average was 94 μm. |
| The Benefits of Polyether-Ether-Ketone Polymers in Partial Edentulous Patients Pacurar M. et al. | The purpose of this article is to present the results of the clinical trials referring to the benefits of skeleton prostheses wearers’patients with BioHPP framework. | 2016 [43] | This PEEK type of dental material represent a beneficial new acquisitionfor the partial edentulous patient. |
| The Advantages of BioHPP Polymer as Superstructure Material in Oral Implantology Bechir M. et al. | The purpose of this article is to present the results of the clinical trials referring to the advantages of BioHPPpolymer as superstructure in oral implantology. | 2016 [44] | BioHPP for fixed prosthetic restoration, like superstructure on dental implant abutments present many advantages. |
| A new material for fixed implant-supported rehabilitations Di Iorio E. et al. | The aims of this study were to describe the implant-supported rehabilitation of a female patient presenting a totally edentulous maxilla and to highlight the clinical features of a new polymer used for the final restoration. | 2015 [45] | This new polymer material, introduced in prosthetic dentistry in 2013, may substitute metal or zirconium thanks to its extraordinary flexibility, great resistance, low weight, optimumpolishing features and low plaque affinity. |
| Short-term comparative evaluation of BioHPP and cast cobalt–chromium as framework for implant supported prostheses: A split mouth clinical randomized trial Amer M. et al. | The purpose of this parallel randomized clinical trial was to evaluate the effects of BioHPP versus cobalt–chromium (Co–Cr) frameworks in screw-retained implant-supported fixed dental prostheses (FDPs) on peri-implant soft and hard tissues clinically and radiographically | 2021 [46] | BioHPP framework represents a viable nonmetallic alternative to cast Co–Cr framework, shown by good soft and hard tissue responses. |
| Evaluation of biocompatibility of veneered Bio HPP and veneered lithium disilicate crowns in anterior zone (Randomized controlled clinical trial) Odeh E. et al. | The aim of the present study is to evaluate the biocompatibility of Bio-High Performance Polymer (Bio HPP) crowns veneered with Visio-Ling versus e.max crowns veneered with e.max veneering system. | 2021 [47] | Bio HPP showed a higher significant difference PD than e.max. |
| One Year Clinical Evaluation of Milled BioHPP (PEEK) Versus Zirconia Veneered Single Crowns (RCT-one-year Evaluation) Badran A.R. et al. | BioHPP PEEK single crowns as a intervention to evaluate the marginal integrity and fracture. | 2021 [48] | BioHPP PEEK is a promising material for dental application and it has been proposed for other prosthodontic applications such as fixed prostheses and removable prostheses. |
| Clinical Application of PEEK as a Provisional Fixed Dental Prosthesis Retained by Reciprocated Guide Surfaces of Healing Abutments During Dental Implant Treatment Kwan J.C. et al. | The aim is to evaluate BioHPP for use in provisional fixed dental prostheses (FDPs) that can be retained by reciprocated guide surfaces of hexagonal-shaped healing abutments during dental implant treatment. | 2021 [49] | The results from this study suggest that PEEK can be a suitable material for use in provisional Fixed Dental Prosthesis during dental implant treatment. |
| Comparative Study Clarifying the Usage of PEEK as Suitable Material to Be Used as Partial Denture Attachment and Framework. Sadek S.A. et al. | This consideration aimed to verify the convention of polyether ether ketone (PEEK) material as an attachment. | 2019 [50] | Utilization of PEEK material as both an attachment and framework decline the strains performed around the abutment teeth and over the edentulous ridge. |
| Comparative Study on the Degree of Bacterial Biofilm Formation of Dental Bridges Made from Three Types of Materials Bolat M. et al. | The aim of this study was to compare the biofilm formation on three types of dental crown materials using adenosine triphosphate (ATP) driven bioluminescence as an innovative tool for the rapid chairside enumeration of oral bacteria and assessment of oral hygiene. | 2019 [51] | The lowest value was shown for Zirconia, comparing with ceramics and BioHpp, but in time we have seen the increase of ATP for all three dental crown materials. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reda, R.; Zanza, A.; Galli, M.; De Biase, A.; Testarelli, L.; Di Nardo, D. Applications and Clinical Behavior of BioHPP in Prosthetic Dentistry: A Short Review. J. Compos. Sci. 2022, 6, 90. https://doi.org/10.3390/jcs6030090
Reda R, Zanza A, Galli M, De Biase A, Testarelli L, Di Nardo D. Applications and Clinical Behavior of BioHPP in Prosthetic Dentistry: A Short Review. Journal of Composites Science. 2022; 6(3):90. https://doi.org/10.3390/jcs6030090
Chicago/Turabian StyleReda, Rodolfo, Alessio Zanza, Massimo Galli, Alberto De Biase, Luca Testarelli, and Dario Di Nardo. 2022. "Applications and Clinical Behavior of BioHPP in Prosthetic Dentistry: A Short Review" Journal of Composites Science 6, no. 3: 90. https://doi.org/10.3390/jcs6030090
APA StyleReda, R., Zanza, A., Galli, M., De Biase, A., Testarelli, L., & Di Nardo, D. (2022). Applications and Clinical Behavior of BioHPP in Prosthetic Dentistry: A Short Review. Journal of Composites Science, 6(3), 90. https://doi.org/10.3390/jcs6030090











