The Relative Importance of Key Factors for Integrating Enterprise Resource Planning (ERP) Systems and Performance Management Practices in the UAE Healthcare Sector
Abstract
1. Introduction
- RQ1—How do ERP systems impact the efficiency and effectiveness of performance management in healthcare settings?
- RQ2—What challenges do healthcare organizations face during the implementation of ERP systems aimed at enhancing performance management?
- RQ3—What are the key factors influencing the successful integration of ERP systems with performance management practices in healthcare organizations?
- RQ4—What are the most critical factors for the successful integration of ERP systems with performance management practices in healthcare organizations within the UAE healthcare sector?
2. Literature Review
2.1. ERP in Healthcare
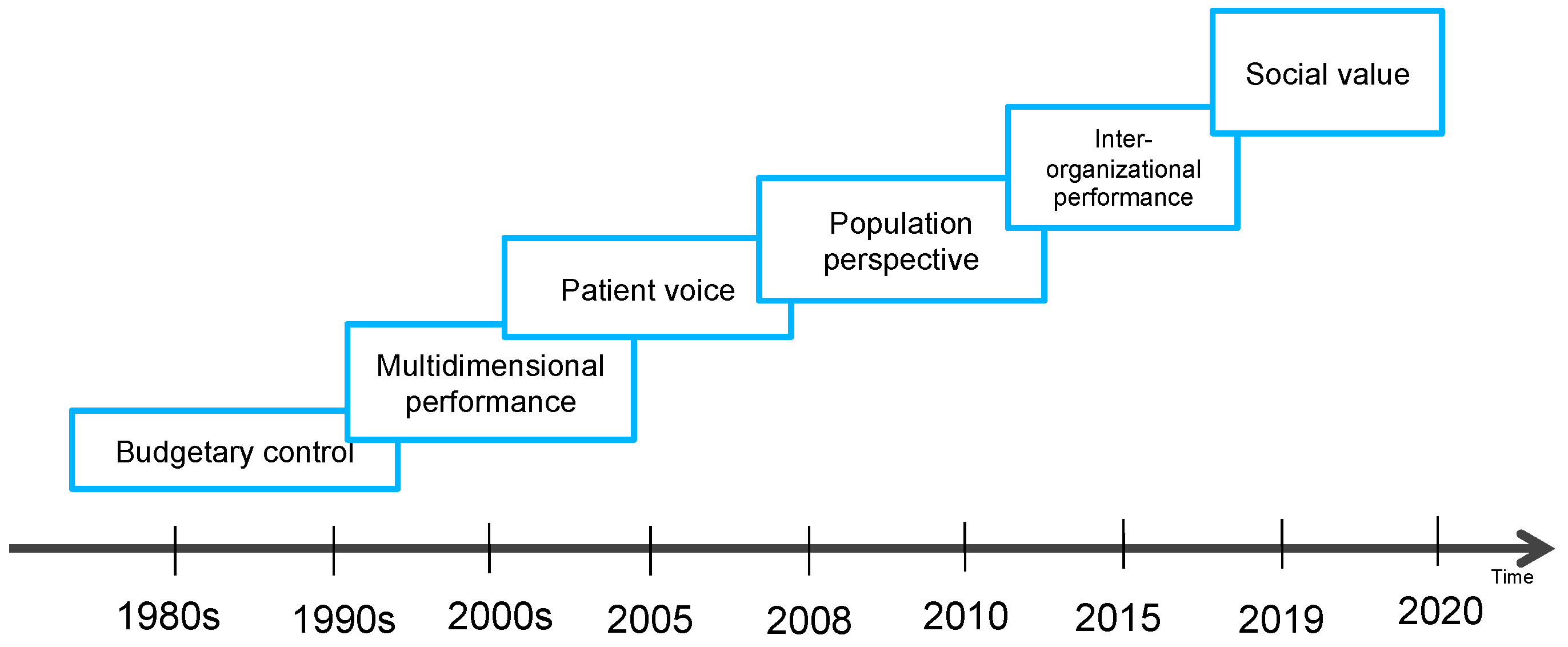
2.2. Performance Management in Healthcare
2.3. Integration of ERP in Healthcare for Enhanced PM
| Categories | Factors | Ref. |
|---|---|---|
| Availability of financial resources to invest in system direct and indirect cost | [44] | |
| Readiness of healthcare organization to adopt and accommodate ERP system | [46] | |
| Availability of system-wide integration to reduce silos | [50] | |
| Availability of top management support | [52] | |
| Clear objectives and requirements for ERP system implementation | [53] | |
| Source of the ERP system | [56] | |
| Chosen implementation strategy | [56] | |
| Present of effective change management plan | [60] | |
| Alignment of ERP systems with business processes | [55] | |
| Vendor support and expertise | [64] | |
| Availability of data quality and migration process | [65] | |
| User involvement and training during implementation | [62] | |
| Customization overload | [32,55,64] | |
| Technical competence of employee | [63] | |
| Readiness for integration | [55] | |
| Availability of project management plan with clear timelines, the establishment of key milestones, and the delineation of responsibilities | [37] | |
| Adherence to regulatory compliance | [58] | |
| Current technological infrastructure of the healthcare facility | [59] | |
| Availability of balance security requirement and compliance | [66] | |
| PM | Access to accurate and timely real information | [71] |
| Availability of performance metrics and measurement tools | [72] | |
| Clear long-term goals and objectives | [73] | |
| Availability of patient-centered metrics | [73] | |
| Effective leadership | [73] | |
| Managerial support and involvement | [76] | |
| Employee involvement and engagement in designing performance metrics | [77] | |
| Effectiveness of organizational individual performance measures (quality, time, cost, and flexibility) | [96] | |
| Effectiveness of performance measurement system (alignment of individual measures with overarching goals, maintaining balance among varying metric) | [96] | |
| Alignment with organizational culture, strategy, and structure | [96] | |
| Responsiveness to market dynamics, customer demands, and competitive landscapes | [96] | |
| Level of organizational technological improvements in performance measurement | [81] | |
| Organizational efficiency in success use of hospital management resources | [71] | |
| Effectiveness of the overall outcomes of a healthcare service | [71] | |
| Flexibility and system’s adaptability to change | [71] | |
| Availability of key performance indicators | [84] | |
| Availability of follow-up and accountability system | [85] |
3. Materials and Methods
3.1. Stage 1—Factors Validation
3.2. Stage 2—Expert Importance Rating of Factors
3.3. Stage 2—Factors Ranking
- ∑W: The sum of the weights of each factor multiplied by the frequency of the answer;
- A: The highest criteria score, which was 5 in this study;
- N: the number of respondents, which was 81 in this study [101].
4. Results
4.1. Factor Validation and Consolidation—Semi Structured Interview
4.2. Ranking of the Factors
4.3. Confirmation of the RII Calculation
5. Discussion
- Strengthening Top-Ranked Factors: Stress the importance of prioritizing top-tier factors such as employee involvement, effective performance measurement, and accurate data utilization; these elements are fundamental, as they ensure the ERP system aligns with real operational needs and engages employees by reflecting their input and impact. By focusing on these high-impact factors, healthcare organizations can directly enhance system effectiveness, increase employee engagement, and ensure organizational alignment.
- Robust Mid-Tier Support: Effective leadership and managerial involvement are crucial in maintaining the momentum of ERP integration. Leaders and managers play crucial roles in bridging the gap between strategic goals and operational execution. They ensure that the ERP system is used correctly and that its data are accurate, facilitating alignment with organizational objectives. This support is essential for configuring ERP systems that complement strategic directions and operational needs for healthcare organizations.
- Proactively Planning for Lower-Ranked Elements: Infrastructure, scalability, security, and compliance, though ranked lower, are foundational for the successful deployment and ongoing effectiveness of ERP systems. Proactively managing these aspects to prepare for future growth, technological advancements, and evolving performance management needs, is recommended. Ensuring that the ERP system is scalable and secure helps maintain its relevance and effectiveness over time.
- Holistic Integration: A comprehensive integration strategy that addresses all factors—high, mid, and lower-ranked factors—is recommended to create a balanced and effective ERP system. This approach not only enhances the immediate effectiveness and efficiency of the ERP implementation but also ensures its long-term sustainability and adaptability within the healthcare setting.
- Address the Ethical Considerations, Opportunities, and Challenges of Digital Health Technology: To safeguard data and performance indicators, organizations should deploy strong cybersecurity protections. Standard protocols for system compatibility will streamline the data flow and improve performance measurement. Staff should receive comprehensive training to reduce resistance and maximize ERP and digital health technology utilization. Performance management and patient engagement can be improved by incorporating advanced analytics, telemedicine, and mobile health apps. The use of ethical technology requires patient confidentiality, informed consent for data use, and equal access to digital health solutions. Clear ethical norms and procedures are essential to stakeholder trust. ERP systems and performance management practices remain effective, relevant, and up to date by reviewing and modifying practices to keep up with changing ethical standards and technology and involving stakeholders for feedback.
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Van Hoa, N.; Van Thu, P.; Dat, N.T.; Loan, L.T.; Phung, T.M. Impact of digital transformation on the decision-making process in logistics and construction enterprises in Vietnam. Int. J. Adv. Multidiscip. Res. Stud. 2023, 3, 339–350. [Google Scholar]
- Kulkarni, N.D.; Director, E.A.S.; Bansal, S.; Manager, E.A.S. Defining Data Migration Strategies for Seamless ERP Transformation Case Study. J. Econ. Manag. Res. 2023, 4, 1–7. [Google Scholar] [CrossRef]
- Nyathani, R.; Allam, K.; Engineer, B.I. Synergizing AI, Cloud Computing, and Big Data for Enhanced Enterprise Resource Planning (ERP) Systems. Int. J. Comput. Tech. 2024, 11, 1–6. [Google Scholar]
- Hong, K.-K.; Kim, Y.-G. The critical success factors for ERP implementation: An organizational fit perspective. Inf. Manag. 2002, 40, 25–40. [Google Scholar] [CrossRef]
- Hendricks, K.B.; Singhal, V.R.; Stratman, J.K. The impact of enterprise systems on corporate performance: A study of ERP, SCM, and CRM system implementations. J. Oper. Manag. 2007, 25, 65–82. [Google Scholar] [CrossRef]
- Morris, J.J. The Impact of Enterprise Resource Planning (ERP) Systems on the Effectiveness of Internal Controls over Financial Reporting. J. Inf. Syst. 2011, 25, 129–157. [Google Scholar] [CrossRef]
- Tarafdar, M.; Gordon, S.R. Understanding the influence of information systems competencies on process innovation: A resource-based view. J. Strateg. Inf. Syst. 2007, 16, 353–392. [Google Scholar] [CrossRef]
- Moon, Y.B. Enterprise Resource Planning (ERP): A review of the literature. Int. J. Manag. Enterp. Dev. 2007, 4, 235–264. [Google Scholar] [CrossRef]
- Aryani, I.; Tanjung, R.A.; Rahmadyah, N.; Nurbaiti, N. Analysis of the Role of ERP Systems in Business Process Integrity. J. Ekon. Manaj. Bisnis Dan Akunt. Rev. 2021, 1, 232–240. [Google Scholar] [CrossRef]
- Andreas, D.; Savitri, D. Information System and Service Quality: An Empirical Study of Their Impact on End-Users Satisfaction ERP Systems. Int. J. Res. Bus. Technol. 2018, 10, 80–84. [Google Scholar] [CrossRef]
- Neef, G.; Wieczorek, L. From quality management system to the integrated management in small and medium-sized enterprises in the field of manufacturing. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2000, 2, 281. [Google Scholar] [CrossRef]
- Rekha, Y.C. Performance Management System with Respect to Retail Industry. SSRN Electron. J. 2014. [Google Scholar] [CrossRef]
- Mueller-Hanson, R. Driving organizational strategy through performance management. In Performance Management Transformation; Oxford University Press: New York, NY, USA, 2020. [Google Scholar]
- Simpson, G.; Simpson, R. Managing the Performance Management Process: The Importance of Employees’ Performance in Determining the Organisation’s Viability and Efficiency. J. Hum. Resour. Leadersh. 2022, 6, 42–56. [Google Scholar] [CrossRef]
- Zomerdijk, L.G.; de Vries, J. Structuring front office and back office work in service delivery systems. Int. J. Oper. Prod. Manag. 2007, 27, 108. [Google Scholar] [CrossRef]
- Azevedo, P.S.; Romão, M.; Rebelo, E. Advantages, Limitations and Solutions in the Use of ERP Systems (Enterprise Resource Planning)—A Case Study in the Hospitality Industry. Procedia Technol. 2012, 5, 264–272. [Google Scholar] [CrossRef][Green Version]
- Garefalakis, A.; Mantalis, G.; Vourgourakis, E.; Spinthiropoulos, K.; Lemonakis, C. Healthcare Firms and the ERP Systems. J. Eng. Sci. Technol. Rev. 2016, 9, 139–144. [Google Scholar] [CrossRef]
- Meesala, A.; Paul, J. Service quality, consumer satisfaction and loyalty in hospitals: Thinking for the future. J. Retail. Consum. Serv. 2018, 40, 261–269. [Google Scholar] [CrossRef]
- Danzon, P.M.; Furukawa, M.; Tan, J.K. E-health: Impacts of internet technologies on various healthcare and services sectors. Int. J. Healthc. Technol. Manag. 2014, 4, 71–86. [Google Scholar]
- Walters, J.K.; Sharma, A.; Malica, E.; Harrison, R. efficiency improvement in public health systems: A rapid evidence synthesis. BMC Health Serv. Res. 2022, 22, 293. [Google Scholar] [CrossRef]
- Aziz, M.A.; Ragheb, M.A.; Ragab, A.A.; El Mokadem, M. The impact of enterprise resource planning on supply chain management practices. Bus. Manag. Rev. 2018, 9, 56–69. [Google Scholar]
- Velcu, O. Exploring the effects of ERP systems on organizational performance. Ind. Manag. Data Syst. 2007, 107, 1316–1334. [Google Scholar] [CrossRef]
- Mahmood, F.; Khan, A.Z.; Bokhari, R.H. ERP issues and challenges: A research synthesis. Kybernetes 2020, 49, 629–659. [Google Scholar] [CrossRef]
- Tarhini, A.; Ammar, H.; Tarhini, T.; Masa’Deh, R. Analysis of the Critical Success Factors for Enterprise Resource Planning Implementation from Stakeholders’ Perspective: A Systematic Review. Int. Bus. Res. 2015, 8, 25. [Google Scholar] [CrossRef]
- Ferreira, A.A.; Kuniyoshi, M.S. Critical factors in the implementation process of integrated management systems. J. Inf. Syst. Technol. Manag. 2015, 12, 145–164. [Google Scholar] [CrossRef]
- Valashani, M.A.; Abukari, A.M. Erp Systems Architecture for the Modern Age: A Review of the State of the Art Technologies. J. Appl. Intell. Syst. Inf. Sci. 2020, 1, 70–90. [Google Scholar] [CrossRef]
- Gonçalves, C.T.; Gonçalves, M.J.A.; Campante, M.I. Developing Integrated Performance Dashboards Visualisations Using Power BI as a Platform. Information 2023, 14, 614. [Google Scholar] [CrossRef]
- Ganesha, K.; Supriya, K.V.; Soundarya, M. Analyzing the waiting time of patients in hospital by applying heuristics process miner. In Proceedings of the 2017 International Conference on Inventive Communication and Computational Technologies (ICICCT), Coimbatore, India, 10–11 March 2017; Available online: https://search.proquest.com/docview/1919640349 (accessed on 23 May 2024).
- Langabeer, J., 2nd; Delgado, R.; Mikhail, O. Technology governance strategies for maximizing healthcare economic value. Developing management systems for IT. J. Healthc. Inf. Manag. 2007, 21, 19–24. Available online: https://www.ncbi.nlm.nih.gov/pubmed/19195277 (accessed on 23 May 2024).
- Hung, S.-Y.; Chen, C.; Wang, K.-H. Critical success factors for the implementation of integrated healthcare information systems projects: An organizational fit perspective. Commun. Assoc. Inf. Syst. 2014, 34, 39. [Google Scholar] [CrossRef]
- Alkhaldi, M.; Moonesar, I.A.; Issa, S.T.; Ghach, W.; Okasha, A.; Albada, M.; Chelli, S.; Takshe, A.A. Analysis of the United Arab Emirates’ contribution to the sustainable development goals with a focus on global health and climate change. Clin. Gov. 2023, 28, 357–367. [Google Scholar] [CrossRef]
- Ghalaita, A.A.; Al Suwaidi, N.; Al Khatib, M.; Elkhatib, M.M. Barriers hindering the adoption of Health Information Systems (HIS): Cases from Dubai’s healthcare providers. Int. J. Excell. E-Solut Manag. 2015, 4, 1–12. [Google Scholar] [CrossRef][Green Version]
- Chopra, R.; Sawant, L.; Kodi, D.; Terkar, R. Utilization of ERP systems in manufacturing industry for productivity improvement. Mater. Today Proc. 2022, 62, 1238–1245. [Google Scholar] [CrossRef]
- Chauhan, V.; Singh, J. Enterprise Resource Planning Systems Implementation in Online Travel Agencies. Int. J. Hosp. Tour. Syst. 2020, 13, 30–37. [Google Scholar]
- Lorincz, P. Evolution of enterprise systems. In Proceedings of the 2007 International Symposium on Logistics and Industrial Informatics, Wildau, Germany, 13–15 September 2007. [Google Scholar] [CrossRef]
- Ametowobla, D.; Prechelt, L. How layered reuse can support harmful micropolitics. In Proceedings of the ACM/IEEE 42nd International Conference on Software Engineering: Software Engineering in Society, Seoul, Republic of Korea, 27 June–19 July 2020. [Google Scholar] [CrossRef]
- Poba-Nzaou, P.; Uwizeyemungu, S.; Raymond, L.; Paré, G. Motivations underlying the adoption of ERP systems in healthcare organizations: Insights from online stories. Inf. Syst. Front. 2014, 16, 591–605. [Google Scholar] [CrossRef]
- Motahar, S.; Safie, N.; Mukhtar, M.; Aljunid, S.; Mostafavi, S. An Applied Approach to Teach Hospital Information Systems Development Using an Open Source ERP Framework. Procedia Technol. 2013, 11, 1259–1265. [Google Scholar] [CrossRef][Green Version]
- Fruggiero, F.; Iannone, R.; Riemma, S. The care for planning and control in a framework for hospital management. In Proceedings of the IADIS International Conference E-Health, Rome, Italy, 20–22 July 2011; pp. 43–52. [Google Scholar]
- Tummers, J.; Tobi, H.; Catal, C.; Tekinerdogan, B. Designing a reference architecture for health information systems. BMC Med. Inform. Decis. Mak. 2021, 21, 210. [Google Scholar] [CrossRef]
- de Almeida, D.R.D.S.M.V. ERP’s for the Healthcare Industry—A Methodology for Smart Choosing the Best ERP in the Market for the Specific Needs of Different Types of Healthcare Organizations. Master’s Thesis, Universidade NOVA de Lisboa, Lisboa, Portugal, 2022. [Google Scholar]
- Perera, P.; Nanayakkara, S.; Perera, A. Benefit of implementing a national level ERP system for health sectors in sri lanka through stock optimization. In Proceedings of the Second International Congress of Interdisciplinary Research and Development, Bangkok, Thailand, 31 May–1 June 2012. [Google Scholar] [CrossRef]
- Sanja, M.M. Impact of Enterprise Resource Planning System in Health Care. Int. J. Acad. Res. Bus. Soc. Sci. 2013, 3, 404. [Google Scholar] [CrossRef] [PubMed]
- Bialas, C.; Bechtsis, D.; Aivazidou, E.; Achillas, C.; Aidonis, D. Digitalization of the healthcare supply chain through the adoption of enterprise resource planning (ERP) systems in hospitals: An empirical study on influencing factors and cost performance. Sustainability 2023, 15, 3163. [Google Scholar] [CrossRef]
- Handayani, P.W.; Hidayanto, A.N.; Budi, I. User acceptance factors of hospital information systems and related technologies: Systematic review. Inform. Health Soc. Care 2018, 43, 401–426. [Google Scholar] [CrossRef]
- Almajali, D.A.; Masa’deh, R.; Tarhini, A. Antecedents of ERP systems implementation success: A study on Jordanian healthcare sector. J. Enterp. Inf. Manag. 2016, 29, 549–565. [Google Scholar] [CrossRef]
- Chofreh, A.G.; Goni, F.A.; Klemeš, J.J. Sustainable Enterprise Resource Planning Systems Implementation: A Framework Development. J. Clean. Prod. 2018, 198, 1345–1354. [Google Scholar] [CrossRef]
- Stefanou, C.J.; Revanoglou, A. ERP integration in a healthcare environment: A case study. J. Enterp. Inf. Manag. 2006, 19, 115–130. [Google Scholar] [CrossRef]
- Mucheleka, M.; Halonen, R. ERP in healthcare. In Proceedings of the International Conference on Enterprise Information Systems, SCITEPRESS—Science and Technology Publications, Barcelona, Spain, 27–30 April 2015; pp. 162–171. [Google Scholar] [CrossRef][Green Version]
- Armitage, G.D.; Suter, E.; Oelke, N.D.; Adair, C.E. Health systems integration: State of the evidence. Int. J. Integr. Care 2009, 9, e82. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.G.; Venkatesh, V. Job Characteristics and Job Satisfaction: Understanding the Role of Enterprise Resource Planning System Implementation. MIS Q. 2010, 34, 143–161. [Google Scholar] [CrossRef]
- Shao, Z.; Feng, Y.; Hu, Q. Effectiveness of top management support in enterprise systems success: A contingency perspective of fit between leadership style and system life-cycle. Eur. J. Inf. Syst. 2016, 25, 131–153. [Google Scholar] [CrossRef]
- Finney, S.; Corbett, M. ERP implementation: A compilation and analysis of critical success factors. Bus. Process Manag. J. 2007, 13, 329–347. [Google Scholar] [CrossRef]
- Velcu, O. Strategic alignment of ERP implementation stages: An empirical investigation. Inf. Manag. 2010, 47, 158–166. [Google Scholar] [CrossRef]
- Xu, A. Integration of an ERP System: A case study onintegration challenges with Microsoft Dynamics AX’. Master’s Dissertation, KTH, School of Industrial Engineering and Management (ITM), Stockolm, Sweden, 2017. Available online: http://kth.diva-portal.org/smash/get/diva2:1143433/FULLTEXT01.pdf (accessed on 23 May 2024).
- Tsai, W.H.; Fan, Y.W.; Der Leu, J.; Chou, L.W.; Yang, C.C. The relationship between implementation variables and performance improvement of ERP systems. Int. J. Technol. Manag. 2007, 38, 350–373. [Google Scholar] [CrossRef]
- Bhattacharya, M.; Ramakrishnan, T.; Fosso Wamba, S. Leveraging ERP systems for improving ERP effectiveness in emergency service organizations: An empirical study. Bus. Process Manag. J. 2023, 29, 710–736. [Google Scholar] [CrossRef]
- Shibly, H.R.; Abdullah, A.; Murad, M.W. ERP Adoption in Organizations: The Factors in Technology Acceptance among Employees; Palgrave Macmillan: Cham, Switzerland, 2022. [Google Scholar] [CrossRef]
- MacKinnon, W.; Wasserman, M. Integrated electronic medical record systems: Critical success factors for implementation. In Proceedings of the 2009 42nd Hawaii International Conference on System Sciences, Waikoloa, HI, USA, 5–8 January 2009. [Google Scholar]
- Françoise, O.; Bourgault, M.; Pellerin, R. ERP implementation through critical success factors’ management. Bus. Process Manag. J. 2009, 15, 371–394. [Google Scholar] [CrossRef]
- Kapupu, R.; Mignerat, M. Change management strategies in ERP implementations: A case study. In Proceedings of the CONF-IRM 2015—International Conference on Information Resources Management, Ottawa, ON, Canada, 18–20 May 2015; pp. 591–605. Available online: https://aisel.aisnet.org/confirm2015/41 (accessed on 23 May 2024).
- Obwegeser, N.; Danielsen, P.; Hansen, K.S.; Helt, M.A.; Nielsen, L.H. Selection and training of super-users for ERP implementation projects. J. Inf. Technol. Case Appl. Res. 2019, 21, 74–89. [Google Scholar] [CrossRef]
- Arif, F.; Kanchymalay, K.; Suryana, N.; Hashim UR, A.; Ismail, N.H. Measuring the effect of customization in influencing the success of ERP implementation. In Proceedings of the International Conference on Industrial Engineering and Business Management (ICIEBM), Yogyakarta, Indonesia, 12–13 October 2010; Available online: http://eprints.itenas.ac.id/174/ (accessed on 23 May 2024).
- Tuli, F.A.; Kaluvakuri, S. Implementation of ERP Systems in Organizational Settings: Enhancing Operational Efficiency and Productivity. Asian Bus. Rev. 2022, 12, 89–96. [Google Scholar] [CrossRef]
- Ali, M.; Xie, Y.; Cullinane, J. Ali, M.; Xie, Y.; Cullinane, J. A decision support system for ERP implementation in small and medium-sized enterprises. In Sociotechnical Enterprise Information Systems Design and Integration; IGI Global: Hershey, PA, USA, 2013; pp. 97–121. [Google Scholar] [CrossRef][Green Version]
- Xu, H.; Nord, J.H.; Brown, N.; Nord, G.D. Data quality issues in implementing an ERP. Ind. Manag. Data Syst. 2002, 102, 47–58. [Google Scholar] [CrossRef]
- Gupta, S.; Misra, S.C. Compliance, network, security and the people-related factors in cloud ERP implementation. Int. J. Commun. Syst. 2016, 29, 1395–1419. [Google Scholar] [CrossRef]
- Mettler, T.; Rohner, P. Performance management in health care: The past, the present, and the future. In Proceedings of the Internationalen Tagung Wirtschaftsinformatik, Wien, Austria, 25-27 February 2009; Available online: https://core.ac.uk/download/pdf/301355456.pdf (accessed on 23 May 2024).
- Osborne, S.P. Public Service Logic: Creating Value for Public Service Users, Citizens, and Society through Public Service Delivery, 1st ed.; Routledge: London, UK, 2020. [Google Scholar]
- Vainieri, M.; Noto, G.; Ferre, F.; Rosella, L.C. A performance management system in healthcare for all seasons? Int. J. Environ. Res. Public Health 2020, 17, 5590. [Google Scholar] [CrossRef]
- Heidari, S.; Tavakkoli-Moghaddam, R.; Salimi, B.; Mehdizadeh-Somarin, Z.; Hamid, M. An integrated approach for evaluating and improving the performance of hospital ICUs based on ergonomic and work-motivational factors. Comput. Biol. Med. 2024, 168, 107773. [Google Scholar] [CrossRef] [PubMed]
- Purbey, S.; Mukherjee, K.; Bhar, C. Performance measurement system for healthcare processes. Int. J. Product. Perform. Manag. 2007, 56, 241–251. [Google Scholar] [CrossRef]
- Star, S.; Russ-Eft, D.; Braverman, M.T.; Levine, R. Performance Measurement and Performance Indicators: A Literature Review and a Proposed Model for Practical Adoption. Hum. Resour. Dev. Rev. 2016, 15, 151–181. [Google Scholar] [CrossRef]
- Butler, M. Performance Measurement in the Health Sector; Institute of Public Administration (IPA): Dublin, Ireland, 2000; Available online: https://www.lenus.ie/handle/10147/575384 (accessed on 23 May 2024).
- Krishnan, S.K. 7 Elements of Effective Performance Management, Indian Institute of Management. 2013. Available online: https://www.researchgate.net/publication/237778624_7_elements_of_effective_performance_management (accessed on 23 May 2024).
- Singh, P.; Twalo, T. Effects Of Poorly Implemented Performance Management Systems on the Job Behavior and Performance of Employees. Iber 2016, 14, 79. [Google Scholar] [CrossRef]
- Mughal, H.A. Support at Work and its Relationship with Employee Performance: Critical Insights for Early Scholars. Acdmhr 2019, 1, 16–21. [Google Scholar] [CrossRef]
- Motyka, B. Employee engagement and performance: A systematic literature review. Int. J. Manag. Econ. 2018, 54, 227–244. [Google Scholar] [CrossRef]
- Hussain, S.D.; Khaliq, A.; Nisar, Q.A.; Kamboh, A.Z.; Ali, S. Impact of Employees’ Recognition, Rewards and Job Stress on Job Performance. Sjom 2019, 2, 69–82. [Google Scholar] [CrossRef]
- Musheke, M.M.; Phiri, J. The Effects of Effective Communication on Organizational Performance Based on the Systems Theory. Ojbm 2021, 09, 659–671. [Google Scholar] [CrossRef]
- Damawan, A.H.; Azizah, S. Resistance to change: Causes and strategies as an organizational challenge. In Proceedings of the 5th ASEAN Conference on Psychology, Counselling, and Humanities (ACPCH 2019), Gelugor, Malaysia, 2–3 November 2019. [Google Scholar] [CrossRef]
- Ippolito, A.; Sorrentino, M.; Capalbo, F.; Di Pietro, A. How technological innovations in performance measurement systems overcome management challenges in healthcare. Int. J. Product. Perform. Manag. 2023, 72, 2584–2604. [Google Scholar] [CrossRef]
- Fadel, K.J.; Tanniru, M.; Weisband, S.P. Understanding process knowledge change in enterprise system implementation: A framework and case study. In Proceedings of the 11th Americas Conference on Information Systems, Omaha, NE, USA, 11–14 August 2005. [Google Scholar]
- Syafar, F.; Husain, H. Development of an integrated framework for successful adoption and implementation of mobile collaboration technology in indonesian healthcare. In Proceedings of the 30th IBIMA (International Business Information Management Association) Conference, Madrid, Spain, 8–9 November 2017; Available online: https://ibima.org/accepted-paper/development-of-an-integrated-framework-for-successful-adoption-and-implementation-of-mobile-collaboration-technology-in-indonesian-healthcare/ (accessed on 23 May 2024).
- Jahangirian, M.; E Taylor, S.J.; Young, T.; Robinson, S. Key performance indicators for successful simulation projects. J. Oper. Res. Soc. 2017, 68, 747–765. [Google Scholar] [CrossRef]
- Han, Y. The impact of accountability deficit on agency performance: Performance-accountability regime. Public Manag. Rev. 2019, 22, 927–948. [Google Scholar] [CrossRef]
- Chakravorty, T.; Jha, K.; Barthwal, S. Linking EHR and ERP Adoption with Flexibility in Care-Delivery and Operational Performance: A Conceptual Review in Hospital Supply Chain. Indian J. Public Health Res. Dev. 2019, 10, 102. [Google Scholar] [CrossRef]
- Øverdal, M.; Haddara, M.; Langseth, M. Exploring public cloud-ERP systems’ impact on organizational performance. In The Future Technologies Conference (FTC); Springer: Cham, Switzerland, 2023. [Google Scholar]
- Rokade, P.N. Optimizing Healthcare System: A Comprehensive Study on the Integration of Enterprise Resource Planning (ERP) in the Healthcare Sector. Int. J. Adv. Res. Sci. Commun. Technol. India 2023, 529–540. [Google Scholar] [CrossRef]
- Wieder, B.; Booth, P.; Matolcsy, Z.P.; Ossimitz, M. The impact of ERP systems on firm and business process performance. J. Enterp. Inf. Manag. 2006, 19, 13–29. [Google Scholar] [CrossRef]
- Ben Fradj, A.; El Asli, N.; Boukherroub, T.; Olivier, C. Developing an integrated performance management and measurement system in healthcare organisations: A Canadian case study. F1000Research 2023, 12, 1420. [Google Scholar] [CrossRef]
- Utami, F.D.; Puspitasari, W.; Saputra, M. Design of planning model for ERP system in warehouse management: An empirical study of public hospital in indonesia. IOP Conf. Ser. Mater. Sci. Eng. 2020, 909, 012061. [Google Scholar] [CrossRef]
- Wijaya, S.F.; Wiratama, J.; Kuswanto, V. An Evaluation of Integrating ERP System to Develop a Strategy Business. In Proceedings of the 2023 International Conference on Information Management and Technology (ICIMTech), Malang, Indonesia, 24–25 August 2023. [Google Scholar] [CrossRef]
- Karim, M.R.; Nordin, N.; Yusof, M.F.; Bin Amin, M.; Islam, A.; Hassan, S. Does ERP implementation mediate the relationship between knowledge management and the perceived organizational performance of the healthcare sector? Evidence from a developing country. Cogent Bus. Manag. 2023, 10, 2275869. [Google Scholar] [CrossRef]
- Hwang, Y.; Lee, Y.; Shin, D.-H. The role of goal awareness and information technology self-efficacy on job satisfaction of healthcare system users. Behav. Inf. Technol. 2016, 35, 548–558. [Google Scholar] [CrossRef]
- Abukhader, S.M. ERP implementation in the private hospitals of Saudi Arabia. Int. J. Healthc. Manag. 2015, 8, 77–88. [Google Scholar] [CrossRef]
- Neely, A.; Gregory, M.; Platts, K. Performance measurement system design: A literature review andresearch agenda. Int. J. Oper. Prod. Manag. 1995, 15, 80–116. [Google Scholar] [CrossRef]
- Ayre, B.A.; Scally, A.J. Critical Values for Lawshe’s Content Validity Ratio: Revisiting the Original Methods of Calculation. 2014. Available online: http://hdl.handle.net/10454/8362 (accessed on 23 May 2024).
- Jeldres, M.R.; Costa, E.D.; Nadim, T.F. A review of Lawshe’s method for calculating content validity in the social sciences. Front. Educ. 2023, 8, 1271335. [Google Scholar] [CrossRef]
- Tessema, A.T. Assessment of Risk Management Practice in Construction Projects Using RII Method. SSRN Electron. J. 2022, 8, 1–11. [Google Scholar] [CrossRef]
- Makwana, D.; Engineer, P.; Dabhi, A.; Chudasama, H. Sampling Methods in Research: A Review. Int. J. Trend Sci. Res. Dev. 2023, 7, 762–768. [Google Scholar]
- Mahmoud, H.; Ahmed, V.; Beheiry, S. Construction cash flow risk index. J. Risk Financ. Manag. 2021, 14, 269. [Google Scholar] [CrossRef]
- Momani, A.M. The Unified Theory of Acceptance and Use of Technology: A New Approach in Technology Acceptance. Int. J. Sociotechnol. Knowl. Dev. 2020, 12, 79–98. [Google Scholar] [CrossRef]
| Stages | Steps | Process |
|---|---|---|
| Stage 1: Factor validation Semi-structured interview One-to-one interviews with healthcare experts in the decision-making process | 1 | Understand the current situation of ERP system implementation within the healthcare sector |
| 2 | Ask experts to verify the list of factors extracted from the literature review based on their relevance within the healthcare sector in UAE and recommend factors that impact the integration of ERP and PM, their importance, as well as additional factors as they see fit | |
| 3 | Consolidate responses from all experts and finalize the shortlisted factors | |
| 4 | Validate the responses using Content Validity Ratio (CVR) | |
| Stage 2: Expert importance rating of factors Online survey sent to healthcare administration experts that utilize the ERP systems in healthcare | 1 | The consolidated list of factors is shared with the experts in the administrative departments in healthcare organizations to rate each factor based on its importance 1 = Very low importance 2 = Low importance 3 = Moderate importance 4 = High importance 5 = Very high importance |
| 2 | Refine consolidated list to remove low rating factors | |
| Stage 3: Factor ranking Online survey sent to the original experts interviewed in phase 1 | 1 | Confirm the rating of the factors with the experts in phase 1 |
| 2 | Publish the final list of factors and their RII | |
| Development of the main contribution | To develop a set of recommended guidelines that guide healthcare organizations to facilitate a seamless connection between these systems, enhancing operational efficiencies and improving overall healthcare delivery | |
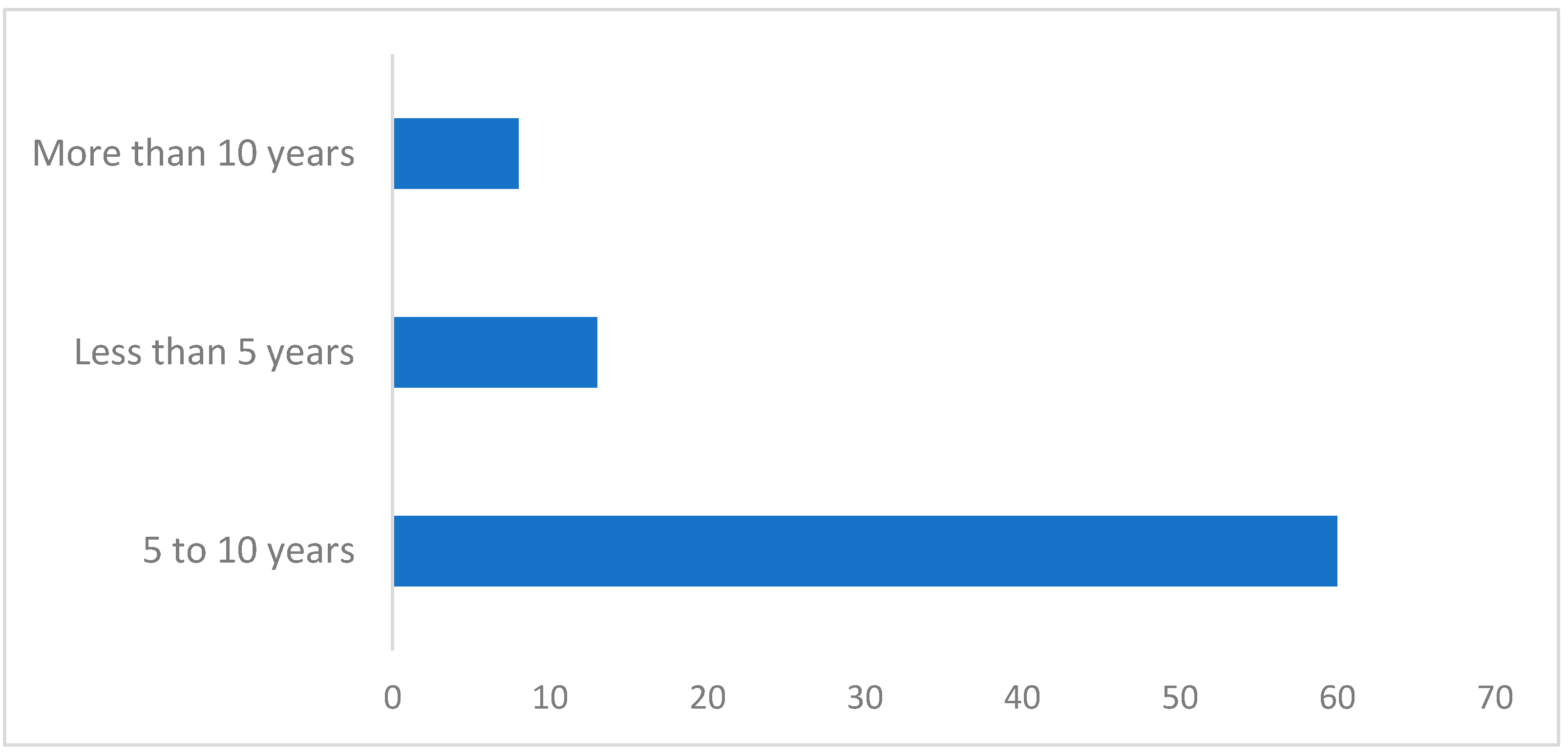
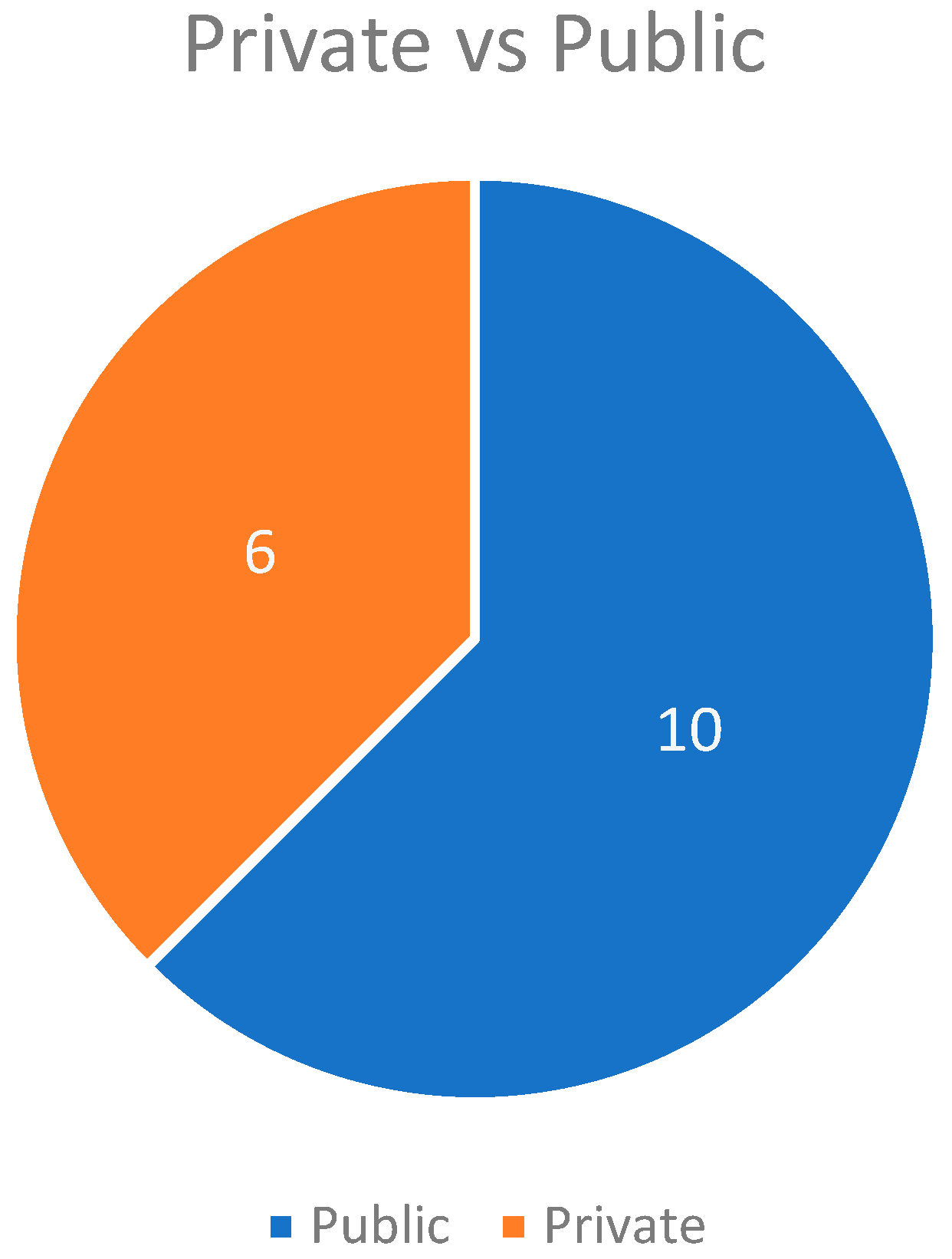
| Sr | Participant | Designation | Organization | Years of Experience |
|---|---|---|---|---|
| 1 | Participant 1 | Senior IT developer | Public | 17 |
| 2 | Participant 2 | Consultant (healthcare solutions and user experience) | Private | 6 |
| 3 | Participant 3 | Supply chain and ERP expert | Private | 5 |
| 4 | Participant 4 | CEO of healthcare solution provider | Private | 14 |
| 5 | Participant 5 | Head of healthcare solution | Public | 25 |
| 6 | Participant 6 | Senior systems analyst | Private | 15 |
| Sr | ERP Factors | CVR | PM Factors | CVR |
|---|---|---|---|---|
| 1 | Readiness of healthcare organization to adopt and accommodate ERP system | 1.0 | Access to accurate and timely real information | 1.0 |
| 2 | Availability of financial resources to invest in system direct and indirect cost | 0.7 | Availability of performance metrics and measurement tools | 1.0 |
| 3 | Availability of system-wide integration to reduce silos | 1.0 | Clear long-term goals and objectives | 0.7 |
| 4 | Availability of top management support | 1.0 | Availability of patient-centered metrics | 1.0 |
| 5 | Clear objectives and requirements for ERP system implementation | 0.7 | Effective leadership | 1.0 |
| 6 | Source of the ERP system | 1.0 | Managerial support and involvement | 1.0 |
| 7 | Chosen implementation strategy | 1.0 | Employee involvement and engagement in designing performance metrics | 1.0 |
| 8 | Presence of effective change management plan | 1.0 | Effectiveness of organizational individual | 1.0 |
| 9 | Alignment of ERP systems with business processes | 1.0 | Effectiveness of performance measurement system | 1.0 |
| 10 | Vendor support and expertise | 1.0 | Alignment with organizational culture, strategy, and structure | 1.0 |
| 11 | Availability of data quality and migration process | 1.0 | Responsiveness to market dynamics, customer demands, and competitive landscapes | 0.3 |
| 12 | User involvement and training during implementation | 1.0 | Level of organizational technological improvements in performance measurement | 0.7 |
| 13 | Customization overload | −1.0 | Organizational efficiency in success use of hospital management resources | 1.0 |
| 14 | Technical competence of employee | 0.7 | Effectiveness of the overall outcomes of a healthcare service | 1.0 |
| 15 | Readiness for integration | 1.0 | Flexibility and system’s adaptability to change | 0.7 |
| 16 | Availability of project management plan with clear timelines, the establishment of key milestones, and the delineation of responsibilities | 1.0 | Availability of key performance indicators | 1.0 |
| 17 | Adherence to regulatory compliance and standards | 0.7 | Availability of follow-up and accountability system | 1.0 |
| 18 | Current technological infrastructure of the healthcare facility | 1.0 | ||
| 19 | Availability of balance security requirement and compliance | 1.0 |
| Sr | Additional Factors |
|---|---|
| 1 | Ease of ERP system scalability |
| 2 | Transparency of data sharing in ERP systems |
| Factors | RII | Rank |
|---|---|---|
| Effectiveness of organizational individual performance measures (quality, time, cost, and flexibility) | 0.8963 | 1 |
| Employee involvement and engagement in designing performance metrics | 0.8667 | 2 |
| Effectiveness of performance measurement system (alignment of individual measures with overarching goals, maintaining balance among varying metric) | 0.8667 | 2 |
| Availability of performance metrics and measurement tools | 0.8642 | 4 |
| Readiness for integration | 0.8568 | 5 |
| User Involvement and training during implementation | 0.8568 | 5 |
| Clear long-term goals and objectives | 0.8519 | 7 |
| Effective leadership | 0.8494 | 8 |
| Managerial support and involvement | 0.8444 | 9 |
| Availability of follow-up and accountability system | 0.8444 | 9 |
| Access to accurate and timely real information | 0.8420 | 11 |
| Availability of data quality and migration process | 0.8321 | 12 |
| Organizational efficiency in success use of hospital management resources | 0.8296 | 13 |
| Availability of patient-centered metrics | 0.8272 | 14 |
| Availability of key performance indicators | 0.8272 | 14 |
| Alignment of ERP systems with business processes | 0.8272 | 14 |
| Alignment with organizational culture, strategy, and structure | 0.8173 | 17 |
| Effectiveness of the overall outcomes of a healthcare service | 0.8173 | 17 |
| Vendor support and expertise | 0.8173 | 17 |
| Chosen implementation strategy | 0.8148 | 20 |
| Availability of balance security requirement and compliance | 0.8148 | 20 |
| Transparency of data sharing in ERP systems | 0.8074 | 22 |
| Source of the ERP system | 0.8074 | 22 |
| Ease of ERP system scalability | 0.8025 | 24 |
| Readiness of healthcare organizations to adopt and accommodate ERP system | 0.8025 | 24 |
| Availability of top management support | 0.8000 | 26 |
| Presence of effective change management plan | 0.7951 | 27 |
| Availability of system-wide integration to reduce silos | 0.7951 | 27 |
| Current technological infrastructure of the healthcare facility | 0.7926 | 29 |
| Adherence to regulatory compliance and standards | 0.7901 | 30 |
| Availability of project management plan with clear timelines, the establishment of key milestones, and the delineation of responsibilities | 0.7852 | 31 |
| Responsiveness to market dynamics, customer demands, and competitive landscapes | 0.7802 | 32 |
| Level of organizational technological improvements in performance measurement | 0.7753 | 33 |
| Flexibility and system’s adaptability to change | 0.7704 | 34 |
| Customization overload | 0.7630 | 35 |
| Availability of financial resources to invest in system direct and indirect cost | 0.7556 | 36 |
| Clear objectives and requirements for ERP system implementation | 0.7531 | 37 |
| Technical competence of employee | 0.7481 | 38 |
| Factors | Rank |
|---|---|
| Effectiveness of organizational individual performance measures (quality, time, cost, and flexibility) | 1 |
| Employee involvement and engagement in designing performance metrics | 2 |
| Effectiveness of performance measurement system (alignment of individual measures with overarching goals, maintaining balance among varying metric) | 2 |
| Availability of performance metrics and measurement tools | 4 |
| Readiness for integration | 5 |
| User involvement and training during implementation | 5 |
| Clear long-term goals and objectives | 7 |
| Effective leadership | 8 |
| Managerial support and involvement | 9 |
| Availability of follow-up and accountability system | 9 |
| Access to accurate and timely real information | 11 |
| Availability of data quality and migration process | 12 |
| Organizational efficiency in success use of hospital management resources | 13 |
| Availability of patient-centered metrics | 14 |
| Availability of key performance indicators | 14 |
| Alignment of ERP systems with business processes | 14 |
| Alignment with organizational culture, strategy, and structure | 17 |
| Effectiveness of the overall outcomes of a healthcare service | 17 |
| Vendor support and expertise | 17 |
| Chosen implementation strategy | 20 |
| Availability of balance security requirement and compliance | 20 |
| Transparency of data sharing in ERP systems | 22 |
| Source of the ERP system | 22 |
| Ease of ERP system scalability | 24 |
| Readiness of healthcare organizations to adopt and accommodate ERP system | 24 |
| Availability of top management support | 26 |
| Presence of effective change management plan | 27 |
| Availability of system-wide integration to reduce silos | 27 |
| Current technological infrastructure of the healthcare facility | 29 |
| Adherence to regulatory compliance and standards | 30 |
| Availability of project management plan with clear timelines, the establishment of key milestones, and the delineation of responsibilities | 31 |
| Responsiveness to market dynamics, customer demands, and competitive landscapes | 32 |
| Level of organizational technological improvements in performance measurement | 33 |
| Flexibility and system’s adaptability to change | 34 |
| Customization overload | 35 |
| Availability of financial resources to invest in system direct and indirect cost | 36 |
| Clear objectives and requirements for ERP system implementation | 37 |
| Technical competence of employee | 38 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Assaf, K.; Alzahmi, W.; Alshaikh, R.; Bahroun, Z.; Ahmed, V. The Relative Importance of Key Factors for Integrating Enterprise Resource Planning (ERP) Systems and Performance Management Practices in the UAE Healthcare Sector. Big Data Cogn. Comput. 2024, 8, 122. https://doi.org/10.3390/bdcc8090122
Al-Assaf K, Alzahmi W, Alshaikh R, Bahroun Z, Ahmed V. The Relative Importance of Key Factors for Integrating Enterprise Resource Planning (ERP) Systems and Performance Management Practices in the UAE Healthcare Sector. Big Data and Cognitive Computing. 2024; 8(9):122. https://doi.org/10.3390/bdcc8090122
Chicago/Turabian StyleAl-Assaf, Karam, Wadhah Alzahmi, Ryan Alshaikh, Zied Bahroun, and Vian Ahmed. 2024. "The Relative Importance of Key Factors for Integrating Enterprise Resource Planning (ERP) Systems and Performance Management Practices in the UAE Healthcare Sector" Big Data and Cognitive Computing 8, no. 9: 122. https://doi.org/10.3390/bdcc8090122
APA StyleAl-Assaf, K., Alzahmi, W., Alshaikh, R., Bahroun, Z., & Ahmed, V. (2024). The Relative Importance of Key Factors for Integrating Enterprise Resource Planning (ERP) Systems and Performance Management Practices in the UAE Healthcare Sector. Big Data and Cognitive Computing, 8(9), 122. https://doi.org/10.3390/bdcc8090122







