A Review of Artificial Intelligence, Big Data, and Blockchain Technology Applications in Medicine and Global Health
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Types of Machine Learning Applications
3.2. Blockchain Technology in Healthcare
Classification of Blockchain Applications
- -
- Integration concerns and initial cost;
- -
- Identity, security, and privacy;
- -
- Standardization;
- -
- Cultural adoption;
- -
- Uncertain regulatory and compliance status.
3.3. Artificial Intelligence and Big Data Analytics Tools and Techniques
3.4. Mobile Health
3.5. Personalized Health Using Machine Learning over Big Data and IoT
4. Discussion
4.1. Heart Disease Prediction
4.2. Alzheimer’s Disease Prediction
4.3. Bioinspired Algorithms Used in Healthcare
4.4. Cancer Diagnosis
4.5. Parkinson’s Disease Diagnosis
4.6. COVID-19 Disease Prediction
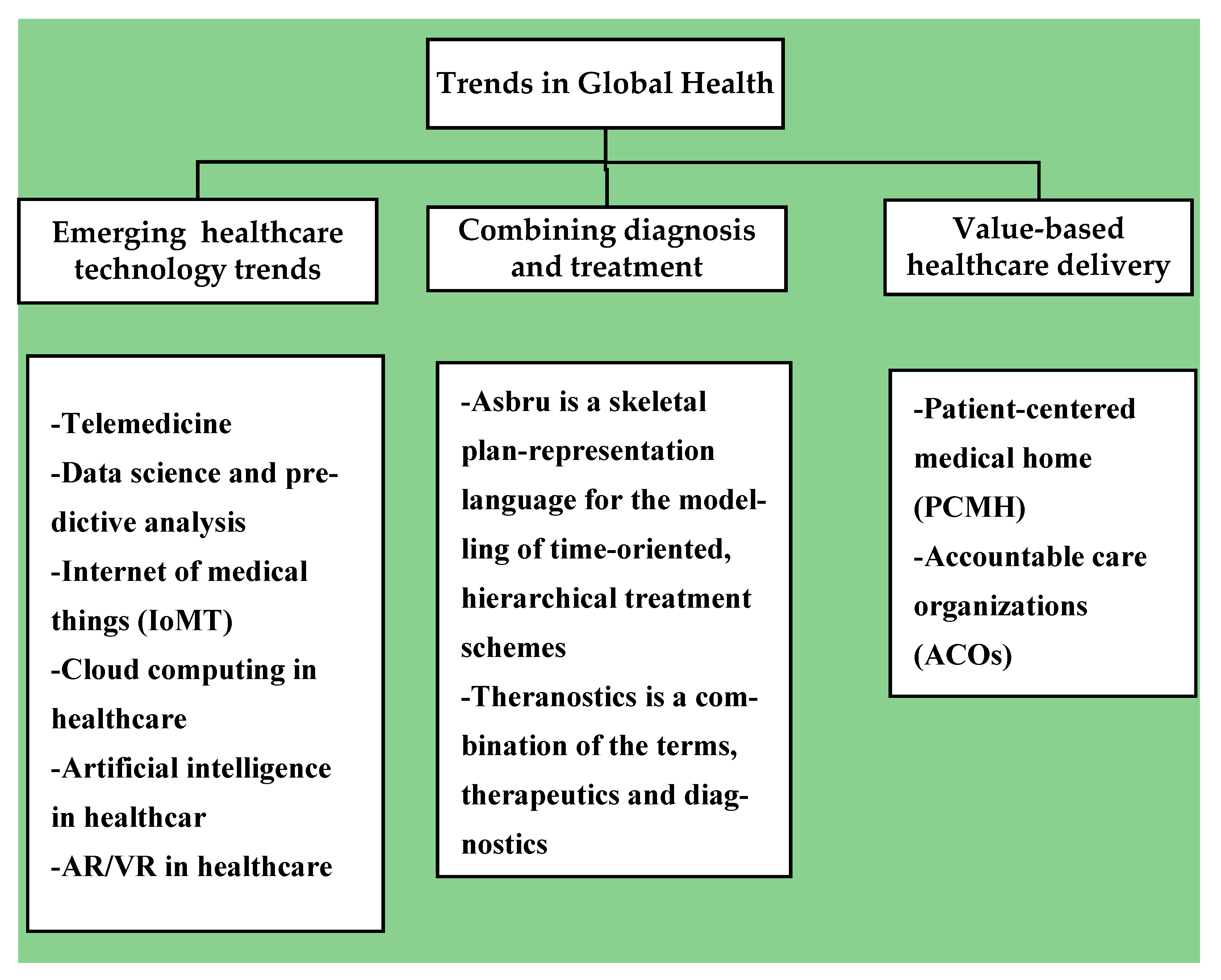
4.7. Trends in Global Health
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dash, S.; Shakyawar, S.K.; Sharma, M.; Sandeep, K. Big data in healthcare: Management, analysis and future prospects. J. Big Data 2019, 6, 1–25. [Google Scholar] [CrossRef] [Green Version]
- Anirudh, V.K. What Is Machine Learning: Definition, Types, Applications and Examples. 13 December 2019. Available online: https://www.toolbox.com/tech/artificial-intelligence/tech-101/what-is-machine-learning-definition-types-applications-and-examples/ (accessed on 24 December 2020).
- Yoon, H.-J. Blockchain Technology and Healthcare. Health Inform. Res. 2019, 25, 59–60. [Google Scholar] [CrossRef]
- Chen, H.S.; Jarrell, J.T.; Carpenter, K.A.; Cohen, D.S.; Huang, X. Blockchain in Healthcare: A Patient-Centered Model. Biomed. J. Sci. Tech. Res. 2019, 20, of15017. [Google Scholar]
- Clohessy, T.; Hasselgren, A.; El-Gazzar, R.; Stendal, K. Blockchain in Health Care: Hope or Hype? J. Med. Internet Res. 2020, 22, e17199. [Google Scholar] [CrossRef]
- Flatworld Solutions. Top 10 Applications of Machine Learning in Healthcare. Available online: https://www.flatworldsolutions.com/healthcare/articles/top-10-applications-of-machine-learning-in-healthcare.php (accessed on 2 January 2021).
- Tandon, A.; Dhir, A.; Islam, N.; Mäntymäki, M. Blockchain in healthcare: A systematic literature review, synthesizing framework and future research agenda. Comput. Ind. 2020, 122, 103290. [Google Scholar] [CrossRef]
- Sadiku, M.N.O.; Eze, K.G.; Musa, S.M. Block chain Technology in Healthcare. Int. J. Adv. Sci. Res. Eng. 2018, 4, 154–159. [Google Scholar] [CrossRef]
- Cernian, A.; Tiganoaia, B.; Sacala, I.; Pavel, A.; Iftemi, A. Patient Data Chain: A Block-chain-Based Approach to Integrate Personal Health Records. Sensors 2020, 20, 6538. [Google Scholar] [CrossRef]
- Tith, D.; Lee, J.S.; Suzuki, H.; Wijesundara, W.M.A.B.; Taira, N.; Obi, T.; Ohyama, N. Patient consent management by a purpose-based consent model for electronic health record based on blockchain technology. Healthc. Inform. Res. 2020, 26, 265–273. [Google Scholar] [CrossRef]
- Benke, K.; Benke, G. Artificial intelligence and big data in public health. Int. J. Environ. Res. Public Health 2018, 15, 2796. [Google Scholar] [CrossRef] [Green Version]
- Kaur, P.; Sharma, M.; Mittal, M. Big Data and Machine Learning Based Secure Healthcare Framework. Procedia Comput. Sci. 2018, 132, 1049–1059. [Google Scholar] [CrossRef]
- Milward, J. What Is Mobile Health? 20 May 2019. Available online: https://www.addiction-ssa.org/knowledge-hub/what-is-mobile-health (accessed on 23 January 2021).
- Khan, Z.F.; Alotaibi, S.R. Applications of Artificial Intelligence and Big Data Analytics in m-Health: A Healthcare System Perspective. J. Health Eng. 2020, 2020, 1–15. [Google Scholar] [CrossRef]
- Nafis, M.T.; Urooj, A.; Biswas, S.S. Recent Machine Learning and Internet of Things (IoT) Applications for Personalized Healthcare: Issues and Challenges. In Sustainable and Energy Efficient Computing Paradigms for Society; Ahad, M., Paiva, S., Zafar, S., Eds.; EAI/Springer Innovations in Communication and Computing: Cham, Switzerland, 2021; pp. 119–126. [Google Scholar] [CrossRef]
- Ed-daoudy, A.; Maalmi, K. A new Internet of Things architecture for real-time prediction of various diseases using machine learning on big data environment. J. Big Data 2019, 6, 1–25. [Google Scholar] [CrossRef]
- Siddiqui, S.; Nesbitt, R.; Shakir, M.Z.; Khan, A.A.; Khan, A.A.; Khan, K.K.; Ramzan, N. Artificial Neural Network (ANN) Enabled Internet of Things (IoT) Architecture for Music Therapy. Electronics 2020, 9, 2019. [Google Scholar] [CrossRef]
- Abdelaziz, A.; Salama, A.S.; Riad, A.M.; Mahmoud, A.N. A machine learning model for predicting of chronic kidney disease based internet of things and cloud computing in smart cities. In Security in Smart Cities: Models, Applications, and Challenges; Springer: Cham, Switzerland, 2019; pp. 93–114. [Google Scholar]
- Almakhadmeh, Z.; Tolba, A. Utilizing IoT wearable medical device for heart disease prediction using higher order Boltzmann model: A classification approach. Measurement 2019, 147, 106815. [Google Scholar] [CrossRef]
- Sivaparthipan, C.; Muthu, B.A.; Manogaran, G.; Maram, B.; Sundarasekar, R.; Krishnamoorthy, S.; Hsu, C.; Chandran, K. Innovative and efficient method of robotics for helping the Parkinson’s disease patient using IoT in big data analytics. Trans. Emerg. Telecommun. Technol. 2019, 31, e3838. [Google Scholar] [CrossRef]
- Grossfield’s, B. Deep Learning VS. Machine Learning: A Simple Way to Learn the Difference. 23 January 2020. Available online: https://www.zendesk.com/blog/machine-learning-and-deep-learning (accessed on 30 January 2021).
- What Is Heart Disease? Heart Disease (for Kids)—Nemours Kidshealth. Available online: https://kidshealth.org/en/kids/heart-disease.html (accessed on 31 July 2021).
- Amin, M.S.; Chiam, Y.K.; Varathan, K.D. Identification of significant features and data mining techniques in predicting heart disease. Telemat. Inform. 2018, 36, 82–93. [Google Scholar] [CrossRef]
- Dua, D.; Karra Taniskidou, E. UCI Machine Learning Repository. Master’s Thesis, School of Information and Computer Science, University of California, Irvine, CA, USA, 2017. [Google Scholar]
- Mohan, S.; Thirumalai, C.; Srivastava, G. Effective Heart Disease Prediction Using Hybrid Machine Learning Techniques. IEEE Access 2019, 7, 81542–81554. [Google Scholar] [CrossRef]
- Archana, S.; Kumar, R. Heart disease prediction using machine learning algorithms. In Proceedings of the 2020 International Conference on Electrical and Electronics Engineering (ICE3), Fargo, ND, USA, 14–15 February 2020; pp. 452–457. [Google Scholar]
- Haq, A.U.; Li, J.P.; Memon, M.H.; Nazir, S.; Sun, R. A Hybrid Intelligent System Framework for the Prediction of Heart Disease Using Machine Learning Algorithms. Mob. Inf. Syst. 2018, 2018, 1–21. [Google Scholar] [CrossRef]
- Saba, B.; Khan, Z.S.; Khan, F.H.; Anjum, A.; Bashir, K. Improving heart disease prediction using feature selection approaches. In Proceedings of the 2019 16th International Bhurban Conference on Applied Sciences and Technology (IBCAST), Islamabad, Pakistan, 8–12 January 2019; pp. 619–623. [Google Scholar]
- Krittanawong, C.; Rogers, A.J.; Aydar, M.; Choi, E.; Johnson, K.W.; Wang, Z.; Narayan, S.M. Integrating blockchain technology with artificial intelligence for cardiovascular medicine. Nat. Rev. Cardiol. 2019, 17, 1–3. [Google Scholar] [CrossRef]
- Jo, T.; Nho, K.; Saykin, A.J. Deep learning in Alzheimer’s disease: Diagnostic classification and prognostic prediction using neuroimaging data. Front. Aging Neurosci. 2019, 11, 220. [Google Scholar] [CrossRef] [Green Version]
- Sharma, A.; Shukla, D.; Goel, T.; Mandal, P.K. BHARAT: An Integrated Big Data Analytic Model for Early Diagnostic Biomarker of Alzheimer’s Disease. Front. Neurol. 2019, 10, 9. [Google Scholar] [CrossRef]
- Lin, W.; Tong, T.; Gao, Q.; Guo, D.; Du, X.; Yang, Y.; Guo, G.; Xiao, M.; Du, M.; Qu, X.; et al. Convolutional neural networks-based MRI image analysis for the Alzheimer’s disease prediction from mild cognitive impairment. Front. Neurosci. 2018, 12, 777. [Google Scholar] [CrossRef]
- Fischl, B.; Dale, A.M. Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc. Natl. Acad. Sci. USA 2000, 97, 11050–11055. [Google Scholar] [CrossRef] [Green Version]
- Fischl, B.; Van Der Kouwe, A.; Destrieux, C.; Halgren, E.; Ségonne, F.; Salat, D.H.; Busa, E.; Seidman, L.J.; Goldstein, J.; Kennedy, D.; et al. Automatically Parcellating the Human Cerebral Cortex. Cereb. Cortex 2004, 14, 11–22. [Google Scholar] [CrossRef] [Green Version]
- Desikan, R.S.; Ségonne, F.; Fischl, B.; Quinn, B.T.; Dickerson, B.C.; Blacker, D.; Buckner, R.L.; Dale, A.M.; Maguire, R.P.; Hyman, B.T.; et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 2006, 31, 968–980. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Jovicich, J.; Salat, D.; van der Kouwe, A.; Quinn, B.; Czanner, S.; Busa, E.; Pacheco, J.; Albert, M.; Killiany, R.; et al. Reliability of MRI-derived measurements of human cerebral cortical thickness: The effects of field strength, scanner upgrade and manufacturer. NeuroImage 2006, 32, 180–194. [Google Scholar] [CrossRef] [PubMed]
- Kautzky, A.; Seiger, R.; Hahn, A.; Fischer, P.; Krampla, W.; Kasper, S.; Kovacs, G.G.; Lanzenberger, R. Prediction of autopsy verified neuropathological change of Alzheimer’s disease using machine learning and MRI. Front. Aging Neurosci. 2018, 10, 406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almubark, I.; Chang, L.-C.; Nguyen, T.; Turner, R.S.; Jiang, X. Early Detection of Alzheimer’s Disease Using Patient Neuropsychological and Cognitive Data and Machine Learning Techniques. In Proceedings of the 2019 IEEE International Conference on Big Data (Big Data), Los Angeles, CA, USA, 9–12 December 2019; pp. 5971–5973. [Google Scholar] [CrossRef]
- Pilozzi, A.; Huang, X. Overcoming Alzheimer’s Disease Stigma by Leveraging Artificial Intelligence and Blockchain Technologies. Brain Sci. 2020, 10, 183. [Google Scholar] [CrossRef] [Green Version]
- Darwish, A. Bio-inspired computing: Algorithms review, deep analysis, and the scope of applications. Futur. Comput. Inform. J. 2018, 3, 231–246. [Google Scholar] [CrossRef]
- Ghoniem, R.M. A Novel Bio-Inspired Deep Learning Approach for Liver Cancer Diagnosis. Information 2020, 11, 80. [Google Scholar] [CrossRef] [Green Version]
- Elgin Christo, V.R.; Khanna Nehemiah, H.; Minu, B.; Kannan, A. Correlation-Based Ensemble Feature Se-lection Using Bioinspired Algorithms and Classification Using Backpropagation Neural Network. Comput. Math. Methods Med. 2019, 1–17. [Google Scholar] [CrossRef]
- Supriya, M.; Deepa, A.J. A novel approach for breast cancer prediction using optimized ANN classifier based on big data environment. Heal. Care Manag. Sci. 2019, 23, 414–426. [Google Scholar] [CrossRef]
- Sharma, M.; Gupta, S.; Sharma, P.; Gupta, D. Bio-inspired algorithms for diagnosis of breast cancer. Int. J. Innov. Comput. Appl. 2019, 10, 164–174. [Google Scholar] [CrossRef]
- Valluru, D.; Jeya, I.J.S. IoT with cloud based lung cancer diagnosis model using optimal support vector machine. Health Care Manag. Sci. 2020, 23, 670–679. [Google Scholar] [CrossRef] [PubMed]
- Olivares, R.; Munoz, R.; Soto, R.; Crawford, B.; Cárdenas, D.; Ponce, A.; Taramasco, C. An Optimized Brain-Based Algorithm for Classifying Parkinson’s Disease. Appl. Sci. 2020, 10, 1827. [Google Scholar] [CrossRef] [Green Version]
- Sharma, P.; Sundaram, S.; Sharma, M.; Sharma, A.; Gupta, D. Diagnosis of Parkinson’s disease using modified grey wolf optimization. Cogn. Syst. Res. 2018, 54, 100–115. [Google Scholar] [CrossRef]
- Hessam, S.; Vahdat, S.; Asl, I.M.; Kazemipoor, M.; Aghaei, A.; Shamshirband, S.; Rabczuk, T. Parkinson’s Disease Detection Using Biogeography-Based Optimization. Comput. Mater. Contin. 2019, 61, 11–26. [Google Scholar] [CrossRef]
- Pasha, A.; Latha, P.H. Bio-inspired dimensionality reduction for Parkinson’s disease (PD) classification. Health Inf. Sci. Syst. 2020, 8, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Jain, R.; Sharma, M.; Gupta, D. Parkinson’s diagnosis using ant-lion optimisation algorithm. Int. J. Innov. Comput. Appl. 2019, 10, 138–146. [Google Scholar] [CrossRef]
- Hosseini, E.; Ghafoor, K.Z.; Sadiq, A.S.; Guizani, M.; Emrouznejad, A. COVID-19 Optimizer Algorithm, Modeling and Controlling of Coronavirus Distribution Process. IEEE J. Biomed. Health Inform. 2020, 24, 2765–2775. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Basset, M.; Mohamed, R.; Elhoseny, M.; Chakrabortty, R.K.; Ryan, M. A Hybrid COVID-19 Detection Model Using an Improved Marine Predators Algorithm and a Ranking-Based Diversity Reduction Strategy. IEEE Access 2020, 8, 79521–79540. [Google Scholar] [CrossRef]
- Altan, A.; Karasu, S. Recognition of COVID-19 disease from X-ray images by hybrid model consisting of 2D curvelet transform, chaotic salp swarm algorithm and deep learning technique. Chaos Solitons Fractals 2020, 140, 110071. [Google Scholar] [CrossRef]
- Al-Qaness, M.A.; Ewees, A.A.; Fan, H.; Abd El Aziz, M. Optimization method for fore-casting confirmed cases of COVID-19 in China. J. Clin. Med. 2020, 9, 674. [Google Scholar] [CrossRef] [Green Version]
- ELGhamrawy, S.M. Diagnosis and Prediction Model for COVID19 Patients Response to Treatment based on Convolutional Neural Networks and Whale Optimization Algorithm Using CT Images. MedRxiv 2020, 1–23. [Google Scholar] [CrossRef] [Green Version]
- Kumar, R.; Wang, W.; Kumar, J.; Yang, T.; Khan, A.; Ali, W.; Ali, I. An Integration of blockchain and AI for secure data sharing and detection of CT images for the hospitals. Comput. Med. Imaging Graph. 2020, 87, 101812. [Google Scholar] [CrossRef] [PubMed]
- Simon, D. Biogeography-based optimization. IEEE Trans. Evol. Comput. 2008, 12, 702–713. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.S. Flower pollination algorithm for global optimization. In Proceedings of the International Conference on Unconventional Computing and Natural Computation, Orléans, France, 3–7 September 2012; pp. 240–249. [Google Scholar]
- Mirjalili, S.; Gandomi, A.H.; Mirjalili, S.Z.; Saremi, S.; Faris, H.; Mirjalili, S.M. Salp Swarm Algorithm: A bio-inspired optimizer for engineering design problems. Adv. Eng. Softw. 2017, 114, 163–191. [Google Scholar] [CrossRef]
- Mirjalili, S.; Lewis, A. The whale optimization algorithm. Adv. Eng. Softw. 2016, 95, 51–67. [Google Scholar] [CrossRef]
- Fusco, A.; Dicuonzo, G.; Dell’Atti, V.; Tatullo, M. Blockchain in healthcare: Insights on COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 7167. [Google Scholar] [CrossRef]
- Sadiku, M.N.; Akhare, Y.P.; Musa, S.M. Emerging technologies in healthcare: A tutorial. Int. J. Adv. Sci. Res. Eng. (IJASRE) 2019, 5, 199–204. [Google Scholar] [CrossRef]
- Seyfang, A.; Miksch, S.; Marcos, M. Combining diagnosis and treatment using ASBRU. Int. J. Med. Inform. 2002, 68, 49–57. [Google Scholar] [CrossRef] [Green Version]
- Filippi, L.; Chiaravalloti, A.; Schillaci, O.; Cianni, R.; Bagni, O. Theranostic approaches in nuclear medicine: Current status and future prospects. Expert Rev. Med. Devices 2020, 17, 331–343. [Google Scholar] [CrossRef] [PubMed]
- NEJM Catalyst. What is Value-Based healthcare? 1 January 2017. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0558 (accessed on 31 July 2021).
- Jolles, M.P.; Lengnick-Hall RMittman, B.S. Core functions and forms of complex health interventions: A patient-centered medical home illustration. J. Gen. Intern. Med. 2019, 34, 1032–1038. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Sl. No | Applications | Examples | Technology |
|---|---|---|---|
| 1 | Medical Imaging Diagnosis | The goal of skin image analysis is to find skin cancer | Computer vision using deep learning |
| 2 | Smart Health Records | OCR recognition is based on machine learning and document categorization techniques that employ vector machines | Handwriting detection technique based on Google Cloud Vision API or Matlab machine learning |
| 3 | Identifying Diseases and Diagnosis | Therapeutic treatments in oncology | Watson Genomics is a product from IBM that combines cognitive computing with genome-based tumor sequencing |
| 4 | Crowdsourced Data Collection | IBM, in conjunction with Medtronic, to develop a platform that can understand, collect, and real-time exchange diabetes and insulin data | Apple’s Research Kit gives consumers access to interactive programs that employ machine learning to cure Asperger’s syndrome and Parkinson’s illness |
| 5 | Drug Discovery and Manufacturing | Biomarker discovery or validation | Deep Genomics uses artificial intelligence, especially deep learning, to help decipher the genome’s meaning |
| 6 | Better Radiotherapy | Medical image analysis | DeepMind Health, a division of Google, is assisting UCLH researchers in the development of algorithms that can distinguish between healthy and malignant cells |
| 7 | Tools for Risk Identification | El Camino Hospital researchers developed a method for forecasting patient falls by combining EHRs, nurse call data, and bed alarm data | Anomaly detection systems can anticipate catastrophic consequences, including strokes, heart attacks, and sepsis |
| 8 | Outbreak Prediction | Networks can aid in the interpretation of this data and the prediction of severe infectious disease epidemics, such as malaria | BlueDot is a specialized tool for tracking epidemics |
| 9 | Personalized Medicine | Based on patients’ clinical history and accessible genetic information, evaluate the danger to the patients | Improved medical technology to spot genetic mutations |
| 10 | Natural Language Processing | Review management and sentiment analysis | NLP-enabled systems that detect and categorize words and phrases using algorithms |
| S. No | Big Data Analytics Tools | Advantages | Disadvantages |
|---|---|---|---|
| 1 | “Xplenty“ is a cloud-based platform for integrating, processing, and preparing data for analytics. | Elasticity and scalability | There is just one billing option: yearly billing |
| 2 | “Apache Cassandra” is a distributed NoSQL database management system that is free and open-source. It is built to handle enormous amounts of data. | No single point of failure | It necessitates extra troubleshooting and maintenance work |
| 3 | “MongoDB” is a document-oriented, NoSQL database | Supports a variety of platforms and technologies | Limited analytics. |
| 4 | Apache “Hadoop” is a software framework for handling large data and clustered file systems | For R&D reasons, this is quite beneficial | Due to its 3× data redundancy, it is possible to run out of storage space |
| 5 | “Datawrapper” is a device-friendly open-source data visualization tool | Works great on any device, whether it’s a phone, a tablet, or a computer | Limited color palettes |
| 6 | “Rapidminer” is a cross-platform solution that combines machine learning and predictive analytics in a single environment | Excellent customer service and technical assistance | The quality of online data services has to be enhanced |
| 7 | “Tableau” is a business intelligence and analytics software application | It comes with a slew of useful features and is lightning fast | Formatting controls could be improved |
| 8 | “KNIME” is an open-source program that stands for Konstanz Information | It works nicely with various languages and technologies | MinerIt is possible to enhance data handling capabilities |
| 9 | Apache “Storm” is a distributed stream processing system that runs on several platforms | Extremely quick and fault-tolerant | Difficult to learn and use |
| 10 | “CDH” (Cloudera Distribution for Hadoop) is aimed at enterprise-class Hadoop implementations | High security and governance | Multiple installation methods are suggested, which seems perplexing |
| Sl.No | Author (Year) Reference No. | ML Algorithms | Parameters Evaluated | Efficiency (%) |
|---|---|---|---|---|
| 1 | Mohammad Shafenoor Amin et al. (2018) [23] | Vote with naive Bayes (NB) and logistic regression (LR) | Accuracy, precision, F-measure | Accuracy—87.41% |
| 2 | Senthilkumar Mohan et al. (2019) [25] | Random forest with linear model | Accuracy, classification error, Pprecision, F-measure, sensitivity, specificity | Accuracy—88.4% |
| 3 | Archana Singh & Rakesh Kumar (2020) [26] | K-nearest neighbor | Accuracy | Accuracy—87% |
| 4 | Amin Ul Haq et al. (2018) [27] | Logistic regression | Accuracy, MCC, AUC, processing time, sensitivity, specificity | Accuracy—89% |
| 5 | Saba Bashir et al. (2019) [28] | Logistic regression SVM | Accuracy | Accuracy—84.85% |
| 6 | Taeho Jo et al. (2019) [30] | Autoencoder (SAE), recurrent neural network (RNN) | Accuracy | Accuracy—98.8%; accuracy—96.0% |
| 7 | Ankita Sharma et al. (2019) [31] | Principle component analysis (PCA) | Sensitivity, specificity | Sensitivity—92%; specificity—94% |
| 8 | Weiming Lin et al. (2018) [32] | Convolutional neural network (CNN) | Accuracy, sensitivity, specificity, AUC | Accuracy—79.9%; AUC—86.1% |
| 9 | Alexander Kautzky et al. (2020) [37] | Random forest, support vector machines | Accuracy, sensitivity, specificity | Accuracy—77% |
| 10 | Ibrahim Almubark et al. (2019) [38] | Random forest (RF), support vector machine (SVM), gradient boosting (GB), and AdaBoost (AB) classifier | Sensitivity, specificity, accuracy | Accuracy—91.08%; accuracy—89.67% |
| Sl.No | Author (Year) Reference No | Database Used | Bioinspired Algorithms | Measured Parameters |
|---|---|---|---|---|
| 1. | Rania M. Ghoniem (2020) [41] | Radiopaedia and LiTS (Liver tumor segmentation challenge) dataset | Artificial bee colony optimization (ABC) algorithm | Specificity, F1-score, accuracy, and computational time |
| 2. | V. R. Elgin Christo et al. (2019) [42] | Wisconsin Diagnostic Breast Cancer (WDBC) dataset and hepatitis dataset | Lion optimization algorithm, differential evolution, and glowworm swarm optimization | Accuracy, precision, sensitivity, and specificity |
| 3. | M. Supriya &A. J. Deepa (2020) [43] | Wisconsin Breast Cancer Database (WBCD) | Gray wolf optimization (GWO) algorithm, modified dragonfly algorithm (MDF) | Accuracy, precision, recall |
| 4. | Moolchand Sharma et al. (2019) [44] | UCI Dataset of Wisconsin Diagnostic Breast Cancer | Particle swarm optimisation, artificial bee colony optimization, ant colony optimization, firefly algorithm | Accuracy |
| 5. | Dinesh Valluru & I.Jasmine Selvakumari Jeya (2019) [45] | Lung CT images from ELCAP Public Lung Image Database | Gray wolf optimization | Accuracy |
| 6. | Rodrigo Olivares et al. (2020) [46] | Parkinson’s disease audio dataset taken from UCI Machine Learning Repository | Bat algorithm | Accuracy, loss |
| 7. | Prerna Sharma et al. (2018) [47] | Real-time Parkinson handwritten and speech dataset | Modified gray wolf optimization (MGWO) | Accuracy, detection rate, false alarm rate |
| 8. | Somayeh Hessam et al. (2019) [48] | Parkinson disease dataset from UCI repository | Biogeography-based optimization (BBO) | Accuracy, rate of error (RMSE) convergence |
| 9. | Akram Pasha, and. Latha P. H (2020) [49] | Parkinson disease dataset from UCI repository | Genetic algorithm and binary particle swarm optimization | Accuracy, precision, recall, F-score |
| 10. | Prerna Sharma et al. (2019) [50] | Parkinson disease dataset from UCI repository | Antlion optimization (ALO) algorithm | Accuracy, computational time |
| 11. | Eghbal Hosseini et al. (2020) [51] | Benchmark functions of well-known optimization problems | COVID-19 optimizer algorithm (CVA) | Mean, standard deviation |
| 12. | Mohamed Abdel-basset et al. (2020) [52] | Images of the COVID-19 chest may be seen on GitHub. | Improved marine predators algorithm (IMPA) | Signal-to-noise ratio (SNR), standard deviation, peak signal-to-noise ratio (PSNR), universal quality index (UQI), structured similarity index metric (SSIM), |
| 13. | Aytaç Altan, and Seçkin Karasu (2020) [53] | 2905 real raw chest X-ray image dataset | Chaotic salp swarm algorithm (CSSA) | Accuracy, sensitivity, specificity, and time consumption |
| 14. | Mohammed A. A. Al-qaness et al. (2020) [54] | COVID-19 confirmed cases in China from 21 January to 18 February 2020 | Salp swarm algorithm (SSA), flower pollination algorithm (FPA) | Mean absolute percentage error (MAPE), mean absolute error (MAE), root mean squared relative error (RMSRE), root mean squared relative error (RMSRE), coefficient of determination (R2), CPU time |
| 15. | Sally Elghamrawy & Aboul Ella Hassanien (2020) [55] | 617 CT scans chest images collected from different resources | Whale optimization algorithm (WOA) | Accuracy, F-score, G-mean, and the area under the ROC curve (AUC) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
M., S.; Chattu, V.K. A Review of Artificial Intelligence, Big Data, and Blockchain Technology Applications in Medicine and Global Health. Big Data Cogn. Comput. 2021, 5, 41. https://doi.org/10.3390/bdcc5030041
M. S, Chattu VK. A Review of Artificial Intelligence, Big Data, and Blockchain Technology Applications in Medicine and Global Health. Big Data and Cognitive Computing. 2021; 5(3):41. https://doi.org/10.3390/bdcc5030041
Chicago/Turabian StyleM., Supriya, and Vijay Kumar Chattu. 2021. "A Review of Artificial Intelligence, Big Data, and Blockchain Technology Applications in Medicine and Global Health" Big Data and Cognitive Computing 5, no. 3: 41. https://doi.org/10.3390/bdcc5030041
APA StyleM., S., & Chattu, V. K. (2021). A Review of Artificial Intelligence, Big Data, and Blockchain Technology Applications in Medicine and Global Health. Big Data and Cognitive Computing, 5(3), 41. https://doi.org/10.3390/bdcc5030041







