An Epidemiological Survey of Intestinal Parasitic Infection and the Socioeconomic Status of the Ethnic Minority People of Moken and Orang Laut
Abstract
1. Introduction
2. Materials and Methods
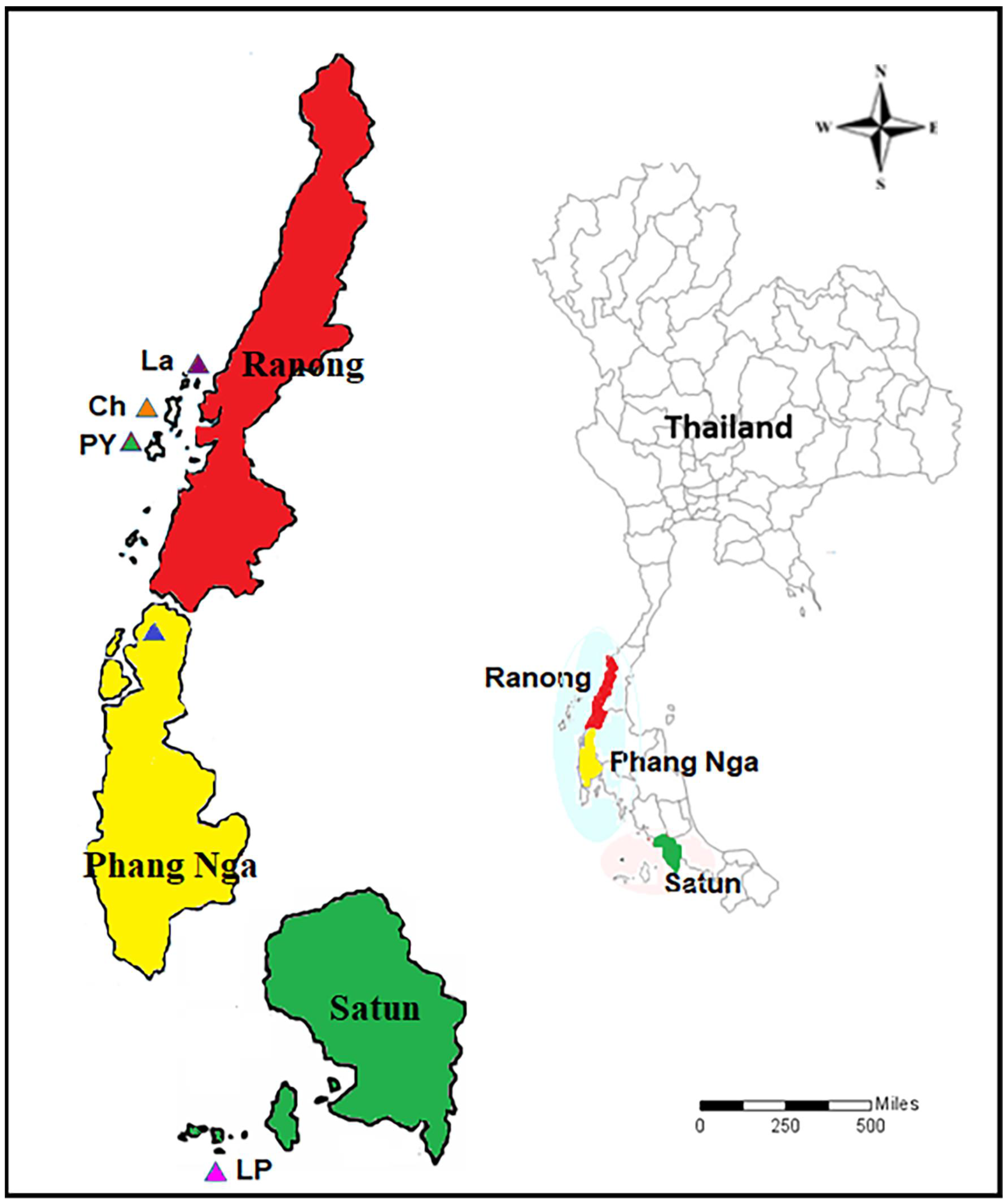
2.1. Study Areas and Study Population
2.2. Sample Collection and Parasitological Diagnosis
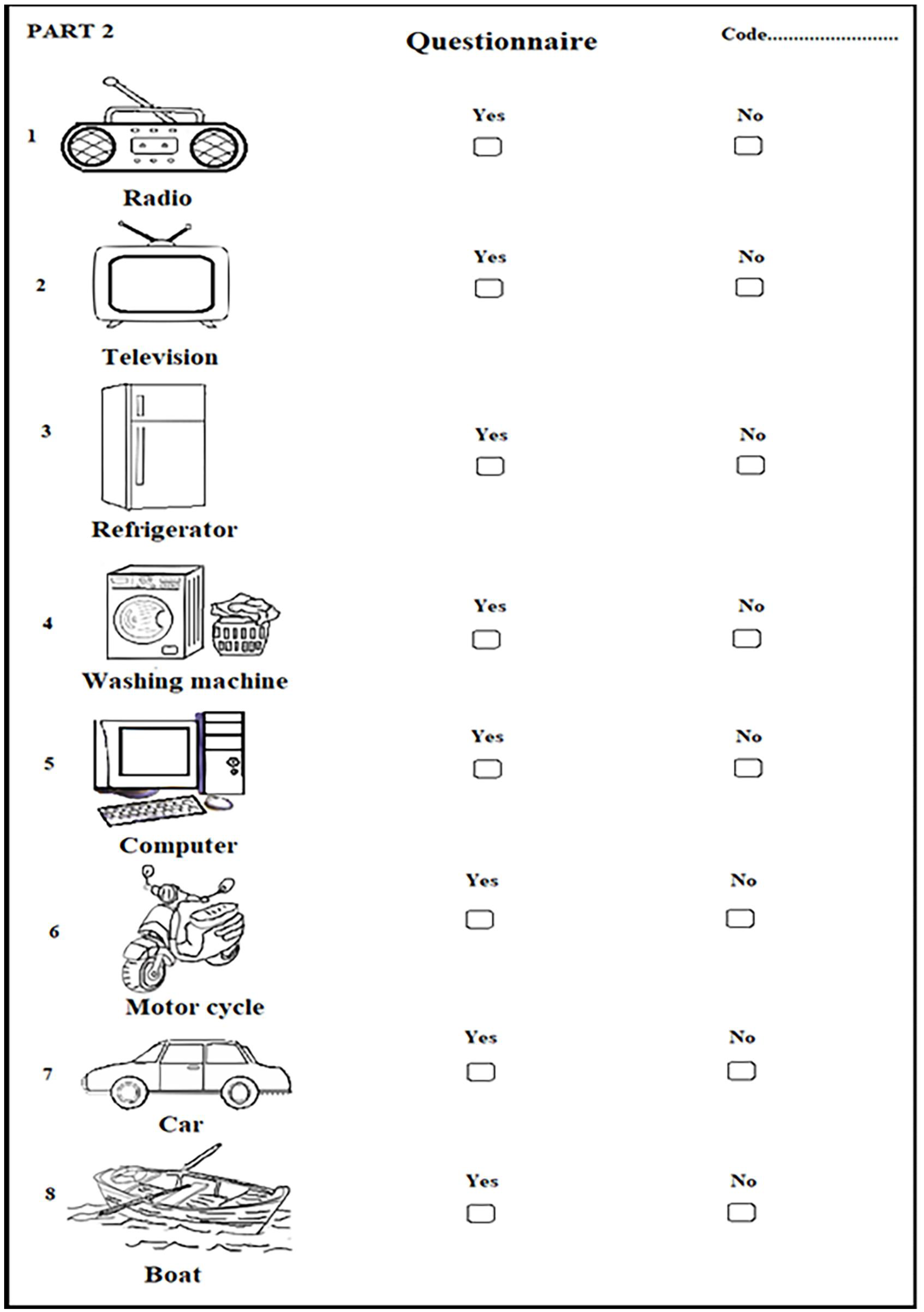
2.3. Socioeconomic Status and Sanitary Condition
2.4. Statistical Analysis
3. Results
3.1. Overall Prevalence of Intestinal Parasitic Infection
3.2. Type and Number of Parasitic Infections in Each Study Group
3.3. Association between the Study Group and Mode of Transmission
3.4. Socioeconomic and Sanitary Conditions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Adams, A.M.; Vuckovic, M.; Birch, E.; Brant, T.A.; Bialek, S.; Yoon, D.; Koroma, J.; Direny, A.; Shott, J.; Lemoine, J.F.; et al. Eliminating Neglected Tropical Diseases in Urban Areas: A Review of Challenges, Strategies and Research Directions for Successful Mass Drug Administration. Trop. Med. Infect. Dis. 2018, 3, 122. [Google Scholar] [CrossRef] [PubMed]
- Yanola, J.; Nachaiwieng, W.; Duangmano, S.; Prasannarong, M.; Somboon, P.; Pornprasert, S. Current prevalence of intestinal parasitic infections and their impact on hematological and nutritional status among Karen hill tribe children in Omkoi District, Chiang Mai Province, Thailand. Acta. Trop. 2018, 180, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Pullan, R.L.; Freeman, M.C.; Gething, P.W.; Brooker, S.J. Geographical inequalities in use of improved drinking water supply and sanitation across Sub-Saharan Africa: Mapping and spatial analysis of cross-sectional survey data. PLoS Med. 2014, 11, e1001626. [Google Scholar] [CrossRef]
- WHO. WHO Preventive Chemotherapy to Control Soil-Transmitted Helminth Infections In At-Risk Population Groups Geneva; 2017. Available online: https://www.who.int/intestinal_worms/resources/9789241550116/en/ (accessed on 11 November 2022).
- Ulaganeethi, R.; Saya, G.K.; Rajkumari, N.; Kumar, S.S.; Ganapathy, K.; Dorairajan, G. Soil-Transmitted Helminth Infections among Antenatal Women in Primary Care Settings in Southern India: Prevalence, Associated Factors and Effect of Anti-Helminthic Treatment. Trop. Med. Infect. Dis. 2023, 8, 48. [Google Scholar] [CrossRef] [PubMed]
- Hotez, P.J.; Alvarado, M.; Basáñez, M.-G.; Bolliger, I.; Bourne, R.; Boussinesq, M.; Brooker, S.J.; Brown, A.S.; Buckle, G.; Budke, C.M.; et al. The Global Burden of Disease Study 2010: Interpretation and Implications for the Neglected Tropical Diseases. PLoS Negl. Trop. Dis. 2014, 8, e2865. [Google Scholar] [CrossRef]
- Pullan, R.L.; Brooker, S.J. The global limits and population at risk of soil-transmitted helminth infections in 2010. Parasit. Vectors 2012, 5, 81. [Google Scholar] [CrossRef]
- Shiferaw, K.; Tesfay, T.; Kalayu, G.; Kiros, G. Human Intestinal Parasites: Prevalence and Associated Risk Factors among Grade School Children in Maksegnit, Northwest Ethiopia. J. Trop. Med. 2021, 10, 6694809. [Google Scholar] [CrossRef]
- Utzinger, J.; Bergquist, R.; Olveda, R.; Zhou, X.N. Important helminth infections in Southeast Asia. Diversity, potential for control and prospects for elimination. Adv. Parasitol. 2010, 72, 1–30. [Google Scholar]
- Dunn, J.C.; Turner, H.C.; Tun, A.; Anderson, R.M. Epidemiological surveys of, and research on, soil-transmitted helminths in Southeast Asia: A systematic review. Parasit. Vectors 2016, 9, 31. [Google Scholar] [CrossRef]
- Wongsaroj, T.; Nithikathkul, C.; Rojkitikul, W.; Nakai, W.; Royal, L.; Rammasut, P. National survey of helminthiasis in Thailand. Asian Biomed. 2014, 8, 779–783. [Google Scholar] [CrossRef]
- Sarasombath, T.P.; Roongruanchai, K.; Sermsart, B.; Monkong, N.; Loymek, S.; Dulyaporn, R.; Nararak, O.; Wongkamchai, S. Prevalence and Health Effects of Intestinal Parasitic Infection in School Children in Satun Province, Thailand: A Cross-Sectional Study. Siriraj Med. J. 2017, 69, 167–174. [Google Scholar]
- Boonjaraspinyo, S.; Boonmars, T.; Kaewsamut, B.; Ekobol, N.; Laummaunwai, P.; Aukkanimart, R.; Wonkchalee, N.; Juasook, A.; Sriraj, P. A cross-sectional study on intestinal parasitic infections in rural communities, northeast Thailand. Korean. J. Parasitol. 2013, 51, 727–734. [Google Scholar] [CrossRef]
- Oninla, S.O.; Onayade, A.A.; Owa, J.A. Impact of intestinal helminthiases on the nutritional status of primary-school children in Osun state, south-western Nigeria. Ann. Trop. Med. Parasitol. 2010, 104, 583–594. [Google Scholar] [CrossRef] [PubMed]
- Fürst, T.; Silué, K.D.; Ouattara, M.; N’Goran, D.N.; Adiossan, L.G.; N’Guessan, Y.; Zouzou, F.; Koné, S.; N’Goran, E.K.; Utzinger, J. Schistosomiasis, soil-transmitted helminthiasis, and sociodemographic factors influence quality of life of adults in Côte d’Ivoire. PLoS Negl. Trop. Dis. 2012, 6, e1855. [Google Scholar] [CrossRef]
- Sayasone, S.; Utzinger, J.; Akkhavong, K.; Odermatt, P. Multiparasitism and intensity of helminth infections in relation to symptoms and nutritional status among children: A cross-sectional study in southern Lao People’s Democratic Republic. Acta. Trop. 2015, 141, 322–331. [Google Scholar] [CrossRef]
- Ellwanger, J.H.; Ziliotto, M.; Kulmann-Leal, B.; Chies, J.A.B. Iron deficiency and soil-transmitted helminth infection: Classic and neglected connections. Parasitol. Res. 2022, 121, 3381–3392. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Morales, A.J.; Barbella, R.A.; Case, C.; Arria, M.; Ravelo, M.; Perez, H.; Urdaneta, O.; Gervasio, G.; Rubio, N.; Maldonado, A.; et al. Intestinal Parasitic Infections among Pregnant Women in Venezuela. Infect. Dis. Obstet. Gynecol. 2006, 23, 125. [Google Scholar] [CrossRef]
- Fink, M.Y.; Singer, S.M. The intersection of immune responses, microbiota and pathogenesis in giardiasis. Trends Parasitol. 2017, 33, 901–913. [Google Scholar] [CrossRef]
- Bouree, P.; Bisaro, F. Parasitic diarrhea. Presse. Med. 2007, 36, 706–716. [Google Scholar] [CrossRef]
- Hanevik, K.; Kristoffersen, E.; Mørch, K.; Rye, K.P.; Sørnes, S.; Svärd, S.; Bruserud, Q.; Langeland, N. Giardia-specific cellular immune responses in post-giardiasis chronic fatigue syndrome. BMC Immunol. 2017, 18, 5. [Google Scholar] [CrossRef]
- Kaewpitoon, S.J.; Loyd, R.A.; Kaewpitoon, N. A Cross-Sectional Survey of Intestinal Helminthiases in Rural Communities of Nakhon Ratchasima Province, Thailand. J. Med. Assoc. Thai. 2015, 98, S27–S32. [Google Scholar] [PubMed]
- Loymek, S.; Wongkamchai, S.; Kob-asa, T.; Choochote, W.; Monkong, N.; Chitnabut, P.; Onrochanakul, J.; Suvutho, S.; Sermsart, B. Impact of a filariasis control program on intestinal helminthic infections; a pilot study in Narathiwat Province, Thailand. Southeast Asian J. Trop. Med. Public Health 2004, 35, 63–67. [Google Scholar]
- WHO. Soil-Transmitted Helminthiases. Available online: https://www.who.int/health-topics/soil-transmitted-helminthiases#tab=tab_1 (accessed on 17 February 2023).
- WHO. Soil-Transmitted Helminthiases. Available online: https://apps.who.int/neglected_diseases/ntddata/sth/sth.html (accessed on 17 February 2023).
- Becker, S.L.; Liwanag, H.J.; Snyder, J.S.; Akogun, O.; Belizario, V., Jr.; Freeman, M.C.; Gyorkos, T.W.; Imtiaz, R.; Keiser, J.; Krolewiecki, A.; et al. Toward the 2020 goal of soil-transmitted helminthiasis control and elimination. PLoS Negl. Trop. Dis. 2018, 14, e0006606. [Google Scholar] [CrossRef] [PubMed]
- Schratz, A.; Pineda, M.F.; Reforma, L.G.; Fox, N.M.; Le Anh, T.; Tommaso Cavalli-Sforza, L.; Henderson, M.K.; Mendoza, R.; Utzinger, J.; Ehrenberg, J.P.; et al. Neglected diseases and ethnic minorities in the Western Pacific Region exploring the links. Adv. Parasitol. 2010, 72, 79–107. [Google Scholar] [PubMed]
- Morgan. Wikipedia. Available online: https://en.wikipedia.org/wiki/Moken#cites_note-25 (accessed on 9 December 2022).
- Urak Lawoi. Wikipedia. Available online: https://en.wikipedia.org/wiki/Orang_Laut.OrangLaut (accessed on 9 December 2022).
- Narkkul, U.; Na-ek, P.; Kaewkungwal, J.; Punsawad, C. Knowledge, Attitudes, and Practices regarding Soil-Transmitted Helminthiasis among Village Health Volunteers in Nakhon Si Thammarat Province, Thailand: A Cross-Sectional Study. Trop. Med. Infect. Dis. 2022, 7, 33. [Google Scholar] [CrossRef] [PubMed]
- Kache, R.; Phasuk, N.; Viriyavejakul, P.; Punsawad, C. Prevalence of soil-transmitted helminth infections and associated risk factors among elderly individuals living in rural areas of southern Thailand. BMC Pub. Health. 2020, 20, 1882. [Google Scholar] [CrossRef]
- Punsawad, C.; Phasuk, N.; Bunratsami, S.; Thongtup, K.; Siripakonuaong, N.; Nongnaul, S. Prevalence of intestinal parasitic infection and associated risk factors among village health volunteers in rural communities of southern Thailand. BMC Public Health 2017, 17, 564. [Google Scholar] [CrossRef]
- Jiraanankul, V.; Aphijirawat, W.; Mungthin, M.; Khositnithikul, R.; Rangsin, R.; Traub, R.J.; Piyaraj, P.; Naaglor, T.; Taamasri, P.; Leelayoova, S. Incidence and risk factors of hookworm infection in a rural community of central Thailand. Am. J. Trop. Med. Hyg. 2011, 84, 594–598. [Google Scholar] [CrossRef]
- Kitvatanachai, S.; Boonslip, S.; Watanasatitarpa, S. Intestinal parasitic infections in Srimum suburban area of Nakhon Ratchasima Province, Thailand. Trop. Biomed. 2008, 25, 237–242. [Google Scholar]
- Anantaphruti, M.T.; Jongsuksuntigul, P.; Imsomboon, T.; Nagai, N.; Muennoo, C.; Saguankiat, S.; Pubampen, S.; Kojima, S. School-based helminthiases control: I. A baseline study of soil-transmitted helminthiases in Nakhon Si Thammarat Province, Thailand. Southeast Asian J. Trop. Med. Public Health. 2002, 33, 113–119. [Google Scholar]
- WHO. Basic Laboratory Methods in Medical Parasitology. 1991. Available online: https://apps.who.int/iris/handle/10665/40793 (accessed on 12 February 2023).
- Clinical Guidelines-Diagnosos and Treatment Manual. Available online: https://Intestinalprotozoaninfections(parasiticdiarrhoea)|MSFMedicalGuidelines (accessed on 12 February 2023).
- WHO. Report of The WHO Informal Consultation on The Use of Chemotherapy For The Control of Morbidity Due To Soil–Transmitted Nematodes In Humans; WHO: Geneva, Switzerland, 1996. [Google Scholar]
- Iegelbauer, K.; Speich, B.; Mäusezahl, D.; Bos, R.; Keiser, J.; Utzinger, J. Effect of sanitation on soil-transmitted helminth infection: Systematic review and meta-analysis. PLoS Med. 2012, 9, e1001162. [Google Scholar]
- Echazú, A.; Bonanno, D.; Juarez, M.; Cajal, S.P.; Heredia, V.; Caropresi, S.; Cimino, R.O.; Caro, N.; Vargas, P.A.; Paredes, G.; et al. Effect of Poor Access to Water and Sanitation As Risk Factors for Soil-Transmitted Helminth Infection: Selectiveness by the Infective Route. PLoS Negl. Trop Dis. 2015, 9, e0004111. [Google Scholar] [CrossRef] [PubMed]
- Stateless at Sea: The Moken of Burma and Thailand HRW. Available online: https://www.hrw.org/report/2015/06/25/stateless-sea/moken-burma-and-thailand (accessed on 12 December 2022).
- Mark, J. Thailand’s Fisherfolk Rebuild after Tsunami. Reuters. 6 May 2005. Available online: https://www.alertnet.org/thenews/photogallery/fisherfolk.html (accessed on 12 December 2022).
- SAN. Save Andaman Network. Nine Months Progress Report. January–February 2005. Available online: https://www.globalgiving.org/pfil/878/SAN_9_Month_Tsunami_Report.pdf (accessed on 12 December 2022).
- The Urak Lawoi, the First Inhabitants of Koh Lipe–Thailand. Available online: https://www.thailandmagazine.com/Magazine.com, (accessed on 12 December 2022).
- Dagne, N.; Alelign, A. Prevalence of Intestinal Protozoan Parasites and Associated Risk Factors among School Children in Merhabete District, Central Ethiopia. J. Parasitol. Res. 2021, 25, 9916456. [Google Scholar] [CrossRef]
- Brooker, S.; Singhasivanon, P.; Waikagul, J.; Supavej, S.; Kojima, S.; Takeuchi, T.; Luong, T.V.; Looareesuwan, S. Mapping soil-transmitted helminths in Southeast Asia and implications for parasite control. Southeast Asian J. Trop. Med. 2003, 34, 24–36. [Google Scholar]
- WHO. Helminth Control in School-Age Children: A Guide For Managers of Control Programme; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Strunz, E.C.; Addiss, D.G.; Stocks, M.E.; Ogden, S.; Utzinger, J.; Freeman, M.C. Water, sanitation, hygiene and soil-transmitted helminth infection: A systematic review and meta-analysis. PLoS Med. 2014, 11, e1001620. [Google Scholar] [CrossRef]
- CDC. Anisakiasis. Available online: https://www.cdc.gov/parasites/anisakiasis/faqs.html (accessed on 12 February 2023).
- Bartram, J.; Cairncross, S. Hygiene, sanitation, and water: Forgotten foundations of health. PLoS Med. 2010, 7, e1000367. [Google Scholar] [CrossRef]
- SDG. Sustainable Development Goals CDP. Available online: https://www.cdp.net/en/policy/program-areas/sustainable-development-goals? (accessed on 18 February 2022).
- Montresor, A.; Mupfasoni, D.; Mikhailov, A.; Mwinzi, P.; Lucianez, A.; Jamsheed, M.; Gasimov, E.; Warusavithana, S.; Yajima, A.; Bisoffi, Z.; et al. The global progress of soil-transmitted helminthiases control in 2020 and World Health Organization targets for 2030. PLoS Negl. Trop. Dis. 2020, 14, e0008505. [Google Scholar] [CrossRef]



| Province | Ethnic | Geographical Features | Total Subject | IPIS Infected Subject | Helminth | Protozoa | Mix Infection | ||
|---|---|---|---|---|---|---|---|---|---|
| Multiple Species of STHs | Multiple Species of Protozoa | Multiple Species of STHs and Protozoa | |||||||
| Ranong | Moken | Island | 328 (100%) | 203 (61.8%) | 190 (57.9%) | 50 (20.9%) | 45 (13.7%) | 3 (0.9%) | 37 (11.3%) |
| Phang Nga | Moken | Coastal | 84 (100%) | 21 (25%) | 15 (17.9%) | 8 (9.5%) | 2 (2.4%) | 1 (1.2%) | 2 (2.4%) |
| Satun | Orang Laut | Island | 279 (100%) | 36 (12.9%) | 6 (2.2%) | 32 (11.5%) | 0 (0%) | 2 (0.7%) | 2 (0.7%) |
| 691 (100%) | 260 (37.6%) | 211 (30.5%) | 90 (13%) | 47 (6.8%) | 6 (0.9%) | 41 (5.9%) | |||
| Intestinal Parasitic Infections (IPIs) | Ranong | Phang Nga | Satun | |||
|---|---|---|---|---|---|---|
| Chang, Payam, Lao Islands | Thub Tawan Village | Lipe Island | ||||
| Number (n = 328) | Prevalence (%) | Number (n = 84) | Prevalence (%) | Number (n = 279) | Prevalence (%) | |
| Overall any parasitic infection | 203 | 62 | 21 | 25 | 36 | 12.9 |
| Single-parasitic infection | 115 | 35 | 16 | 19 | 32 | 11.5 |
| Mix-parasitic infection | 88 | 26.8 | 5 | 5.9 | 4 | 1.4 |
| Overall any helminthic infection | 190 | 57.9 | 15 | 17.9 | 6 | 2.2 |
| Overall any protozoa infection | 50 | 20.9 | 8 | 9.5 | 32 | 11.5 |
| STHs | ||||||
| Ascaris lumbricoides | 159 | 48.5 | 3 | 3.6 | 2 | 0.7 |
| Hookworm | 7 | 2.1 | 3 | 3.6 | 1 | 0.4 |
| Trichuris trichiura | 91 | 27.7 | 9 | 10.7 | 2 | 0.7 |
| Strongyloides stercoralis | 4 | 1.2 | 0 | 0 | 2 | 0.7 |
| Water/food-borne protozoa | ||||||
| Giardia duodenalis | 11 | 3.4 | 4 | 4.8 | 13 | 4.7 |
| Entamoeba histolytica | 4 | 1.2 | 0 | 0 | 0 | 0 |
| Entamoeba coli | 12 | 3.7 | 1 | 1.2 | 3 | 1.1 |
| Endolimax nana | 4 | 1.2 | 0 | 0 | 0 | 0 |
| Blastocystis hominis | 30 | 9.1 | 5 | 6 | 19 | 6.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wattano, S.; Kerdpunya, K.; Keawphanuk, P.; Hunnangkul, S.; Loimak, S.; Tungtrongchitra, A.; Wongkamchai, M.; Wongkamchai, S. An Epidemiological Survey of Intestinal Parasitic Infection and the Socioeconomic Status of the Ethnic Minority People of Moken and Orang Laut. Trop. Med. Infect. Dis. 2023, 8, 161. https://doi.org/10.3390/tropicalmed8030161
Wattano S, Kerdpunya K, Keawphanuk P, Hunnangkul S, Loimak S, Tungtrongchitra A, Wongkamchai M, Wongkamchai S. An Epidemiological Survey of Intestinal Parasitic Infection and the Socioeconomic Status of the Ethnic Minority People of Moken and Orang Laut. Tropical Medicine and Infectious Disease. 2023; 8(3):161. https://doi.org/10.3390/tropicalmed8030161
Chicago/Turabian StyleWattano, Suphaluck, Kamonwan Kerdpunya, Phongton Keawphanuk, Saowalak Hunnangkul, Sumas Loimak, Aunchalee Tungtrongchitra, Metta Wongkamchai, and Sirichit Wongkamchai. 2023. "An Epidemiological Survey of Intestinal Parasitic Infection and the Socioeconomic Status of the Ethnic Minority People of Moken and Orang Laut" Tropical Medicine and Infectious Disease 8, no. 3: 161. https://doi.org/10.3390/tropicalmed8030161
APA StyleWattano, S., Kerdpunya, K., Keawphanuk, P., Hunnangkul, S., Loimak, S., Tungtrongchitra, A., Wongkamchai, M., & Wongkamchai, S. (2023). An Epidemiological Survey of Intestinal Parasitic Infection and the Socioeconomic Status of the Ethnic Minority People of Moken and Orang Laut. Tropical Medicine and Infectious Disease, 8(3), 161. https://doi.org/10.3390/tropicalmed8030161






