Integrated Tuberculosis and COVID-19 Activities in Karachi and Tuberculosis Case Notifications
Abstract
:1. Introduction
2. Methods
2.1. Adaptations
2.1.1. Integrating TB and COVID-19 Activities
2.1.2. Delivery of Medicines at Doorsteps
2.1.3. Personal Protection Equipment (PPE) Provision
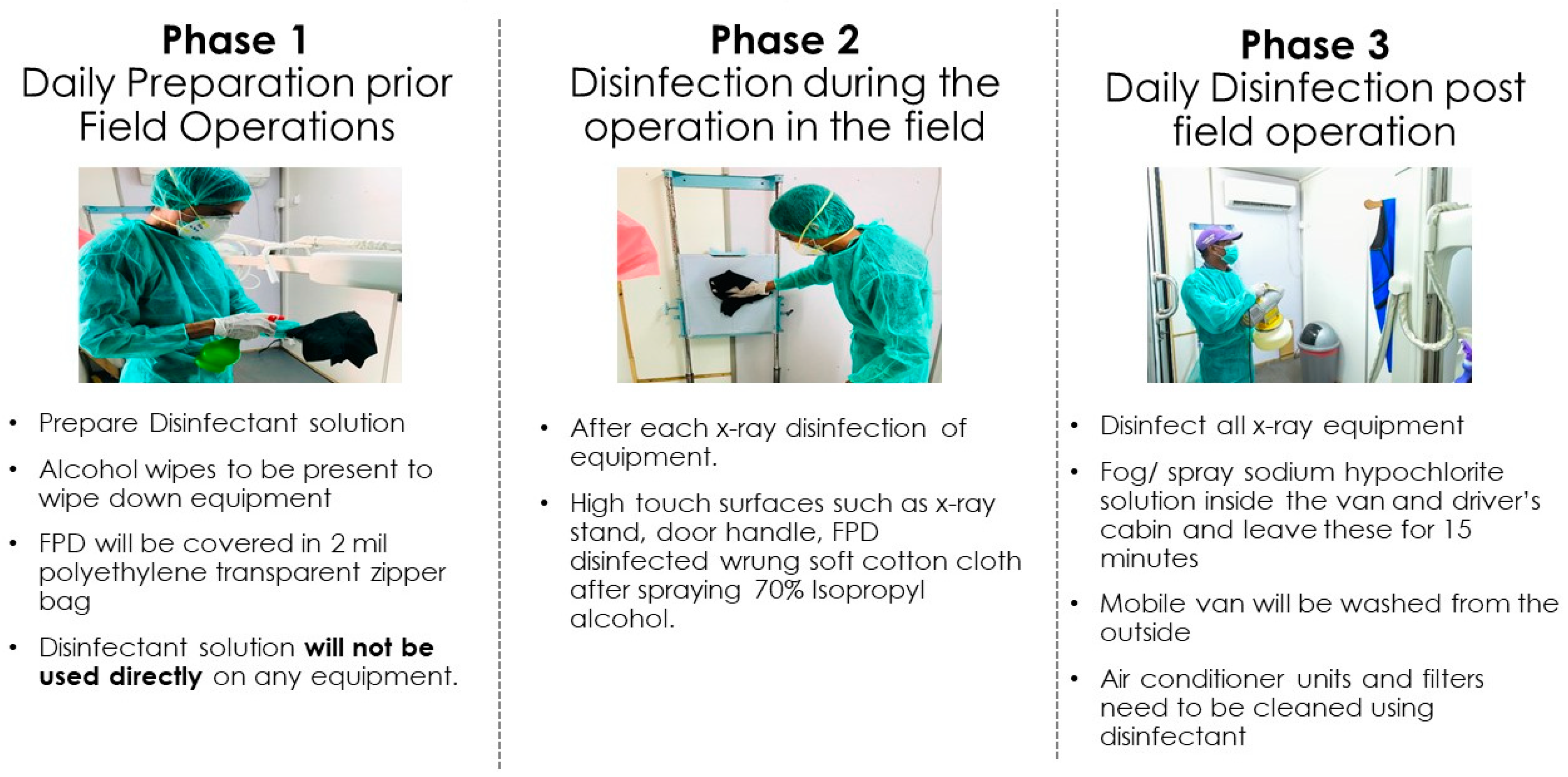
2.1.4. Patient Safety and Disinfection Protocol
2.1.5. Workforce Burnout Monitoring
2.1.6. Use of Telehealth and Mental Health Integration
2.2. Programmatic Data
2.3. Data Analysis
2.4. Ethical Approval
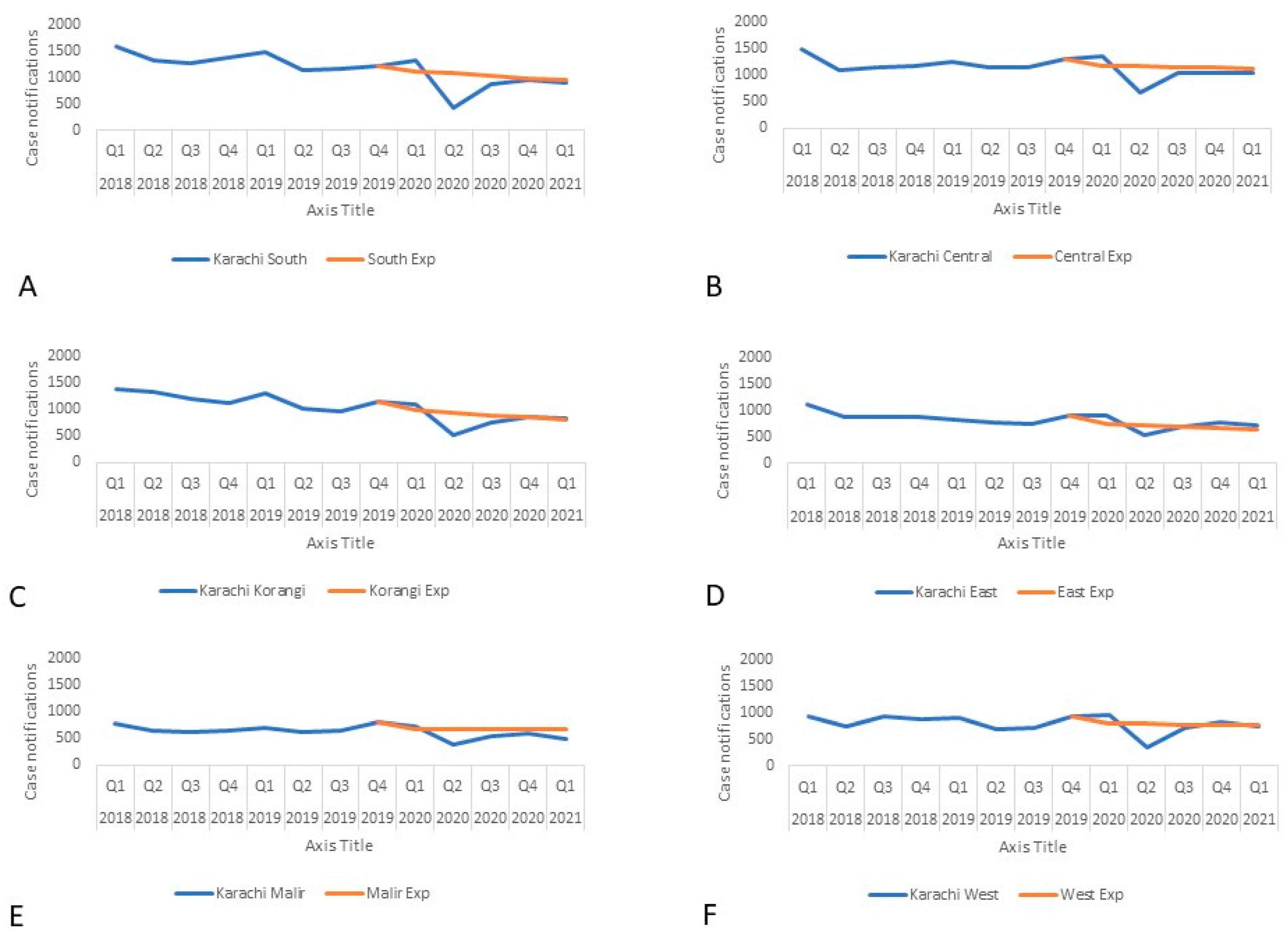
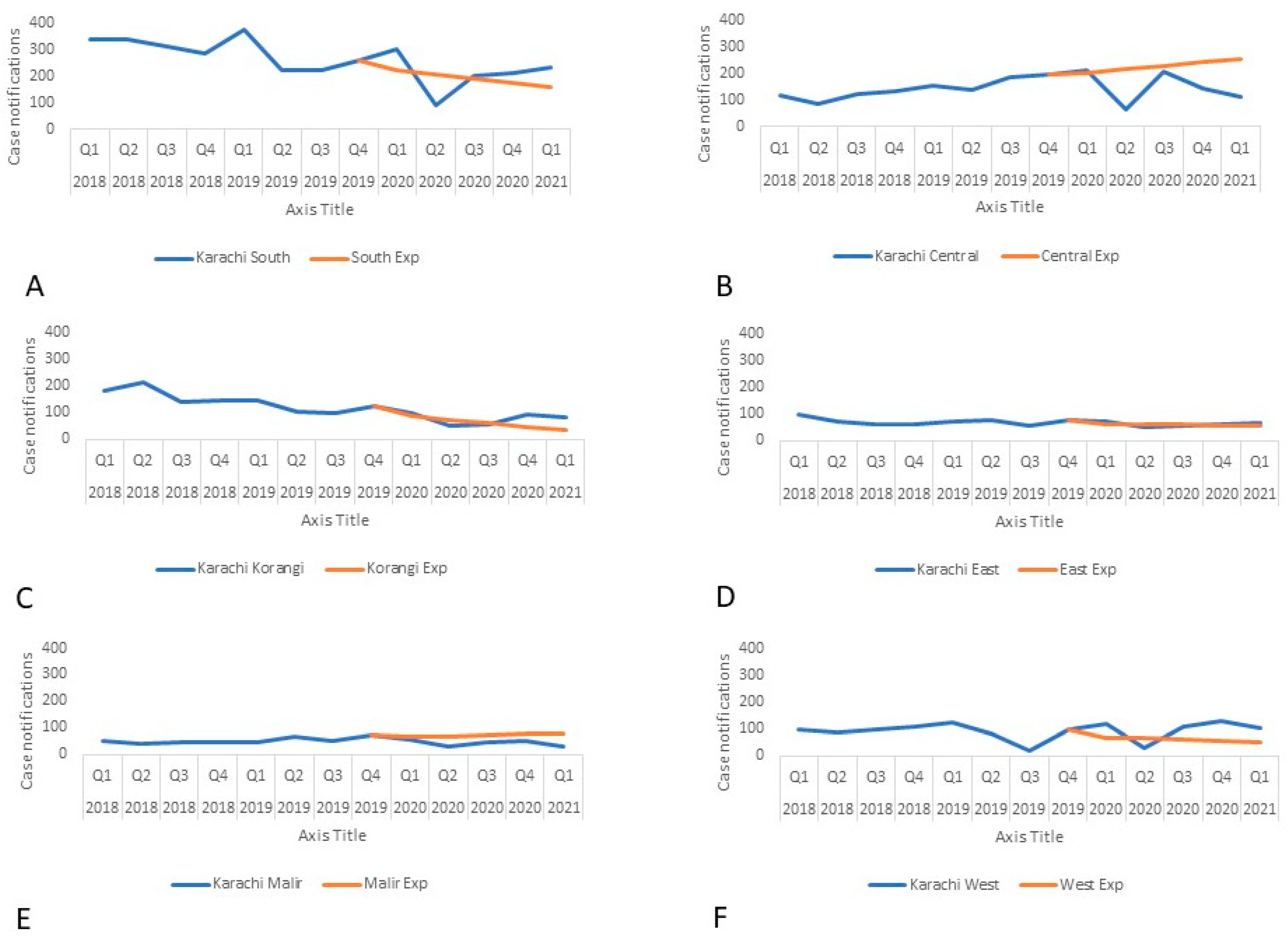
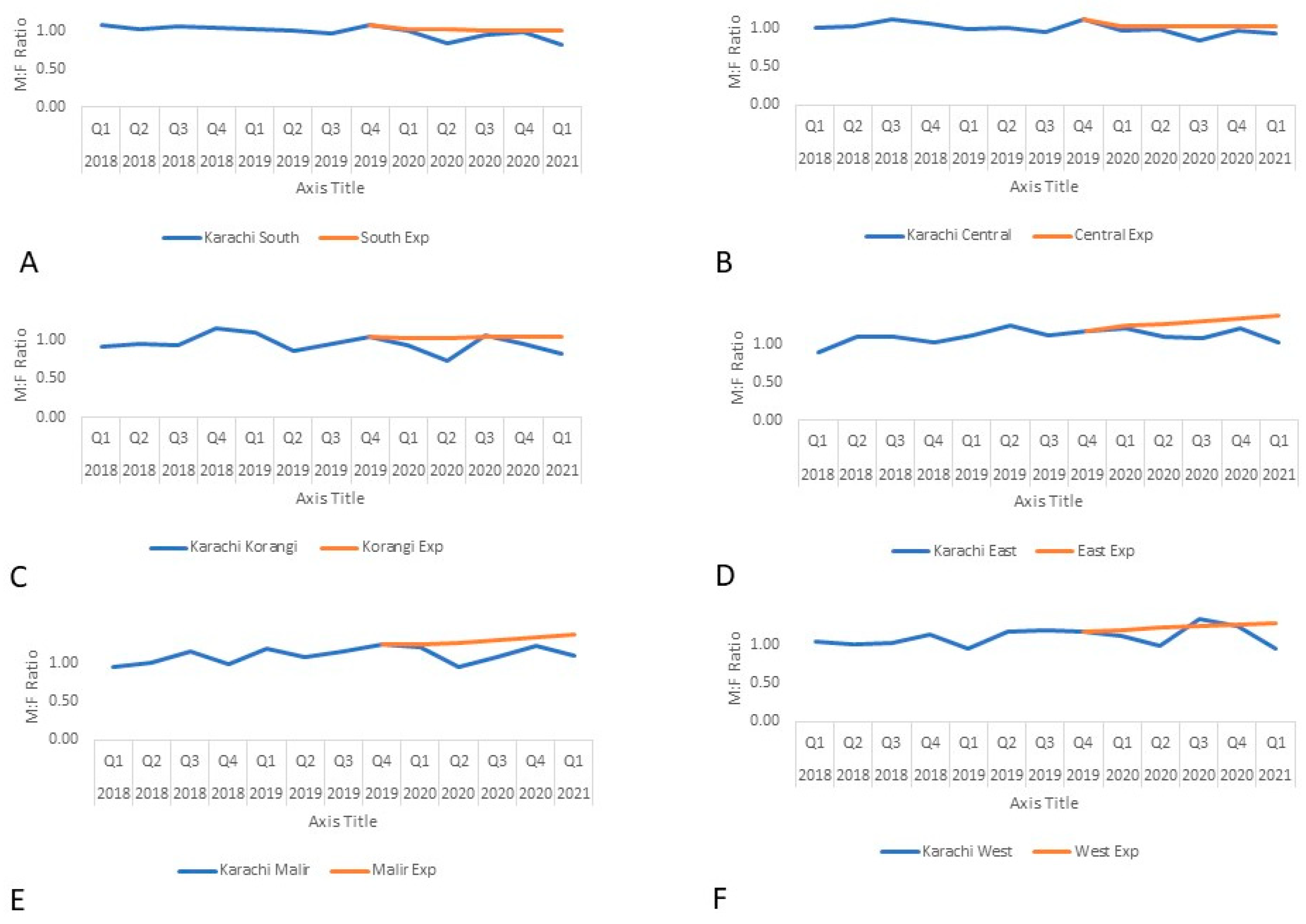
3. Results
4. Discussion
Lessons Learned
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Quaglio, G.; Tognon, F.; Finos, L.; Bome, D.; Sesay, S.; Kebbie, A.; Di Gennaro, F.; Camara, B.S.; Marotta, C.; Pisani, V.; et al. Impact of Ebola outbreak on reproductive health services in a rural district of Sierra Leone: A prospective observational study. BMJ Open 2019, 9, e029093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wingfield, T.; Cuevas, L.E.; MacPherson, P.; A Millington, K.; Squire, S.B. Tackling two pandemics: A plea on World Tuberculosis Day. Lancet Respir. Med. 2020, 8, 536–538. [Google Scholar] [CrossRef] [Green Version]
- Musso, M.; Di Gennaro, F.; Gualano, G.; Mosti, S.; Cerva, C.; Fard, S.N.; Libertone, R.; Di Bari, V.; Cristofaro, M.; Tonnarini, R.; et al. Concurrent cavitary pulmonary tuberculosis and COVID-19 pneumonia with in vitro immune cell anergy. Infection 2021, 49, 1061–1064. [Google Scholar] [CrossRef] [PubMed]
- Wingfield, T.; Karmadwala, F.; MacPherson, P.; Millington, K.A.; Walker, N.F.; E Cuevas, L.; Squire, S.B. Challenges and opportunities to end tuberculosis in the COVID-19 era. Lancet Respir. Med. 2021, 9, 556–558. [Google Scholar] [CrossRef]
- Zimmer, A.J.; Klinton, J.S.; Oga-Omenka, C.; Heitkamp, P.; Nyirenda, C.N.; Furin, J.; Pai, M. Tuberculosis in times of COVID-19. J. Epidemiol. Commun. Health 2021. [Google Scholar] [CrossRef] [PubMed]
- Pai, M.; Kasaeva, T.; Swaminathan, S. Covid-19’s Devastating Effect on Tuberculosis Care—A Path to Recovery. N. Engl. J. Med. 2022, 10, 2118145. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.A.; Safdar, N.; Chandir, S.; Khan, U.; Khowaja, S.; Riaz, N.; Manjar, R.; Jaswal, M.; Khan, A.J.; Hussain, H. Tuberculosis control and care in the era of COVID-19. Health Policy Plan. 2020, 1130–1132. [Google Scholar] [CrossRef] [PubMed]
- Di Gennaro, F.; Gualano, G.; Timelli, L.; Vittozzi, P.; Di Bari, V.; Libertone, R.; Cerva, C.; Pinnarelli, L.; Nisii, C.; Ianniello, S.; et al. Increase in Tuberculosis Diagnostic Delay during First Wave of the COVID-19 Pandemic: Data from an Italian Infectious Disease Referral Hospital. Antibiotics 2021, 10, 272. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Tuberculosis Control Report 2021; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Stop TB Partnership. The Potential Impact of the COVID-19 Response on Tuberculosis in High-Burden Countries: A Modelling Analysis; Stop TB Partnership: Geneva, Switzerland, 2020. [Google Scholar]
- Abid, K.; Bari, Y.A.; Younas, M.; Javaid, S.T.; Imran, A. Progress of COVID-19 Epidemic in Pakistan. Asia Pac. J. Public Health 2020, 32, 154–156. [Google Scholar] [CrossRef] [PubMed]
- Hussain, H.R. Smart Lockdowns: Pakistan’s COVID-19 Silver-Lining? 2020. Available online: http://www.saisperspectives.com/covid19-pandemic/2020/7/28/smart-lockdowns-pakistans-covid-19-silver-lining (accessed on 8 December 2021).
- Fatima, R.; Akhtar, N.; Yaqoob, A.; Harries, A.D.; Khan, M.S. Building better tuberculosis control systems in a post-COVID world: Learning from Pakistan during the COVID-19 pandemic. Int. J. Infect. Dis. 2021, 113, S88–S90. [Google Scholar] [CrossRef] [PubMed]
- Zero TB Initiative. 2021. Available online: https://www.zerotbinitiative.org/ (accessed on 8 December 2021).
- qXR Detects Various Abnormalities on Chest X-rays. 2020. Available online: http://qure.ai/qxr/ (accessed on 8 December 2021).
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef] [Green Version]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moosa, S.; Shah, S.; Mohiuddin, A.F.; Haider, K.F.; Khowaja, S. Proactive Teleconsultation for Coronavirus Disease 2019 Cases Identified Through the Community-Testing Initiative in Karachi, Pakistan: A Low-Cost Value-Added Service to Support a Pandemic Response in a Resource-Limited Setting. Telemed. E-Health 2021. [Google Scholar] [CrossRef] [PubMed]
- Stop TB Partnership. One Year On, New Data show Global Impact of COVID-19 on TB Epidemic Is Worse than Expected 2021. Available online: https://stoptb.org/webadmin/cms/docs/20210316_TB%20and%20COVID_One%20Year%20on_Media%20Brief_FINAL.pdf (accessed on 8 December 2021).
- World Health Organization. Roadmap Towards Ending TB in Children and Adolescents; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Eyo, A.S.; Obot, V.O.; Onyedinachi, O.; Vasquez, N.A.; Bigio, J.; Sanaie, A.; Beulah, F.; Ette, U.; Uju, D.; Rahman, T. A Multi-Faceted Approach to Tuberculosis Active Case Finding among Remote Riverine Communities in Southern Nigeria. Int. J. Environ. Res. Public Health 2021, 18, 9424. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.; Amanullah, F.; Codlin, A.J.; Siddiqui, S.; Jaswal, M.; Ahmed, J.F.; Saleem, S.; Khurshid, A.; Hussain, H. Improving childhood tuberculosis detection and treatment through facility-based screening in rural Pakistan. Int. J. Tuberc. Lung Dis. 2018, 22, 851–857. [Google Scholar] [CrossRef] [PubMed]
- Telisinghe, L.; Shaweno, D.; Hayes, R.J.; Dodd, P.J.; Ayles, H.M. The effect of systematic screening of the general population on TB case notification rates. Int. J. Tuberc. Lung Dis. 2021, 25, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Jamal, W.Z.; Habib, S.; Khowaja, S.; Safdar, N.; Zaidi, S.M.A. COVID-19: Ensuring continuity of TB services in the private sector. Int. J. Tuberc. Lung Dis. 2020, 24, 870–872. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, R.R.; Watson, G.P. Keeping Employees Safe During COVID-19: The Role of Safety Climate. 2021. Available online: https://www.siop.org/Research-Publications/Items-of-Interest/ArtMID/19366/ArticleID/4944/Keeping-Employees-Safe-During-COVID-19-The-Role-of-Safety-Climate (accessed on 8 December 2021).
- Malik, A.A.; Hussain, H.; Creswell, J.; Siddiqui, S.; Ahmed, J.F.; Madhani, F.; Habib, A.; Khan, A.J.; Amanullah, F. The Impact of Funding on Childhood TB Case Detection in Pakistan. Trop. Med. Infect. Dis. 2019, 4, 146. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malik, A.A.; Hussain, H.; Maniar, R.; Safdar, N.; Mohiuddin, A.; Riaz, N.; Pasha, A.; Khan, S.; Kazmi, S.S.H.; Kazmi, E.; et al. Integrated Tuberculosis and COVID-19 Activities in Karachi and Tuberculosis Case Notifications. Trop. Med. Infect. Dis. 2022, 7, 12. https://doi.org/10.3390/tropicalmed7010012
Malik AA, Hussain H, Maniar R, Safdar N, Mohiuddin A, Riaz N, Pasha A, Khan S, Kazmi SSH, Kazmi E, et al. Integrated Tuberculosis and COVID-19 Activities in Karachi and Tuberculosis Case Notifications. Tropical Medicine and Infectious Disease. 2022; 7(1):12. https://doi.org/10.3390/tropicalmed7010012
Chicago/Turabian StyleMalik, Amyn A., Hamidah Hussain, Rabia Maniar, Nauman Safdar, Amal Mohiuddin, Najam Riaz, Aneeta Pasha, Salman Khan, Syed Saleem Hasan Kazmi, Ershad Kazmi, and et al. 2022. "Integrated Tuberculosis and COVID-19 Activities in Karachi and Tuberculosis Case Notifications" Tropical Medicine and Infectious Disease 7, no. 1: 12. https://doi.org/10.3390/tropicalmed7010012
APA StyleMalik, A. A., Hussain, H., Maniar, R., Safdar, N., Mohiuddin, A., Riaz, N., Pasha, A., Khan, S., Kazmi, S. S. H., Kazmi, E., & Khowaja, S. (2022). Integrated Tuberculosis and COVID-19 Activities in Karachi and Tuberculosis Case Notifications. Tropical Medicine and Infectious Disease, 7(1), 12. https://doi.org/10.3390/tropicalmed7010012






