Vertical Infestation Profile of Aedes in Selected Urban High-Rise Residences in Malaysia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Sites
2.2. Ovitrap Surveillance
2.3. Data Analysis
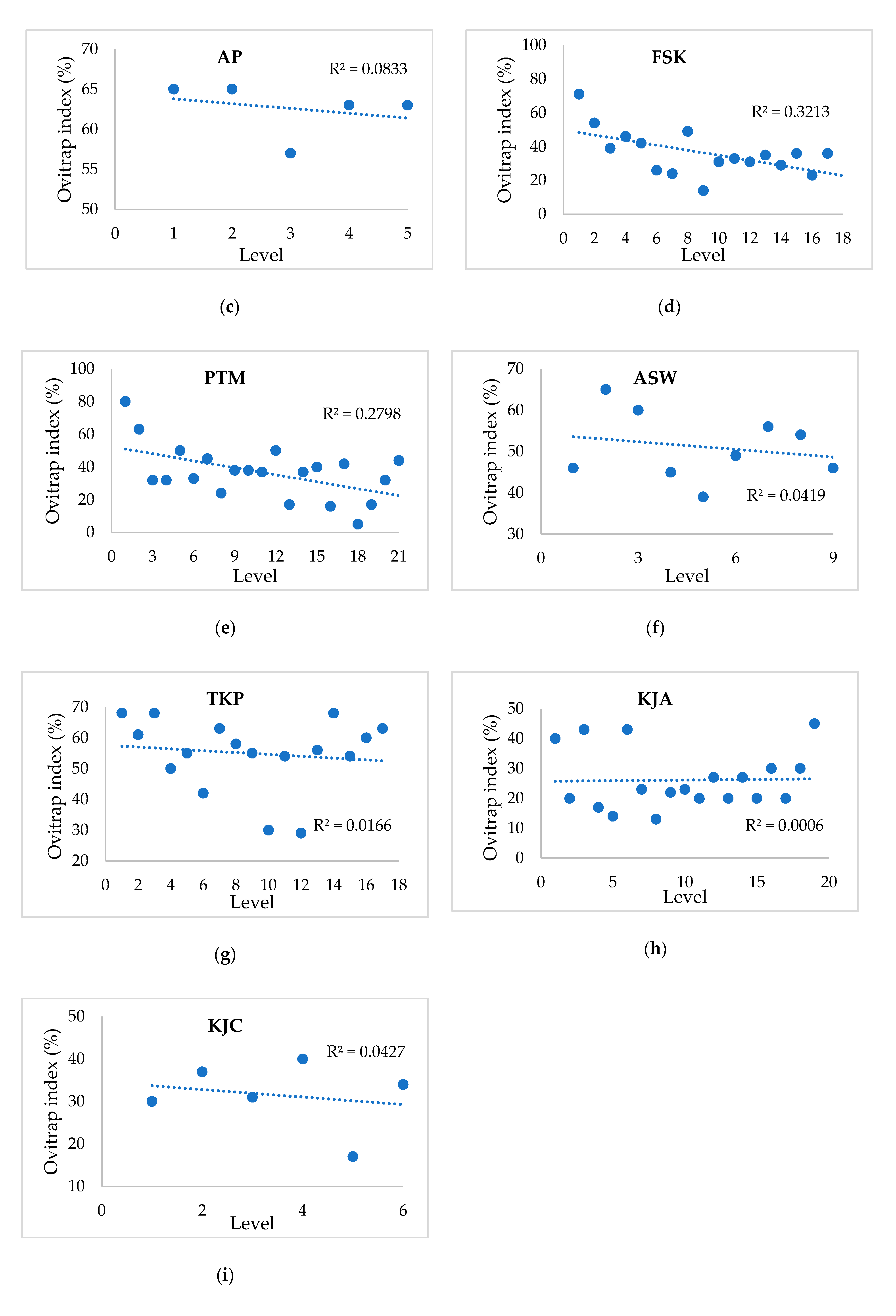
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethical Approval
References
- WHO. Dengue and Severe Dengue. Available online: https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue (accessed on 15 April 2020).
- WHO. Dengue Guidelines for Diagnosis, Treatment, Prevention and Control: New Edition; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Deng, S.Q.; Yang, X.; Wei, Y.; Chen, J.T.; Wang, X.J.; Peng, H.J. A review on dengue vaccine development. Vaccines 2020, 8, 63. [Google Scholar]
- Kato, F.; Ishida, Y.; Oishi, S.; Fujii, N.; Watanabe, S.; Vasudevan, S.G.; Tajima, S.; Takasaki, T.; Suzuki, Y.; Ichiyama, K.; et al. Novel antiviral activity of bromocriptine against dengue virus replication. Antivir. Res. 2016, 131, 141–147. [Google Scholar]
- WHO. WHO Region of the AMERICAS Records Highest Number of Dengue Cases in History; Cases Spike in Other Regions. Available online: https://www.who.int/news-room/detail/21-11-2019-who-region-of-the-americas-records-highest-number-of-dengue-cases-in-history-cases-spike-in-other-regions (accessed on 15 April 2020).
- Ministry of Health Malaysia. Kenyataan Akhbar Ketua Pengarah Kesihatan Malaysia. Situasi semasa Demam Denggi, Zika, dan Chikungunya di Malaysia. Available online: http://www.moh.gov.my/index.php/database_stores/store_view_page/17/1119 (accessed on 15 April 2020).
- Lau, K.W.; Chen, C.D.; Lee, H.L.; Izzul, A.A.; Asri-Isa, M.; Zulfadli, M.; Sofian-Azirun, M. Vertical distribution of Aedes mosquitoes in multiple storey buildings in Selangor and Kuala Lumpur, Malaysia. Trop. Biomed. 2013, 30, 36–45. [Google Scholar]
- Sarip, A.G.; Foong, L. Exploring the Perception of Lifestyle Housing Development in Malaysia; The Asia Pacific Network for Housing Research: Gwangju, Korea, 2015. [Google Scholar]
- New Straits Times. Malaysian House Buyers Increasingly Drawn to High-Rise Living. Available online: https://www.nst.com.my/news/2016/07/161815/malaysian-house-buyers-increasingly-drawn-high-rise-living (accessed on 15 April 2020).
- Ministry of Health Malaysia. Garis Panduan Halatuju Baharu Dalam Kawalan Denggi; Vector Borne Disease Sector, Disease Control Division, Ministry of Health Malaysia: Putrajaya, Malaysia, 2014. [Google Scholar]
- Muir, L.E.; Kay, B.H. Aedes aegypti survival and dispersal estimated by mark-release-recapture in northern Australia. Am. J. Trop. Med. Hyg. 1998, 58, 277–282. [Google Scholar]
- Harrington, L.C.; Buonaccorsi, J.P.; Edman, J.D.; Costero, A.; Kittayapong, P.; Clark, G.G.; Scott, T.W. Analysis of survival of young and old Aedes aegypti (Diptera: Culicidae) from Puerto Rico and Thailand. J. Med. Entomol. 2001, 38, 537–547. [Google Scholar]
- Verdonschot, P.F.M.; Besse-Lototskaya, A.A. Flight distance of mosquitoes (Culicidae): A metadata analysis to support the management of barrier zones around rewetted and newly constructed wetlands. Limnologica 2014, 45, 69–79. [Google Scholar]
- Ministry of Health Malaysia. Panduan Pengabutan (fogging) di Premis/ Bangunan Melebihi Lima (5) Tingkat; Ministry of Health Malaysia: Putrajaya, Malaysia, 2010. [Google Scholar]
- Jayathilake, H.; Wickramasinghe, M.; De Silva, N. Oviposition and vertical dispersal of Aedes mosquitoes in multiple storey buildings in Colombo district, Sri Lanka. J. Vector Borne. Dis. 2015, 52, 245–251. [Google Scholar]
- Chadee, D.D. Observations on the seasonal prevalence and vertical distribution patterns of oviposition by Aedes aegypti (L) (Diptera: Culicidae) in urban high-rise apartments in Trinidad, West Indies. J. Vector Ecol. 2004, 29, 323–330. [Google Scholar]
- Liew, C.; Curtis, C.F. Horizontal and vertical dispersal of dengue vector mosquitoes, Aedes aegypti and Aedes albopictus, in Singapore. Med. Vet. Entomol. 2004, 18, 351–360. [Google Scholar]
- Roslan, M.A.; Shafie, A.; Ngui, R.; Lim, Y.A.; Sulaiman, W.Y. Vertical infestation of the dengue vectors Aedes aegypti and Aedes albopictus in apartments in Kuala Lumpur, Malaysia. J. Am. Mosq. Control Assoc. 2013, 29, 328–336. [Google Scholar]
- Wan-Norafikah, O.; Nazni, W.A.; Noramiza, S.; Shafa’ar-Ko’ohar, S.; Azirol-Hisham, A.; Nor-Hafizah, R.; Sumarni, M.G.; Mohd-Hasrul, H.; Sofian-Azirun, M.; Lee, H.L. Vertical dispersal of Aedes (Stegomyia) spp. in high-rise apartments in Putrajaya, Malaysia. Trop. Biomed. 2010, 27, 662–667. [Google Scholar]
- Sairi, F.A.M.; Dom, N.C.; Camalxaman, S.N. Infestation profile of Aedes mosquitoes in multi-storey buildings in Selangor, Malaysia. Procedia Soc. Behav. Sci. 2016, 222, 283–289. [Google Scholar]
- Lee, H.L. Aedes ovitrap and larval survey in several suburban communities in Selangor, Malaysia. Mosq-Borne. Dis. Bull. 1992, 9, 9–15. [Google Scholar]
- Parija, S. Illustrated keys: Some mosquitoes of Peninsula Malaysia. Trop. Parasitol. 2014, 4, 70. [Google Scholar]
- Pratt, H.D.; Stojanovich, C.J.; Magennis, N.J. Workbook on Identification of Aedes Aegypti Larvae; U.S. Department of Health, Education and Welfare: Atlanta, GA, USA, 1964.
- IBM, C.R. IBM SPSS Statistics for Windows, Version 25.0; IBM Corp.: Armonk, NY, USA, 2017. [Google Scholar]
- Mahmud, M.; Mutalip, H.; Lodz, N.A.; Shahar, H. Study on key Aedes spp breeding containers in dengue outbreak localities in Cheras district, Kuala Lumpur. Int. J. Mosq. Res. 2018, 5, 23–30. [Google Scholar]
- Estrada-Franco, J.G.; Craig, G.B. Biology, Disease Relationships, and Control of Aedes Albopictus; Pan American Health Organization: Washington, DC, USA, 1995. [Google Scholar]
- Dieng, H.; Saifur, R.G.M.; Hassan, A.A.; Salmah, M.R.C.; Boots, M.; Satho, T.; Jaal, Z.; Abu Bakar, S. Indoor-breeding of Aedes albopictus in northern peninsular Malaysia and its potential epidemiological implications. PLoS ONE 2010, 5, e11790. [Google Scholar]
- Rozilawati, H.; Zairi, J.; Adanan, C.R. Seasonal abundance of Aedes albopictus in selected urban and suburban areas in Penang, Malaysia. Trop. Biomed. 2007, 24, 83–94. [Google Scholar]
- Hashim, N.A.; Ahmad, A.H.; Talib, A.; Athaillah, F.; Krishnan, K.T. Co-breeding association of Aedes albopictus (Skuse) and Aedes aegypti (Linnaeus) (Diptera: Culicidae) in relation to location and container size. Trop. Life. Sci. Res. 2018, 29, 213–227. [Google Scholar]
- Service, M.W. Mosquito (Diptera: Culicidae) dispersal—The long and short of it. J. Med. Entomol. 1997, 34, 579–588. [Google Scholar]
- Nyamah, M.A.; Sulaiman, S.; Omar, B. Categorization of potential breeding sites of dengue vectors in Johor, Malaysia. Trop. Biomed. 2010, 27, 33–40. [Google Scholar]
- Zainon, N.; Mohd-rahim, F.; Roslan, D.; Abd Samat, A.H. Prevention of Aedes breeding habitats for urban high-rise building in Malaysia. Plan. Malays. J. 2016, 14, 115–128. [Google Scholar]
- Costero, A.; Edman, J.D.; Clark, G.G.; Scott, T.W. Life table study of Aedes aegypti (Diptera: Culicidae) in Puerto Rico fed only human blood versus blood plus sugar. J. Med. Entomol. 1998, 35, 809–813. [Google Scholar]
- Dye, C. Vectorial capacity: Must we measure all its components? Parasitol. Today 1986, 2, 203–209. [Google Scholar]
- Harrington, L.C.; Edman, J.D.; Scott, T.W. Why do female Aedes aegypti (Diptera: Culicidae) feed preferentially and frequently on human blood? J. Med. Entomol. 2001, 38, 411–422. [Google Scholar]
- Hoffmann, E.J.; Miller, J.R. Reassessment of the role and utility of wind in suppression of mosquito (Diptera: Culicidae) host finding: Stimulus dilution supported over flight limitation. J. Med. Entomol. 2003, 40, 607–614. [Google Scholar]
- Hales, S.; de Wet, N.; Maindonald, J.; Woodward, A. Potential effect of population and climate changes on global distribution of dengue fever: An empirical model. Lancet 2002, 360, 830–834. [Google Scholar]


| Study Site | Total Number of Ovitraps |
|---|---|
| GC8 | 300 |
| GC10 | 500 |
| AP | 200 |
| FSK | 700 |
| PTM | 400 |
| ASW | 360 |
| TKP | 510 |
| KJA | 570 |
| KJC | 190 |
| Study Site | Ovitrap Collected | Ovitrap Index (%) | Ae. aegypti | Ae. albopictus | Ratio Ae. aegypti: Ae. albopictus | ||
|---|---|---|---|---|---|---|---|
| Total Larvae | Overall Percentage (%) | Total Larvae | Overall Percentage (%) | ||||
| GC8 | 297/300 | 48.00 ± 2.90 | 5216 | 94.02 | 332 | 5.98 | 15.7: 1 |
| GC10 | 454/500 | 41.00 ± 2.30 | 5258 | 84.63 | 955 | 15.37 | 5.5: 1 |
| AP | 200/200 | 63.00 ± 3.40 | 1640 | 62.60 | 980 | 37.40 | 1.7: 1 |
| FSK | 658/700 | 37.00 ± 1.90 | 3111 | 91.10 | 304 | 8.90 | 10.3: 1 |
| PTM | 371/400 | 37.00 ± 2.50 | 1614 | 76.17 | 505 | 23.83 | 3.2: 1 |
| ASW | 351/360 | 51.00 ± 2.70 | 4483 | 90.22 | 486 | 9.78 | 9.3: 1 |
| TKP | 448/510 | 55.00 ± 2.40 | 8847 | 92.45 | 722 | 7.55 | 12.3: 1 |
| KJA | 564/570 | 26.00 ± 1.90 | 1898 | 96.79 | 63 | 3.21 | 30.6: 1 |
| KJC | 188/190 | 31.00 ± 3.40 | 738 | 94.98 | 39 | 5.02 | 18.7: 1 |
| Study Site | Single Breeding | Cohabitation | |||||
|---|---|---|---|---|---|---|---|
| Ae. aegypti | Ae. albopictus | ||||||
| Percentage of Positive Ovitraps (%) | Mean Larvae per Ovitrap ± SE | Percentage of Positive Ovitraps (%) | Mean Larvae per Ovitrap ± SE | Percentage of Positive Ovitraps (%) | Mean Larvae per Ovitrap ± SE | Ratio Ae. aegypti: Ae. albopictus | |
| GC8 | 90.97 | 16.96 ± 1.66 | 5.56 | 0.79 ± 0.37 | 3.47 | 0.93 ± 0.45 | 1.86: 1.00 |
| GC10 | 78.38 | 10.56 ± 0.99 | 13.51 | 1.40 ± 0.39 | 8.11 | 1.73 ± 0.57 | 1.45: 1.00 |
| AP | 64.80 | 7.38 ± 0.91 | 21.60 | 4.14 ± 1.18 | 13.60 | 1.59 ± 0.45 | 1.08: 1.00 |
| FSK | 90.24 | 4.55 ± 0.34 | 6.91 | 0.38 ± 0.11 | 2.85 | 0.26 ± 0.10 | 2.31: 1.00 |
| PTM | 78.68 | 4.25 ± 0.50 | 18.38 | 1.16 ± 0.31 | 2.94 | 0.30 ± 0.16 | 1.00: 1.90 |
| ASW | 79.33 | 11.32 ± 1.22 | 10.61 | 0.89 ± 0.27 | 10.61 | 1.95 ± 0.51 | 2.10: 1.00 |
| TKP | 82.26 | 17.33 ± 1.50 | 6.05 | 0.45 ± 0.16 | 11.69 | 3.58 ± 0.74 | 2.92: 1.00 |
| KJA | 96.62 | 3.37 ± 0.30 | 3.38 | 0.11 ± 0.07 | 0.00 | 0.00 ± 0.00 | 0.00: 0.00 |
| KJC | 94.92 | 3.76 ± 0.53 | 3.39 | 0.11 ± 0.09 | 1.69 | 0.27 ± 0.27 | 1.78: 1.00 |
| Level | Approximate Height (m) | GC8 | GC10 | AP | FSK | PTM | ASW | TKP | KJA | KJC |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 0.0–3.0 | 36.16 ± 5.02 | 26.72 ± 3.71 | 14.90 ± 2.80 | 9.88 ± 1.40 | 14.10 ± 3.40 | 11.21 ± 3.08 | 36.29 ± 8.81 | 5.13 ± 1.73 | 4.10 ± 1.48 |
| 2 | 3.1–6.0 | 19.28 ± 3.91 | 12.99 ± 2.07 | 13.28 ± 2.68 | 6.57 ± 1.66 | 9.16 ± 2.62 | 15.83 ± 3.68 | 33.39 ± 8.59 | 1.67 ± 0.77 | 4.93 ± 1.53 |
| 3 | 6.1–9.0 | 14.22 ± 2.76 | 10.73 ± 2.25 | 14.18 ± 3.68 | 3.63 ± 1.05 | 6.05 ± 2.27 | 17.38 ± 3.82 | 20.21 ± 4.00 | 3.73 ± 1.07 | 3.76 ± 1.20 |
| 4 | 9.1–12.0 | 13.72 ± 3.34 | 10.04 ± 1.97 | 12.08 ± 3.99 | 6.23 ± 1.60 | 7.58 ± 3.56 | 9.38 ± 2.68 | 23.42 ± 7.21 | 2.59 ± 1.13 | 5.47 ± 1.52 |
| 5 | 12.1–15.0 | 10.53 ± 2.73 | 8.76 ± 2.08 | 11.08 ± 2.19 | 5.87 ± 1.42 | 7.83 ± 2.90 | 7.89 ± 2.67 | 17.90 ± 4.86 | 1.31 ± 0.91 | 2.23 ± 1.11 |
| 6 | 15.1–18.0 | 4.64 ± 1.59 | 5.44 ± 3.49 | 15.64 ± 4.04 | 14.75 ± 5.71 | 4.67 ± 1.12 | 4.31 ± 1.71 | |||
| 7 | 18.1–21.0 | 4.92 ± 1.81 | 5.45 ± 2.31 | 19.79 ± 5.25 | 25.25 ± 7.09 | 4.30 ± 1.75 | ||||
| 8 | 21.1–24.0 | 8.38 ± 1.81 | 3.12 ± 1.79 | 15.64 ± 4.41 | 17.21 ± 5.65 | 2.27 ± 1.28 | ||||
| 9 | 24.1–27.0 | 2.76 ± 1.51 | 5.50 ± 2.13 | 14.51 ± 4.21 | 12.86 ± 4.38 | 2.22 ± 0.97 | ||||
| 10 | 27.1–30.0 | 4.08 ± 1.28 | 3.25 ± 1.93 | 16.55 ± 8.33 | 4.07 ± 1.59 | |||||
| 11 | 30.1–33.0 | 1.53 ± 1.48 | 8.11 ± 3.44 | 19.61 ± 7.04 | 2.73 ± 1.09 | |||||
| 12 | 33.1–36.0 | 3.72 ± 1.29 | 9.06 ± 2.94 | 5.54 ± 2.86 | 3.03 ± 1.01 | |||||
| 13 | 36.1–39.0 | 3.15 ± 1.03 | 1.28 ± 0.80 | 23.00 ± 6.57 | 4.00 ± 1.68 | |||||
| 14 | 39.1–42.0 | 4.00 ± 1.41 | 4.58 ± 1.45 | 33.68 ± 7.43 | 2.80 ± 1.01 | |||||
| 15 | 42.1–45.0 | 5.23 ± 1.49 | 5.10 ± 2.69 | 10.86 ± 2.93 | 2.90 ± 1.23 | |||||
| 16 | 45.1–48.0 | 3.08 ± 1.10 | 0.89 ± 0.57 | 32.48 ± 8.58 | 2.97 ± 1.09 | |||||
| 17 | 48.1–51.0 | 5.31 ± 1.71 | 6.68 ± 2.46 | 17.73 ± 5.33 | 3.07 ± 1.18 | |||||
| 18 | 51.1–54.0 | 0.05 ± 0.05 | 3.90 ± 1.33 | |||||||
| 19 | 54.1–57.0 | 1.17 ± 0.76 | 8.66 ± 2.01 | |||||||
| 20 | 57.1–60.0 | 6.00 ± 2.29 | ||||||||
| 21 | 60.1–63.0 | 7.28 ± 4.52 | ||||||||
| r | −0.304 | −0.231 | −0.070 | −0.172 | −0.203 | −0.024 | −0.059 | 0.024 | −0.028 | |
| P | 0.000 | 0.000 | 0.322 | 0.000 | 0.000 | 0.657 | 0.211 | 0.576 | 0.705 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ab Hamid, N.; Mohd Noor, S.N.; Isa, N.R.; Md Rodzay, R.; Bachtiar Effendi, A.M.; Hafisool, A.A.; Azman, F.A.; Abdullah, S.F.; Kamarul Zaman, M.K.; Mohd Norsham, M.I.; et al. Vertical Infestation Profile of Aedes in Selected Urban High-Rise Residences in Malaysia. Trop. Med. Infect. Dis. 2020, 5, 114. https://doi.org/10.3390/tropicalmed5030114
Ab Hamid N, Mohd Noor SN, Isa NR, Md Rodzay R, Bachtiar Effendi AM, Hafisool AA, Azman FA, Abdullah SF, Kamarul Zaman MK, Mohd Norsham MI, et al. Vertical Infestation Profile of Aedes in Selected Urban High-Rise Residences in Malaysia. Tropical Medicine and Infectious Disease. 2020; 5(3):114. https://doi.org/10.3390/tropicalmed5030114
Chicago/Turabian StyleAb Hamid, Nurulhusna, Siti Nurfadhlina Mohd Noor, Nur Rasyidah Isa, Rohaiyu Md Rodzay, Ainaa Mardia Bachtiar Effendi, Afiq Ahnaf Hafisool, Fatin Atirah Azman, Siti Farah Abdullah, Muhammad Khairi Kamarul Zaman, Mohd Iqbal Mohd Norsham, and et al. 2020. "Vertical Infestation Profile of Aedes in Selected Urban High-Rise Residences in Malaysia" Tropical Medicine and Infectious Disease 5, no. 3: 114. https://doi.org/10.3390/tropicalmed5030114
APA StyleAb Hamid, N., Mohd Noor, S. N., Isa, N. R., Md Rodzay, R., Bachtiar Effendi, A. M., Hafisool, A. A., Azman, F. A., Abdullah, S. F., Kamarul Zaman, M. K., Mohd Norsham, M. I., Amanzuri, N. H., Abd Khalil, N., Zambari, I. F., Mat Rani, A. N., Ariffin, F. D., Omar, T., Wasi Ahmad, N., & Lee, H. L. (2020). Vertical Infestation Profile of Aedes in Selected Urban High-Rise Residences in Malaysia. Tropical Medicine and Infectious Disease, 5(3), 114. https://doi.org/10.3390/tropicalmed5030114





