Abstract
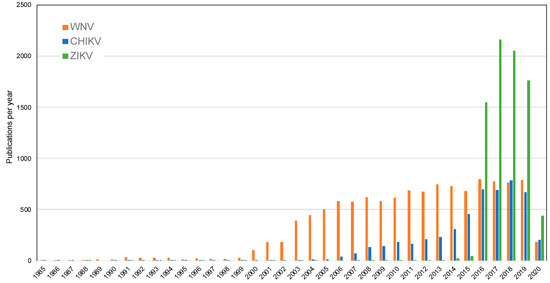
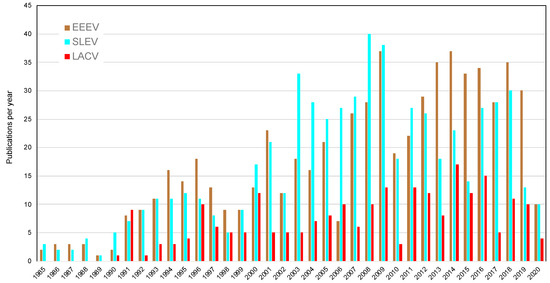
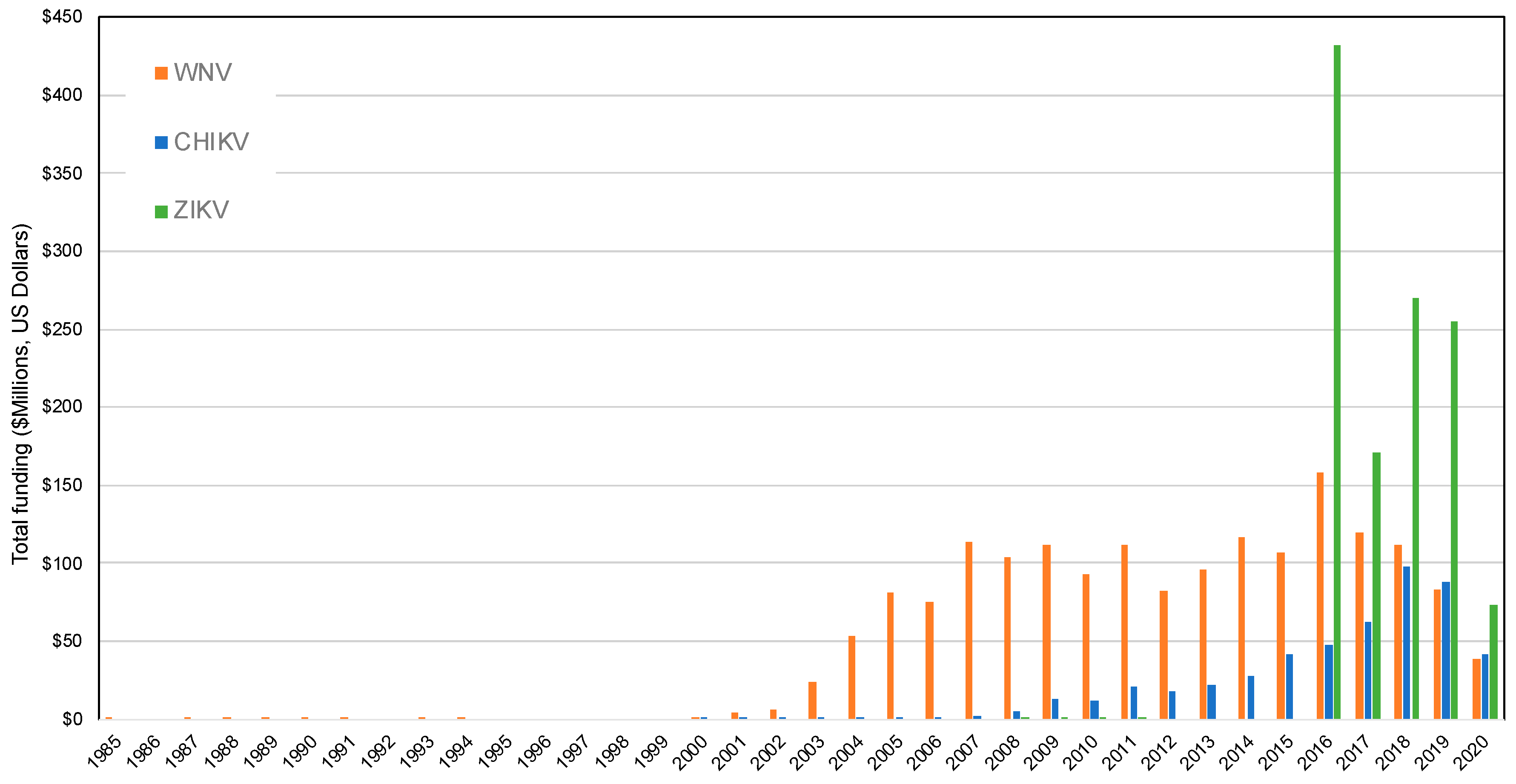
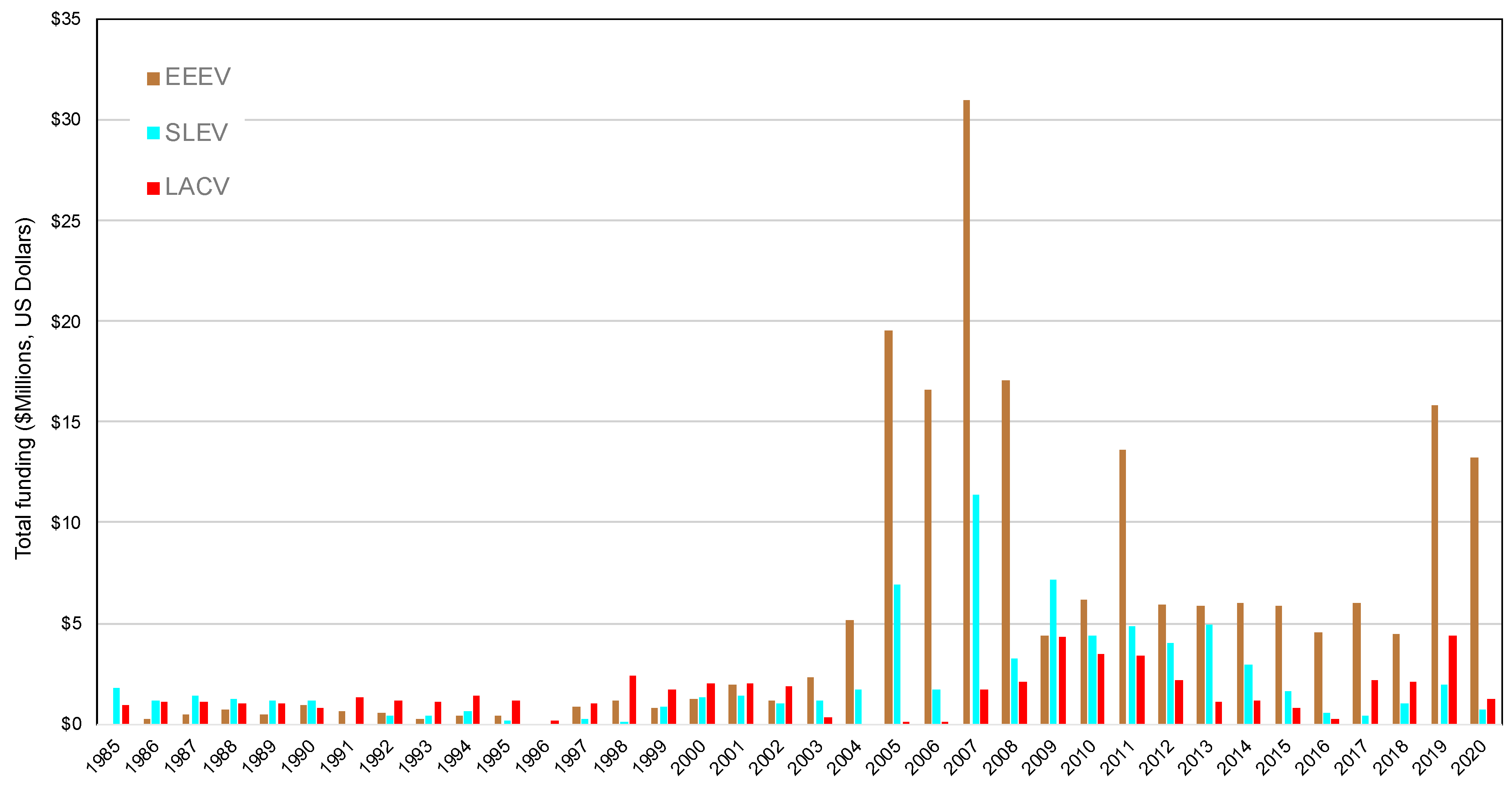
Mosquito-borne viruses will continue to emerge and generate a significant public health burden around the globe. Here, we provide a longitudinal perspective on how the emergence of mosquito-borne viruses in the Americas has triggered reactionary funding by sponsored agencies, stimulating a number of publications, innovative development of traps, and augmented capacity. We discuss the return on investment (ROI) from the oscillation in federal funding that influences demand for surveillance and control traps and leads to innovation and research productivity.
Keywords:
mosquito; emerging virus; outbreak; surveillance; trap; Aedes; Culex; Zika virus; West Nile virus 1. Introduction
While outbreaks of infectious diseases are devastating to human and animal populations, surges in private and public funding for outbreak pathogens have positively influenced research and innovation. Contemporary outbreak response efforts now incorporate digital media; electronic surveillance tools; mathematical modelling; sequencing; and teams of experts that include anthropologists, social scientists, and other diverse disciplinarians [1]. Outbreak stimulus funding leads to increased scientific productivity on outbreak pathogens, and incites innovation [2]. For example, an innovation workshop convened after an anthrax bioterrorism attack in 2001, to discuss new surveillance and pathogen detection approaches [3]. The Ebola Grand Challenge program, funded by the US Centers for Disease Control and Prevention (CDC), United States Agency for International Development (USAID), the United States Executive Office, and the Department of Defense, provided financial backing to 14 innovative projects to improve the response to Ebola outbreaks. These projects included protective suits, health care and technology solutions, and decontaminants [4]. The USAID Zika Grand Challenge program in 2016 received over 900 applications and provided 30 million dollars to innovative ideas to address Zika virus transmission [5]. Currently, during the COVID-19 pandemic, innovations are emerging such as new ventilators, drones delivering medical supplies, and the use of artificial intelligence in medicine [6,7,8,9]. Ideally, these scientific advances will aid in combatting the current epidemic as well as fuel innovation in preparedness for future emerging disease events, leading to return on investment (ROI).
The introduction and spread of numerous mosquito-borne viruses around the globe has also shepherded a wave of innovation to improve upon industry-standard sampling techniques that more efficiently capture the target vector species, physiological cohort, or virus-infected population of vectors [10]. Ramirez et al. [10] recently reviewed traditional surveillance approaches in the context of novel innovations that have advanced surveillance capacity, including pathogen surveillance from sugar feeding vectors, next-generation sequencing (eDNA (environmental DNA) for presence or absence of vectors in habitats), and xenosurveillance for vectors and pathogens. Additionally, modernized sampling strategies have also been expanded to incorporate technical advancements in such areas as infrared scanning, citizen science, and drones [11,12,13,14]. Driving the introduction and incorporation of novel trapping approaches to surveillance programs is the persistent emergence of mosquito-borne pathogens.
2. Arbovirus Emergence in the U.S.
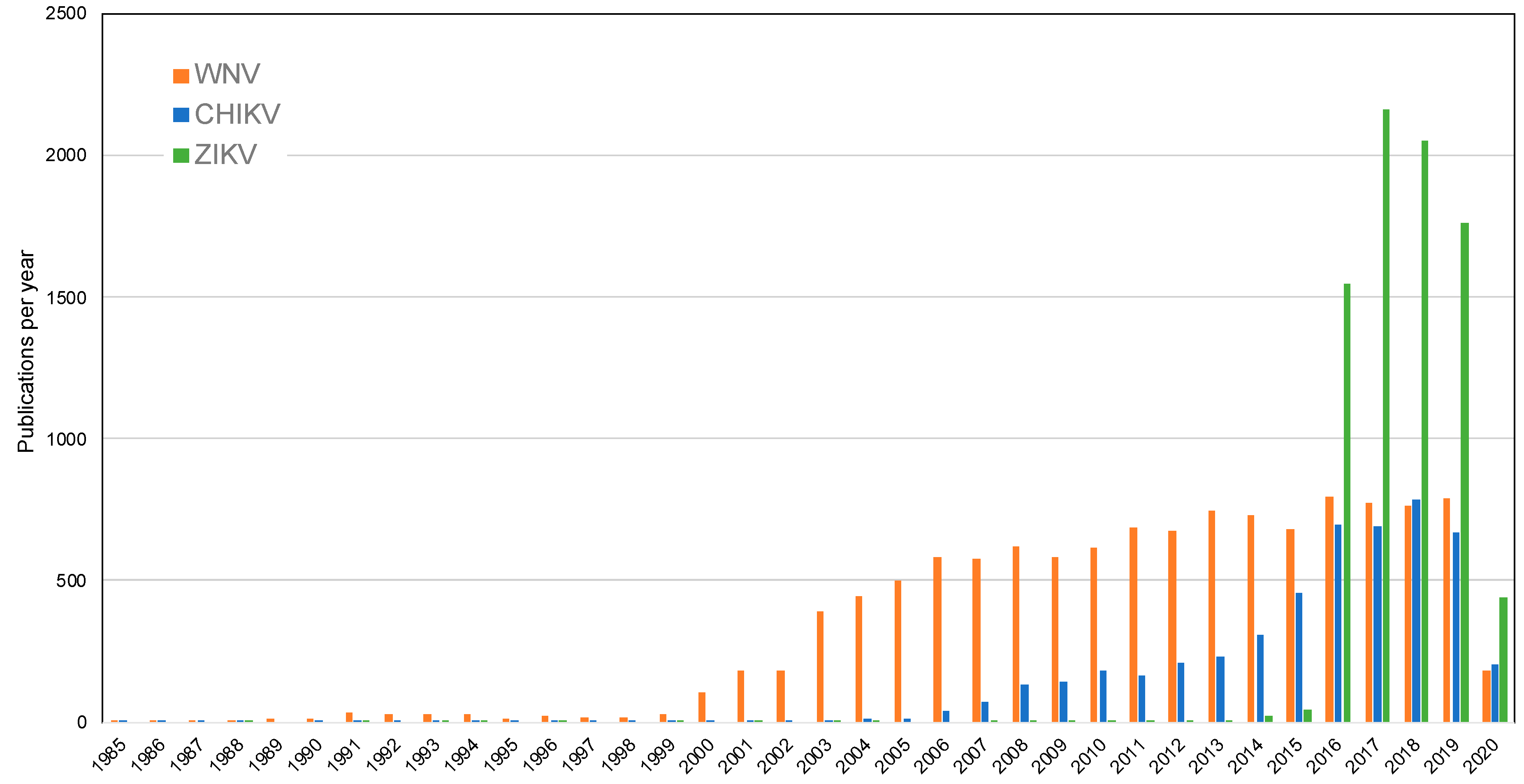
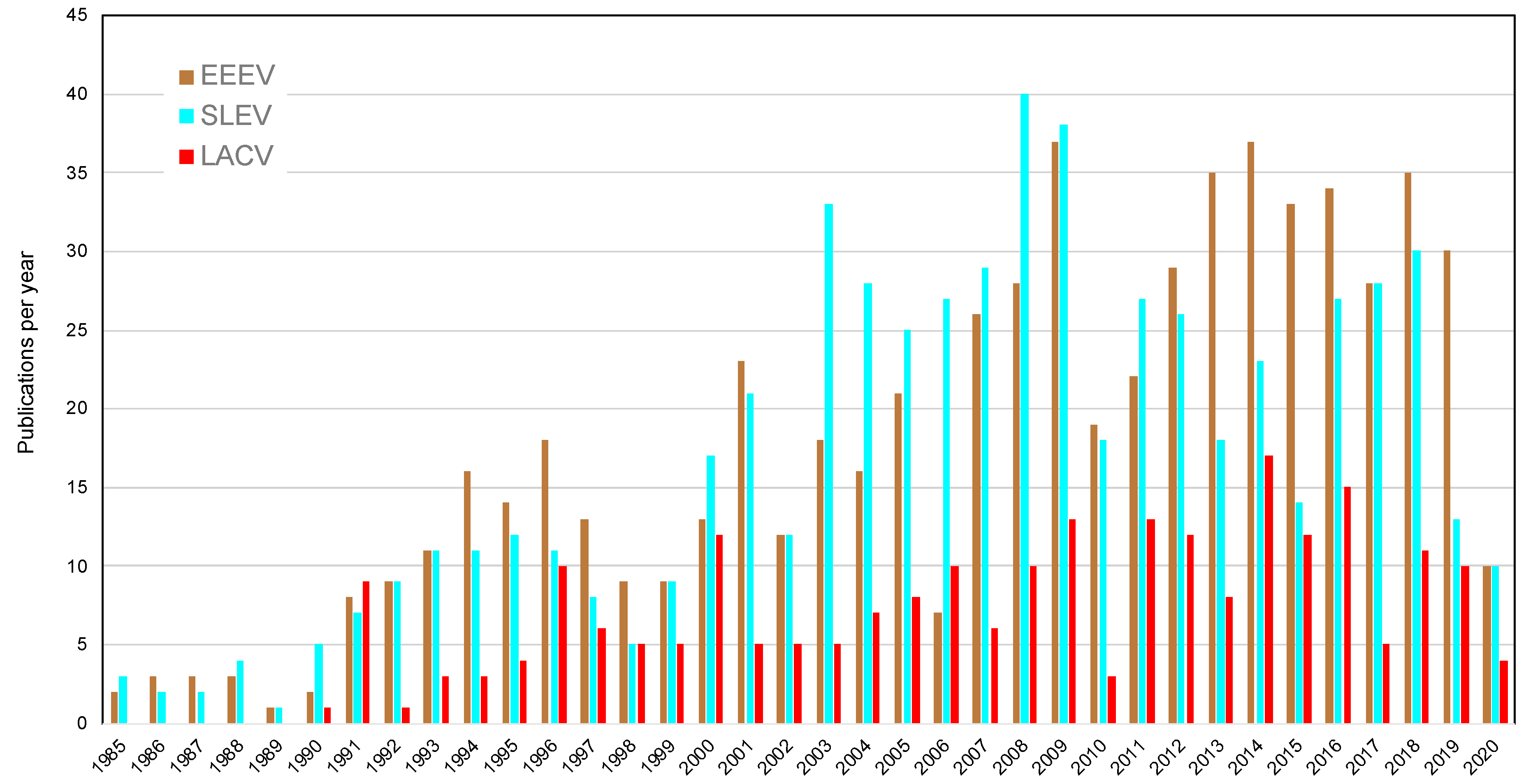
Many arboviruses cause a significant disease burden to the public each year. West Nile virus (WNV) (introduced in 1999), St. Louis encephalitis virus (SLEV), Jamestown Canyon virus (JCV), La Crosse encephalitis virus (LACV), Eastern equine encephalitis virus (EEEV), and Powassan (POWV, tick-borne) are tracked through the CDC database, ArboNET [15]. In the last several years, incidence of JCV and POWV has been increasing [15,16,17,18]. Additionally, a multistate outbreak of EEEV occurred in the northeastern US in 2019, in which the 34 reported cases far exceeded the historical average of around eight cases/year [19]. Through the first half of the 20th century, Western equine encephalitis virus (WEEV) was also widespread and caused significant morbidity and mortality in humans and horses; however, this virus has largely disappeared from most areas over the past several decades for unconfirmed reasons, with the last human case in the United States reported in 1999 [20,21].
In 2013, chikungunya (CHIKV) was first reported in the Americas, followed by Zika virus (ZIKV) two years later [22,23]. These virus invasions came during a time of increasing dengue virus (DENV) incidence, range expansion, and replacement of dominant serotypes in different geographic areas [24,25,26]. The Pan American Health Organization (PAHO) reported a 30% increase in the number of dengue cases, from 7,641,334 between 2001 and 2010 to 10,851,043 between 2011 and 2017 [26,27]. Intensive transmission of Aedes-borne viruses in the Americas coupled with the expanding range of Ae. aegypti mosquitoes presents a continual threat of these viruses gaining a foothold in the United States as well [28,29,30]. To date, cases of DENV, ZIKV, and CHIKV in the United States have predominately been traveler-associated, with the exception of local transmission of ZIKV in Florida and Texas during 2017 [31,32].
4. Innovation of Mosquito Surveillance Tools
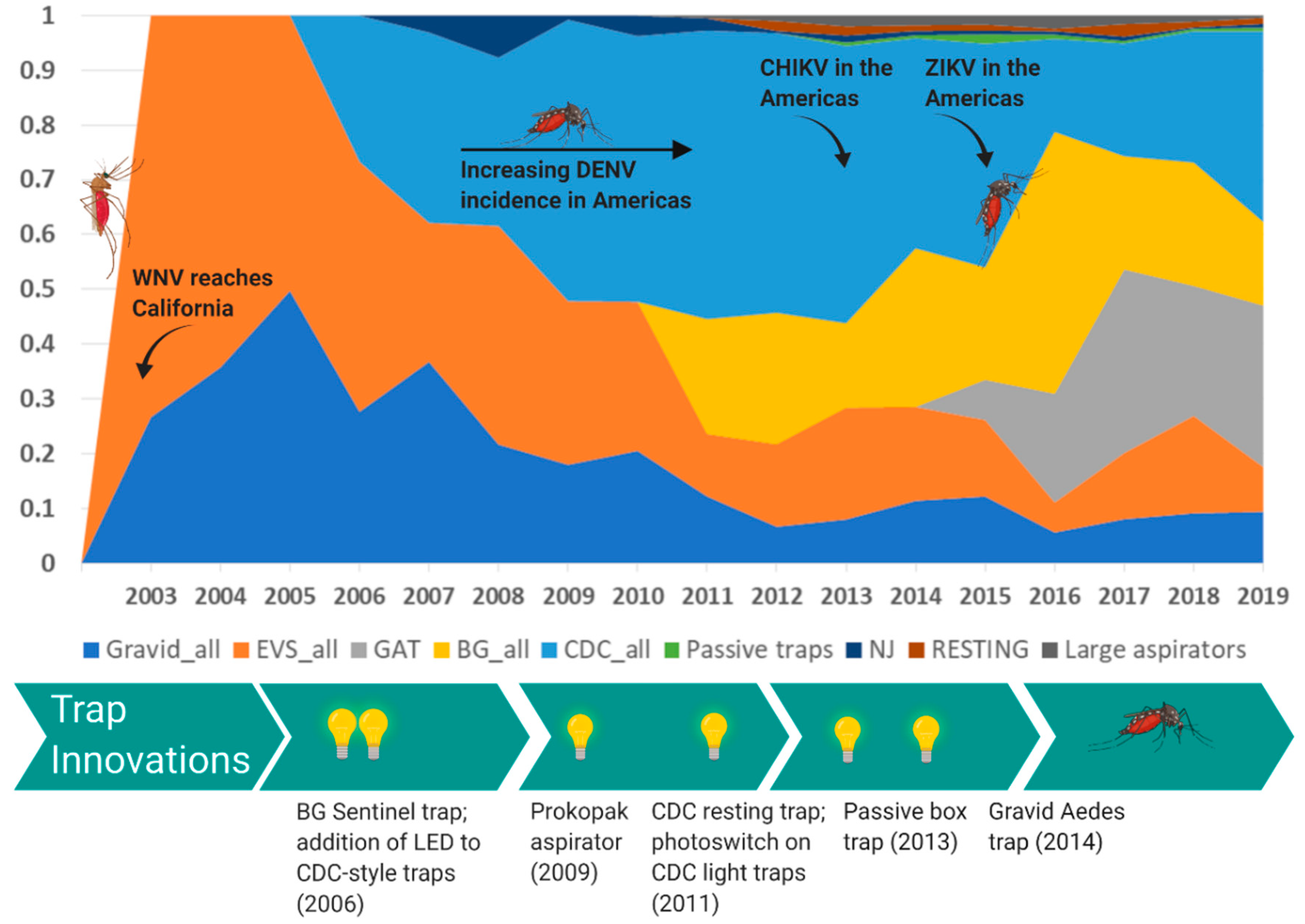
The evolution of mosquito trapping tools targeting Culex and Aedes mosquitoes has followed suit, being driven by the emergence of these viruses, the resulting resources generated by federal agencies, and consumer demand. To visualize trends in trap usage over time, we evaluated BioQuip Products sales data in each main trap category between 2003 and 2019 (Figure 5). As the United States has experienced emergences and threats of first Culex and now also Aedes-borne viruses, innovations to traditional mosquito trapping tools targeting these vector groups have arisen, with the proportion of sales in different categories fluctuating over time in response to arbovirus outbreak and funding availability (Figure 1). The diversity of traps sold by BioQuip Products also increased substantially from two categories in 2003 to nine categories by 2014 (Figure 3) as new innovations came to market. Undoubtedly, the surge of Aedes-borne viruses in particular during this time period has influenced the development and sales of novel traps targeting Ae. aegypti mosquitoes.
Figure 5.
Proportion of traps sold per year by BioQuip Products. Product numbers represented included: Gravid traps (2800, 2800S), BG traps (2880, 2883), NJ light trap (2856), EVS traps (2801A, 2780, 2780NS1, 2780NS2), Centers for Disease Control and Prevention (CDC) traps (2848, 2770, 2836BQ, 2836BQX), resting traps (2799), Gravid Aedes Traps (2797), passive traps (2887, 2887P), large aspirators (2888A, 2846). Inset: Proportion of trap types sold per year by BioQuip Products. Product numbers represented included: Gravid traps (2800, 2800S), BG traps (2880, 2883), NJ light trap (2856, 2857, 2858), EVS traps (2801A, 2780, 2780NS1, 2780NS2), CDC traps (2848, 2770, 2836BQ, 2836BQX), resting traps (2799), Gravid Aedes Traps (2797), passive traps (2887, 2887P), and large aspirators (2888A, 2846).
4.1. Culex-Borne Virus Surveillance
The CDC light trap has become an industry standard for collection of mosquitoes for the purposes of arbovirus surveillance. The similar EVS (Encephalitis Vector Survey) trap [39] is also routinely used for arbovirus surveillance and operates on a similar principle as the CDC light trap using light and carbon dioxide (CO2) as attractants. Between 2003 and 2010, trap sales were dominated by suction traps using light and CO2 as attractants, and gravid traps, largely for Culex vectors of WNV and SLEV. Due to the sustained threat of WNV year after year [36], traps targeting Culex vectors are expected to remain a mainstay in the industry.
Several specific innovations have either improved the functionality of the standard light trap or targeted different physiological cohorts of mosquitoes. In 2006, BioQuip released the first commercially available light-emitting-diode (LED) CDC-style light trap with customizable colors (Figure 3). Bayonet mounted LED chips were also available to replace the white incandescent lights in existing CDC style light traps. The passive box trap offered an alternative to CDC light traps, by providing a CO2-baited trap that was not reliant on a power source and could be used to sample arbovirus vectors in more remote areas [40]. A collapsible passive trap was also developed to address portability issues [41]. A photo switch option also added to light traps, allowing researchers the flexibility to set traps when convenient and conserve battery power. Finally, the CDC resting trap was introduced in 2011 for the purpose of collecting blood-engorged mosquitoes to determine vertebrate host utilization [42]. Passive and resting traps represent a smaller proportion of sales over the last several years, suggesting their utility may be serving the research community as opposed to being integrated into large-scale operational surveillance activities.
4.2. Aedes-Borne Virus Surveillance
Surveillance for viruses transmitted by Ae. aegypti mosquitoes requires very different tools and strategies than for those used for Culex-borne viruses. These urbanized, day-biting, container-breeding mosquitoes are generally not attracted to the suction and gravid traps that are so efficient at catching Culex mosquitoes [43]. The growing need for traps that effectively collected Aedes mosquitoes led to the innovation of the BG Sentinel Mosquito Trap in 2006 (Biogents AG, Regensburg, Germany) [44], among others. BG sentinel traps began selling at BioQuip in 2011, and sales comprised approximately 50% of the total traps sold by BioQuip in 2016 following the introduction of CHIKV and ZIKV to the Americas (Figure 3). Similarly, gravid Aedes traps (GAT) [45,46] were introduced between 2013 and 2014. Conceptually based on traditional gravid traps [47], these traps do not require electricity to function. GAT sales quickly grew to approximately 30% of the traps sold by BioQuip in 2016 (Figure 5). The InsectaZooka© and the Prokopak aspirator [48] are lightweight, portable field aspirators developed as an alternative to backpack models. These devices facilitate the collection of resting and engorged mosquitoes from indoor and outdoor resting sites.
5. Conclusions
The emergence of mosquito-borne viruses has occurred repeatedly in recent decades, and studies predict that these emergences will continue. Much of our response to these events is reactionary, triggered by the increase in attention, funding, publication, innovation, and preventive measures for public health. The long-term impact or return on investment of outbreak spending is evidenced by scientific advancements (publications) and innovation, but we advocate for a more sustainable, economical, and effective approach by minimizing the oscillations of boom and bust in funding and capacity for mosquito-borne viruses. Our goal should be to optimize the cost-effectiveness of budgetary spending by adopting resource allocation for biosecurity threats that maximize benefits while minimizing the total cost given anticipated expenditures incurred in the event of mosquito-borne viral outbreaks [49,50].
Author Contributions
Conceptualization, G.L.H., R.C.K., and L.W.C.; data curation, K.F.; writing—original draft preparation, R.C.K.; writing—review and editing, R.C.K., G.L.H., L.W.C., and K.F.; visualization, R.C.K., G.L.H., and L.W.C.; project administration, G.L.H.; funding acquisition, G.L.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded in part by the Department of Homeland Security (DHS) Science and Technology Directorate (S&T) under agreement # HSHQDC-17-C-B0003.
Acknowledgments
The viewpoints described herein represent those of the authors and not necessarily their institutions or funding agency.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Houlihan, C.F.; Whitworth, J.A. Outbreak science: Recent progress in the detection and response to outbreaks of infectious diseases. Clin. Med. 2019, 19, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Jayabalisingham, B.; Hessen, M.; James, C. Infectious Disease Outbreak Research: Insights and Trends 2020 [Webinar] In Scopus Webinar Series. Available online: https://www.brighttalk.com/webcast/13703/391874. (accessed on 1 April 2020).
- Pavlin, J.A.; Mostashari, F.; Kortepeter, M.G.; Hynes, N.A.; Chotani, R.A.; Mikol, Y.B.; Ryan, M.A.K.; Neville, J.S.; Gantz, D.T.; Writer, J.V.; et al. Innovative Surveillance Methods for Rapid Detection of Disease Outbreaks and Bioterrorism: Results of an Interagency Workshop on Health Indicator Surveillance. Am. J. Public Health 2003, 93, 1230–1235. [Google Scholar] [CrossRef] [PubMed]
- USAID. Fighting Ebola: A Grand Challenge for Development. Available online: http://www.ebolagrandchallenge.net (accessed on 7 April 2020).
- USAID. Combating Zika | Grand Challenge for Development | U.S. Agency for International Development. Available online: https://www.usaid.gov/grandchallenges/zika (accessed on 25 April 2020).
- Bashir, N. James Dyson Designed a New Ventilator in 10 days. He’s Making 15,000 for the Pandemic Fight. Available online: https://www.cnn.com/2020/03/26/tech/dyson-ventilators-coronavirus/index.html (accessed on 7 April 2020).
- Bhatt, K.; Pourmand, A.; Sikka, N. Targeted Applications of Unmanned Aerial Vehicles (Drones) in Telemedicine. Telemed. E-Health 2018, 24, 833–838. [Google Scholar] [CrossRef] [PubMed]
- Roblin, S. Will Blood-Bearing Delivery Drones Transform Disaster Relief and Battlefield Medicine? Available online: https://www.forbes.com/sites/sebastienroblin/2019/10/22/will-blood-bearing-delivery-drones--transform-disaster-relief-and-battlefield-medicine/ (accessed on 7 April 2020).
- Shapiro, G. How Innovation Is Helping Mitigate the Coronavirus Threat; STAT: Boston, MA, USA, 2020. [Google Scholar]
- Ramírez, A.; Meyer, D.; Ritchie, S. Searching for the proverbial needle in a haystack: Advances in mosquito-borne arbovirus surveillance. Parasit. Vectors 2018, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Cohnstaedt, L.; Ladner, J.; Campbell, L.; Busch, N.; Barrera, R. Determining Mosquito Distribution from Egg Data: The Role of the Citizen Scientist. Am. Biol. Teach. 2016, 78, 317–322. [Google Scholar] [CrossRef]
- Esperança, P.M.; Blagborough, A.M.; Da, D.F.; Dowell, F.E.; Churcher, T.S. Detection of Plasmodium berghei infected Anopheles stephensi using near-infrared spectroscopy. Parasit. Vectors 2018, 11, 377. [Google Scholar] [CrossRef]
- Fernandes, J.N.; Dos Santos, L.M.B.; Chouin-Carneiro, T.; Pavan, M.G.; Garcia, G.A.; David, M.R.; Beier, J.C.; Dowell, F.E.; Maciel-De-Freitas, R.; Sikulu-Lord, M.T. Rapid, noninvasive detection of Zika virus in mosquitoes by near-infrared spectroscopy. Sci. Adv. 2018, 4, eaat0496. [Google Scholar] [CrossRef]
- Norris, D.; Ray, A.; Guda, T.; Keogh, E.; Singh, S.; Zhu, Y.; Debboun, M.; Reyna, M.; Vigilant, M.; Carpi, G.; et al. Project premonition project: Field trials of a robotic smart trap for mosquito identification and bionomics. Am. J. Trop. Med. Hyg. 2017, 97, 610–611. [Google Scholar]
- Curren, E.J.; Lehman, J.; Kolsin, J.; Walker, W.L.; Martin, S.W.; Staples, J.E.; Hills, S.L.; Gould, C.V.; Rabe, I.B.; Fischer, M.; et al. West Nile Virus and Other Nationally Notifiable Arboviral Diseases—United States, 2017. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1137–1142. [Google Scholar] [CrossRef]
- Gaensbauer, J.T.; Lindsey, N.P.; Messacar, K.; Staples, J.E.; Fischer, M. Neuroinvasive arboviral disease in the United States: 2003 to 2012. Pediatrics 2014, 134, e642–e650. [Google Scholar] [CrossRef]
- Krow-Lucal, E.R.; Lindsey, N.P.; Fischer, M.; Hills, S.L. Powassan Virus Disease in the United States, 2006–2016. Vector Borne Zoonotic Dis. 2018, 18, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Pastula, D.M.; Hoang Johnson, D.K.; White, J.L.; Dupuis, A.P.; Fischer, M.; Staples, J.E. Jamestown Canyon Virus Disease in the United States-2000–2013. Am. J. Trop. Med. Hyg. 2015, 93, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Lindsey, N.P.; Martin, S.W.; Staples, J.E.; Fischer, M. Notes from the Field: Multistate Outbreak of Eastern Equine Encephalitis Virus—United States, 2019. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 50–51. [Google Scholar] [CrossRef] [PubMed]
- Adams, D.; Gallagher, K.; Jajosky, R.A.; Ward, J.; Sharp, P.; Anderson, W.; Abellera, J.; Aranas, A.; Mayes, M.; Wodajo, M.; et al. Summary of Notifiable Diseases—United States, 2010. Morb. Mortal. Wkly. Rep. 2010, 59, 1–111. [Google Scholar]
- Robb, L.L.; Hartman, D.A.; Rice, L.; deMaria, J.; Bergren, N.A.; Borland, E.M.; Kading, R.C. Continued Evidence of Decline in the Enzootic Activity of Western Equine Encephalitis Virus in Colorado. J. Med. Entomol. 2019, 56, 584–588. [Google Scholar] [CrossRef]
- Fischer, M.; Staples, J.E. Arboviral Diseases Branch, National Center for Emerging and Zoonotic Infectious Diseases, CDC Notes from the field: Chikungunya virus spreads in the Americas—Caribbean and South America, 2013–2014. MMWR Morb. Mortal. Wkly. Rep. 2014, 63, 500–501. [Google Scholar]
- Zanluca, C.; de Melo, V.C.A.; Mosimann, A.L.P.; Santos, G.I.V.D.; Santos, C.N.D.D.; Luz, K. First report of autochthonous transmission of Zika virus in Brazil. Mem. Inst. Oswaldo Cruz 2015, 110, 569–572. [Google Scholar] [CrossRef]
- Balmaseda, A.; Standish, K.; Mercado, J.C.; Matute, J.C.; Tellez, Y.; Saborío, S.; Hammond, S.N.; Nuñez, A.; Avilés, W.; Henn, M.R.; et al. Trends in patterns of dengue transmission over 4 years in a pediatric cohort study in Nicaragua. J. Infect. Dis. 2010, 201, 5–14. [Google Scholar] [CrossRef]
- Brathwaite, D.O.; San Martín, J.L.; Montoya, R.H.; del Diego, J.; Zambrano, B.; Dayan, G.H. The history of dengue outbreaks in the Americas. Am. J. Trop. Med. Hyg. 2012, 87, 584–593. [Google Scholar] [CrossRef]
- Salles, T.S.; da Encarnação Sá-Guimarães, T.; de Alvarenga, E.S.L.; Guimarães-Ribeiro, V.; de Meneses, M.D.F.; de Castro-Salles, P.F.; Dos Santos, C.R.; do Amaral Melo, A.C.; Soares, M.R.; Ferreira, D.F.; et al. History, epidemiology and diagnostics of dengue in the American and Brazilian contexts: A review. Parasit. Vectors 2018, 11, 264. [Google Scholar] [CrossRef]
- PAHO. Number of Reported Cases of Dengue and Dengue Hemorrhagic Fever (DHF), Region of the Americas (by Country and Subregion) 1980–2018. Available online: https://www.paho.org/data/index.php/en/mnu-topics/indicadores-dengue-en/dengue-nacional-en/252-dengue-pais-ano-en.html (accessed on 7 April 2020).
- Kraemer, M.U.G.; Reiner, R.C.; Brady, O.J.; Messina, J.P.; Gilbert, M.; Pigott, D.M.; Yi, D.; Johnson, K.; Earl, L.; Marczak, L.B.; et al. Past and future spread of the arbovirus vectors Aedes aegypti and Aedes albopictus. Nat. Microbiol. 2019, 4, 854–863. [Google Scholar] [CrossRef] [PubMed]
- Pless, E.; Gloria-Soria, A.; Evans, B.R.; Kramer, V.; Bolling, B.G.; Tabachnick, W.J.; Powell, J.R. Multiple introductions of the dengue vector, Aedes aegypti, into California. PLoS Negl. Trop. Dis. 2017, 11, e0005718. [Google Scholar] [CrossRef] [PubMed]
- Ryan, S.J.; Carlson, C.J.; Mordecai, E.A.; Johnson, L.R. Global expansion and redistribution of Aedes-borne virus transmission risk with climate change. PLoS Negl. Trop. Dis. 2019, 13, e0007213. [Google Scholar] [CrossRef] [PubMed]
- Castro, L.A.; Fox, S.J.; Chen, X.; Liu, K.; Bellan, S.E.; Dimitrov, N.B.; Galvani, A.P.; Meyers, L.A. Assessing real-time Zika risk in the United States. BMC Infect. Dis. 2017, 17, 284. [Google Scholar] [CrossRef] [PubMed]
- Florida State Health Department. Department of Health Daily Zika Update | Florida Department of Health. Available online: http://www.floridahealth.gov/newsroom/2017/01/012717-zika-update.html (accessed on 18 April 2020).
- Kaplan, S. Congress Approves $1.1 Billion in Zika Funding. Available online: https://www.scientificamerican.com/article/congress-approves-1-1-billion-in-zika-funding/ (accessed on 15 April 2020).
- MMWR. Assessing Capacity for Surveillance, Prevention, and Control of West Nile Virus Infection—United States, 1999 and 2004. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5506a2.htm (accessed on 15 April 2020).
- Hadler, J.; Patel, D.; Bradley, K.; Hughes, J.; Blackmore, C.; Etkind, P.; Kan, L.; Getchell, J.; Blumenstock, J.; Engel, J. National Capacity for Surveillance, Prevention, and Control of West Nile Virus and Other Arbovirus Infections—United States, 2004 and 2012. MMWR Morb. Mortal. Wkly. Rep. 2014, 63, 281–284. [Google Scholar]
- CDC. Statistics & Maps | West Nile Virus | CDC. Available online: https://www.cdc.gov/westnile/statsmaps/index.html (accessed on 18 April 2020).
- CDC. CDC Awards Nearly $184 Million to Continue the Fight against Zika. Available online: https://www.cdc.gov/media/releases/2016/p1222-zika-funding.html (accessed on 15 April 2020).
- CDC. ELC 5-year Focus, Funding, and Impact | DPEI | CDC. Available online: https://www.cdc.gov/ncezid/dpei/elc/history-of-elc.html (accessed on 25 April 2020).
- Rohe, D.L.; Fall, R.P. A miniature Battery Powered CO2 Baited Light Trap for Mosquito Borne Encephalitis Surveillance. Available online: https://eurekamag.com/research/000/583/000583985.php (accessed on 7 March 2019).
- Ritchie, S.A.; Cortis, G.; Paton, C.; Townsend, M.; Shroyer, D.; Zborowski, P.; Hall-Mendelin, S.; Van Den Hurk, A.F. A simple non-powered passive trap for the collection of mosquitoes for arbovirus surveillance. J. Med. Entomol. 2013, 50, 185–194. [Google Scholar] [CrossRef]
- Meyer, D.B.; Johnson, B.J.; Fall, K.; Buhagiar, T.S.; Townsend, M.; Ritchie, S.A. Development, Optimization, and Field Evaluation of the Novel Collapsible Passive Trap for Collection of Mosquitoes. J. Med. Entomol. 2018, 55, 706–710. [Google Scholar] [CrossRef]
- Panella, N.A.; Crockett, R.J.K.; Biggerstaff, B.J.; Komar, N. The Centers for Disease Control and Prevention resting trap: A novel device for collecting resting mosquitoes. J. Am. Mosq. Control Assoc. 2011, 27, 323–325. [Google Scholar] [CrossRef]
- Service, M. Mosquito Ecology: Field Sampling Methods, 2nd ed.; Springer eBook Collection; Springer: Dordrecht, The Netherland, 1993; ISBN 978-94-015-8113-4. [Google Scholar]
- Maciel-de-Freitas, R.; Eiras, A.E.; Lourenço-de-Oliveira, R. Field evaluation of effectiveness of the BG-Sentinel, a new trap for capturing adult Aedes aegypti (Diptera: Culicidae). Mem. Inst. Oswaldo Cruz 2006, 101, 321–325. [Google Scholar] [CrossRef]
- Eiras, A.E.; Buhagiar, T.S.; Ritchie, S.A. Development of the gravid Aedes trap for the capture of adult female container-exploiting mosquitoes (Diptera: Culicidae). J. Med. Entomol. 2014, 51, 200–209. [Google Scholar] [CrossRef]
- Mackay, A.J.; Amador, M.; Barrera, R. An improved autocidal gravid ovitrap for the control and surveillance of Aedes aegypti. Parasit. Vectors 2013, 6, 225. [Google Scholar] [CrossRef] [PubMed]
- Reiter, P. A revised version of the CDC Gravid Mosquito Trap. J. Am. Mosq. Control Assoc. 1987, 3, 325–327. [Google Scholar] [PubMed]
- Vazquez-Prokopec, G.M.; Galvin, W.A.; Kelly, R.; Kitron, U. A new, cost-effective, battery-powered aspirator for adult mosquito collections. J. Med. Entomol. 2009, 46, 1256–1259. [Google Scholar] [CrossRef] [PubMed]
- Kompas, T.; Chu, L.; Pham, V.H.; Spring, D. Budgeting and portfolio allocation for biosecurity measures—Kompas. Aust. J. Agric. Resour. Econ. 2019, 63, 412–438. [Google Scholar] [CrossRef]
- Kompas, T.; Che, T.N.; Ha, P.V.; Chu, L. Cost–Benefit Analysis for Biosecurity Decisions. In Invasive Species: Risk Assessment and Management; Cambridge University Press: Cambridge, UK, 2017. [Google Scholar]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).