‘Know Your Epidemic’: Are Prisons a Potential Barrier to TB Elimination in an Australian Context?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Analysis
2.2. Ethics Statement
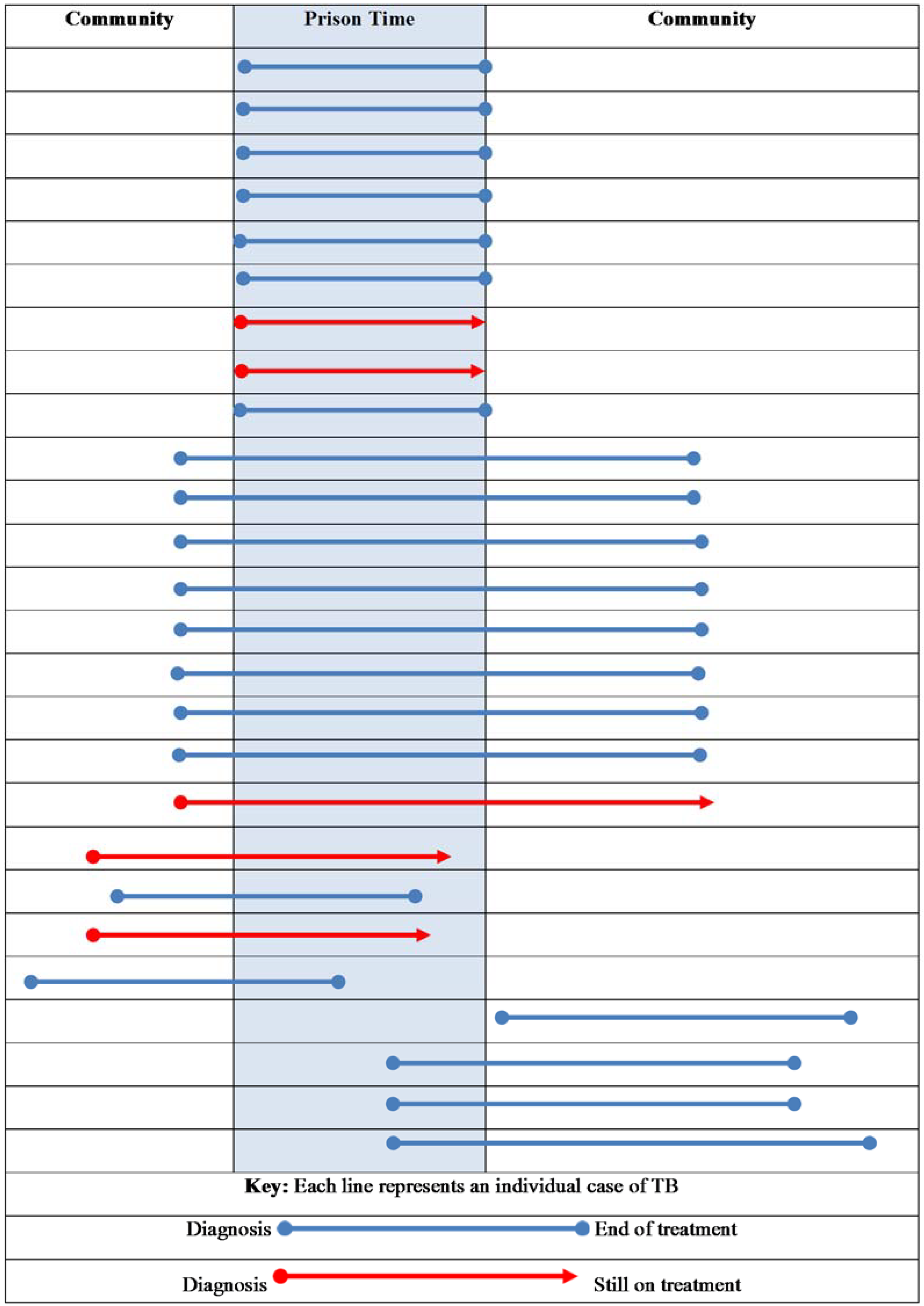
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bone, A.; Aerts, A.; Grzemska, M.; Kimerling, M.; Kluge, H.; Michael, L.; Françoise, P.; Mario, R.; Francis, V. Tuberculosis Control in Prisons: A Manual for Programme Managers; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Centres for Disease Control and Prevention. Prevention and Control of Tuberculosis in Correctional and Detention Facilities: Recommendations from CDC; Centres for Disease Control and Prevention: Atlanta, GA, USA, 2006.
- Macneil, J.R.; Lobato, M.N.; Moore, M. An Unanswered health disparity: Tuberculosis among correctional inmates, 1993 through 2003. Am. J. Public Health 2005, 95, 1800–1805. [Google Scholar] [CrossRef] [PubMed]
- Baussano, I.; Williams, B.G.; Nunn, P.; Beggiato, M.; Fedeli, U.; Scano, F. Tuberculosis incidence in prisons: A systematic review. PLoS Med. 2010, 7, 1470. [Google Scholar] [CrossRef] [PubMed]
- Lambert, L.A.; Armstrong, L.R.; Lobato, M.N.; Ho, C.; France, A.M.; Haddad, M.B. Tuberculosis in jails and prisons: United States, 2002–2013. Am. J. Public Health 2016, 106, 2231–2237. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, C.J.; Chitnis, A.S.; Barry, P.M.; Shah, N. Tuberculosis trends in California correctional facilities, 1993–2013. Int. J. Tuberc. Lung Dis. 2017, 21, 922–929. [Google Scholar] [CrossRef] [PubMed]
- Butler, T.; Levy, M. Mantoux positivity among prison inmates—New South Wales, 1996. Aust. N. Z. J. Public Health 1999, 23, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.H.; Butler, T.G.; Zhou, J. Prevalence of Mantoux positivity and annual risk of infection for tuberculosis in New South Wales Prisoners, 1996 and 2001. N. S. W. Public Health Bull. 2007, 18, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Department of Health & Human Services, State Government of Victoria, Australia. Notify a Condition Now. 2018. Available online: https://www2.health.vic.gov.au/public-health/infectious-diseases/notify-condition-now (accessed on 9 August 2018).
- Dale, K.; Tay, E.; Trevan, P.; Denholm, J.T. Mortality among tuberculosis cases in Victoria, 2002–2013: Case fatality and factors associated with death. Int. J. Tuberc. Lung Dis. 2016, 20, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2003. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02003?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2004. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02004?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2005. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02005?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2006. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02006?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2007. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02007?OpenDocument (accessed on 01 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2008. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02008?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2009. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02009?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2010. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02010?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2011. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02011?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2012. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02012?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2013. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02013?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2014. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02014?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2015. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02015?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2016. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02016?OpenDocument (accessed on 1 August 2018).
- Australian Bureau of Statistics. 4517.0-Prisoners in Australia. 2017. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02017?OpenDocument (accessed on 1 August 2018).
- Department of Health & Human Services, State Government of Victoria, Australia. Management, Control and Prevention of Tuberculosis Guidelines for Health Care Providers. 2015. Available online: https://www2.health.vic.gov.au/about/publications/policiesandguidelines/tuberculosis-guidelines-2015 (accessed on 25 August 2018).
- Dale, K.D.; Globan, M.; Tay, E.L.; Trauer, J.M.; Trevan, P.G.; Denholm, J.T. Recurrence of tuberculosis in a low-incidence setting without directly observed treatment: Victoria, Australia, 2002–2014. Int. J. Tuberc. Lung Dis. 2017, 21, 550–555. [Google Scholar] [CrossRef] [PubMed]
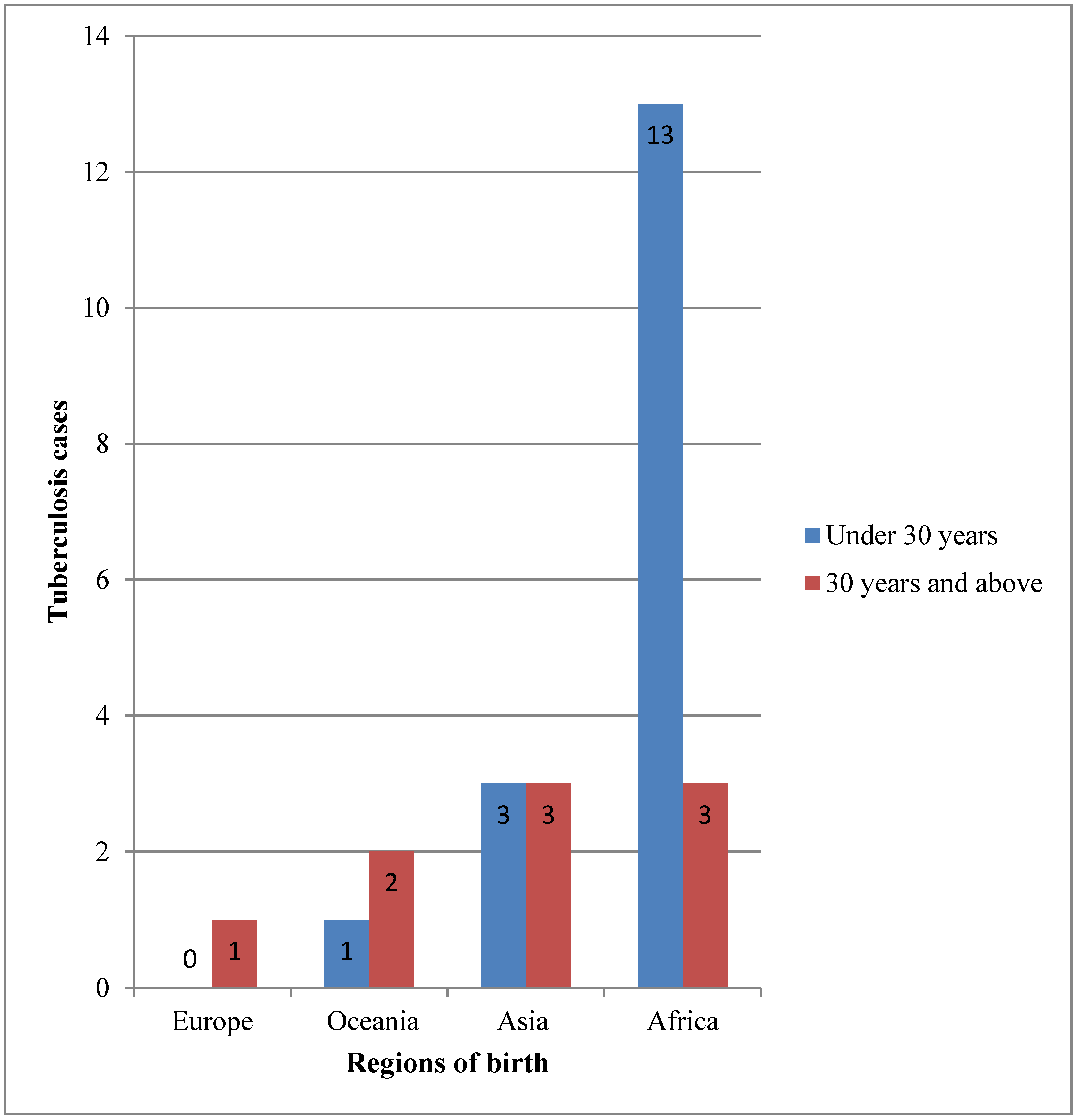
| Variables | Prison | General TB Population | p Value 3 | ||
|---|---|---|---|---|---|
| n | (%) | n | (%) | ||
| Total | 26 | 5619 | |||
| Gender | |||||
| Male | 24 | (92.3) | 3058 | (54.4) | |
| Female | 2 | (7.7) | 2561 | (45.6) | <0.0001 |
| Age in years | |||||
| <30 | 17 | (65.4) | 2257 | (40.2) | |
| ≥30 | 9 | (34.6) | 3362 | (59.8) | 0.008 |
| Median age (IQR) | 26.5 | (23–36) | 33 | (25–53) | 0.0271 4 |
| Country of birth | |||||
| Australian | 2 | (7.7) | 573 | (10.2) | |
| Overseas | 24 | (92.3) | 5041 | (89.7) | |
| Not stated | 0 | (0.0) | 5 | (0.1) | 1.000 |
| Site of disease | |||||
| Pulmonary | 13 | (50) | 2353 | (41.9) | |
| Pulmonary plus other sites | 5 | (19.2) | 759 | (13.5) | |
| Extrapulmonary | 8 | (30.8) | 2507 | (44.6) | 0.315 |
| Sputum smear positive 1 | 10 | (38.5) | 941 | (30.2) | 0.047 |
| Lung cavity on chest X ray (CXR) or computed tomography (CT) 1 | 7 | (38.9) | 6 06 | (6.0) | 0.099 |
| Drug susceptibility testing 2 | |||||
| Fully susceptible | 19 | (100) | 3958 | (91.1) | |
| MDR TB | 0 | (0.0) | 80 | (1.8) | |
| Mono- or polyresistant (not MDR TB) | 0 | (0.0) | 290 | (6.7) | |
| Not tested or recorded | 0 | (0.0) | 19 | (0.4) | NC |
| Treatment history | |||||
| New case | 22 | (84.6) | 5377 | (95.7) | |
| Relapse following full treatment | 4 | (15.4) | 150 | (2.7) | |
| Relapse following partial treatment | 0 | (0.0) | 54 | (1.0) | |
| Unknown/not stated | 0 | (0.0) | 38 | (0.7) | 0.018 |
| Treatment Outcome/Assessable Outcomes | Total | TB Cases with Prison History during Treatment | General TB Population | ||||
|---|---|---|---|---|---|---|---|
| n | % | (95% CI) | n | % | (95% CI) | ||
| Treatment success (completed treatment or cured) | 4839 | 21 | 91.3 | (70.4–97.9) | 4818 | 95.9 | (95.3–96.5) |
| Interrupted treatment | 27 | 1 | 4.4 | (0.6–26.1) | 26 | 0.5 | (0.4–0.8) |
| Defaulted | 63 | 1 | 4.4 | (0.6–26.1) | 62 | 1.2 | (1.0–1.6) |
| Died of tuberculosis | 52 | 0 | 0.0 | 52 | 1.0 | (0.8–1.4) | |
| Failure | 0 | 0 | 0.0 | 0 | 0.0 | ||
| Lost to follow-up, outcome unknown | 64 | 0 | 0.0 | 64 | 1.3 | (1.0–1.6) | |
| Total assessable | 5045 | 23 | 100.0 | 5022 | 100 | ||
| Non-accessible outcomes | |||||||
| Transferred out of Australia | 228 | 0 | 0.0 | 228 | 38.2 | (34.4–42.2) | |
| Died of other causes | 178 | 0 | 0.0 | 178 | 29.8 | (26.3–33.6) | |
| Still under treatment | 194 | 3 | 1.0 | 191 | 32.0 | (28.4–35.9) | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moyo, N.; Tay, E.L.; Denholm, J. ‘Know Your Epidemic’: Are Prisons a Potential Barrier to TB Elimination in an Australian Context? Trop. Med. Infect. Dis. 2018, 3, 93. https://doi.org/10.3390/tropicalmed3030093
Moyo N, Tay EL, Denholm J. ‘Know Your Epidemic’: Are Prisons a Potential Barrier to TB Elimination in an Australian Context? Tropical Medicine and Infectious Disease. 2018; 3(3):93. https://doi.org/10.3390/tropicalmed3030093
Chicago/Turabian StyleMoyo, Nompilo, Ee Laine Tay, and Justin Denholm. 2018. "‘Know Your Epidemic’: Are Prisons a Potential Barrier to TB Elimination in an Australian Context?" Tropical Medicine and Infectious Disease 3, no. 3: 93. https://doi.org/10.3390/tropicalmed3030093
APA StyleMoyo, N., Tay, E. L., & Denholm, J. (2018). ‘Know Your Epidemic’: Are Prisons a Potential Barrier to TB Elimination in an Australian Context? Tropical Medicine and Infectious Disease, 3(3), 93. https://doi.org/10.3390/tropicalmed3030093






