Trends in Tuberculosis Incidence in the Australian-Born in Victoria: Opportunities and Challenges to Elimination
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Demographics
3.2. Clinical Characteristics
3.3. Treatment Outcomes
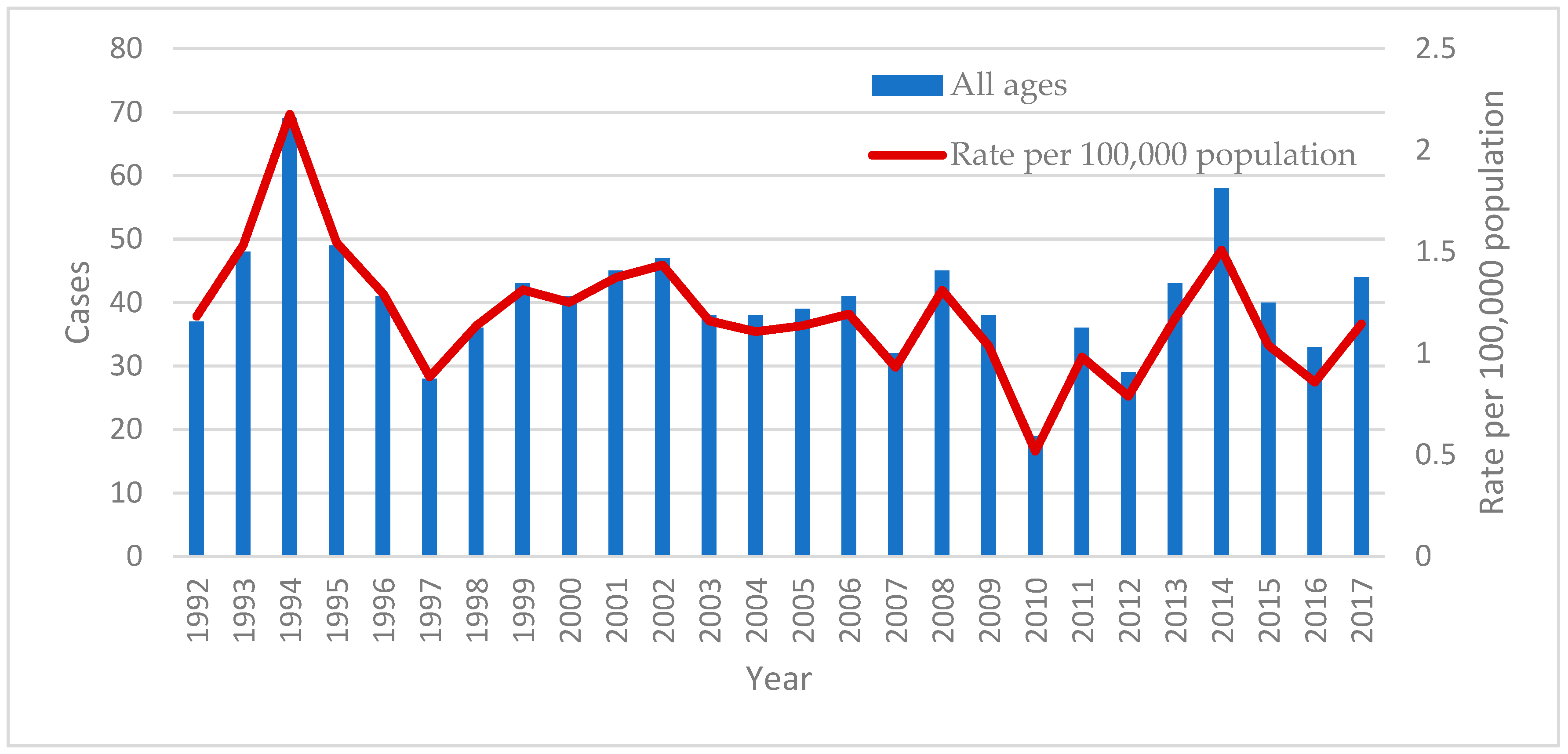
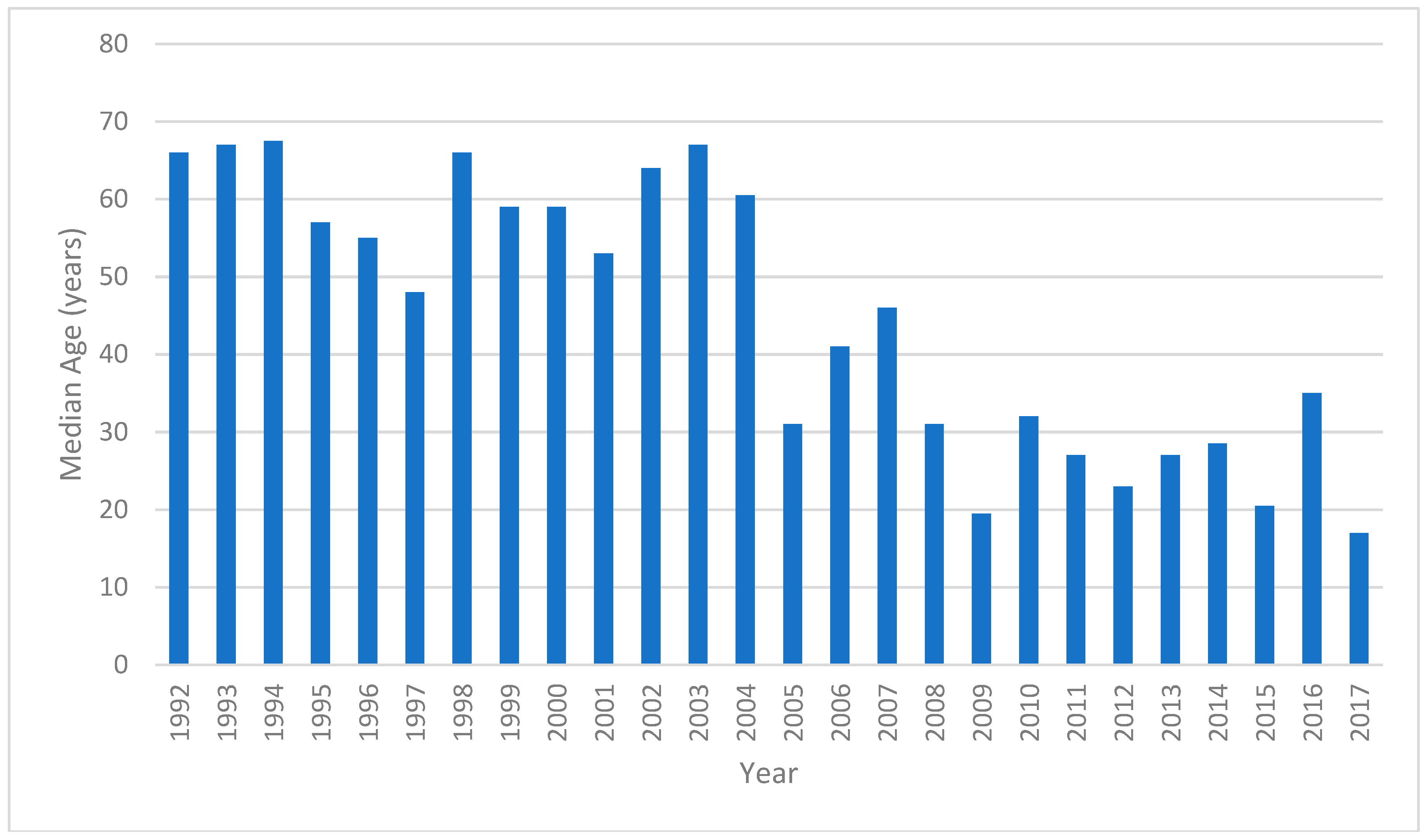
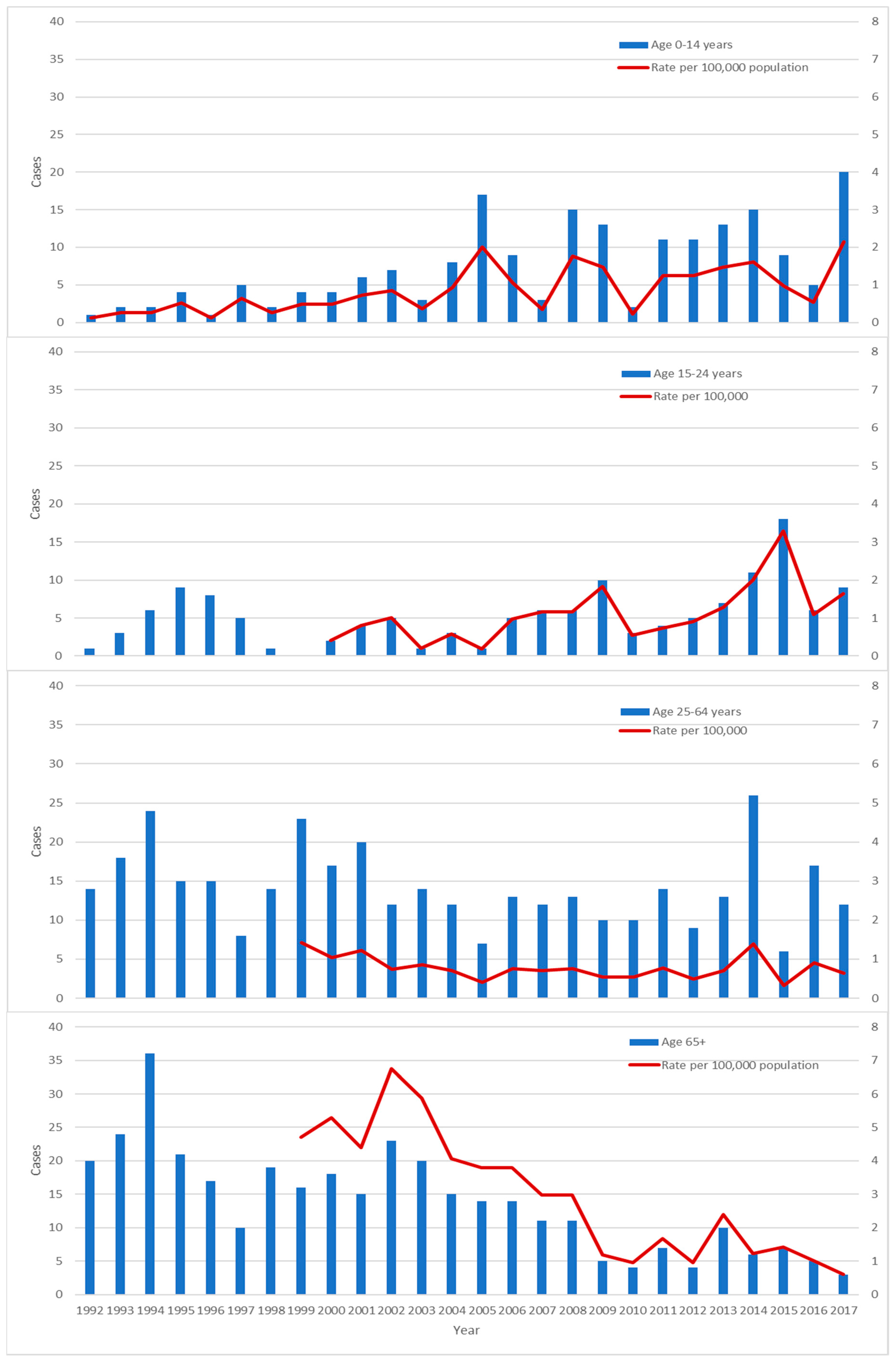
3.4. Trends
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization (WHO). The End TB Strategy: Global Strategy and Targets for Tuberculosis Prevention, Care and Control after 2015; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Lonnroth, K.; Migliori, G.B.; Abubakar, I.; D’Ambrosio, L.; de Vries, G.; Diel, R.; Douglas, P.; Falzon, D.; Gaudreau, M.A.; Goletti, D.; et al. Towards tuberculosis elimination: An action framework for low-incidence countries. Eur. Respir. J. 2015, 45, 928–952. [Google Scholar] [CrossRef] [PubMed]
- Toms, C.; Stapledon, R.; Waring, J.; Douglas, P. Tuberculosis notifications in Australia, 2012 and 2013. Commun. Dis. Intell. Q. Rep. 2015, 39, 217–235. [Google Scholar]
- Lavender, C.J.; Globan, M.; Kelly, H.; Brown, L.K.; Sievers, A.; Fyfe, J.A.; Lauer, T.; Leslie, D.E. Epidemiology and control of tuberculosis in Victoria, a low-burden state in south-eastern Australia, 2005–2010. Int. J. Tuberc. Lung Dis. 2013, 17, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Bareja, C.; Waring, J.; Stapledon, R.; Toms, C.; Douglas, P. Tuberculosis notifications in Australia, 2011. Commun. Dis. Intell. Q. Rep. 2014, 38, 356–368. [Google Scholar]
- 3101.0: Australian Demographic Statistics. September 2017. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/mf/3101.0 (accessed on 17 June 2018).
- Tuberculosis Case Definition. Available online: http://www.health.gov.au/internet/main/publishing.nsf/content/cda-surveil-nndss-casedefs-cd_tb.htm (accessed on 19 June 2018).
- WHO. Tuberculosis Country Profiles. Available online: http://www.who.int/tb/country/data/profiles/en/ (accessed on 26 June 2018).
- Dale, K.; Tay, E.; Trevan, P.; Denholm, J.T. Mortality among tuberculosis cases in Victoria, 2002–2013: Case fatality and factors associated with death. Int. J. Tuberc. Lung Dis. 2016, 20, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Census of Population and Housing. 1991. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2101.01991?OpenDocument (accessed on 23 June 2018).
- Census of Population and Housing. 1996. Available online: http://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/1996/communityprofile/2?opendocument (accessed on 23 June 2018).
- Census of Population and Housing. 2001. Available online: http://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2001/quickstat/2?opendocument (accessed on 23 June 2018).
- Census of Population and Housing. 2006. Available online: http://abs.gov.au/websitedbs/censushome.nsf/home/historicaldata2006 (accessed on 23 June 2018).
- Census of Population and Housing. 2011. Available online: http://www.abs.gov.au/websitedbs/censushome.nsf/home/historicaldata2011?opendocument&navpos=280 (accessed on 23 June 2018).
- Census of Population and Housing. 2016. Available online: http://www.abs.gov.au/websitedbs/D3310114.nsf/Home/Census?OpenDocument&ref=topBar (accessed on 23 June 2018).
- McPherson, M.E.; Leslie, D.; Sievers, A.; Patel, M.; Kelly, H. Epidemiology of laboratory confirmed tuberculosis in Victoria, 1990 to 2004. Commun. Dis. Intell. Q. Rep. 2008, 32, 237–241. [Google Scholar] [PubMed]
- Globan, M.; Lavender, C.; Leslie, D.; Brown, L.; Denholm, J.; Raios, K.; Sievers, A.; Kelly, H.; Fyfe, J. Molecular epidemiology of tuberculosis in Victoria, Australia, reveals low level of transmission. Int. J. Tuberc. Lung Dis. 2016, 20, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Dale, K.D.; Globan, M.; Tay, E.L.; Trauer, J.M.; Trevan, P.G.; Denholm, J.T. Recurrence of tuberculosis in a low-incidence setting without directly observed treatment: Victoria, Australia, 2002–2014. Int. J. Tuberc. Lung Dis. 2017, 21, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Parvaresh, L.; Crighton, T.; Martinez, E.; Bustamante, A.; Chen, S.; Sintchenko, V. Recurrence of tuberculosis in a low-incidence setting: A retrospective cross-sectional study augmented by whole genome sequencing. BMC Infect. Dis. 2018, 18, 265. [Google Scholar] [CrossRef] [PubMed]
- Teo, S.S.; Tay, E.L.; Douglas, P.; Krause, V.L.; Graham, S.M. The epidemiology of tuberculosis in children in Australia, 2003–2012. Med. J. Aust. 2015, 203, 440. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.J.; Johnston, V.; Appuhamy, R.D.; Kaczmarek, M.; Hurwitz, M. The epidemiology of tuberculosis in the Australia Capital Territory, 2006–2015. Commun. Dis. Intell. Q. Rep. 2017, 41, 231–240. [Google Scholar]
- 3412.0—Migration, Australia, 2016–2017. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/mf/3412.0/ (accessed on 8 August 2018).
- Denholm, J.T.; McBryde, E.S. Can Australia eliminate TB? Modelling immigration strategies for reaching MDG targets in a low-transmission setting. Aust. N. Z. J. Public Health 2014, 38, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Denholm, J.T.; Matteelli, A.; Reis, A. Latent tuberculous infection: Ethical considerations in formulating public health policy. Int. J. Tuberc. Lung Dis. 2015, 19, 137–140. [Google Scholar] [CrossRef] [PubMed]
- ASID. Recommendations for Comprehensive Post-Arrival Health Assessment for People from Refugee-Like Backgrounds; Australian Society for Infectious Diseases: Surry Hills, NSW, Australia, 2016.
- The BCG vaccine: Information and recommendations for use in Australia. National Tuberculosis Advisory Committee update October 2012. Commun. Dis. Intell. Q. Rep. 2013, 37, 65–72.
| Characteristic | All Ages | 0–14 Years | ≥15 Years |
|---|---|---|---|
| Number of cases | 1057 | 192 | 865 |
| Median age (IQR) | 47 years (20, 73) | 3 years (2, 7) | 57 years (31, 76) |
| Male (%) | 618 (58.5) | 106 (55.2) | 512 (59.2) |
| Metropolitan (%) | 830 (78.5) | 178 (92.7) | 652 (75.4) |
| HIV co-infection 1 | 7 | 0 | 7 |
| Method of diagnosis (%) | |||
| Culture | 712 (67.4) | 62 (32.3) | 650 (75.1) |
| Radiologic | 145 (13.7) | 96 (50.0) | 49 (5.7) |
| Nucleic acid testing/microscopy | 61 (5.8) | 14 (7.3) | 47 (5.4) |
| Histology | 39 (3.7) | 3 (1.6) | 36 (4.2) |
| Clinical | 34 (3.2) | 12 (6.3) | 22 (2.5) |
| Missing | 66 (6.2) | 5 (2.6) | 61 (7.1) |
| Multi-drug resistance 2 | 8 | 1 | 7 |
| Manifestation (%) 3 | |||
| Pulmonary only | 610 (57.7) | 106 (55.2) | 504 (58.3) |
| Pulmonary and extrapulmonary | 128 (12.1) | 25 (13.0) | 103 (11.9) |
| Miliary | 20 (1.9) | 6 (3.1) | 14 |
| Extrapulmonary only | 273 (25.8) | 59 (30.7) | 214 (24.7) |
| Extrapulmonary manifestations | |||
| Lymphadenitis | 127 (12.0) | 50 (26.0) | 77 (8.9) |
| Pleural | 105 (9.9) | 6 (3.1) | 99 (11.4) |
| Bone/joint | 38 (3.6) | 5 (2.6) | 33 (3.8) |
| Genitourinary | 33 (3.1) | 1 (0.5) | 32 (3.7) |
| Meningeal | 18 (1.7) | 9 (4.7) | 9 (1.0) |
| Cutaneous | 7 (0.7) | 1 (0.5) | 6 (0.7) |
| Pericardial | 5 (0.5) | 0 | 5 (0.6) |
| Other | 5 (0.5) | 2 (1.0) | 3 (0.3) |
| Recurrence (%) | 13 (1.2) | 2 (1.0) | 11 (1.3) |
| Treatment outcomes 4 | |||
| Median duration (IQR) | 212 days (184, 278) | ||
| Completed treatment | 508 | 140 | 368 |
| Still on treatment | 36 | 18 | 18 |
| Death during treatment | 57 | 0 | 57 |
| Death from TB | 8 | 0 | 8 |
| Default | 4 | 1 | 3 |
| Lost to follow-up | 8 | 2 | 6 |
| Country or Region | Number (%) |
|---|---|
| Total | 149 |
| Africa | 60 (40.3) |
| Sudan | 24 (16.1) |
| Somalia | 25 (16.8) |
| Ethiopia | 9 (6.0) |
| Algeria | 1 (0.7) |
| Zimbabwe | 1 (0.7) |
| Southeast Asia | 49 (32.9) |
| Vietnam | 26 (17.4) |
| Philippines | 9 (6.0) |
| Indonesia | 3 (2.0) |
| Malaysia | 2 (1.3) |
| Timor-Leste | 2 (1.3) |
| Laos | 3 (2.0) |
| Cambodia | 3 (2.0) |
| Myanmar | 1 (0.7) |
| North Asia | 7 (4.7) |
| China | 6 (4.0) |
| Tibet | 1 (0.7) |
| South Asia | 15 (10.0) |
| India | 14 (9.4) |
| Pakistan | 1 (0.7) |
| Middle East | 8 (5.4) |
| Afghanistan | 7 (4.7) |
| Iraq | 1 (0.7) |
| Pacific Islands | 9 (6.0) |
| Tonga | 4 (2.7) |
| Samoa | 4 (2.7) |
| Fiji | 1 (0.7) |
| South America | |
| Peru | 1 (0.7) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xie, O.; Tay, E.L.; Denholm, J. Trends in Tuberculosis Incidence in the Australian-Born in Victoria: Opportunities and Challenges to Elimination. Trop. Med. Infect. Dis. 2018, 3, 112. https://doi.org/10.3390/tropicalmed3040112
Xie O, Tay EL, Denholm J. Trends in Tuberculosis Incidence in the Australian-Born in Victoria: Opportunities and Challenges to Elimination. Tropical Medicine and Infectious Disease. 2018; 3(4):112. https://doi.org/10.3390/tropicalmed3040112
Chicago/Turabian StyleXie, Ouli, Ee Laine Tay, and Justin Denholm. 2018. "Trends in Tuberculosis Incidence in the Australian-Born in Victoria: Opportunities and Challenges to Elimination" Tropical Medicine and Infectious Disease 3, no. 4: 112. https://doi.org/10.3390/tropicalmed3040112
APA StyleXie, O., Tay, E. L., & Denholm, J. (2018). Trends in Tuberculosis Incidence in the Australian-Born in Victoria: Opportunities and Challenges to Elimination. Tropical Medicine and Infectious Disease, 3(4), 112. https://doi.org/10.3390/tropicalmed3040112






