Abstract
Studies on the burden of COVID-19 cases in Colombia have focused on specific populations and short timeframes. A retrospective observational study was conducted on adult patients aged 18 diagnosed with COVID-19 who received inpatient and/or outpatient medical care at a large health maintenance organization, to evaluate the burden of COVID-19 cases in Colombia (from March 2020 to January 2023) and associations with demographic and clinical characteristics. COVID-19 cases were identified with ICD-10 codes and confirmed by a laboratory test. The statistical analysis focused on descriptors of the frequency of events. A multivariate regression model was used to identify factors associated with severe conditions and death. Of the 953,661 cases detected, most cases (~79%) were mild or moderate (handled as outpatients). There were 20.1% (N = 191,260) severe cases and 0.9% (N = 8841) critical cases. Most COVID patients were unvaccinated (94.6%) and had, on average, one comorbidity. Hypertension (19.1%), immunocompromised condition (23.8%), mental health conditions (15%), obesity (10.8%), and cancer (11.2%) were the common prevalent comorbidities. The presence of comorbidity increased the risk of severe or critical COVID-19. COVID-19 cases were associated with the lack of vaccination and comorbidities. Effective vaccination strategies are needed to reduce the burden of COVID-19 in Colombia and, considering budgetary constraints, it is advisable to prioritize the elderly or populations with underlying conditions.
1. Introduction
The burden of coronavirus disease (COVID-19) has been vast and multifaceted, affecting countries worldwide with different degrees of severity, leading to unprecedented health crises, economic disruptions, and social challenges [1,2].
COVID-19 manifests itself in many degrees of severity, ranging from no symptoms to a severe illness that may involve respiratory failure, septic shock, and problems with multiple organs [3]. Although most cases of COVID-19 are asymptomatic, mild, or moderate, they run the underlying risk of becoming severe or even life-threatening. Moreover, symptoms can persist and debilitate the patient [4]. According to some studies, around 5–10% of patients with the disease require hospitalization [5]. Those most at risk have a chronic illness or are immunocompromised, pregnant, or over 65 years of age [3,6].
Different resources have been developed in Colombia to mitigate the impact of COVID-19, with appropriate measures coordinated through multiple public policies [7]. For instance, vaccination against COVID-19 was implemented in accordance with a national plan, which began on 17 February 2021. The prioritized populations were soon extended to all adults on July 17 of the same year [8]. However, the disease continues to represent a public health problem, as evidenced by the current Ten-Year Public Health Plan [9]. The constant evolution of the disease remains a concern, as well as the changes in the behavior of the general population regarding awareness, prevention, and vaccination [10,11].
Although different studies have been carried out in the country to understand the characteristics of patients infected with COVID-19, they have each approached the issue with a specific focus. Research has been conducted with short timeframes [12] and on populations in certain cities [13], the elderly [14], patients with specific risk factors [15], and cases involving hospitalization [16,17]. To comprehend the evolution of the disease and make appropriate public policies, it is crucial to analyze the demographic and clinical characteristics of COVID-19 cases over the extended period of the pandemic. Therefore, the current contribution aimed to evaluate the burden of COVID-19 cases in Colombia (from March 2020 to January 2023) and associations with demographic and clinical characteristics by analyzing a large sample of adult databases.
2. Materials and Methods
2.1. Study Design and Population
A retrospective observational study was carried out on adult patients diagnosed with COVID-19. The sample population had received inpatient and/or outpatient medical care at one of the largest health maintenance organizations (HMOs) in Colombia, which covers 10.08% of the population (~5 million people), according to the Ministry of Health [18]. The data were extracted from an integrated clinical records database from March 2020 to January 2023, identifying adult cases using International Classification of Diseases 10th Revision codes for COVID-19. A diagnosis had to be confirmed with a laboratory test for a case to be considered.
This study used structured databases and was approved by the institutional ethical committee of SURA (Comité de ética y BPC en investigación en salud, CEI-SURA) by Act No. 101 dated 19 July 2023. Informed consent was unnecessary because of the retrospective study design, implying minimal risk and no patient intervention.
The observation window for a COVID-19 case refers to the period from the moment the diagnosis of COVID-19 was confirmed (index date) until the end of follow-up. This period lasted for 45 days after the index date for outpatients or hospitalization.
The COVID-19 cases were categorized by severity according to the World Health Organization (WHO) guidelines and its healthcare resource utilization [19]. Mild cases were managed through outpatient care or by telemedicine or phone consultations. Moderate cases were treated on an outpatient basis or at home with oxygen therapy. Severe cases required hospitalization, and critical cases involved treatment in the intensive care unit.
We defined the high-risk age group as individuals over 60 or 65 years of age, primarily due to the complications generated by a COVID-19 infection [20,21]. The risk factors for severe COVID-19 were herein identified in accordance with the guidelines provided by the Centers for Disease Control and Prevention (CDC) [21]. In addition to the aforementioned age factor, the risk factors included a history of cancer, chronic kidney disease (CKD), chronic lung disease, dementia or other neurological condition, type 1 or type 2 diabetes, Down syndrome, cardiovascular disease, Human Immunodeficiency Virus (HIV) infection or Acquired Immunodeficiency Syndrome (AIDS), hypertension, an immune deficiency or immunocompromised condition, liver disease, obesity, sickle-cell disease, thalassemia, current or past smoking, and a solid organ or blood transplant [21]. Reinfection was considered if a COVID infection took place 45 days or more after the previous infection [22,23,24].
Vaccination status is classified as follows:
- unvaccinated: without any COVID-19 vaccination record
- partially vaccinated: a single dose of the messenger ribonucleic acid (mRNA) or adenoviral vector vaccines
- fully vaccinated: two doses of the mRNA or adenoviral vector vaccines, or a single dose of the Johnson & Johnson vaccine
- fully vaccinated + booster: fully vaccinated and some additional COVID-19 vaccine dose
Finally, patient death is considered to be related to COVID-19 if it occurred within the previously defined timeframe for the disease.
2.2. Statistical Analysis
Descriptive statistics were generated to analyze demographic and clinical variables. We used percentages and frequencies to describe dichotomic, ordinal, and nominal variables, while mean and standard deviation (SD) were calculated for quantitative variables.
To comprehend the evolution of the burden of COVID-19 during different timeframes, indicators such as the monthly and annual cumulative frequency, the crude mortality rate, and the case fatality rate were calculated from the frequency of occurrence of events. The incidence rate was calculated as (new cases/population) × 100,000. The mortality rate was ascertained using a similar approach.
To explore the changes in the burden of disease associated with the introduction of vaccination strategies at the national level, a subgroup analysis was performed using the first infection cases. The test of equal or given proportions was employed to assess statistically relevant changes within groups.
Two multivariate logistic regression models were used. In one, the dependent variable was a severe or critical COVID-19 case, and in the other, a deceased patient. Associations were assessed based on patient characteristics. A statistical analysis was performed using R statistical language (v. 4.3.1) [25], with significance set at 5%.
3. Results
3.1. Demographic and Clinical Characteristics
A total of 953,661 adult cases qualified for inclusion in the study, corresponding to 894,326 patients. The mean age was 42.3 years (±15), with 18–49-year-olds comprising most cases (71.2%, n = 678,559), followed by 50–64-year-olds (20.6%), and then the elderly (65 years of age or older; 8.3%). Around 56% of the sample was female, 57.1% lived in Antioquia, almost all lived in urban areas (99.4%), and of the cases that reported data, the most reported being of mixed race (24.4%) (Table 1). The majority (61.7%) reported earnings under two times the minimum wage (In 2022, this corresponded to subjects with a monthly income below 470 United States Dollars (USD)).

Table 1.
Demographic and clinical characteristics of COVID-19 positive cases in a large HMO (from March 2020 to January 2023).
The mean weight was 68.5 kg (±22.2) and the average height was 151.1 cm (±45.5). Only 0.5% of the cases involved pregnancy. Most of the sample had a mild or moderate condition (79%) handled in outpatient care, while 20.1% of the cases were severe, and 0.9% critical. Reinfected cases constituted 6.2% of the sample. The average number of comorbidities was 1.0 (±1.4), and the most frequent comorbidities were an immunocompromised condition (23.8%, n = 226,623), hypertension (19.1%), a mental health condition (15%), cancer (11.2%), and obesity (10.8%). Medication was taken chronically by 45.5% of the patients. A risk factor for severe COVID-19 was found in about 9.1% of all COVID-19 cases (Table 1).
Most cases (94.6%, n = 901,966) were unvaccinated, and only a small proportion (3.4%, n = 32,823) were fully vaccinated. Vaccinated cases (partial, full, or full plus booster) had a higher average age and number of comorbidities and tended to be concentrated among females. It was more common for subjects from higher-income households to be vaccinated, and for vaccinated patients to have milder conditions than those unvaccinated (Table 1).
3.2. Frequency of Cases by Year and Age Group
COVID-19 cases were more frequent in 2021 (54.9%), followed by 26.8% in 2020. Among the different variants over time in Colombia [26,27], the Mu variant dominance period was associated with the highest percentage of cases (21%) (Figure 1).
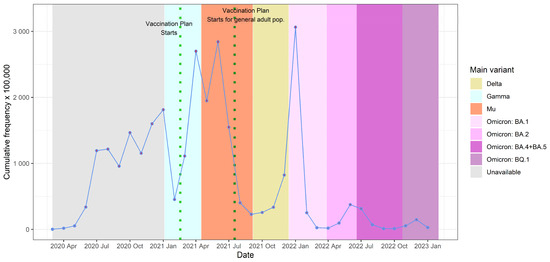
Figure 1.
Monthly cumulative frequency of confirmed cases and variant predominance in Colombia, March 2020 to January 2023. Note 1: Variant predominance was based on data from the National Health Institute (INS, by its acronym in Spanish) [26] and Holdcroft et al. [27]. Note 2: The vaccination plan began on 17 February 2021, with prioritized populations such as healthcare workers; later, on July 17 of the same year, it was extended to all adults.
The monthly cumulative frequency of COVID-19 cases reveals a multimodal behavior with several peaks. The Colombian vaccination plan started [8] on 17 February 2021, and was extended to all adults on 17 July 2021. The peaks were successively higher as time passed until reaching the greatest number of cases in January 2022, after which time the number of cases per month diminished. The first peak (in April 2021, the predominance of the Gamma variant) was constituted by 2698.7 cases per 100,000 members of the HMO (confidence interval [CI] 95%; 2681.4–2716.1). The second peak (in June 2021, predominance of the Mu variant) consisted of 2841.5 cases per 100,000 members (CI 95%; 2823.8–2859.2). The third peak (in January 2022, the predominance of the Omicron BA.1 variant) comprised 3063.2 cases per 100,000 members (CI 95%; 3045.4–3081.0). This general pattern is similar to that found in other reports, which also describe the highest peak in January 2022 [28,29].
The annual pattern of cases from 2020–2022 displays an inverted U-shape, with 7640 cases per 100,000 members of the HMO (CI 95%; 7610–7671) in 2020, rising to 13,559 (CI 95%; 13,520–13,598) in 2021, and falling to 4237 (CI 95%; 4217–4257) in 2022. The greatest risk of developing COVID-19 corresponded to middle-aged adults (18–49 years of age) (Figure 2A). The presence of comorbidities led to a 1.25- to 7.78-fold increase in the risk of infection. For example, patients with an immunocompromised condition showed an annual frequency of 59,421 cases per 100,000 members in 2020 (CI 95%; 58,835–60,011), 60,557 in 2021 (CI 95%; 60,119–60,998), and 19,214 in 2022 (CI 95%; 19,023–19,405), which indicates a 7.78-, 4.47-, and 4.53-fold greater risk of infection, respectively, compared to the overall sample (Figure 2B).
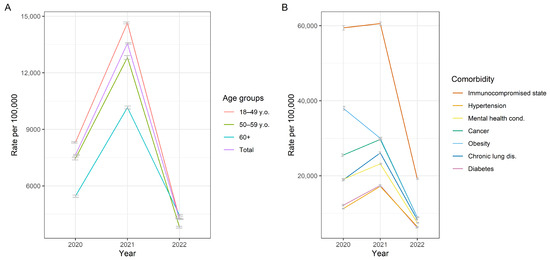
Figure 2.
Annual frequency of COVID-19 cases from 2020 to 2022 by age groups (A) and main comorbidities (B).
3.3. Severity and Vaccination Status
A lower proportion of critical and severe cases was observed for the vaccinated versus unvaccinated patients. Critical cases constituted 0.9% of the total number of unvaccinated subjects in the sample (8846/901,966) and 0.5% of those fully vaccinated (151/32,823). This pattern is even more prominent for severe cases, which made up 20.4% of the total number of unvaccinated subjects (184,014/901,966) and 9.5% of those fully vaccinated (3116/32,823). Hence, the proportion of mild cases was slightly higher among the vaccinated than unvaccinated patients, being 88.1% (28,907/32,823) for the former and 78.0% (703,237/901,966) for the latter (Appendix A).
With a greater age, the risk of the severity of the disease increased. Indeed, the mean age for the mild cases was 40.2 (±13.8) years, and for the critical cases, it was 58.8 (±14.6) years (Appendix A). Additionally, individuals with certain comorbidities represented a larger proportion of total critical cases than their proportion of total mild cases. For example, individuals with an immunocompromised condition were responsible for 21.5% of mild cases and 28.5% of critical cases. Moreover, individuals with hypertension accounted for 13.9% of mild cases and 49.0% of critical cases, and individuals with mental health conditions were responsible for 13.9% of mild cases and 17.8% of critical cases (Figure 3).
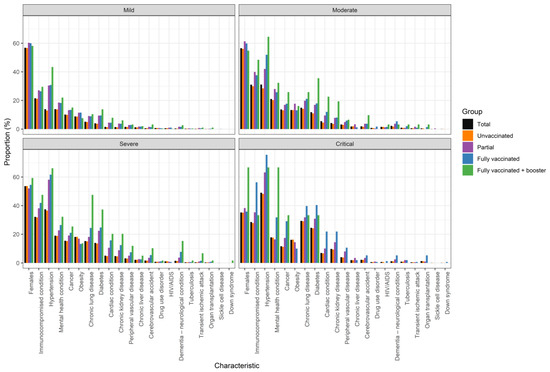
Figure 3.
COVID-19 severity in relation to vaccination status, gender, and the presence of comorbidities.
These patterns are exacerbated by variations in vaccination status. For instance, the mean age for mild cases was 39.6 ± 13.3 years for unvaccinated patients and 58.3 ± 14.4 years for fully vaccinated patients. Meanwhile, for critical cases, it was 50.1 ± 16.7 years for unvaccinated patients and 73.9 ± 12.3 years for fully vaccinated patients (Appendix A).
The logistic regression model confirmed that a greater age and/or weight, male sex, a higher number of comorbidities, and especially reinfection (compared to first infections, ceteris paribus, reinfection cases had a 2.9-fold greater risk of being severe or critical COVID-19) have a positive and statistically significant association with the probability (odds ratio, OR) of developing severe or critical COVID-19. Conversely, full vaccination status and a higher income tend to decrease the same probability (OR) (Table 2).

Table 2.
Logistic regression model results using a severe or critical condition as the dependent variable (Model 1) and using death as the dependent variable (Model 2).
On the other hand, there was a difference in the proportion of severe and critical cases before and after the start of the vaccination plan for all adults (17 July 2021). Severe cases constituted 24.6% of the total cases before vaccination began and 8.3% of the total cases afterwards. Critical cases represented 1.1% (7762/685,840) before vaccination began and 0.4% (1079/267,821) afterwards. Both differences were statistically significant according to the test of equal or given proportions. The opposite tendency can be appreciated when comparing the proportion of these cases between 2022 (Appendix B provides annual figures for 2022 on the distribution of death cases by care setting and age, among other characteristics) and 2023 (taking into account that in the latter year, the data is only available for January). In 2022, the severe cases were at 6.6% of the total cases (11,396/173,770), and at 11.0% (127/1156) in January 2023. Similarly, in 2022, the critical cases were at 0.3% (455/173,770), and at 0.8% (9/1156) in January 2023. Both differences were statistically significant.
3.4. Trends by Risk Factor
Considering the first-infection cases, 894,876 were analyzed. Individuals 65 years of age or older constituted 8.2% (n = 55,287) of all cases before the vaccination plan began, and 12.6% (n = 28,179) afterwards. They had a lower proportion of cases with comorbidity subsequent to (versus prior to) the implementation of the plan (83.6% vs. 84.8%). This same pattern held for certain comorbidities such as hypertension (67.8% vs. 68.5%), obesity (8.2% vs. 9.5%), chronic lung disease (21.1% vs. 23.1%), and diabetes (25.6% vs. 28.3%). For other comorbidities, however, the reverse pattern occurred, with a higher proportion found after the vaccination plan began. Examples include a mental health condition (24.5% vs. 21.9%), cancer (19.6% vs. 18.7%), and dementia (7.6% vs. 5.2%). No significant differences were detected in this regard for some comorbidities, such as chronic kidney disease, chronic liver disease, an immunocompromised condition, HIV, tuberculosis, and sickle cell disease (Table 3).

Table 3.
Proportion of cases for each comorbidity prior to and subsequent to the implementation of the vaccination plan for all adults, categorized by age group.
3.5. Mortality and Case Fatality Rate
Analogous to the trend observed with case frequency, the annual pattern of the crude mortality rate showed an inverted U-shape. It was 70.6 per 100,000 members of the HMO (CI 95%; 67.81–73.43) in 2020, 160.2 (CI 95%; 156.19–164.22) in 2021, and 22.5 (CI 95%; 21.07–23.97) in 2022. Likewise, the annual case fatality rate was 0.92% (CI 95%; 0.89–0.96%) in 2020, 1.18% (CI 95%; 1.15–1.21%) in 2021, and 0.53% (CI 95%; 0.50–0.57%) in 2022 (Figure 4).
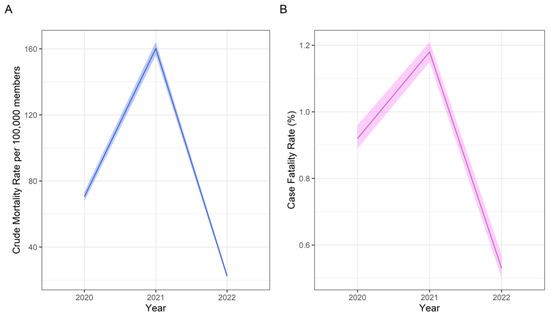
Figure 4.
Annual crude mortality rate (A) and case fatality rate (B).
On the other hand, logistic regression revealed the association of an increased probability of death (measured by the odds ratio, OR) with greater age or weight, a higher number of comorbidities, and a more severe condition (compared to mild cases, critical cases have a higher probability (measured by OR) of death). Moreover, there were more deaths among males than females, and proportionally more (versus total cases) in January 2023 compared to the annual figures for 2022 (2023 = 53.6% males vs. 2022 = 52.7% males).
Contrarily, some clinical characteristics have an inverse relationship, decreasing the risk of death, such as a full vaccination status, a higher income, and reinfection (Table 2).
4. Discussion
The present study evaluated the burden of COVID-19 cases of adults in a large HMO in Colombia between March 2020 and January 2023. Almost 1 million cases were found during this timeframe, most of them were mild or moderate (handled as outpatients), with a low household income, and around 42 years old. The burden of severe and critical cases tended to be borne by males, aged 49 years and older, unvaccinated, and with comorbidities.
The monthly burden of disease reached its third and highest peak in January 2022, with over 2600 cases per 100,000 members of the HMO. During the last 11 months of observation, the incidence did not exceed 400 cases per 100,000 members. The frequency and mortality rate varied substantially in accordance with the different waves of COVID variants.
The current analysis provides insights into the clinical and demographic characteristics of COVID-19 cases during the first 35 months since its appearance in Colombia. Over 90% of the sample comprised urban residents and unvaccinated individuals. There were slightly more cases of females than males, except in relation to critical cases. The group of 18–49-year-olds constituted the majority of cases, but the elderly had a greater risk of a severe or critical condition. Moreover, the existence of comorbidity increased the risk of severe or critical COVID-19. The general findings about the demographical and clinical characteristics are consistent with publications in the literature, particularly with those who reported greater severity of COVID-19 associated with obesity and being male and/or elderly [4,30,31,32].
Due to the priorities of the Colombian vaccination plan, most vaccinated cases were older adults. Thus, a higher number of comorbidities was found among vaccinated than unvaccinated patients. The plan was divided into stages, with priority given as follows: (i) the population over 80 years of age and healthcare workers; (ii) police, military, and the population from 60 to 79 years old; (iii) educational workers and teachers, caregivers, and the population of 16–59 years of age with a risk factor (e.g., hypertension, diabetes, kidney failure, HIV, cancer, tuberculosis, asthma, and obesity); (iv) the incarcerated population, homeless people, and high-risk professions; and finally, (v) the population 16 years old and over and groups not mentioned in the previous stages, starting with the population from 50 to 59 years of age [8].
Similar to observations reported in other cities and regions, the results suggest that the Colombian vaccination plan is related to a decrease in the absolute frequency of cases across all groups and a reduction in the severity of the cases [14,33] However, certain groups at risk did not receive special protective measures, particularly in the group with mental and neurological disorders, such as dementia or a mental health condition. On the other hand, some authors argue that immunocompromised cases are not all at high risk of COVID-19, but rather that there are subgroups within this group that differ in their prognosis and risk [34].
Despite the national vaccination plan not prioritizing income or socioeconomic status, and most cases in the study sample belonging to households with an income under two times the minimum wage, vaccinated cases tended to be concentrated in higher-income households, and it can be argued that this behavior represents social inequality. According to the data, a full vaccination reduces the probability of death and a severe or critical condition. Also, promoting a protective influence against death from COVID-19 was reinfection, although a greater probability existed of developing a severe or critical condition. A worrisome result is the increase in the proportion of severe and critical cases and of the OR of death in January of 2023 compared to the annual data in 2022 and 2020, respectively.
At the time of writing this manuscript, virtually no published studies collecting data beyond 2023 have been found in Latin America, leaving as the main reference dashboards with highly aggregated information, which for Colombia indicated a recent peak in August 2024 that did not exceed 4000 cases [35]. In this context, as Ulrichs et al. [36] mentioned, some variations of the COVID-19 epidemiology and burden are expected to occur, those being an increase in immunized cases, a decrease in disease severity, a reduction in detection, and further co-occurrence with other respiratory diseases. This follow-up is required in future studies.
In view of the above findings, the competent authorities and the health sector in general must not let down their guard in at least four aspects. Firstly, it is understandable that disease prevention messages have diminished compared to the period of the health emergency [37], but disease awareness must continue to be present. Secondly, detection and reporting of confirmed cases of COVID-19 should not be neglected. The broad screening guidelines implemented during the emergency have been relaxed, as shown by the daily test per million of 1938 in June 2021 and 357 in June 2022 [38,39,40]. Thirdly, COVID-19 vaccination coverage should be sustained and expanded, considering the problematic behavior of the cases in January 2023. Fourthly, vaccination and prevention campaigns need to be accompanied by strategies to address the spread of misinformation to facilitate evidence-based policy decisions [41], such as partnerships with fact-checking organizations. Azevedo et al. [42] argued that in Brazil, these agencies played an important role in shaping public trust and behavior.
The current contribution in Colombia used a large integrated clinical records database for a diverse sample involving many different healthcare providers and settings, providing a comprehensive landscape of the burden of the disease. Unlike most studies that focus on a specific setting, age group, or limited timeframe, this research provides a broader perspective. Moreover, the study had the ability to split the analyses by different subgroups and time spans, allowing an in-depth characterization of the demographic and clinical characteristics of COVID-19 cases in the country. Nevertheless, some limitations exist, such as the incompleteness of the data on the race variable (missing in over 60% of the cases). This variable has often been key to explaining disparities in COVID-19 outcomes [43,44]. Studies in Latin-American countries have indicated that mixed and black race persons tend to have increased mortality risks [45]. On a similar note, over 60% of cases concentrated in Antioquia and Bogotá are characterized by their location in the Andean mountains, high population density, and leading economic development in the country. This may reduce the comparability of the results to other regions of the country. Moreover, there may have been under-reporting or misclassification of comorbidities. Furthermore, in-depth clinical information was not provided (e.g., symptoms, laboratory test results, and the variant per case), nor was information on some relevant outpatient behavior, such as the use of over-the-counter drugs. Finally, data was not collected on asymptomatic cases. The present study can only demonstrate associations and not causality between variables, and its results cannot be generalized to the entire Colombian population.
In conclusion, COVID-19 cases in Colombia showed peaks in April and June of 2021 and January 2022, each successively higher, followed by a decline in the number of cases. Severe and critical cases were associated with a lack of vaccination, and/or weight, reinfection, and comorbidities (especially hypertension, an immunocompromised condition, a mental health condition, obesity, and cancer). Effective vaccination strategies are needed to reduce the burden of COVID-19 in Colombia, and, considering budgetary constraints, it is advisable to prioritize the elderly or populations with underlying conditions.
Author Contributions
Conceptualization, J.A., J.M.R., J.B.-L., C.F.M., J.R.S., J.Y., F.M., A.C.H.-D., O.E., A.R., L.E.P.J., J.L.R. and M.H.K.; Data curation, J.B.-L., F.J.G., C.J.B., A.C.H.-D. and L.E.P.J.; Formal analysis, J.A. and J.B.-L.; Investigation, J.A., J.M.R., J.B.-L., C.F.M., J.R.S., J.Y., F.M., A.C.H.-D., O.E., M.G., L.E.P.J., J.L.R. and M.H.K.; Methodology, J.A., J.M.R., J.B.-L., C.F.M., J.R.S., J.Y., F.M., O.E., A.R., L.E.P.J., J.L.R. and M.H.K.; Project administration, J.M.R.; Supervision, J.M.R., J.B.-L. and L.E.P.J.; Validation, J.A.; Visualization, J.A.; Writing—original draft, J.A. and M.G.; Writing—review and editing, J.A., J.M.R., J.B.-L., C.F.M., J.R.S., J.Y., F.M., F.J.G., C.J.B., A.C.H.-D., O.E., A.R., M.G., L.E.P.J., J.L.R. and M.H.K. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by PFIZER, and a grant number is not applicable.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the HMO SURA (Comité de ética y BPC en investigación en salud, CEI-SURA; protocol code C4591060) by Act No. 101 dated 19 July 2023.
Informed Consent Statement
Informed consent was unnecessary because of the retrospective study design, implying minimal risk and no patient intervention.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
J Bolaños-López, FJ Gonzalez, C Bello, AC Herrera, LE Perez are paid employees of Biociencias-Sura. J Arciniegas, JM Reyes, C Mendoza, J Spinardi, J Yang, O Escobar, M Garcia, J LaRotta and MH Kyaw are paid employees of Pfizer. F Maleki and AC Rubio, were paid employees of Pfizer at the time of the study’s design and development. The funder had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Appendix A. COVID-19 Severity in Relation to Vaccination Status, Age, Gender, and the Presence of Comorbidities
| Total | Unvaccinated | Partial | Fully Vaccinated | Fully + Booster | |||
| Mild, n (%) | 746,408 (100) | 703,237 (94.2) | 13,458 (1.8) | 28,907 (3.9) | 806 (0.1) | ||
| Age, mean (SD) | 40.2 (±13.8) | 39.6 (±13.3) | 50.1 (±17.8) | 50.1 (±16.7) | 60.4 (±17.1) | ||
| Female, n (%) | 424,148 (56.8) | 398,218 (56.6) | 8121 (60.3) | 17,341 (60) | 468 (58.1) | ||
| Comorbidities, n (%) | Immunocompromised condition | 160,426 (21.5) | 148,899 (21.2) | 3652 (27.1) | 7637 (26.4) | 238 (29.5) | |
| Hypertension | 103,813 (13.9) | 90,457 (12.9) | 4096 (30.4) | 8910 (30.8) | 350 (43.4) | ||
| Mental health condition | 103,943 (13.9) | 96,010 (13.7) | 2488 (18.5) | 5268 (18.2) | 177 (22) | ||
| Cancer | 75,321 (10.1) | 69,552 (9.9) | 1773 (13.2) | 3875 (13.4) | 121 (15) | ||
| Obesity | 65,886 (8.8) | 60,980 (8.7) | 1532 (11.4) | 3313 (11.5) | 61 (7.6) | ||
| Chronic lung disease | 38,191 (5.1) | 34,325 (4.9) | 1222 (9.1) | 2560 (8.9) | 84 (10.4) | ||
| Diabetes | 30,074 (4) | 25,947 (3.7) | 1268 (9.4) | 2748 (9.5) | 111 (13.8) | ||
| Cardiac condition | 11,063 (1.5) | 9113 (1.3) | 602 (4.5) | 1284 (4.4) | 64 (7.9) | ||
| Chronic kidney disease | 10,306 (1.4) | 8683 (1.2) | 508 (3.8) | 1066 (3.7) | 49 (6.1) | ||
| Peripheral vascular disease | 11,020 (1.5) | 9800 (1.4) | 373 (2.8) | 821 (2.8) | 26 (3.2) | ||
| Chronic liver disease | 8599 (1.2) | 7862 (1.1) | 230 (1.7) | 491 (1.7) | 16 (2) | ||
| Cerebrovascular accident | 4492 (0.6) | 3871 (0.6) | 198 (1.5) | 397 (1.4) | 26 (3.2) | ||
| Drug use disorder | 5333 (0.7) | 5067 (0.7) | 99 (0.7) | 164 (0.6) | 3 (0.4) | ||
| HIV/AIDS | 4353 (0.6) | 3944 (0.6) | 121 (0.9) | 286 (1) | 2 (0.2) | ||
| Dementia—neurological condition | 3121 (0.4) | 2452 (0.3) | 211 (1.6) | 436 (1.5) | 22 (2.7) | ||
| Tuberculosis | 2100 (0.3) | 1948 (0.3) | 63 (0.5) | 86 (0.3) | 3 (0.4) | ||
| Transient ischemic attack | 1647 (0.2) | 1412 (0.2) | 88 (0.7) | 139 (0.5) | 8 (1) | ||
| Organ transplantation | 980 (0.1) | 845 (0.1) | 31 (0.2) | 96 (0.3) | 8 (1) | ||
| Sickle cell disease | 345 (0) | 325 (0) | 5 (0) | 15 (0.1) | - | ||
| Down syndrome | 85 (0) | 75 (0) | 3 (0) | 7 (0) | - | ||
| Moderate, n (%) | 7152 (100) | 6229 (87.1) | 243 (3.4) | 649 (9.1) | 31 (0.4) | ||
| Age, mean (SD) | 47.7 (17.6) | 46.2 (16.9) | 55. (20.2) | 57.7 (19.3) | 62.9 (18.7) | ||
| Female, n (%) | 4044 (56.5) | 3490 (56) | 149 (61.3) | 388 (59.8) | 17 (54.8) | ||
| Comorbidities, n (%) | Immunocompromised condition | 2220 (31) | 1864 (29.9) | 97 (39.9) | 244 (37.6) | 15 (48.4) | |
| Hypertension | 2226 (31.1) | 1767 (28.4) | 102 (42) | 337 (51.9) | 20 (64.5) | ||
| Mental health condition | 1504 (21) | 1259 (20.2) | 68 (28) | 167 (25.7) | 10 (32.3) | ||
| Cancer | 979 (13.7) | 815 (13.1) | 41 (16.9) | 115 (17.7) | 8 (25.8) | ||
| Obesity | 953 (13.3) | 820 (13.2) | 43 (17.7) | 85 (13.1) | 5 (16.1) | ||
| Chronic lung disease | 1069 (14.9) | 876 (14.1) | 48 (19.8) | 137 (21.1) | 8 (25.8) | ||
| Diabetes | 844 (11.8) | 676 (10.9) | 41 (16.9) | 116 (17.9) | 11 (35.5) | ||
| Cardiac condition | 390 (5.5) | 282 (4.5) | 23 (9.5) | 78 (12) | 7 (22.6) | ||
| Chronic kidney disease | 302 (4.2) | 225 (3.6) | 19 (7.8) | 52 (8) | 6 (19.4) | ||
| Peripheral vascular disease | 230 (3.2) | 178 (2.9) | 12 (4.9) | 38 (5.9) | 2 (6.5) | ||
| Chronic liver disease | 132 (1.8) | 116 (1.9) | 8 (3.3) | 8 (1.2) | - | ||
| Cerebrovascular accident | 137 (1.9) | 101 (1.6) | 9 (3.7) | 24 (3.7) | 3 (9.7) | ||
| Drug use disorder | 58 (0.8) | 46 (0.7) | 1 (0.4) | 11 (1.7) | - | ||
| HIV/AIDS | 106 (1.5) | 92 (1.5) | 3 (1.2) | 10 (1.5) | 1 (3.2) | ||
| Dementia—neurological condition | 154 (2.2) | 109 (1.7) | 9 (3.7) | 35 (5.4) | 1 (3.2) | ||
| Tuberculosis | 63 (0.9) | 47 (0.8) | 2 (0.8) | 13 (2) | 1 (3.2) | ||
| Transient ischemic attack | 43 (0.6) | 32 (0.5) | 4 (1.6) | 6 (0.9) | 1 (3.2) | ||
| Organ transplantation | 34 (0.5) | 24 (0.4) | - | 9 (1.4) | 1 (3.2) | ||
| Sickle cell disease | 4 (0.1) | 3 (0) | 1 (0.4) | - | - | ||
| Down syndrome | 4 (0.1) | 4 (0.1) | - | - | - | ||
| Severe, n (%) | 191,260 (100) | 184,014 (96.2) | 4071 (2.1) | 3116 (1.6) | 59 (0) | ||
| Age, mean (SD) | 49.6 (16.4) | 49.0 (16.2) | 62.2 (15.2) | 66.1 (17.9) | 72.3 (18) | ||
| Female, n (%) | 102,594 (53.6) | 98,744 (53.7) | 2116 (52) | 1699 (54.5) | 35 (59.3) | ||
| Comorbidities, n (%) | Immunocompromised condition | 61,460 (32.1) | 58,577 (31.8) | 1550 (38.1) | 1305 (41.9) | 28 (47.5) | |
| Hypertension | 71,514 (37.4) | 67,190 (36.5) | 2367 (58.1) | 1918 (61.6) | 39 (66.1) | ||
| Mental health conditions | 36,318 (19) | 34,553 (18.8) | 924 (22.7) | 822 (26.4) | 19 (32.2) | ||
| Cancer | 29,403 (15.4) | 27,958 (15.2) | 776 (19.1) | 654 (21) | 15 (25.4) | ||
| Obesity | 34,683 (18.1) | 33,577 (18.2) | 688 (16.9) | 410 (13.2) | 8 (13.6) | ||
| Chronic lung disease | 29,106 (15.2) | 27,581 (15) | 738 (18.1) | 759 (24.4) | 28 (47.5) | ||
| Diabetes | 26,622 (13.9) | 24,921 (13.5) | 910 (22.4) | 769 (24.7) | 22 (37.3) | ||
| Cardiac condition | 9717 (5.1) | 8790 (4.8) | 426 (10.5) | 489 (15.7) | 12 (20.3) | ||
| Chronic kidney disease | 9250 (4.8) | 8492 (4.6) | 360 (8.8) | 386 (12.4) | 12 (20.3) | ||
| Peripheral vascular disease | 6134 (3.2) | 5686 (3.1) | 207 (5.1) | 234 (7.5) | 7 (11.9) | ||
| Chronic liver disease | 4282 (2.2) | 4092 (2.2) | 108 (2.7) | 79 (2.5) | 3 (5.1) | ||
| Cerebrovascular accident | 3341 (1.7) | 3016 (1.6) | 147 (3.6) | 172 (5.5) | 6 (10.2) | ||
| Drug use disorder | 1519 (0.8) | 1450 (0.8) | 35 (0.9) | 33 (1.1) | 1 (1.7) | ||
| HIV/AIDS | 2199 (1.1) | 2139 (1.2) | 37 (0.9) | 23 (0.7) | - | ||
| Dementia—neurological condition | 2871 (1.5) | 2467 (1.3) | 151 (3.7) | 244 (7.8) | 9 (15.3) | ||
| Tuberculosis | 900 (0.5) | 854 (0.5) | 25 (0.6) | 20 (0.6) | 1 (1.7) | ||
| Transient ischemic attack | 1014 (0.5) | 922 (0.5) | 41 (1) | 47 (1.5) | 4 (6.8) | ||
| Organ transplantation | 786 (0.4) | 740 (0.4) | 19 (0.5) | 26 (0.8) | 1 (1.7) | ||
| Sickle cell disease | 95 (0) | 90 (0) | 4 (0.1) | 1 (0) | - | ||
| Down syndrome | 35 (0) | 33 (0) | 1 (0) | - | 1 (1.7) | ||
| Critical, n (%) | 8841 (100) | 8486 (96) | 201 (2.3) | 151 (1.7) | 3 (0) | ||
| Age, mean (SD) | 58.8 (14.6) | 58.3 (14.4) | 67.7 (13.1) | 73.9 (12.3) | 77.3 (6.4) | ||
| Female, n (%) | 3109 (35.2) | 2976 (35.1) | 77 (38.3) | 54 (35.8) | 2 (66.7) | ||
| Comorbidities, n (%) | Immunocompromised condition | 2517 (28.5) | 2360 (27.8) | 71 (35.3) | 85 (56.3) | 1 (33.3) | |
| Hypertension | 4330 (49) | 4087 (48.2) | 127 (63.2) | 114 (75.5) | 2 (66.7) | ||
| Mental health condition | 1576 (17.8) | 1493 (17.6) | 33 (16.4) | 48 (31.8) | 2 (66.7) | ||
| Cancer | 1027 (11.6) | 947 (11.2) | 35 (17.4) | 44 (29.1) | 1 (33.3) | ||
| Obesity | 1419 (16.1) | 1375 (16.2) | 29 (14.4) | 15 (9.9) | (0) | ||
| Chronic lung disease | 2593 (29.3) | 2468 (29.1) | 64 (31.8) | 60 (39.7) | 1 (33.3) | ||
| Diabetes | 2167 (24.5) | 2043 (24.1) | 62 (30.8) | 61 (40.4) | 1 (33.3) | ||
| Cardiac condition | 622 (7) | 569 (6.7) | 20 (10) | 33 (21.9) | - | ||
| Chronic kidney disease | 855 (9.7) | 793 (9.3) | 29 (14.4) | 33 (21.9) | - | ||
| Peripheral vascular disease | 357 (4) | 325 (3.8) | 16 (8) | 16 (10.6) | - | ||
| Chronic liver disease | 175 (2) | 165 (1.9) | 7 (3.5) | 3 (2) | - | ||
| Cerebrovascular accident | 196 (2.2) | 181 (2.1) | 7 (3.5) | 8 (5.3) | - | ||
| Drug use disorder | 54 (0.6) | 51 (0.6) | 2 (1) | 1 (0.7) | - | ||
| HIV/AIDS | 62 (0.7) | 60 (0.7) | - | 2 (1.3) | - | ||
| Dementia—neurological condition | 103 (1.2) | 90 (1.1) | 5 (2.5) | 8 (5.3) | - | ||
| Tuberculosis | 80 (0.9) | 73 (0.9) | 4 (2) | 3 (2) | - | ||
| Transient ischemic attack | 41 (0.5) | 39 (0.5) | 1 (0.5) | 1 (0.7) | - | ||
| Organ transplantation | 113 (1.3) | 103 (1.2) | 2 (1) | 8 (5.3) | - | ||
| Sickle cell disease | 7 (0.1) | 7 (0.1) | - | - | - | ||
| Down syndrome | 8 (0.1) | 7 (0.1) | - | 1 (0.7) | - |
Appendix B. Additional Data Focused on 2022
| Proportion of high risk comorbidities | |
| Age group “18–29” | 30.1% |
| Age group “30–49” | 39.4% |
| Age group “50–64” | 60.2% |
| Age group “65–74” | 78.3% |
| Age group “75+” | 90.8% |
| Probability infection being symptomatic (%) in 2022 | |
| Age group “18–29” | 3.1% |
| Age group “30–49” | 4.9% |
| Age group “50–64” | 3.9% |
| Age group “65–74” | 4.3% |
| Age group “75+” | 6.0% |
| Hospitalization rate among symptomatic patients (%) in 2022 | |
| Age group “18–29” | 0.3% |
| Age group “30–49” | 0.6% |
| Age group “50–64” | 1.6% |
| Age group “65–74” | 3.5% |
| Age group “75+” | 1.0% |
| Risk for hospitalization of with comorbidities patient group | 2.6% |
| Risk for hospitalization of NON comorbidities patient group | 0.5% |
| Critical care/ICU admission rate among hospitalized patients (%) in 2022 | |
| Age group “18–29” | 12.1% |
| Age group “30–49” | 13.7% |
| Age group “50–64” | 21.8% |
| Age group “65–74” | 25.1% |
| Age group “75+” | 15.1% |
| Risk for ICU of with comorbidities patient group | 0.4% |
| Risk for ICU of with NON comorbidities patient group | 0.1% |
| Probability of death among patients on normal ward (%) in 2022 | |
| Age group “18–29” | 1.2% |
| Age group “30–49” | 1.1% |
| Age group “50–64” | 5.7% |
| Age group “65–74” | 12.0% |
| Age group “75+” | 22.4% |
| Risk for death in GW of with comorbidities patient group | 10.4% |
| Risk for death in GW of NON comorbidities patient group | 4.6% |
| Probability of death among patients on critical care (%) in 2022 | |
| Age group “18–29” | 9.1% |
| Age group “30–49” | 14.7% |
| Age group “50–64” | 25.4% |
| Age group “65–74” | 55.2% |
| Age group “75+” | 52.1% |
| Risk for death in ICU of with comorbidities patient group | 35.3% |
| Risk for death in ICU of NON comorbidities patient group | 41.0% |
| Probability of death among patients on outpatient care (%) in 2022 | |
| Age group “18–29” | 0.0% |
| Age group “30–49” | 0.0% |
| Age group “50–64” | 0.2% |
| Age group “65–74” | 0.7% |
| Age group “75+” | 3.7% |
| Risk for death outpatient of with comorbidities patient group | 0.5% |
| Risk for death outpatient of NON comorbidities patient group | 0.0% |
References
- Decerf, B.; Friedman, J.; Mendes, A.; Pennings, S.; Yonzan, N. Lives, Livelihoods, and Learning: A Global Perspective on the Well-Being Impacts of the COVID-19 Pandemic; World Bank: Washington, DC, USA, 2024. [Google Scholar]
- Espinola, N.; Loudet, C.I.; Luxardo, R.; Moreno, C.; Kyaw, M.H.; Spinardi, J.; Mendoza, C.F.; Carballo, C.M.; Dantas, A.C.; Abalos, M.G.; et al. COVID-19 Disease and Economic Burden to Healthcare Systems in Adults in Six Latin American Countries Before Nationwide Vaccination Program: Ministry of Health Database Assessment and Literature Review. Int. J. Environ. Res. Public Health 2025, 22, 669. [Google Scholar] [CrossRef]
- Umakanthan, S.; Sahu, P.; Ranade, A.V.; Bukelo, M.M.; Rao, J.S.; Abrahao-Machado, L.F.; Dahal, S.; Kumar, H.; Kv, D. Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19). Postgrad. Med. J. 2020, 96, 753–758. [Google Scholar] [CrossRef]
- Brodin, P. Immune determinants of COVID-19 disease presentation and severity. Nat. Med. 2021, 27, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Salzberger, B.; Buder, F.; Lampl, B.; Ehrenstein, B.; Hitzenbichler, F.; Holzmann, T.; Schmidt, B.; Hanses, F. Epidemiology of SARS-CoV-2. Infection 2021, 49, 233–239. [Google Scholar] [CrossRef]
- Kim, L.; Garg, S.; O’Halloran, A.; Whitaker, M.; Pham, H.; Anderson, E.J.; Armistead, I.; Bennett, N.M.; Billing, L.; Como-Sabetti, K.; et al. Risk Factors for Intensive Care Unit Admission and In-hospital Mortality Among Hospitalized Adults Identified through the US Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET). Clin. Infect. Dis. 2021, 72, e206–e214. [Google Scholar] [CrossRef]
- MSPS CORONAVIRUS (COVID-19) 2023. Available online: https://www.minsalud.gov.co/salud/publica/PET/Paginas/Covid.aspx (accessed on 2 April 2024).
- MSPS; DNP; MHCP; IETS. Plan Nacional de Vacunación Contra el COVID-19; Ministerio de Salud y Protección Social: Bogotá, Colombia, 2021. [Google Scholar]
- MSPS. Resolución 2367 de 2023; MSPS: Bogotá, Colombia, 2023. [Google Scholar]
- Ramos Valencia, O.A.; Buitrón Gonzalez, Y.; Sotelo Daza, J.S.; Villaquiran, A.F. Factores asociados a la intención de vacunación contra el COVID-19 en Popayán, Cauca, Colombia. Vacunas 2023, 24, 174–181. [Google Scholar] [CrossRef]
- LaRotta, J.; Escobar, O.; Ávila-Aguero, M.L.; Torres, J.P.; Sini de Almeida, R.; Morales, G.d.C.; Srivastava, A. COVID-19 in Latin America: A Snapshot in Time and the Road Ahead. Infect. Dis. Ther. 2023, 12, 389–410. [Google Scholar] [CrossRef]
- Ospina, J.; Hincapié- Palacio, D.; Ochoa, J.; Velásquez, C.; Almanza Payares, R. Monitoring COVID-19 in Colombia during the first year of the pandemic. J. Public Health Res. 2022, 11, 227990362211157. [Google Scholar] [CrossRef] [PubMed]
- Laajaj, R.; De Los Rios, C.; Sarmiento-Barbieri, I.; Aristizabal, D.; Behrentz, E.; Bernal, R.; Buitrago, G.; Cucunubá, Z.; De La Hoz, F.; Gaviria, A.; et al. COVID-19 spread, detection, and dynamics in Bogota, Colombia. Nat. Commun. 2021, 12, 4726. [Google Scholar] [CrossRef]
- Rojas-Botero, M.L.; Fernández-Niño, J.A.; Arregocés-Castillo, L.; Palacios-Clavijo, A.; Pinto-Álvarez, M.; Ruiz-Gómez, F. Real-world effectiveness of COVID-19 vaccines among Colombian adults: A retrospective, population-based study of the ESPERANZA cohort. PLoS Glob. Public Health 2023, 3, e0001845. [Google Scholar] [CrossRef]
- Arias-Murillo, Y.R.; Benavides-V, C.A.; Salinas-N, M.A.; Osorio-Arango, K.; Plazas-Sierra, C.; Cortés, J.A. SARS-CoV2/COVID-19 Infection in Transplant Recipients and in Patients on the Organ Transplant Waiting List in Colombia. Transplant. Proc. 2021, 53, 1237–1244. [Google Scholar] [CrossRef] [PubMed]
- Machado-Alba, J.E.; Valladales-Restrepo, L.F.; Machado-Duque, M.E.; Gaviria-Mendoza, A.; Sánchez-Ramírez, N.; Usma-Valencia, A.F.; Rodríguez-Martínez, E.; Rengifo-Franco, E.; Forero-Supelano, V.H.; Gómez-Ramirez, D.M.; et al. Factors associated with admission to the intensive care unit and mortality in patients with COVID-19, Colombia. PLoS ONE 2021, 16, e0260169. [Google Scholar] [CrossRef]
- Rebellón-Sánchez, D.E.; Guzmán, T.M.; Rodriguez, S.; Llanos-Torres, J.; Vinueza, D.; Tafurt, E.; Beltrán, E.; Martínez, Á.; Rosso, F. Navigating the waves in Colombia: A cohort study of inpatient care during four COVID-19 waves. Braz. J. Infect. Dis. 2024, 28, 103737. [Google Scholar] [CrossRef]
- MSPS Cifras de Aseguramiento en Salud-junio 2023. 2023. Available online: https://www.minsalud.gov.co/proteccionsocial/Paginas/cifras-aseguramiento-salud.aspx (accessed on 2 August 2023).
- WHO. Clinical Management of COVID-19: Living Guideline; WHO: Geneva, Switzerland, 2023. [Google Scholar]
- Amariles, P.; Granados, J.; Ceballos, M.; Montoya, C.J. COVID-19 in Colombia endpoints. Are we different, like Europe? Res. Soc. Adm. Pharm. 2021, 17, 2036–2039. [Google Scholar] [CrossRef] [PubMed]
- CDC. Underlying Medical Conditions Associated with Higher Risk for Severe COVID-19: Information for Healthcare Professionals. Cent. Dis. Control. Prev. 2020. Available online: https://www.cdc.gov/covid/hcp/clinical-care/underlying-conditions.html?CDC_AAref_Val=https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html (accessed on 2 July 2023).
- Rodriguez-Morales, A.J.; Cardona-Ospina, J.A.; Villamil-Gómez, W.E. Should we concern about reinfection in COVID-19? Infectio 2020, 25, 77. [Google Scholar] [CrossRef]
- Stein, C.; Nassereldine, H.; Sorensen, R.J.D.; Amlag, J.O.; Bisignano, C.; Byrne, S.; Castro, E.; Coberly, K.; Collins, J.K.; Dalos, J.; et al. Past SARS-CoV-2 infection protection against re-infection: A systematic review and meta-analysis. Lancet 2023, 401, 833–842. [Google Scholar] [CrossRef]
- Toro-Huamanchumo, C.J.; Hilario-Gomez, M.M.; Pinedo-Castillo, L.; Zumarán-Nuñez, C.J.; Espinoza-Gonzales, F.; Caballero-Alvarado, J.; Rodriguez-Morales, A.J.; Barboza, J.J. Clinical and epidemiological features of patients with COVID-19 reinfection: A systematic review. New Microbes New Infect. 2022, 48, 101021. [Google Scholar] [CrossRef]
- R Core Team R. A Language and Environment for Statistical Computing 2023; R Foundation for Statistical Computing: Vienna, Austria, 2023. [Google Scholar]
- INS COVID-19 en Colombia. Corte 07-06-2023: Genoma. COVID-19 En Colomb n.d. Available online: https://www.ins.gov.co/Noticias/Paginas/coronavirus-genoma.aspx (accessed on 20 February 2024).
- Holdcroft, E.; Aksamentov, I.; Neher, R.; Bedford, T.; Hadfield, J.; Zuber, M.; Scott-Brown, J.; Sanderson, T.; Bloom, J.; Roemer, C.; et al. Overview of Variants in Countries: Colombia. CoVariants n.d. Available online: https://covariants.org/per-country?country=Colombia (accessed on 20 February 2024).
- Mathieu, E.; Ritchie, H.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; Ortiz-Ospina, E.; et al. Coronavirus Pandemic (COVID-19); Our World Data 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 16 May 2025).
- INS Históricos de Casos por Fecha de Inicio de Síntomas. COVID-19 En Colomb Corte 07-06-2023 2023. Available online: https://www.ins.gov.co/Noticias/Paginas/coronavirus-casos.aspx (accessed on 20 March 2024).
- Reyes, L.F.; Bastidas, A.; Narváez, P.O.; Parra-Tanoux, D.; Fuentes, Y.V.; Serrano-Mayorga, C.C.; Ortíz, V.; Caceres, E.L.; Ospina-Tascon, G.; Díaz, A.M.; et al. Clinical characteristics, systemic complications, and in-hospital outcomes for patients with COVID-19 in Latin America. LIVEN-Covid-19 study: A prospective, multicenter, multinational, cohort study. PLoS ONE 2022, 17, e0265529. [Google Scholar] [CrossRef]
- Bouziotis, J.; Arvanitakis, M.; Preiser, J.-C. Association of body mass index with COVID-19 related in-hospital death. Clin. Nutr. 2022, 41, 2924–2926. [Google Scholar] [CrossRef]
- Guntur, V.P.; Modena, B.D.; Manka, L.A.; Eddy, J.J.; Liao, S.-Y.; Goldstein, N.M.; Zelarney, P.; Horn, C.A.; Keith, R.C.; Make, B.J.; et al. Characteristics and outcomes of ambulatory patients with suspected COVID-19 at a respiratory referral center. Respir. Med. 2022, 197, 106832. [Google Scholar] [CrossRef]
- Arregocés-Castillo, L.; Fernández-Niño, J.; Rojas-Botero, M.; Palacios-Clavijo, A.; Galvis-Pedraza, M.; Rincón-Medrano, L.; Pinto-Álvarez, M.; Ruiz-Gómez, F.; Trejo-Valdivia, B. Effectiveness of COVID-19 vaccines in older adults in Colombia: A retrospective, population-based study of the ESPERANZA cohort. Lancet Healthy Longev. 2022, 3, e242–e252. [Google Scholar] [CrossRef] [PubMed]
- Nomoto, H.; Suzuki, S.; Asai, Y.; Hayakawa, K.; Gatanaga, H.; Terada, M.; Suzuki, K.; Ohtsu, H.; Toyoda, A.; Ohmagari, N. Clinical characteristics and prognosis of immunosuppressed inpatients with COVID-19 in Japan. J. Infect. Chemother. 2022, 28, 224–231. [Google Scholar] [CrossRef] [PubMed]
- WHO. COVID-19 Cases, Country Level Trends. WHO COVID-19 Dashboard 2025. Available online: https://data.who.int/dashboards/covid19/cases?n=c (accessed on 29 April 2025).
- Ulrichs, T.; Rolland, M.; Wu, J.; Nunes, M.C.; El, C.; Chit, A. Changing epidemiology of COVID-19: Potential future impact on vaccines and vaccination strategies. Expert Rev. Vaccines 2024, 23, 510–522. [Google Scholar] [CrossRef] [PubMed]
- Mantilla-Morrón, M.; Suárez-Palacio, D.; Urina-Triana, M.A. The Level of Knowledge, Attitudes, and Practices in a Caribbean Colombian Population That Recovered from COVID-19 during the Pandemic. Healthcare 2023, 11, 3119. [Google Scholar] [CrossRef] [PubMed]
- Hasell, J.; Mathieu, E.; Beltekian, D.; Macdonald, B.; Giattino, C.; Ortiz-Ospina, E.; Roser, M.; Ritchie, H. A cross-country database of COVID-19 testing. Sci. Data 2020, 7, 345. [Google Scholar] [CrossRef]
- Our World in Data Testing for COVID-19. Test COVID-19 Colomb n.d. Available online: https://ourworldindata.org/coronavirus-testing (accessed on 22 May 2024).
- INS. Datos Abiertos Pruebas PCR procesadas de COVID-19 en Colombia. 2024. Available online: https://www.datos.gov.co/Salud-y-Protecci-n-Social/Pruebas-PCR-procesadas-de-COVID-19-en-Colombia-Dep/8835-5baf/about_data (accessed on 24 April 2024).
- John, J.N.; Gorman, S.; Scales, D. Understanding Interventions to Address Infodemics Through Epidemiological, Socioecological, and Environmental Health Models: Framework Analysis. JMIR Infodemiology 2025, 5, e67119. [Google Scholar] [CrossRef]
- Azevedo, N.H.; Massi, L.; Lima, G.S. Thematic trends in fact-checking in Brazil’s COVID-19 infodemic: The first year in focus. An. Acad. Bras. Ciênc. 2025, 97, e20240316. [Google Scholar] [CrossRef]
- Longcoy, J.; Patwari, R.; Hasler, S.; Johnson, T.; Avery, E.; Stefanini, K.; Suzuki, S.; Ansell, D.; Lynch, E. Racial and Ethnic Differences in Hospital Admissions of Emergency Department COVID-19 Patients. Med. Care 2022, 60, 415–422. [Google Scholar] [CrossRef]
- Shortreed, S.M.; Gray, R.; Akosile, M.A.; Walker, R.L.; Fuller, S.; Temposky, L.; Fortmann, S.P.; Albertson-Junkans, L.; Floyd, J.S.; Bayliss, E.A.; et al. Increased COVID-19 Infection Risk Drives Racial and Ethnic Disparities in Severe COVID-19 Outcomes. J. Racial Ethn. Health Disparities 2023, 10, 149–159. [Google Scholar] [CrossRef]
- Ribeiro, K.B.; Ribeiro, A.F.; Veras, M.A.D.S.M.; De Castro, M.C. Social inequalities and COVID-19 mortality in the city of São Paulo, Brazil. Int. J. Epidemiol. 2021, 50, 732–742. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).