1. Introduction
Snakebite envenoming (SBE) is a significant public health concern, particularly in tropical and subtropical regions [
1]. As per the World Health Organization (WHO), approximately five million people are bitten by snakes, and every year, 1.8 to 2.7 million people suffer from Envenoming [
1]. It leads to disabilities and psychological consequences in the aftermath of snakebites, particularly in developing regions. Underprivileged and rural communities in tropical and subtropical countries face major consequences [
2].
Considering the impact, WHO listed snakebite envenoming as a priority neglected tropical disease in 2017. It was recognized as developing and tropical countries facing almost 95% of the world’s snakebite-related burden. The decision aimed to highlight the urgency and create opportunities for increased investment in research funding to improve snakebite management in these regions. One of the primary reasons for its earlier removal from the Neglected Tropical Diseases (NTD) list was the lack of sufficient data from developing countries like India, which made it challenging to fully grasp the extent of the problem [
3].
SBE continues to be a significant yet long-neglected public health challenge in India, disproportionately affecting rural and tribal populations, particularly agricultural and forest-based communities [
4]. India accounts for nearly half of the global snakebite deaths, with an estimated 58,000 annual fatalities and three times as many long-term disabilities [
1].
India’s response to this public health challenge has evolved over time. The journey began with anti-venom (ASV) manufacturing at the Central Research Institute in Kasauli in 1920, followed by the Haffkine’s Institute in Mumbai in 1945 [
2]. Earlier approaches primarily focused on clinical management through training medical officers and ensuring the availability of anti-snake venom (ASV) in public health facilities. These efforts included the release of the Standard Treatment Guidelines for Snakebite Management in 2017, which was further refined in 2019 by the Ministry of Health and Family Welfare (MoHFW), which served as a guiding document for clinicians [
5].
Further, the Indian Council of Medical Research (ICMR) established a National Task Force Expert Group on Research on Snakebite in India. In 2019, two major research studies were funded under this initiative—one aimed at comprehensive data discovery to assess the burden, and the other focused on implementation research for health system strengthening [
5].
The evidence generated through these efforts has brought to light stark regional disparities in snakebite incidence, mortality, morbidity, and the capacity of the health system to respond. These findings emphasize that enhancing health infrastructure, empowering communities with accurate knowledge, and tailoring interventions to local contexts are pivotal for reducing the snakebite burden.
Further, a white paper was released by ICMR in 2020 [
3], which discussed the various reasons that could be attributed to the high mortality and morbidity due to venomous snakes and provided recommendations on policy decisions, improvement on the quality of venom and anti-snake venom and in promoting awareness on how to avoid snakebite. A Nationally Representative Mortality Survey conducted in March 2001 [
6] in India has highlighted that snakebite remains an underestimated cause of accidental death in modern India, and it is significantly underreported. The study suggested that an effective intervention involving education and anti-venom provision would reduce snakebite deaths in India.
The absence of a coordinated, multisectoral, and evidence-based approach has hindered the effectiveness of these interventions. Recognizing the urgent need for a structured, integrated, and sustainable approach, the National Action Plan for Prevention and Control of Snakebite Envenoming in India was developed. This plan aims to provide a comprehensive framework for reducing snakebite-related deaths and disabilities through coordinated actions across health, veterinary, environmental, and community sectors.
2. Current Scenario in India
Earlier research studies in India have shown that snakebite accounts for nearly half of the world’s snakebite-related deaths, with approximately 58,000 deaths resulting from an estimated 3–4 million snakebites annually [
7]. It is highlighted in these studies that a significant number of snakebite victims do not seek medical attention at clinics or hospitals, leading to a substantial underreporting of cases [
2]. The burden of premature deaths due to snakebite envenoming in India is estimated at 2.97 million disability-adjusted life years (DALYs), compared to the global burden of 6.07 million DALYs [
8].
Currently, snakebite cases and related deaths in India are monitored through the Integrated Diseases Surveillance Program–Integrated Health Information Portal (IDSP–IHIP). Community health workers document snakebite cases using the S (Suspected) form, while Medical Officers (MO) report presumptive snakebite cases and fatalities using the P form. Recently, IDSP launched a community reporting tool for any outbreak-related alert. In 2024, over 1.20 Lakhs cases were reported, with 370 deaths.
This gap in reporting is being addressed through continued IHIP training across all states and sensitization by the program division to gather snakebite-related data from stakeholders at the field level, i.e., forest department, agriculture department, and revenue department mainly documented for compensation/medico-legal requirements.
A dedicated informational and data portal is also being developed in the IHIP portal as part of the recent notification of snakebite cases and deaths, which in turn is expected to improve reporting from all sectors, including the private sector.
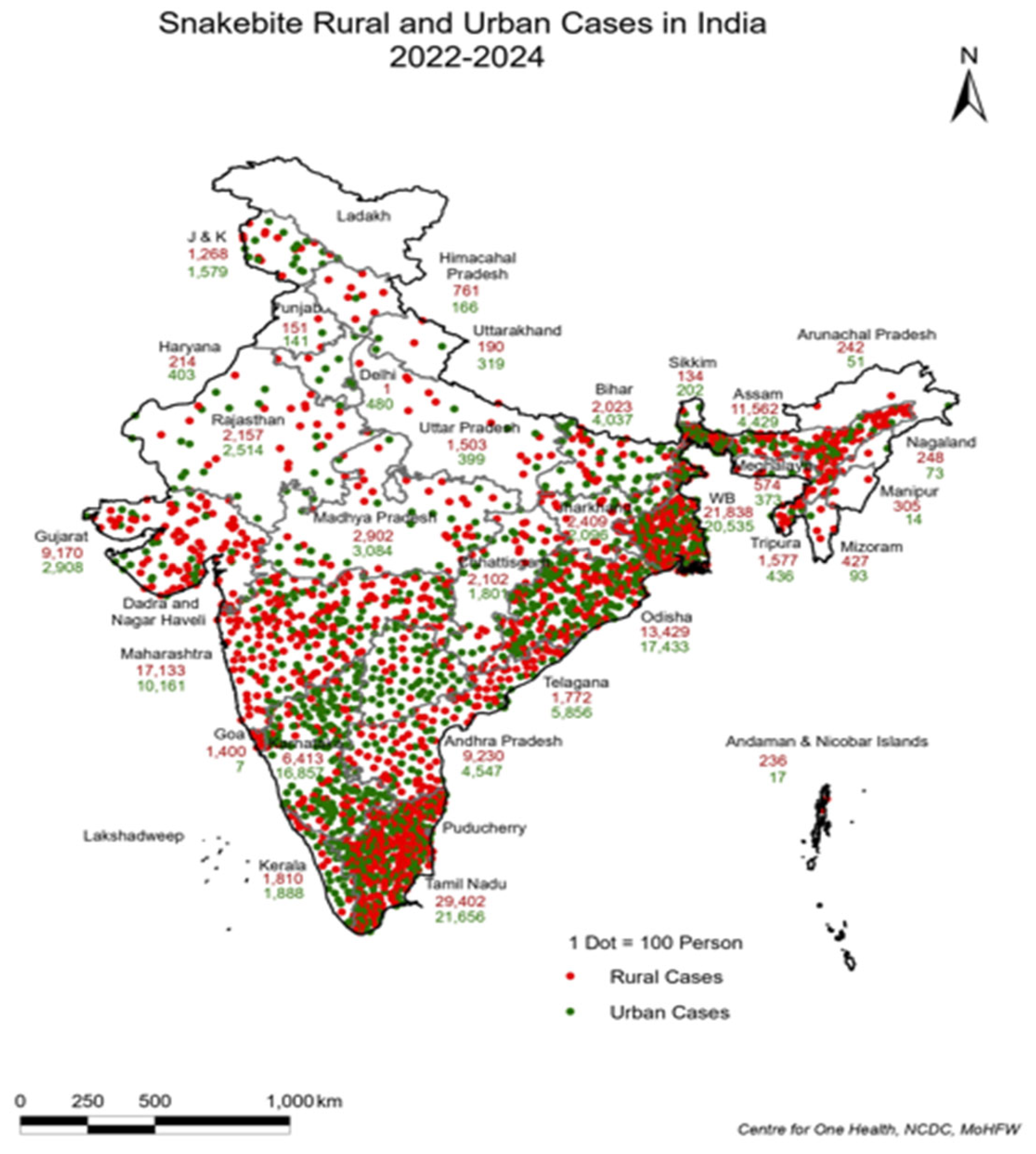
This staggering burden, primarily concentrated in rural (
Figure 1) and agricultural communities, is exacerbated by factors such as underreporting cases, delayed access to treatment, and a lack of adequately trained healthcare professionals. The bites of the “big four” venomous snake species, i.e., Indian cobra (
Naja naja), Russell’s viper (
Daboia russelii), common krait (
Bungarus caeruleus), and saw-scaled viper (
Echis carinatus) account for most of these cases.
As per the reported number of snakebites in IDSP, 46% of cases are being reported in rural areas. However,
Figure 1 also illustrates that snakebites are now increasingly reported from urban areas, likely due to unplanned urbanization, climate change, water logging, etc.
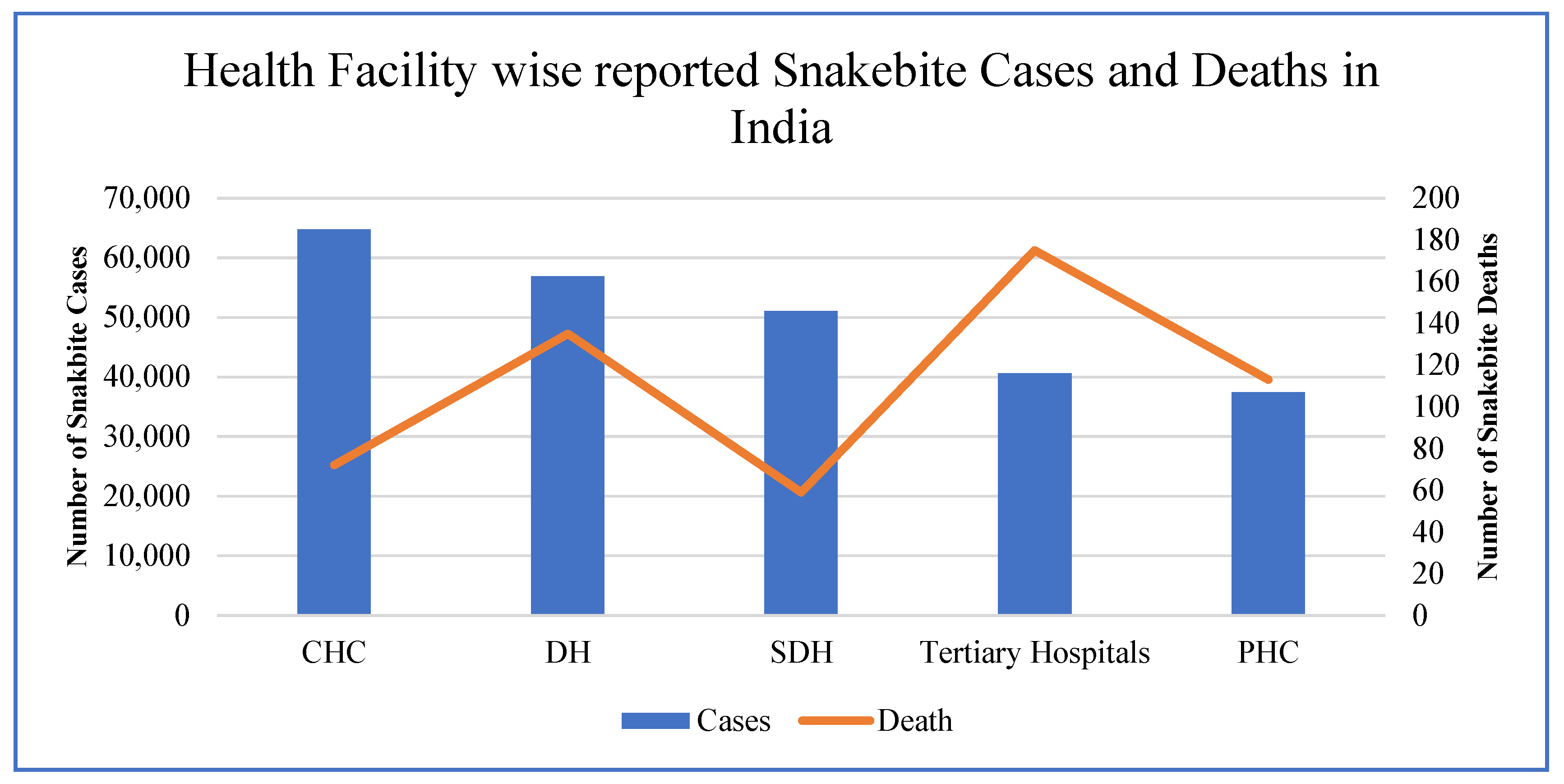
Figure 2 illustrates the distribution of snakebite cases and related deaths across different health facilities in India, highlighting significant variations in case reporting and fatality rates. Community Health Centers (CHCs) report the highest number of cases, followed by District Hospitals (DHs) and Sub-District Hospitals (SDHs), while Primary Health Centers (PHCs) record the lowest. However, mortality trends show a contrasting pattern, with tertiary hospitals experiencing the highest number of deaths, likely due to delayed referrals and patients arriving in critical condition.
This is also corroborated by research studies undertaken in India, e.g., Mohapatra et al. (2011) [
9] indicated that CHCs and DHs are the primary points of care for snakebite victims in rural India, whereas higher fatalities at tertiary hospitals suggest inefficiencies in early intervention. Additionally, PHCs report fewer cases but relatively higher mortality, underscoring the lack of adequate treatment facilities at the primary level. Other research studies also emphasize the same findings with an urgent need for improved snakebite management, timely referrals, and better-equipped rural healthcare centers to reduce mortality rates. Accordingly, under the Health System Strengthening (HSS) component of the National Health Mission (NHM), issues are being addressed through improved and timely transport of patients as part of 108 ambulance services. This ensures the availability of ASV and other emergency drugs, e.g., neostigmine up to the PHC level, and upskilling of medical officers at the PHC level to manage these cases.
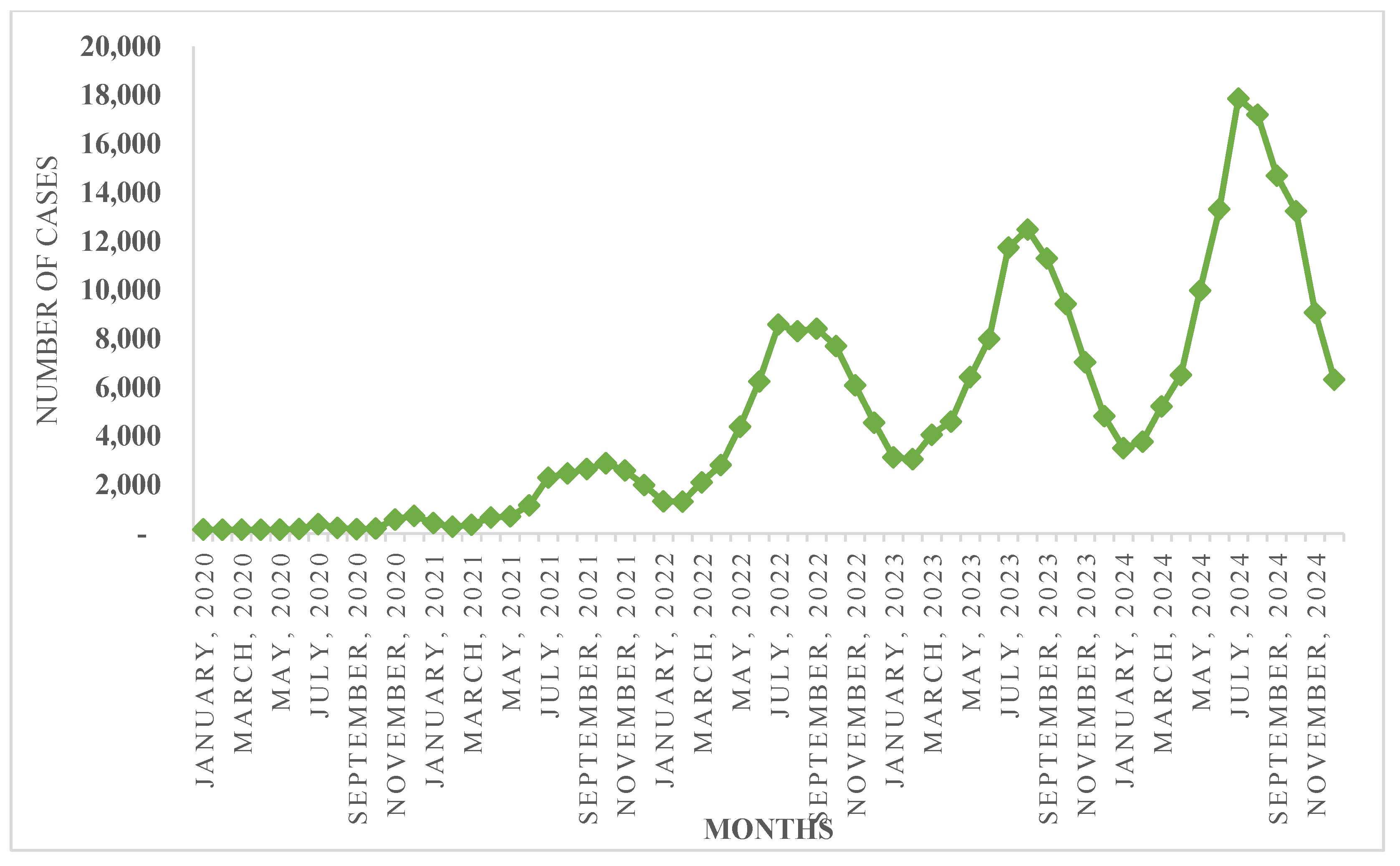
Data from IDSP–IHIP also reveals that snakebite cases typically peak in June and start declining in October, showing a seasonal pattern of increased incidents over the years (
Figure 3). Densely populated, low-altitude agricultural regions in states such as Karnataka, West Bengal, Jharkhand, Odisha, and Madhya Pradesh account for the majority of snakebite deaths, particularly during the rainy season when human–snake encounters are more common both indoors and outdoors. Considering these trends, a checklist for ensuring the availability of logistics and equipment is prepared, and states are encouraged to undertake training as part of pre-monsoon preparedness.
Addressing the immense burden of snakebite envenoming in India requires concerted and collaborative efforts to strengthen surveillance, enhance access to timely medical care, and promote community awareness.
3. Journey Towards Development of National Action Plan for Prevention and Control of Snakebite Envenoming (NAPSE) in India
Snakebite envenoming remains a critical yet often overlooked public health concern in India, particularly in rural and underserved regions where timely medical intervention is limited. To address this pressing issue, the Government of India initiated the development of the National Action Plan for Prevention and Control of Snakebite Envenoming in India (NAPSE), a comprehensive framework built through extensive collaboration, expert consultations, and community engagement.
The foundation for NAPSE was laid during a regional consultation on snakebite envenoming in the Southeast Asia Region (SEAR) in March 2022, where experts emphasized the need for a structured and strategic plan to tackle the multifaceted challenges of snakebite envenoming, especially among vulnerable populations.
During the consultation, it was highlighted that only 30% of SEAR countries have a national program dedicated to the prevention and control of snakebite envenoming. Among these, Myanmar, Nepal, and Thailand have established programs under respective health authorities.
A concerning finding was that only two countries, Bangladesh and Thailand, had a dedicated national strategy or plan for addressing snakebite envenoming.
Recognizing the urgency, the first National Consultation on Developing an Action Plan for Prevention and Control of Snakebite Envenoming was convened on 26 July 2022 under the leadership of the Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare. This event marked a pivotal step in solidifying India’s commitment to addressing snakebite envenoming at a national level.
A major outcome of the consultation was the recommendation to establish a dedicated program under the National Health Mission (NHM) to ensure uniform implementation of snakebite prevention and control initiatives across states and union territories. In response, the Centre for One Health, under the National Centre for Disease Control (NCDC), developed a proposal advocating for the inclusion of snakebite prevention activities under NHM. This proposal was subsequently presented at the 9th EPC meeting on 18 August 2022 and received approval from the Mission Steering Group of NHM, marking a significant milestone in integrating snakebite envenoming into India’s national health agenda.
As per the recommendation of the consultation, a core committee was constituted to draft NAPSE. Between February and March 2023, multiple consultative meetings were held with key stakeholders, including anti-snake venom manufacturers, NGOs, clinical experts, and communication officers.
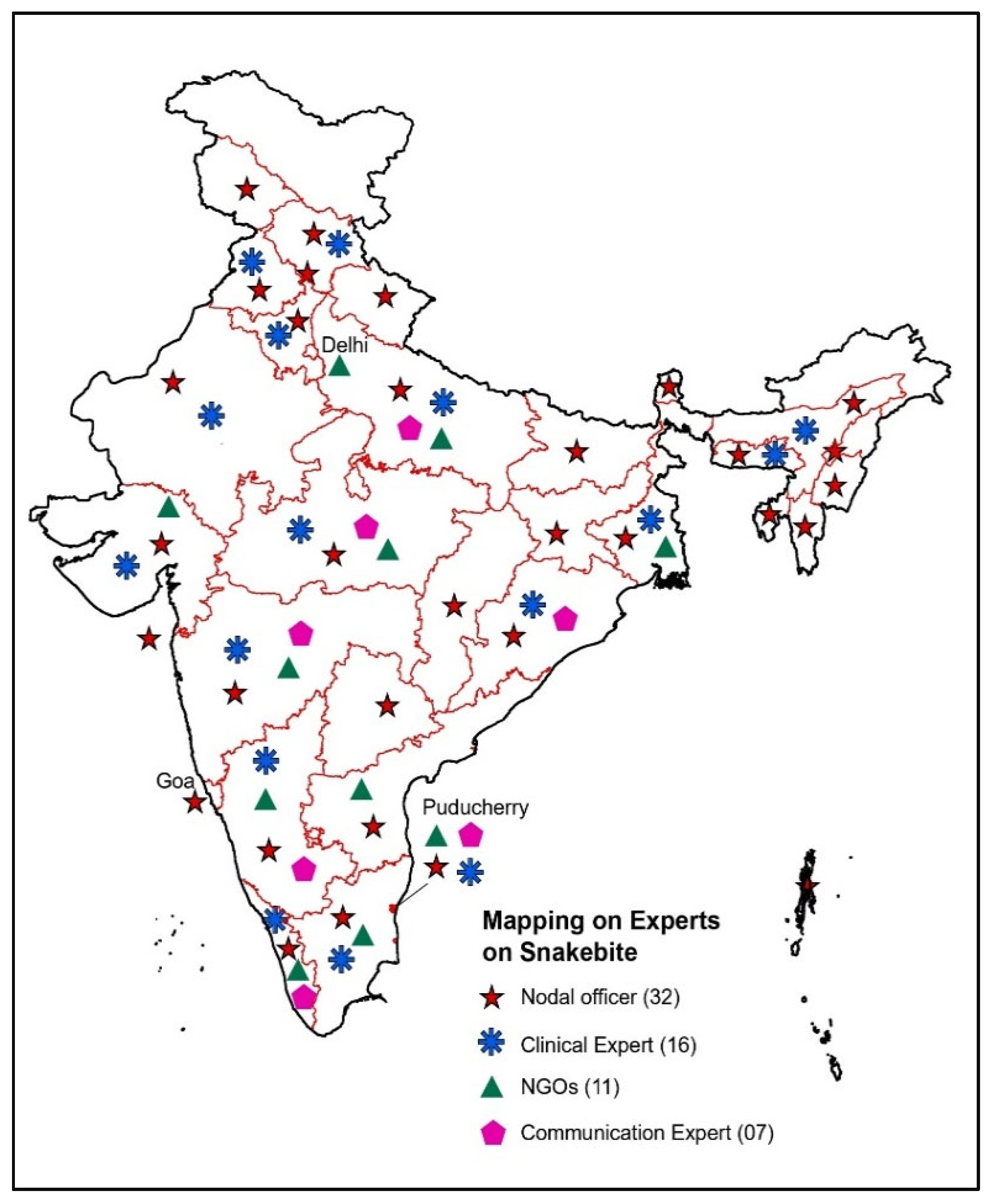
The Program division has mapped experts such as State Nodal Officers, Clinical Experts, NGOs, Communication experts, etc., in all States/UTs (
Figure 4 and
Figure 5). Their collective insights ensured that the plan was evidence-based and tailored to real-world challenges.
An inter-ministerial meeting on 28 August 2023 further reinforced a collaborative approach by bringing together various government ministries to define their roles and responsibilities under NAPSE. This initiative aimed to facilitate seamless implementation and align efforts across multiple sectors. Furthermore, the drafting process involved direct engagement with communities and healthcare professionals to identify on-ground challenges and ensure that the plan addressed the specific needs of those most affected by snakebites.
Understanding the importance of grassroots involvement, the drafting process also included community interactions and consultations with clinicians to identify challenges and requirements from the ground level. This ensured that the plan was not only comprehensive but also tailored to address the specific needs of communities most affected by snakebites.
The culmination of these efforts was the official launch of the National Action Plan for Prevention and Control of Snakebite Envenoming in India (NAPSE) in March 2024. The plan is a landmark initiative that aims to halve snakebite-related deaths by 2030, reflecting the government’s commitment to saving lives and improving public health. NAPSE adopts a One Health approach, integrating human, animal, and environmental health strategies to address snakebite envenoming comprehensively.
The key milestones in the planning and development of NAPSE are described in
Table 1.
It focuses on key areas such as strengthening the production and distribution of high-quality anti-venom, building healthcare capacity, enhancing transportation and emergency response systems, raising community awareness, and fostering multisectoral collaboration.
With this, India aims to lead the efforts in the Southeast Asia region for snakebite prevention and control efforts and contribute to the global goal of WHO to halve deaths by 2030.
A summary of initiatives by different countries in this regard is described in
Table 2.
4. Challenges in the Implementation of NAPSE
The implementation of the National Action Plan for Prevention and Control of Snakebite Envenoming (NAPSE) faces several challenges that could hinder its implementation. One of the most significant issues is the underreporting of snakebite cases due to inadequate surveillance systems and cultural stigma, which limits the availability of accurate data for informed decision-making. Ensuring consistent access to quality anti-snake venom (ASV) in rural and remote areas remains a logistical challenge. Many healthcare professionals, especially in primary health care, lack adequate training in managing snakebite envenoming, leading to delays or mismanagement in treatment. Poor emergency referral systems, including the lack of ambulances, further exacerbate the problem. Public awareness is another critical gap, as myths and misconceptions about snakebites often drive victims to seek harmful traditional remedies instead of timely medical care.
The success of NAPSE also depends on effective inter-sectoral coordination, which is often hampered by overlapping mandates and poor communication among stakeholders in the human health, wildlife, and veterinary sectors. Moreover, behavioral resistance among communities to adopt preventive measures or seek medical care promptly remains a persistent challenge. Addressing these challenges will require strengthening surveillance systems, ensuring equitable ASV distribution, enhancing healthcare provider training, establishing robust referral mechanisms, fostering inter-sectoral collaboration, and launching sustained awareness campaigns tailored to regional needs. By overcoming these barriers, NAPSE can achieve its mission of reducing snakebite-related deaths and disabilities across India.
5. Way Forward
Research studies over the years from 2000–2019 have identified several critical gaps in snakebite management across venom supply, legislation, medical care, and public awareness. Venom-related gaps include the absence of zonal venom banks, exclusion of region-specific venoms in ASV manufacturing, reliance on wild snakes for venom collection, lack of quality testing, unregulated venom pricing, and insufficient research on alternative ASV production techniques and monovalent ASVs. Legislative gaps involve the lack of mandatory reporting, standardized ICD coding, school-based awareness programs, and the medico-legal classification of snakebites, which delays treatment. Medical and diagnostic gaps include inadequate healthcare worker training, absence of venom detection kits, non-uniform treatment protocols, lack of curriculum integration, and exclusion of snakebite treatment from government health schemes. Public awareness and outreach gaps stem from limited prevention knowledge, the absence of large-scale preventive measures, continued belief in traditional remedies, and the lack of a 24/7 snakebite helpline.
To address the numerous challenges and achieve the objectives of the National Action Plan for Snakebite Envenoming (NAPSE), a well-rounded, multifaceted approach is essential. Recognizing the complexity of the issue and the diverse needs across the country, the ministry has devised a strategic roadmap to ensure no region or community is left behind in the fight against snakebite mortality and morbidity.
A critical step in this direction is the designation of snakebite as a notifiable disease in India, strengthening surveillance and data collection efforts. This measure will enhance the ability to track cases accurately, identify high-risk areas, and allocate resources effectively for prevention and treatment.
Currently, the priority is to improve the safety and quality of current polyvalent snake venom. A committee on monitoring antisera has been constituted to review the above issues with manufacturers and regulators. Collaboration is being made with domestic and international stakeholders to support the venom collection centers for improving the quality of venom. Further, one of the important initiatives under the program is to strengthen the Regional Venom Centers in five regions of India. These Regional Venom Centers will focus on conducting region-specific venom research on the Big Four snake species—Indian cobra (
Naja naja), Russell’s viper (
Daboia russelii), common krait (
Bungarus caeruleus), and saw-scaled viper (
Echis carinatus)—as well as other venomous species unique to different zones. A key priority will be the development of region-specific ASVs, ensuring that anti-venom formulations effectively neutralize the venoms of species prevalent in specific geographical areas. Studies suggest that region-specific anti-snake venoms (ASVs) significantly improve treatment outcomes compared to generalized ASVs. Research studies [
3] show that tailored ASVs can enhance neutralization efficiency and reduce treatment-related complications. By strengthening these research and production capabilities, the Regional Venom Centers will play a crucial role in improving snakebite treatment, reducing mortality, and enhancing public health outcomes across India.
In addition to improving access to anti-venom, strengthening Poison Information Centers (PICs) in every state and union territory is an important initiative under the program. These centers will serve as knowledge hubs, equipping healthcare professionals with evidence-based guidelines, training, and support for snakebite management. Standardizing treatment protocols through PICs ensures that snakebite victims receive prompt and effective care, regardless of their location. The current protocol of administrating the first dose with at least 10 vials at PHC/CHC level is being advocated to ensure that 90% of toxins are neutralized in every snakebite victim to ensure the saving of lives. Investigation of every death reported under the system or scanned in media reports using a standardized verbal autopsy form is a key tool adopted by the program addressing the issues responsible for snakebite deaths.
Moreover, upgrading emergency treatment facilities is one of the key priorities. Healthcare providers will undergo specialized and standardized training in snakebite treatment, and medical infrastructure will be enhanced to address the high-risk cases of Snakebite Envenoming.
Beyond improving clinical response, focus has also been placed on improving the transportation and referral system, as timely medical intervention is crucial in saving lives. Additionally, the program division has focused on conducting community awareness campaigns and educational programs, particularly targeting rural and tribal populations who are most vulnerable to snakebites. Some Information, Education, and Communication materials have also been developed. These initiatives will emphasize the importance of seeking immediate medical attention rather than relying on traditional remedies, which often exacerbate the situation. By dispelling myths and misconceptions, these programs will empower communities to respond effectively to snakebite emergencies.
To maximize the impact of these efforts, the MoHFW has taken significant steps to collaborate with stakeholders. Government agencies, healthcare institutions, non-governmental organizations (NGOs), and community organizations have been roped in a coordinated manner, pooling resources, expertise, and networks to achieve shared objectives. This collective approach will ensure that snakebite envenoming is tackled in a sustainable and effective manner.
Regular monitoring and evaluation mechanisms will also be implemented to assess progress, identify gaps, and make data-driven adjustments to strategies. By maintaining flexibility and responsiveness, the program can adapt to changing circumstances and emerging challenges over time.
Through this comprehensive and concerted effort, the ambitious goal of halving snakebite-related deaths by 2030 becomes both realistic and achievable. These initiatives will not only reduce the burden of snakebite envenoming but will also strengthen public health systems, build community resilience, and save countless lives, ultimately contributing to improved health outcomes and a healthier future for India.