Refractive Effect of Epithelial Remodelling in Myopia after Transepithelial Photorefractive Keratectomy
Abstract
1. Introduction
2. Materials and Methods
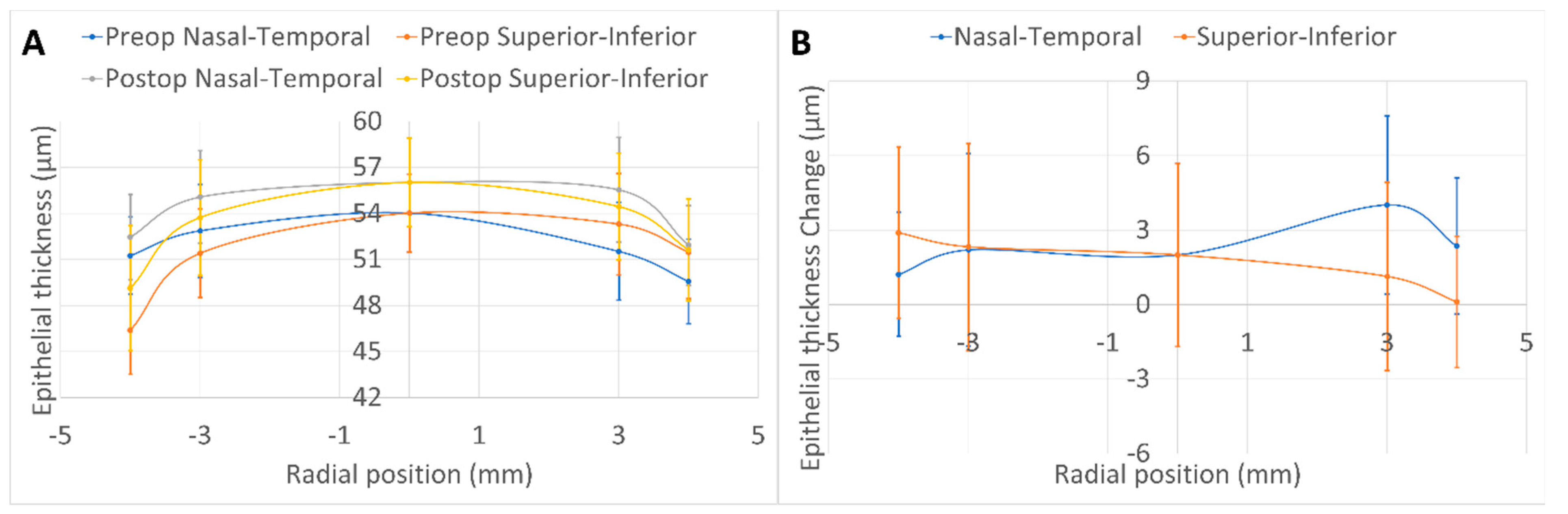
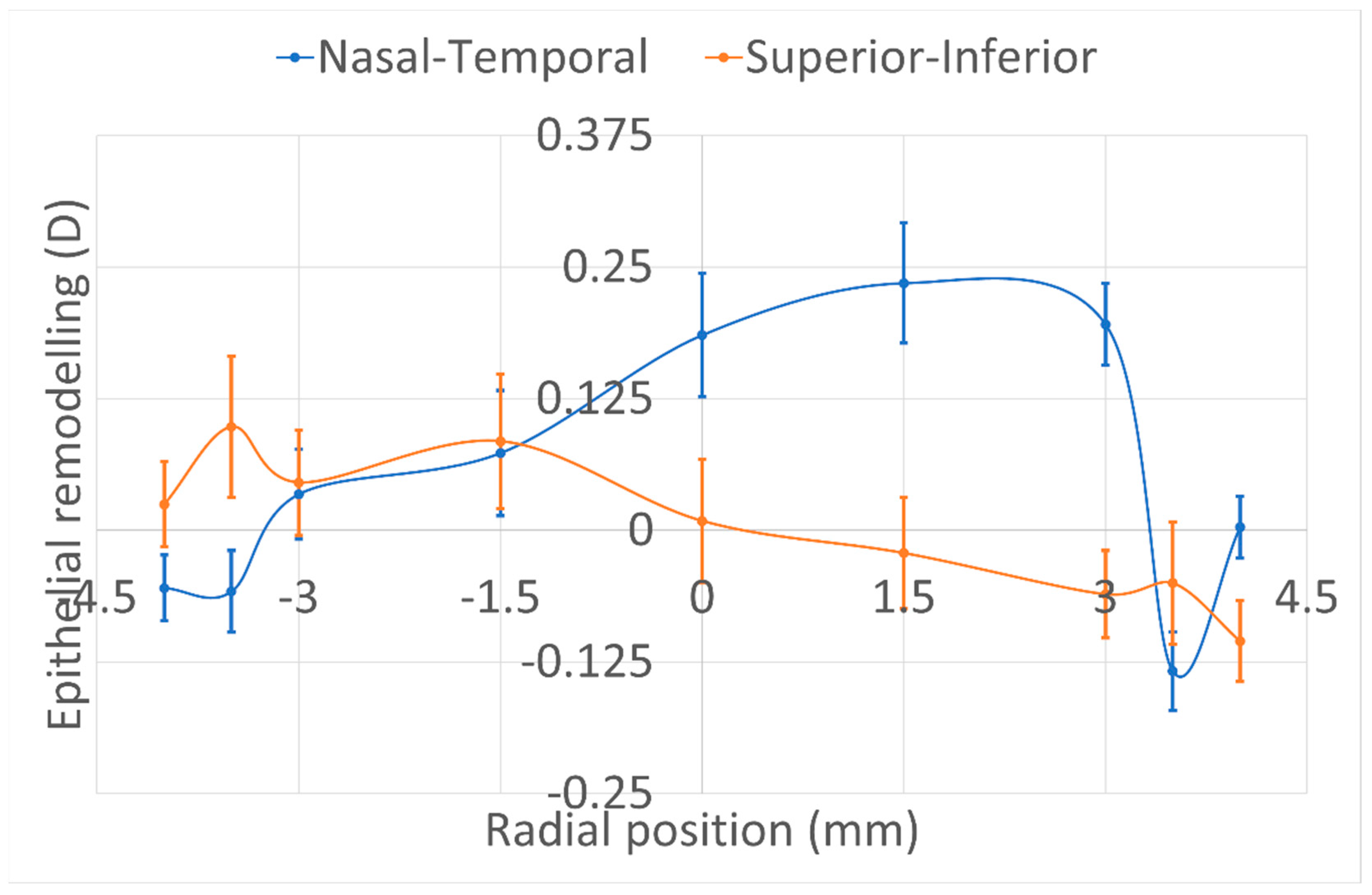
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Marshall, J.; Trokel, S.; Rothery, S.; Krueger, R.R. A Comparative Study of Corneal Incisions Induced by Diamond and Steel Knives and Two Ultraviolet Radiations from an Excimer Laser. Br. J. Ophthalmol. 1986, 70, 482–501. [Google Scholar] [CrossRef] [PubMed]
- Munnerlyn, C.R.; Koons, S.J.; Marshall, J. Photorefractive Keratectomy: A Technique for Laser Refractive Surgery. J. Cataract Refract. Surg. 1988, 14, 46–52. [Google Scholar] [CrossRef]
- Buratto, L.; Ferrari, M. Excimer Laser Intrastromal Keratomileusis: Case Reports. J. Cataract Refract. Surg. 1992, 18, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.; Shah, S.; Sengupta, S. Results of Small Incision Lenticule Extraction: All-in-One Femtosecond Laser Refractive Surgery. J. Cataract Refract. Surg. 2011, 37, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Ficker, L.A.; Bates, A.K.; Steele, A.D.M.; Lyons, C.J.; Milliken, A.B.; Astin, C.; Slattery, K.; Kirkness, C.M. Excimer Laser Photorefractive Keratectomy for Myopia: 12 Month Follow-Up. Eye 1993, 7, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Dausch, D.; Klein, R.; Schröder, E.; Dausch, B. Excimer Laser Photorefractive Keratectomy with Tapered Transition Zone for High Myopia: A Preliminary Report of Six Cases. J. Cataract Refract. Surg. 1993, 19, 590–594. [Google Scholar] [CrossRef]
- Seiler, T.; Holschbach, A.; Derse, M.; Jean, B.; Genth, U. Complications of Myopic Photorefractive Keratectomy with the Excimer Laser. Ophthalmology 1994, 101, 153–160. [Google Scholar] [CrossRef]
- Lohmann, C.P.; Guell, J.L. Regression After LASIK for the Treatment of Myopia: The Role of the Corneal Epithelium. Semin. Ophthalmol. 1998, 13, 79–82. [Google Scholar] [CrossRef]
- Reinstein, D.Z.; Archer, T.J.; Gobbe, M. Rate of Change of Curvature of the Corneal Stromal Surface Drives Epithelial Compensatory Changes and Remodeling. J. Refract. Surg. 2014, 30, 800–802. [Google Scholar] [CrossRef]
- Sedaghat, M.-R.; Momeni-Moghaddam, H.; Gazanchian, M.; Reinstein, D.Z.; Archer, T.J.; Randleman, J.B.; Hosseini, S.R.; Nouri-Hosseini, G. Corneal Epithelial Thickness Mapping After Photorefractive Keratectomy for Myopia. J. Refract. Surg. 2019, 35, 632–641. [Google Scholar] [CrossRef]
- Spadea, L.; Fasciani, R.; Necozione, S.; Balestrazzi, E. Role of the Corneal Epithelium in Refractive Changes Following Laser in Situ Keratomileusis for High Myopia. J. Refract. Surg. 2000, 16, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Reinstein, D.Z.; Archer, T.J.; Gobbe, M. Lenticule Thickness Readout for Small Incision Lenticule Extraction Compared to Artemis Three-Dimensional Very High-Frequency Digital Ultrasound Stromal Measurements. J. Refract. Surg. 2014, 30, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Shetty, R.; Narasimhan, R.; Dadachanji, Z.; Patel, P.; Maheshwari, S.; Chabra, A.; Sinha Roy, A. Early Corneal and Epithelial Remodeling Differences Identified by OCT Imaging and Artificial Intelligence Between Two Transepithelial PRK Platforms. J. Refract. Surg. 2020, 36, 678–686. [Google Scholar] [CrossRef] [PubMed]
- de Ortueta, D.; Arba Mosquera, S.; Baatz, H. Comparison of Standard and Aberration-Neutral Profiles for Myopic LASIK with the SCHWIND ESIRIS Platform. J. Refract. Surg. 2009, 25, 339–349. [Google Scholar] [CrossRef]
- Aslanides, I.M.; Padroni, S.; Arba Mosquera, S.; Ioannides, A.; Mukherjee, A. Comparison of Single-Step Reverse Transepithelial All-Surface Laser Ablation (ASLA) to Alcohol-Assisted Photorefractive Keratectomy. Clin. Ophthalmol. 2012, 6, 973–980. [Google Scholar] [CrossRef]
- Reinstein, D.Z.; Archer, T.J.; Randleman, J.B. JRS Standard for Reporting Astigmatism Outcomes of Refractive Surgery. J. Refract. Surg. 2014, 30, 654–659. [Google Scholar] [CrossRef]
- de Ortueta, D.; Arba Mosquera, S.; Baatz, H. Aberration-Neutral Ablation Pattern in Hyperopic LASIK with the ESIRIS Laser Platform. J. Refract. Surg. 2009, 25, 175–184. [Google Scholar] [CrossRef]
- Fan, L.; Xiong, L.; Zhang, B.; Wang, Z. Longitudinal and Regional Non-Uniform Remodeling of Corneal Epithelium After Topography-Guided FS-LASIK. J. Refract. Surg. 2019, 35, 88–95. [Google Scholar] [CrossRef]
- Savini, G.; Schiano-Lomoriello, D.; Hoffer, K.J. Repeatability of Automatic Measurements by a New Anterior Segment Optical Coherence Tomographer Combined with Placido Topography and Agreement with 2 Scheimpflug Cameras. J. Cataract Refract. Surg. 2018, 44, 471–478. [Google Scholar] [CrossRef]
- de Ortueta, D.; Arba Mosquera, S. Topographic Stability after Hyperopic LASIK. J. Refract. Surg. 2010, 26, 547–554. [Google Scholar] [CrossRef]
- Available online: https://www.iso.org/obp/ui/#iso:std:iso:10938:ed-2:v1:en (accessed on 29 September 2021).
- de Ortueta, D.; von Rüden, D.; Verma, S.; Magnago, T.; Arba-Mosquera, S. Transepithelial Photorefractive Keratectomy in Moderate to High Astigmatism With a Non-Wavefront-Guided Aberration-Neutral Ablation Profile. J. Refract. Surg. 2018, 34, 466–474. [Google Scholar] [CrossRef] [PubMed]
- Kato, N.; Toda, I.; Hori-Komai, Y.; Sakai, C.; Tsubota, K. Five-Year Outcome of LASIK for Myopia. Ophthalmology 2008, 115, 839–844.e2. [Google Scholar] [CrossRef]
- el-Agha, M.S.; Johnston, E.W.; Bowman, R.W.; Cavanagh, H.D.; McCulley, J.P. Excimer Laser Treatment of Spherical Hyperopia: PRK or LASIK? Trans. Am. Ophthalmol. Soc. 2000, 98, 59–66; discussion 66–69. [Google Scholar] [PubMed]
- Spadea, L.; Sabetti, L.; D’Alessandri, L.; Balestrazzi, E. Photorefractive Keratectomy and LASIK for the Correction of Hyperopia: 2-Year Follow-Up. J. Refract. Surg. 2006, 22, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.E.; Klyce, S.D.; McDonald, M.B.; Liu, J.C.; Kaufman, H.E. Changes in Corneal Topography after Excimer Laser Photorefractive Keratectomy for Myopia. Ophthalmology 1991, 98, 1338–1347. [Google Scholar] [CrossRef] [PubMed]
- Kanellopoulos, A.J. Comparison of Corneal Epithelial Remodeling Over 2 Years in LASIK Versus SMILE: A Contralateral Eye Study. Cornea 2019, 38, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Ryu, I.-H.; Kim, B.J.; Lee, J.-H.; Kim, S.W. Comparison of Corneal Epithelial Remodeling After Femtosecond Laser-Assisted LASIK and Small Incision Lenticule Extraction (SMILE). J. Refract. Surg. 2017, 33, 250–256. [Google Scholar] [CrossRef]
- Kanellopoulos, A.J.; Asimellis, G. Longitudinal Postoperative Lasik Epithelial Thickness Profile Changes in Correlation with Degree of Myopia Correction. J. Refract. Surg. 2014, 30, 166–171. [Google Scholar] [CrossRef]
- Reinstein, D.Z.; Srivannaboon, S.; Gobbe, M.; Archer, T.J.; Silverman, R.H.; Sutton, H.; Coleman, D.J. Epithelial Thickness Profile Changes Induced by Myopic LASIK as Measured by Artemis Very High-Frequency Digital Ultrasound. J. Refract. Surg. 2009, 25, 444–450. [Google Scholar] [CrossRef]
- Lin, D.T.C.; Holland, S.P.; Verma, S.; Hogden, J.; Arba-Mosquera, S. Postoperative Corneal Asphericity in Low, Moderate, and High Myopic Eyes After Transepithelial PRK Using a New Pulse Allocation. J. Refract. Surg. 2017, 33, 820–826. [Google Scholar] [CrossRef]
- Kaluzny, B.J.; Szkulmowski, M.; Bukowska, D.M.; Wojtkowski, M. Spectral OCT with Speckle Contrast Reduction for Evaluation of the Healing Process after PRK and Transepithelial PRK. Biomed. Opt. Express 2014, 5, 1089–1098. [Google Scholar] [CrossRef] [PubMed]
- Jun, I.; Kang, D.S.Y.; Arba-Mosquera, S.; Kim, E.K.; Seo, K.Y.; Kim, T.-I. Clinical Outcomes of Transepithelial Photorefractive Keratectomy According to Epithelial Thickness. J. Refract. Surg. 2018, 34, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Netto, M.V.; Mohan, R.R.; Sinha, S.; Sharma, A.; Dupps, W.; Wilson, S.E. Stromal Haze, Myofibroblasts, and Surface Irregularity after PRK. Exp. Eye Res. 2006, 82, 788–797. [Google Scholar] [CrossRef]
- Vinciguerra, P.; Azzolini, M.; Airaghi, P.; Radice, P.; De Molfetta, V. Effect of Decreasing Surface and Interface Irregularities after Photorefractive Keratectomy and Laser in Situ Keratomileusis on Optical and Functional Outcomes. J. Refract. Surg. 1998, 14, S199–S203. [Google Scholar] [CrossRef] [PubMed]
- Vinciguerra, P.; Camesasca, F.I.; Vinciguerra, R.; Arba-Mosquera, S.; Torres, I.; Morenghi, E.; Randleman, J.B. Advanced Surface Ablation With a New Software for the Reduction of Ablation Irregularities. J. Refract. Surg. 2017, 33, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Moshirfar, M.; Desautels, J.D.; Walker, B.D.; Murri, M.S.; Birdsong, O.C.; Hoopes, P.C.S. Mechanisms of Optical Regression Following Corneal Laser Refractive Surgery: Epithelial and Stromal Responses. Med. Hypothesis Discov. Innov. Ophthalmol. 2018, 7, 1–9. [Google Scholar] [PubMed]
- Fantes, F.E.; Waring, G.O. Effect of Excimer Laser Radiant Exposure on Uniformity of Ablated Corneal Surface. Lasers Surg. Med. 1989, 9, 533–542. [Google Scholar] [CrossRef]
- Reinstein, D.Z.; Archer, T.J.; Gobbe, M. Improved Effectiveness of Transepithelial PTK versus Topography-Guided Ablation for Stromal Irregularities Masked by Epithelial Compensation. J. Refract. Surg. 2013, 29, 526–533. [Google Scholar] [CrossRef]
- Huang, D.; Tang, M.; Shekhar, R. Mathematical Model of Corneal Surface Smoothing after Laser Refractive Surgery. Am. J. Ophthalmol. 2003, 135, 267–278. [Google Scholar] [CrossRef]
- Aslanides, I.M.; Kymionis, G.D. Trans Advanced Surface Laser Ablation (TransPRK) Outcomes Using SmartPulseTechnology. Cont Lens Anterior Eye 2017, 40, 42–46. [Google Scholar] [CrossRef]
- Kaluzny, B.J.; Piotrowiak-Slupska, I.; Kaszuba-Modrzejewska, M.; Stachura, J.; Arba-Mosquera, S.; Verma, S. Three-Year Outcomes after High Hyperopia Correction Using Photorefractive Keratectomy with a Large Ablation Zone. Br. J. Ophthalmol. 2019, 103, 849–854. [Google Scholar] [CrossRef] [PubMed]
- Gauthier-Fournet, L.; Penin, F.; Arba Mosquera, S. Six-Month Outcomes After High Hyperopia Correction Using Laser-Assisted In Situ Keratomileusis With a Large Ablation Zone. Cornea 2019, 38, 1147–1153. [Google Scholar] [CrossRef] [PubMed]
- Simon, G.; Ren, Q.; Kervick, G.N.; Parel, J.M. Optics of the Corneal Epithelium. Refract. Corneal Surg. 1993, 9, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Salah-Mabed, I.; Saad, A.; Gatinel, D. Topography of the Corneal Epithelium and Bowman Layer in Low to Moderately Myopic Eyes. J. Cataract Refract. Surg. 2016, 42, 1190–1197. [Google Scholar] [CrossRef]
- Lohmann, C.P.; Patmore, A.; O’Brart, D.; Reischl, U.; Winkler Mohrenfels, C.; Marshall, J. Regression and Wound Healing after Excimer Laser PRK: A Histopathological Study on Human Corneas. Eur. J. Ophthalmol. 1997, 7, 130–138. [Google Scholar] [CrossRef]
- Moller-Pedersen, T.; Cavanagh, H.D.; Petroll, W.M.; Jester, J.V. Stromal Wound Healing Explains Refractive Instability and Haze Development after Photorefractive Keratectomy: A 1-Year Confocal Microscopic Study. Ophthalmology 2000, 107, 1235–1245. [Google Scholar] [CrossRef]
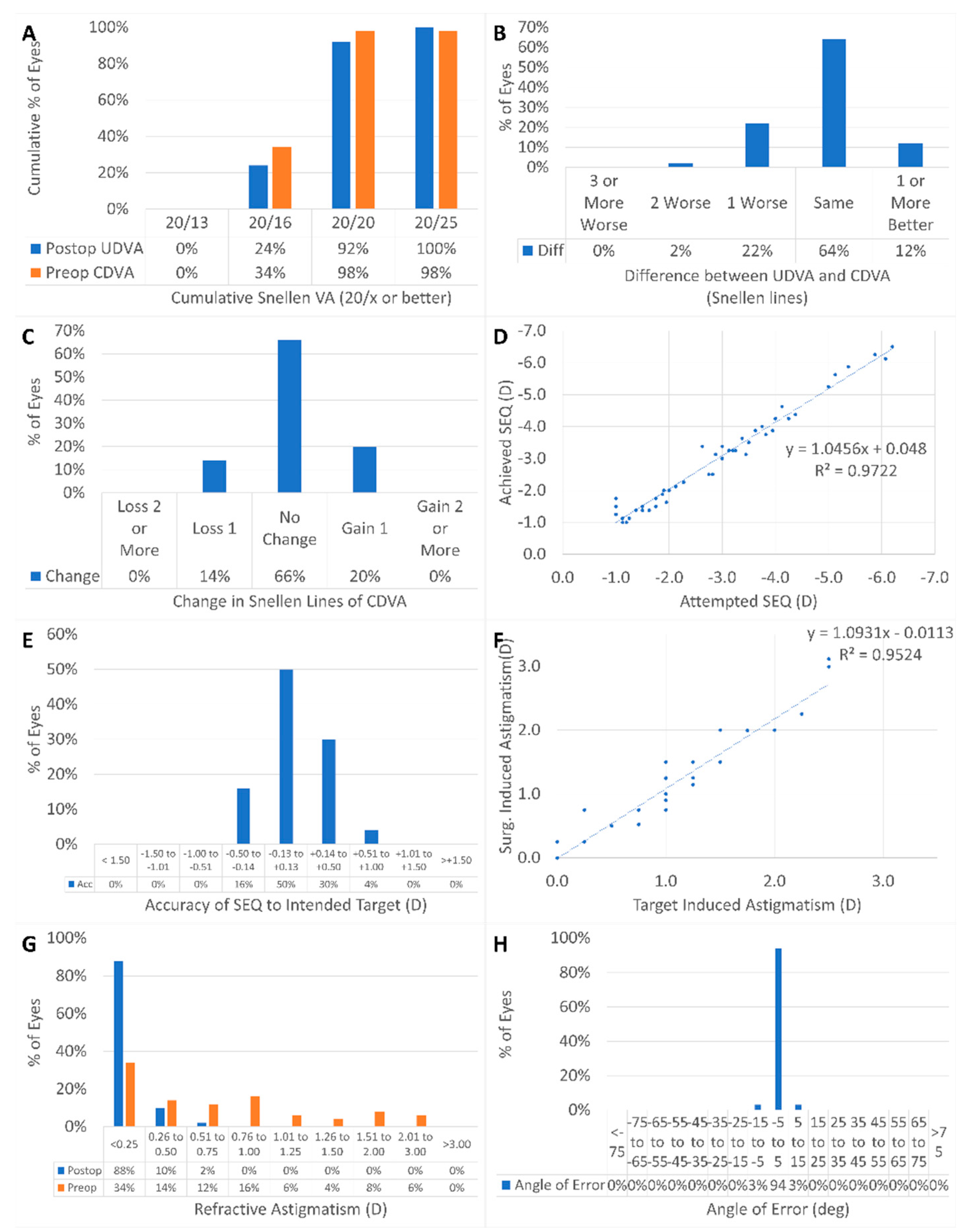



| Parameter (Unit) | Preoperative Value | Postoperative Value | p-Value |
|---|---|---|---|
| Number of eyes | 50 | 50 | --- |
| Laterality OD (%) | 48% | 48% | --- |
| UDVA (logMAR) | 0.9 ± 0.5 (0.2 to 2.0) | 0.0 ± 0.1 (−0.1 to 0.1) | <0.0001 |
| Manifest sphere (D) | −2.41 ± 1.49 −6.00 to 0.00) | 0.18 ± 0.23 (−0.25 to 0.75) | <0.0001 |
| Manifest cylinder (D) | −0.80 ± 0.69 (−2.50 to 0.00) | −0.11 ± 0.19 (−0.75 to 0.00) | <0.0001 |
| CDVA (logMAR) | 0.0 ± 0.1 (−0.1 to 0.2) | 0.0 ± 0.1 (−0.1 to 0.1) | 0.2 |
| Target sphere (D) | 0.05 ± 0.11 (−0.10 to 0.32) | --- | --- |
| Optical zone (mm) | 6.9 ± 0.2 (6.5 to 7.5) | --- | --- |
| Ablation depth (µm) | 111 ± 23 (75 to 162) | --- | --- |
| 3 mm flat keratometry (D) | 42.9 ± 1.7 (39.6 to 47.2) | 40.2 ± 2.4 35.6 to 46.4) | <0.0001 |
| 3 mm steep keratometry (D) | 43.8 ± 1.9 (41.1 to 49.7) | 41.0 ± 2.5 (36.0 to 47.0) | <0.0001 |
| Thinnest epithelium (µm) | 47 ± 3 (42 to 53) | 48 ± 4 (39 to 54) | 0.006 |
| X-position thinnest epithelium (µm) | 46 ± 209 (−272 to 280) | 27 ± 176 (−277 to 207) | 0.2 |
| Y-position thinnest epithelium (µm) | 190 ± 123 (−216 to 280) | 32 ± 234 (−280 to 279) | 0.008 |
| Central epithelium thickness (µm) | 54 ± 3 (48 to 58) | 56 ± 3 (47 to 61) | 0.0002 |
| 3 mm nasal epithelium thickness (µm) | 53 ± 3 (47 to 59) | 55 ± 3 (44 to 61) | 0.0001 |
| 3 mm temporal epithelium thickness (µm) | 52 ± 3 (46 to 59) | 56 ± 3 (46 to 63) | <0.0001 |
| 3 mm superior epithelium thickness (µm) | 51 ± 3 (46 to 57) | 54 ± 4 (44 to 61) | 0.0001 |
| 3 mm inferior epithelium thickness (µm) | 53 ± 3 (47 to 60) | 54 ± 3 (44 to 60) | 0.02 |
| 4 mm nasal epithelium thickness (µm) | 51 ± 3 (45 to 56) | 52 ± 3 (46 to 58) | 0.0007 |
| 4 mm temporal epithelium thickness (µm) | 50 ± 3 (44 to 57) | 52 ± 3 (46 to 58) | <0.0001 |
| 4 mm superior epithelium thickness (µm) | 46 ± 3 (40 to 55) | 49 ± 4 (38 to 56) | <0.0001 |
| 4 mm inferior epithelium thickness (µm) | 51 ± 3 (46 to 58) | 52 ± 3 (42 to 58) | 0.4 |
| Central corneal thickness (µm) | 551 ± 30 (490 to 628) | 484 ± 42 (405 to 582) | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Ortueta, D.; von Rüden, D.; Arba-Mosquera, S. Refractive Effect of Epithelial Remodelling in Myopia after Transepithelial Photorefractive Keratectomy. Vision 2022, 6, 74. https://doi.org/10.3390/vision6040074
de Ortueta D, von Rüden D, Arba-Mosquera S. Refractive Effect of Epithelial Remodelling in Myopia after Transepithelial Photorefractive Keratectomy. Vision. 2022; 6(4):74. https://doi.org/10.3390/vision6040074
Chicago/Turabian Stylede Ortueta, Diego, Dennis von Rüden, and Samuel Arba-Mosquera. 2022. "Refractive Effect of Epithelial Remodelling in Myopia after Transepithelial Photorefractive Keratectomy" Vision 6, no. 4: 74. https://doi.org/10.3390/vision6040074
APA Stylede Ortueta, D., von Rüden, D., & Arba-Mosquera, S. (2022). Refractive Effect of Epithelial Remodelling in Myopia after Transepithelial Photorefractive Keratectomy. Vision, 6(4), 74. https://doi.org/10.3390/vision6040074





