Kyrieleis Arteriolitis Associated with Acute Retinal Necrosis Due to Herpes Simplex Virus Type 1 Secondary to Herpetic Encephalitis
Abstract
:1. Introduction
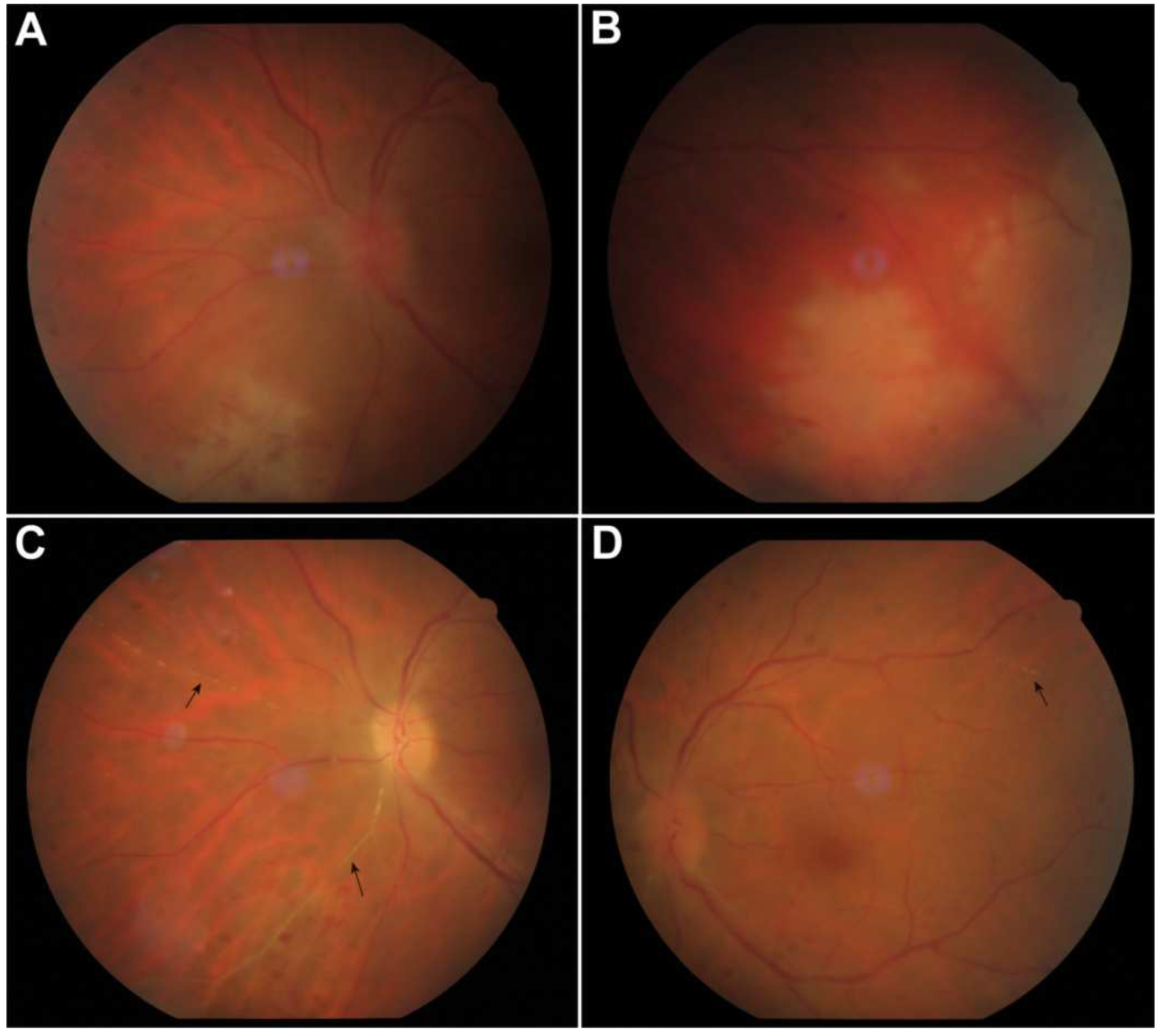
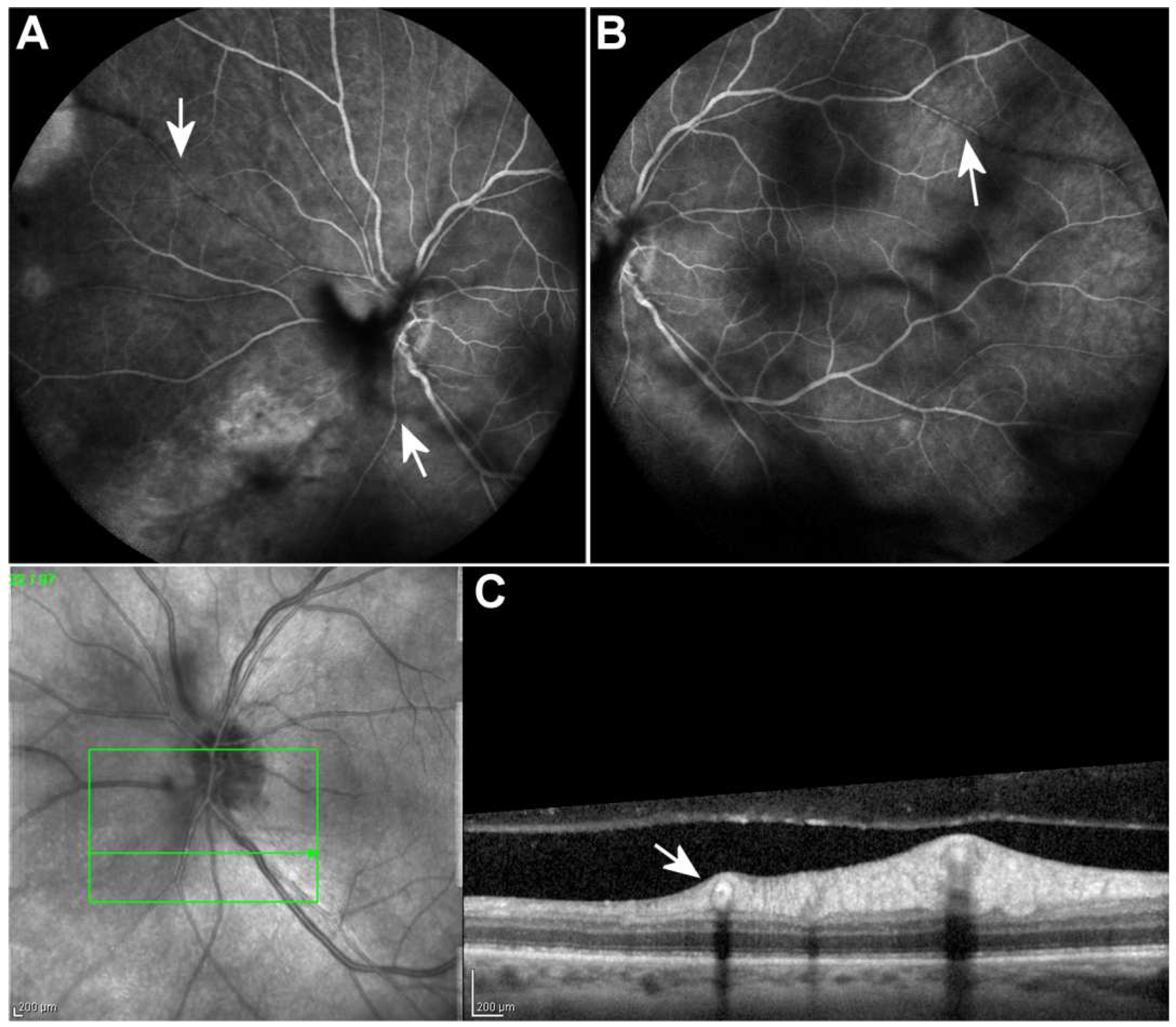
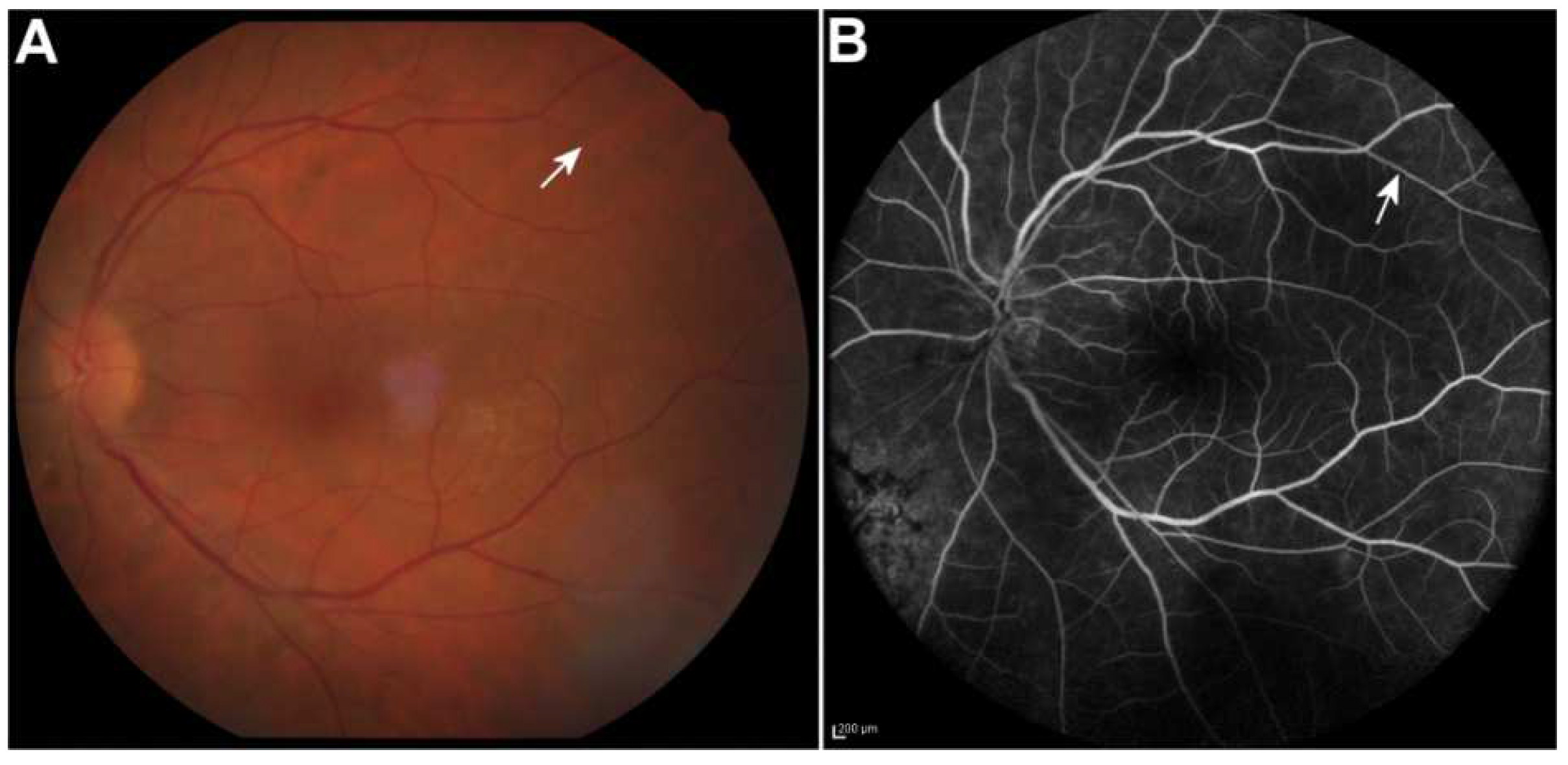
2. Case Report
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Holland, G.N.; Executive Committee of the American Uveitis Society. Standard diagnostic criteria for the acute retinal necrosis syndrome. Am. J. Ophthalmol. 1994, 117, 663–667. [Google Scholar] [CrossRef]
- Shantha, J.G.; Weissman, H.M.; Debiec, M.R.; Albini, T.A.; Yeh, S. Advances in the Management of Acute Retinal Necrosis. Int. Ophthalmol. Clin. 2015, 55, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.-Y.; Li, M.-D.; Ye, J.-J.; Zhao, C.; Hu, Y.-T.; Di, Y. Varicella-zoster virus as a causative agent of acute retinal necrosis in younger patients. Chin. Med. J. Engl. 2019, 132, 659–663. [Google Scholar] [CrossRef] [PubMed]
- Lau, C.H.; Missoten, T.; Salzmann, J.; Lightman, S.L. Acute retinal necrosis features, management, and outcomes. Ophthalmology 2007, 114, 756–762. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, M.J.; Venkatesan, A. Herpes Simplex Virus-1 Encephalitis in Adults: Pathophysiology, Diagnosis, and Management. Neurotherapeutics 2016, 13, 493–508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kennedy, P.G.E.; Chaudhuri, A. Herpes simplex encephalitis. J. Neurol. Neurosurg. Psychiatry 2002, 73, 237–238. [Google Scholar] [CrossRef] [PubMed]
- Kianersi, F.; Masjedi, A.; Ghanbari, H. Acute Retinal Necrosis after Herpetic Encephalitis. Case Rep. Ophthalmol. 2010, 1, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Witmer, M.T.; Levy-Clarke, G.A.; Fouraker, B.D.; Madow, B. Kyrieleis plaques associated with acute retinal necrosis from herpes simplex virus type 2. Retin. Cases Brief Rep. 2011, 5, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Pichi, P.; Veronese, C.; Lembo, A.; Invernizzi, A.; Mantovani, A.; Herbort, C.P.; Cunningham, E.T., Jr.; Morara, M.; Ricci, F.; Neri, P.; et al. New appraisals of Kyrieleis plaques: A multimodal imaging study. Br. J. Ophthalmol. 2017, 101, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Francés-Muñoz, E.; Gallego-Pinazo, R.; López-Lizcano, R.; García-Delpech, S.; Mullor, J.L.; Díaz-Llopis, M. Kyrieleis’ vasculitis in acute retinal necrosis. Clin. Ophthalmol. 2010, 4, 837–838. [Google Scholar] [PubMed] [Green Version]
- Patel, A.; Pomykala, M.; Mukkamala, K.; Gentile, R.C. Kyrieleis plaques in cytomegalovirus retinitis. J. Ophthalmic Inflamm. Infect. 2011, 1, 189–191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chazalon, É.; Conrath, J.; Ridings, B.; Matonti, F. Artérite de Kyrieleis: Présentation de deux cas et revue de la littérature. J. Fr. Ophtalmol. 2013, 36, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Empeslidis, T.; Konidaris, V.; Brent, A.; Vardarinos, A.; Deane, J. Kyrieleis plaques in herpes zoster virus-associated acute retinal necrosis: A case report. Eye 2013, 27, 1110–1112. [Google Scholar] [CrossRef] [PubMed]
- Villena-Irigoyen, O.; Echevarría-Lucas, L.; Castro-Gómez, M.; Bellido-Muñoz, R.M. Bilateral acute retinal necrosis due to varicella zoster virus in an elderly patient. Arch. Soc. Esp. Oftalmol. 2015, 90, 549–553. [Google Scholar] [CrossRef] [PubMed]
- Goel, N.; Sawhney, A. Kyrieleis plaques associated with Herpes Simplex Virus type 1 acute retinal necrosis. Saudi J. Ophthalmol. 2016, 30, 144–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chawla, R.; Tripathy, K.; Sharma, Y.R.; Venkatesh, P.; Vohra, R. Periarterial Plaques (Kyrieleis’ Arteriolitis) in a Case of Bilateral Acute Retinal Necrosis. Semin. Ophthalmol. 2017, 32, 251–252. [Google Scholar] [CrossRef] [PubMed]
- Ning, B.K.; Kelly, S.P.; Chu, C.; Morgan, E. Sequential retinal necrosis secondary to varicella zoster in unrecognised long-standing HIV infection: Patient safety report. BMJ Case Rep. 2018, 2018, bcr-2017-222237. [Google Scholar] [CrossRef] [PubMed]
- Kaza, H.; Patel, A.; Pathengay, A. Persistence of Kyrieleis arteriolitis in bilateral acute retinal necrosis. Indian J. Ophthalmol. 2020, 68, 1974. [Google Scholar] [CrossRef] [PubMed]
| Patient: 52-year-old Caucasian female |
| Chief complaint and duration: 3-day history of blurred vision, redness, floaters and photophobia in OS |
| Previous ocular history: Unremarkable |
| Previous medical history: Herpes simplex virus-1 encephalitis 4 months ago |
| Best corrected visual acuity: OD: 20/20 OS: 20/33 |
| Anterior segment examination: OD: unremarkable OS: dilated ciliary blood vessels and intense anterior chamber activity |
| Dilated fundus examination: OD: unremarkable OS: prominent vitritis, coalescing areas of peripheral retinal necrosis from2 o’clock over 6 o’clock to 10 o’clock without involvement of the posterior pole and mild optic disk edema |
| Case Report and Year of Publication | Causative Viral Agent | Patient’s Age/Gender | Eye(s) with ARN and KA | Time between Diagnosis of ARN and Observation of KA |
|---|---|---|---|---|
| Francés-Muñoz et al. [10] (2010) | VZV | 76/Female | OU | 2 weeks |
| Witmer et al. [8] (2011) | HSV-2 | 19/Female | OS | 6.5 weeks |
| Empeslidis et al. [13] (2013) | VZV | 56/Male | OS | KA present at diagnosis of ARN |
| Villena-Irigoyen et al. [14] (2015) | VZV | 77/Male | ARN: OU KA: OS | 4 weeks |
| Goel et al. [15] (2016) | HSV-1 | 55/Male | OS | 1 week |
| Chawla et al. [16] (2017) | VZV | 43/Male | ARN: OU KA: OD | Unknown (diagnosis of ARN and description of KA made by different medical teams) |
| Ning et al. [17] (2018) | VZV | Age not specified/Female | OD | KA present at diagnosis of ARN |
| Kaza et al. [18] (2020) | Not specified | 36/Male | OU | KA present at diagnosis of ARN |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makri, O.E.; Tsekouras, I.K.; Leonidou, L.; Kagkelaris, K.; Kozobolis, V.; Georgakopoulos, C.D. Kyrieleis Arteriolitis Associated with Acute Retinal Necrosis Due to Herpes Simplex Virus Type 1 Secondary to Herpetic Encephalitis. Vision 2022, 6, 27. https://doi.org/10.3390/vision6020027
Makri OE, Tsekouras IK, Leonidou L, Kagkelaris K, Kozobolis V, Georgakopoulos CD. Kyrieleis Arteriolitis Associated with Acute Retinal Necrosis Due to Herpes Simplex Virus Type 1 Secondary to Herpetic Encephalitis. Vision. 2022; 6(2):27. https://doi.org/10.3390/vision6020027
Chicago/Turabian StyleMakri, Olga E., Iasonas K. Tsekouras, Leonidia Leonidou, Konstantinos Kagkelaris, Vassilios Kozobolis, and Constantinos D. Georgakopoulos. 2022. "Kyrieleis Arteriolitis Associated with Acute Retinal Necrosis Due to Herpes Simplex Virus Type 1 Secondary to Herpetic Encephalitis" Vision 6, no. 2: 27. https://doi.org/10.3390/vision6020027
APA StyleMakri, O. E., Tsekouras, I. K., Leonidou, L., Kagkelaris, K., Kozobolis, V., & Georgakopoulos, C. D. (2022). Kyrieleis Arteriolitis Associated with Acute Retinal Necrosis Due to Herpes Simplex Virus Type 1 Secondary to Herpetic Encephalitis. Vision, 6(2), 27. https://doi.org/10.3390/vision6020027






