A Review of Depth of Focus in Measurement of the Amplitude of Accommodation
Abstract
1. Introduction
 and
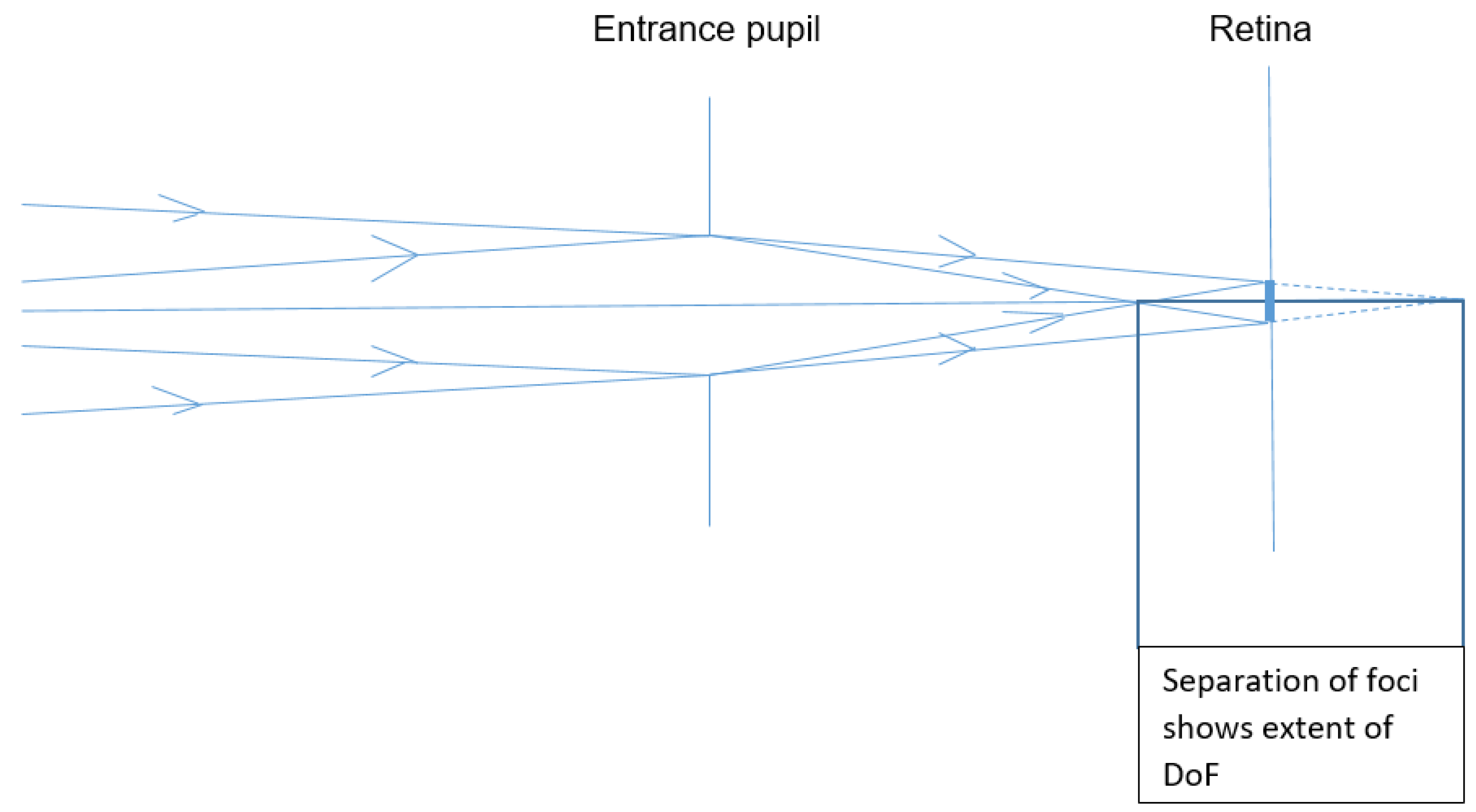
and  of differing vergences, which both form the same blur circle of diameter
of differing vergences, which both form the same blur circle of diameter  on the retina. If the blur circle is small enough for the observer to ignore, the depth of focus will be the difference between the two vergences at the entrance pupil.
on the retina. If the blur circle is small enough for the observer to ignore, the depth of focus will be the difference between the two vergences at the entrance pupil.- Inherent imprecision in image formation, due to diffraction and aberration as explained by Lipson et al. [2]
- Non-inherent imprecision of focussing, due to suboptimal production of the physical elements of the focussing system
- Limitations to the detection of blur, as discussed by Wang and Ciuffreda [3].
2. Factors Influencing the Effect of DoF on the Measurement of AoA
3. Research Showing that DoF Affects Measurement of AoA
4. Effect of the Method of Measurement
5. Reduction of the Error Due to DoF in AoA Measurement
6. Conclusions
Funding
Conflicts of Interest
References
- Charman, W.M. Forming an optical image: The optical elements of the eye. In Optometry: Science, Techniques and Clinical Management, 2nd ed.; Rosenfield, M., Logan, N., Edwards, K., Eds.; Elsevier: Edinburgh, UK, 2009; p. 11. [Google Scholar]
- Lipson, S.; Lipson, A.; Lipson, H. Optical Physics, 4th ed.; Cambridge University Press: Cambridge, UK, 2010; p. 38. [Google Scholar]
- Wang, B.; Ciuffreda, K.J. Depth-of-focus of the human eye: Theory and clinical implications. Surv. Ophthalmol. 2006, 51, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Atchison, D.A.; Charman, W.M.; Woods, R.L. Subjective depth of focus of the eye. Optom. Vis. Sci. 1997, 74, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Campbell, F. The depth of focus of the human eye. J. Physiol. 1954, 125, 29–30. [Google Scholar] [PubMed]
- Tucker, J.; Charman, W.N. The depth of focus of the human eye for Snellen letters. Am. J. Optom. Physiol. Opt. 1975, 52, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Cufflin, M.P.; Mankowska, A.; Mallen, E.A. Effect of blur adaptation on blur sensitivity and discrimination in emmetropes and myopes. Invest. Ophthalmol. Vis. Sci. 2007, 48, 2932–2939. [Google Scholar] [CrossRef] [PubMed]
- General Optical Council. Optometry Core Competencies (Stage 1). Available online: https://www.optical.org/en/Education/core-competencies--core-curricula/index.cfm (accessed on 24 August 2018).
- College of Optometrists. The Routine Eye Examination. Available online: http://guidance.college-optometrists.org/guidance-contents/advanced-search/?searchterm=a42 (accessed on 24 August 2018).
- Donders, F.; Moore, W.D. On the Anomalies of the Accommodation and Refraction of the Eye: With a Preliminary Essay on Physiological Dioptrics; The New Sydenham Society: London, UK, 1864; pp. 207–209.
- Burns, D.H.; Evans, B.J.W.; Allen, P.M. Clinical measurement of amplitude of accommodation: A review. OiP 2014, 15, 75–86. [Google Scholar]
- Rosenfield, M.; Cohen, A.S. Push-up amplitude of accommodation and target size. Ophthalmic Physiol. Opt. 1995, 15, 231–232. [Google Scholar] [CrossRef]
- Kragha, I.K. Amplitude of accommodation: Population and methodological differences. Ophthalmic Physiol. Opt. 1986, 6, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Turner, M.J. Observations on the normal subjective amplitude of accommodation. Br. J. Physiol. Opt. 1958, 15, 70–100. [Google Scholar] [PubMed]
- Atchison, D.A.; Capper, E.J.; McCabe, K.L. Critical subjective measurement of amplitude of accommodation. Optom. Vis. Sci. 1994, 71, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, S. Geometrical and Visual Optics, 2nd ed.; McGraw-Hill: London, UK, 2013; pp. 171–172. [Google Scholar]
- Winn, B.; Whitaker, D.; Elliott, D.B.; Phillips, N.J. Factors affecting light-adapted pupil size in normal human subjects. Invest. Ophthalmol. Vis. Sci. 1994, 35, 1132–1137. [Google Scholar] [PubMed]
- Marg, E.; Morgan, M.W. The pupillary near reflex; the relation of pupillary diameter to accommodation and the various components of convergence. J. Optom. Arch. Am. Acad. Optom. 1949, 26, 183–198. [Google Scholar] [CrossRef]
- Peavler, W.S. Pupil size, information overload and performance differences. Psychophysiology 1974, 11, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Gilzenrat, M.S.; Nieuwenhuis, S.; Jepma, M.; Cohen, J.D. Pupil diameter tracks changes in control state predicted by the adaptive gain theory of locus coeruleus function. Cogn. Affect. Behav. Neurosci. 2010, 10, 252–269. [Google Scholar] [CrossRef] [PubMed]
- Rabbetts, B.R.; Bennett, A.G. Clinical Visual Optics, 4th ed.; Butterworth-Heinemann: Oxford, UK, 2007; pp. 128–131. [Google Scholar]
- Rosenfield, M. Clinical Assessment of Accommodation. In Optometry: Science, Techniques and Clinical Management, 2nd ed.; Rosenfield, M., Logan, N., Edwards, K., Eds.; Elsevier: Edinburgh, UK, 2009; pp. 230–232. [Google Scholar]
- Scheiman, M.; Wick, B. Clinical Management of Binocular Vision, 1st ed.; Lippincott: Philadelphia, PA, USA, 1994; p. 20. [Google Scholar]
- Barrett, B.T. Assessment of Binocular Vision and Accommodation. In Clinical procedures in Primary Eye Care, 4th ed.; Elliott, D., Ed.; Butterworth-Heinemann Elsevier: Oxford, UK, 2013; pp. 178–181. [Google Scholar]
- Wagstaff, D. The objective measurement of the amplitude of accommodation-Part 4. Optician 1966, 151, 213–215. [Google Scholar]
- Hamasaki, D.; Ong, J.; Marg, E. The amplitude of accommodation in presbyopia. Optom. Vis. Sci. 1956, 33, 3–14. [Google Scholar] [CrossRef]
- Lancaster, W.B. Stigmatoscopy. Trans. Am. Ophthalmol. Soc. 1934, 32, 130–142. [Google Scholar] [PubMed]
- Charman, W.N. The path to presbyopia: Straight or crooked? Ophthalmic Physiol. Opt. 1989, 9, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.C.; Stark, L.; Nguyen, A.; Wong, J.; Lakshminarayanan, V.; Mueller, E. Changes in accommodation with age: Static and dynamic. Am. J. Optom. Physiol. Opt. 1988, 65, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Wagstaff, D. The objective measurement of the amplitude of accommodation-Part 8. Optician 1966, 151, 486–490. [Google Scholar]
- Duane, A. Studies in monocular and binocular accommodation with their clinical applications. Am. J. Ophthalmol. 1922, 5, 865–877. [Google Scholar] [CrossRef]
- Sergienko, N.M.; Nikonenko, D.P. Measurement of amplitude of accommodation in young persons. Clin. Exp. Optom. 2015, 98, 359–361. [Google Scholar] [CrossRef] [PubMed]
- Benzoni, J.A.; Rosenfield, M. Clinical amplitude of accommodation in children between 5 and 10 years of age. Optom. Vis. Dev. 2012, 43, 109–114. [Google Scholar]
- Wolf, A.V.; Hodge, H.C. Effects of atropine sulphate, methylatropine nitrate (metropine) and homatropine hydrobromide on adult human eyes. Arch. Ophthalmol. 1946, 36, 293–301. [Google Scholar] [CrossRef]
- Nayak, B.K.; Ghose, S.; Singh, J.P. A comparison of cycloplegic and manifest refractions on the NR-100OF (an objective Auto Refractometer). Br. J. Ophthalmol. 1987, 71, 73–75. [Google Scholar] [CrossRef] [PubMed]
- Woehrle, M.; Peters, R.; Frantz, K. Accommodative amplitude determination: Can we substitute the pull-away for the push-up method? Optom. Vis. Dev. 1997, 28, 246–249. [Google Scholar]
- Leon, A.; Estrada, J.M.; Rosenfield, M. Age and the amplitude of accommodation measured using dynamic retinoscopy. Ophthalmic Physiol. Opt. 2016, 36, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Antona, B.; Barra, F.; Barrio, A.; Gonzales, E.; Sanchez, I. Repeatability intraexaminer and agreement in amplitude of accommodation measurements. Graefe’s Arch. Clin. Exp. Ophthalmol. 2009, 247, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Wold, R.M. The spectacle amplitude of accommodation of children aged six to ten. Am. J. Optom. Arch. Am. Acad. Optom. 1967, 44, 642–664. [Google Scholar] [CrossRef] [PubMed]
- Ostrin, L.A.; Glasser, A. Accommodation measurements in a prepresbyopic and presbyopic population. J. Cataract Refract. Surg. 2014, 30, 1435–1444. [Google Scholar] [CrossRef] [PubMed]
- Sterner, B.; Gellerstedt, M.; Anders, S. The amplitude of accommodation in 6–10-year-old children–not as good as expected! Ophthalmic Physiol. Opt. 2004, 24, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Adler, P.; Scally, A.J.; Barrett, B.T. Test–retest reproducibility of accommodation measurements gathered in an unselected sample of UK primary school children. Br. J. Ophthalmol. 2013, 97, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Jackson, E. Amplitude of accommodation at different periods of life. Cal. State J. Med. 1907, 5, 163–166. [Google Scholar] [PubMed]
- Berens, C.; Fonda, G. A Spanish-English accommodation and near-test card using photoreduced type. Am. J. Ophthalmol. 1950, 33, 1788–1792. [Google Scholar] [CrossRef]
- Somers, W.W.; Ford, C.A. Effect of relative distance magnification on the monocular amplitude of accommodation. Optom. Vis. Sci. 1983, 60, 920–924. [Google Scholar] [CrossRef]
- Stark, L.R.; Atchison, D.A. Subject instructions and methods of target presentation in accommodation research. Invest. Ophthalmol. Vis. Sci. 1994, 35, 528–537. [Google Scholar] [PubMed]
- Aldaba, M.; Otero, C.; Pujol, J.; Atchison, D.A. Does the Badal optometer stimulate accommodation accurately? Ophthalmic Physiol. Opt. 2017, 37, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, J. The Lindsay Accommodation Measure. Optician 1954, 127, 273–274. [Google Scholar]
- Hokoda, S.C.; Ciuffreda, K.J. Measurement of accommodative amplitude in amblyopia. Ophthalmic Physiol. Opt. 1982, 2, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Rosenfield, M.; Cohen, A.S. Repeatability of clinical measurements of the amplitude of accommodation. Ophthalmic Physiol. Opt. 1996, 16, 247–249. [Google Scholar] [CrossRef]
- Momeni-Moghaddam, H.; Wolffsohn, J.S.; Azimi, A.; Babaei-Malekkolaei, E. Effect of target distance on accommodative amplitude measured using the minus-lens technique. Clin. Exp. Optom. 2013, 97, 62–65. [Google Scholar] [CrossRef] [PubMed]
- Gwiazda, J.; Thorn, F.; Bauer, J.; Held, R. Myopic children show insufficient accommodative response to blur. Invest. Ophthalmol. Vis. Sci. 1993, 34, 690–694. [Google Scholar]
- Bernal-Molina, P.; Montés-Micó, R.; Legras, R.; López-Gil, N. Depth-of-field of the accommodating eye. Optom. Vis. Sci. 2014, 91, 1208–1214. [Google Scholar] [CrossRef] [PubMed]
- Allen, P.M.; O’Leary, D.J. Accommodation functions: Co-dependency and relation to refractive error. Vis. Res. 2006, 46, 491–505. [Google Scholar] [CrossRef] [PubMed]
| Study Ref | How the Study Reduced the DoF | n | Ratio of Results with Reduced DoF to Results with a Standard Push-Up Method without Reduced DoF, for a Range of Age Groups | ||||
|---|---|---|---|---|---|---|---|
| 0–17 | 18–31 | 32–40 | 41–50 | Over 51 | |||
| [15] | Reduced test-object subtense | 60 | 0.62 | 0.66 | 0.69 | 0.78 | |
| [26] | Stigmatoscopy | 106 | 0.24 | 0.10 | |||
| [38] | Minus lens method | 61 | 0.76 | ||||
| [39] | Minus lens method | 125 | 0.74 | ||||
| [39] | Retinoscopy | 125 | 0.87 | ||||
| [40] | Minus lens method | 31 | 0.60 | 0.40 | 0.36 | ||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burns, D.H.; Allen, P.M.; Edgar, D.F.; Evans, B.J.W. A Review of Depth of Focus in Measurement of the Amplitude of Accommodation. Vision 2018, 2, 37. https://doi.org/10.3390/vision2030037
Burns DH, Allen PM, Edgar DF, Evans BJW. A Review of Depth of Focus in Measurement of the Amplitude of Accommodation. Vision. 2018; 2(3):37. https://doi.org/10.3390/vision2030037
Chicago/Turabian StyleBurns, David H., Peter M. Allen, David F. Edgar, and Bruce J. W. Evans. 2018. "A Review of Depth of Focus in Measurement of the Amplitude of Accommodation" Vision 2, no. 3: 37. https://doi.org/10.3390/vision2030037
APA StyleBurns, D. H., Allen, P. M., Edgar, D. F., & Evans, B. J. W. (2018). A Review of Depth of Focus in Measurement of the Amplitude of Accommodation. Vision, 2(3), 37. https://doi.org/10.3390/vision2030037





