Male Army ROTC Cadets Fail to Meet Military Dietary Reference Intakes and Exhibit a High Prevalence of Low Energy Availability and Poor Sleep Quality
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Dietary Intake
2.3. Exercise Energy Expenditure
2.4. Body Composition
2.5. Energy Availability
2.6. Pittsburgh Sleep Quality Index
2.7. Statistical Analysis
3. Results
3.1. Participants
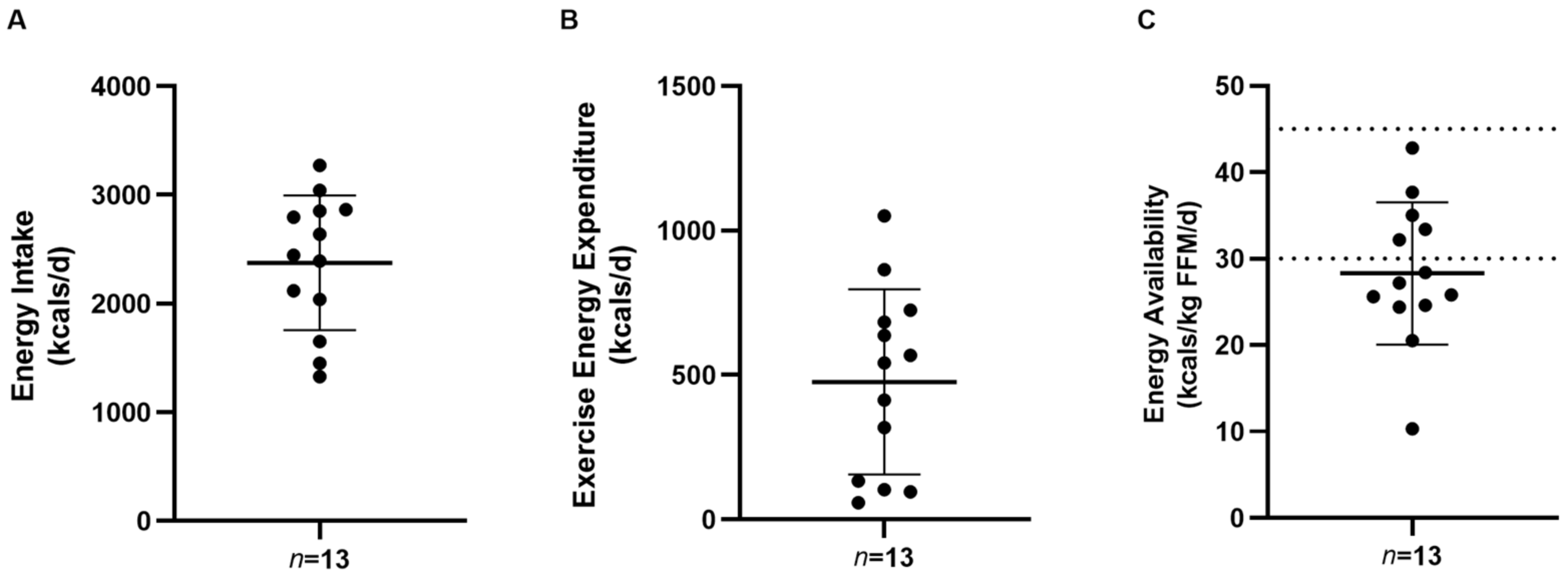
3.2. Energy Intake, Exercise Energy Expenditure, and Energy Availability Prevalence in Male Army ROTC Cadets
3.3. Energy and Macronutrient Intakes Relative to the Military Dietary Reference Intakes (MDRI) in Male Army ROTC Cadets
3.4. Energy and Macronutrient Intakes by EA Status in Male Army ROTC Cadets
3.5. Dietary Habits of Male Army ROTC Cadets
3.6. Sleep Quality of Male Army ROTC Cadets
3.7. Correlational Analyses
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Performance Triad Guide: Sleep, Activity, and Nutrition; The United States Army: Arlington County, VA, USA, 2015.
- Mountjoy, M.; Sundgot-Borgen, J.K.; Burke, L.M.; Ackerman, K.E.; Blauwet, C.; Constantini, N.; Lebrun, C.; Lundy, B.; Melin, A.K.; Meyer, N.L.; et al. IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update. Br. J. Sport Med. 2018, 52, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Melin, A.K.; Areta, J.L.; Heikura, I.A.; Stellingwerff, T.; Torstveit, M.K.; Hackney, A.C. Direct and indirect impact of low energy availability on sports performance. Scand. J. Med. Sci. Sport 2023, 14, 327. [Google Scholar] [CrossRef] [PubMed]
- Loucks, A. Exercise Training in the Normal Female: Effects of Low Energy Availability on Reproductive Function. In Endocrinology of Physical Activity and Sport; Humana Press: Totowa, NJ, USA, 2013; pp. 185–206. [Google Scholar] [CrossRef]
- Areta, J.L.; Taylor, H.L.; Koehler, K. Low energy availability: History, definition and evidence of its endocrine, metabolic and physiological effects in prospective studies in females and males. Eur. J. Appl. Physiol. 2021, 121, 1–21. [Google Scholar] [CrossRef]
- Melin, A.K.; Heikura, I.A.; Tenforde, A.; Mountjoy, M. Energy Availability in Athletics: Health, Performance, and Physique. Int. J. Sport Nutr. Exerc. Metab. 2019, 29, 152–164. [Google Scholar] [CrossRef] [PubMed]
- Beermann, B.L.; Lee, D.G.; Almstedt, H.C.; McCormack, W.P. Nutritional Intake and Energy Availability of Collegiate Distance Runners. J. Am. Coll. Nutr. 2020, 39, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Logue, D.M.; Madigan, S.M.; Melin, A.; Delahunt, E.; Heinen, M.; Donnell, S.M.; Corish, C.A. Low Energy Availability in Athletes 2020: An Updated Narrative Review of Prevalence, Risk, Within-Day Energy Balance, Knowledge, and Impact on Sports Performance. Nutrients 2020, 12, 835. [Google Scholar] [CrossRef] [PubMed]
- Magee, M.K.; Lockard, B.L.; Zabriskie, H.A.; Schaefer, A.Q.; Luedke, J.A.; Erickson, J.L.; Jones, M.T.; Jagim, A.R. Prevalence of Low Energy Availability in Collegiate Women Soccer Athletes. J. Funct. Morphol. Kinesiol. 2020, 5, 96. [Google Scholar] [CrossRef]
- Melin, A.; Tornberg, A.B.; Skouby, S.; Moller, S.S.; Sundgot-Borgen, J.; Faber, J.; Sidelmann, J.J.; Aziz, M.; Sjodin, A. Energy availability and the female athlete triad in elite endurance athletes. Scand. J. Med. Sci. Sport 2015, 25, 610–622. [Google Scholar] [CrossRef]
- Moss, S.L.; Randell, R.K.; Burgess, D.; Ridley, S.; ÓCairealláin, C.; Allison, R.; Rollo, I. Assessment of energy availability and associated risk factors in professional female soccer players. Eur. J. Sport Sci. 2021, 21, 861–870. [Google Scholar] [CrossRef]
- Reed, J.L.; De Souza, M.J.; Kindler, J.M.; Williams, N.I. Nutritional practices associated with low energy availability in Division I female soccer players. J. Sport Sci. 2014, 32, 1499–1509. [Google Scholar] [CrossRef]
- Mah, C.D.; Kezirian, E.J.; Marcello, B.M.; Dement, W.C. Poor sleep quality and insufficient sleep of a collegiate student-athlete population. Sleep Health 2018, 4, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Ritland, B.M.; Simonelli, G.; Gentili, R.J.; Smith, J.C.; He, X.; Oh, H.; Balkin, T.J.; Hatfield, B.D. Sleep health and its association with performance and motivation in tactical athletes enrolled in the Reserve Officers’ Training Corps. Sleep Health 2019, 5, 309–314. [Google Scholar] [CrossRef]
- Torres-McGehee, T.M.; Emerson, D.M.; Flanscha-Jacobson, A.; Uriegas, N.A.; Moore, E.M.; Smith, A.B. Examination of Energy Availability, Mental Health, and Sleep Patterns among Athletic Trainers. J. Athl. Train. 2023. [Google Scholar] [CrossRef]
- Loucks, A.B.; Kiens, B.; Wright, H.H. Energy availability in athletes. J. Sport Sci. 2011, 29 (Suppl. 1), S7–S15. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Evans, J.D. Straightforward Statistics for the Behavioral Sciences; Thomson Brooks/Cole Publishing Co., Ltd.: Belmont, CA, USA, 1996; p. 1750. [Google Scholar]
- Defense, D.O. (Ed.) Nutrition and Menu Standards for Human Performance Optimization; Defense; Department of Defense: Washington, DC, USA, 2017. [Google Scholar]
- Edwards, V.C.; Myers, S.D.; Wardle, S.L.; Siddall, A.G.; Powell, S.D.; Needham-Beck, S.; Kefyalew, S.S.; Singh, P.A.; Orford, E.R.; Venables, M.C.; et al. Nutrition and Physical Activity During British Army Officer Cadet Training: Part 1-Energy Balance and Energy Availability. Int. J. Sport Nutr. Exerc. Metab. 2022, 32, 195–203. [Google Scholar] [CrossRef]
- Nattiv, A.; De Souza, M.J.; Koltun, K.J.; Misra, M.; Kussman, A.; Williams, N.I.; Barrack, M.T.; Kraus, E.; Joy, E.; Fredericson, M. The Male Athlete Triad-A Consensus Statement From the Female and Male Athlete Triad Coalition Part 1: Definition and Scientific Basis. Clin. J. Sport Med. 2021, 31, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Position of the Academy of Nutrition and Dietetics, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and Athletic Performance. Can. J. Diet. Pract. Res. 2016, 77, 54. [CrossRef]
- Daniels, E.; Hanson, J. Energy-Adjusted Dietary Intakes Are Associated with Perceived Barriers to Healthy Eating but Not Food Insecurity or Sports Nutrition Knowledge in a Pilot Study of ROTC Cadets. Nutrients 2021, 13, 3053. [Google Scholar] [CrossRef]
- Lutz, L.J.; Gaffney-Stomberg, E.; Karl, J.P.; Hughes, J.M.; Guerriere, K.I.; McClung, J.P. Dietary Intake in Relation to Military Dietary Reference Values During Army Basic Combat Training; a Multi-center, Cross-sectional Study. Mil. Med. 2019, 184, e223–e230. [Google Scholar] [CrossRef] [PubMed]
- Petersen, H.L.; Peterson, C.T.; Reddy, M.B.; Hanson, K.B.; Swain, J.H.; Sharp, R.L.; Alekel, D.L. Body composition, dietary intake, and iron status of female collegiate swimmers and divers. Int. J. Sport Nutr. Exerc. Metab. 2006, 16, 281–295. [Google Scholar] [CrossRef]
- Viner, R.T.; Harris, M.; Berning, J.R.; Meyer, N.L. Energy Availability and Dietary Patterns of Adult Male and Female Competitive Cyclists With Lower Than Expected Bone Mineral Density. Int. J. Sport Nutr. Exerc. Metab. 2015, 25, 594–602. [Google Scholar] [CrossRef] [PubMed]
- Melin, A.; Tornberg, A.B.; Skouby, S.; Moller, S.S.; Faber, J.; Sundgot-Borgen, J.; Sjodin, A. Low-energy density and high fiber intake are dietary concerns in female endurance athletes. Scand. J. Med. Sci. Sport 2016, 26, 1060–1071. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, T.J.; Wardle, S.L.; Greeves, J.P. Energy Deficiency in Soldiers: The Risk of the Athlete Triad and Relative Energy Deficiency in Sport Syndromes in the Military. Front. Nutr. 2020, 7, 142. [Google Scholar] [CrossRef] [PubMed]
- Nindl, B.C.; Barnes, B.R.; Alemany, J.A.; Frykman, P.N.; Shippee, R.L.; Friedl, K.E. Physiological consequences of U.S. Army Ranger training. Med. Sci. Sport Exerc. 2007, 39, 1380–1387. [Google Scholar] [CrossRef]
- Margolis, L.M.; Murphy, N.E.; Martini, S.; Spitz, M.G.; Thrane, I.; McGraw, S.M.; Blatny, J.M.; Castellani, J.W.; Rood, J.C.; Young, A.J.; et al. Effects of winter military training on energy balance, whole-body protein balance, muscle damage, soreness, and physical performance. Appl. Physiol. Nutr. Metab. 2014, 39, 1395–1401. [Google Scholar] [CrossRef]
- Nindl, B.C.; Leone, C.D.; Tharion, W.J.; Johnson, R.F.; Castellani, J.W.; Patton, J.F.; Montain, S.J. Physical performance responses during 72 h of military operational stress. Med. Sci. Sport Exerc. 2002, 34, 1814–1822. [Google Scholar] [CrossRef]
- Keramidas, M.E.; Gadefors, M.; Nilsson, L.O.; Eiken, O. Physiological and psychological determinants of whole-body endurance exercise following short-term sustained operations with partial sleep deprivation. Eur. J. Appl. Physiol. 2018, 118, 1373–1384. [Google Scholar] [CrossRef]
- Murphy, N.E.; Carrigan, C.T.; Philip Karl, J.; Pasiakos, S.M.; Margolis, L.M. Threshold of Energy Deficit and Lower-Body Performance Declines in Military Personnel: A Meta-Regression. Sport Med. 2018, 48, 2169–2178. [Google Scholar] [CrossRef]
- Smith, A.; Emerson, D.; Winkelmann, Z.; Potter, D.; Torres-McGehee, T. Prevalence of Eating Disorder Risk and Body Image Dissatisfaction among ROTC Cadets. Int. J. Environ. Res. Public. Health 2020, 17, 8137. [Google Scholar] [CrossRef]
- Macdiarmid, J.; Blundell, J. Assessing dietary intake: Who, what and why of under-reporting. Nutr. Res. Rev. 1998, 11, 231–253. [Google Scholar] [CrossRef] [PubMed]
- Burrows, T.L.; Ho, Y.Y.; Rollo, M.E.; Collins, C.E. Validity of Dietary Assessment Methods When Compared to the Method of Doubly Labeled Water: A Systematic Review in Adults. Front. Endocrinol. 2019, 10, 850. [Google Scholar] [CrossRef]
- Jayne, J.M.; Karl, J.P.; McGraw, S.M.; O’Connor, K.; DiChiara, A.J.; Cole, R.E. Eating Behaviors Are Associated With Physical Fitness and Body Composition Among US Army Soldiers. J. Nutr. Educ. Behav. 2021, 53, 480–488. [Google Scholar] [CrossRef]
- Purvis, D.L.; Lentino, C.V.; Jackson, T.K.; Murphy, K.J.; Deuster, P.A. Nutrition as a component of the performance triad: How healthy eating behaviors contribute to soldier performance and military readiness. U. S. Army Med. Dep. J. 2013, 9, 66–78. [Google Scholar]
- Angus, R.G.; Heslegrave, R.J.; Myles, W.S. Effects of prolonged sleep deprivation, with and without chronic physical exercise, on mood and performance. Psychophysiology 1985, 22, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Walker, M.P.; Stickgold, R. Sleep-dependent learning and memory consolidation. Neuron 2004, 44, 121–133. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, K.; Leproult, R.; Van Cauter, E. Impact of sleep debt on metabolic and endocrine function. Lancet 1999, 354, 1435–1439. [Google Scholar] [CrossRef] [PubMed]
- Reilly, T.; Piercy, M. The effect of partial sleep deprivation on weight-lifting performance. Ergonomics 1994, 37, 107–115. [Google Scholar] [CrossRef]
- Martin, B.J. Effect of sleep deprivation on tolerance of prolonged exercise. Eur. J. Appl. Physiol. Occup. Physiol. 1981, 47, 345–354. [Google Scholar] [CrossRef]
- Knowles, O.E.; Drinkwater, E.J.; Urwin, C.S.; Lamon, S.; Aisbett, B. Inadequate sleep and muscle strength: Implications for resistance training. J. Sci. Med. Sport 2018, 21, 959–968. [Google Scholar] [CrossRef]
- Ritland, B.M.; Simonelli, G.; Gentili, R.J.; Smith, J.C.; He, X.; Mantua, J.; Balkin, T.J.; Hatfield, B.D. Effects of sleep extension on cognitive/motor performance and motivation in military tactical athletes. Sleep Med. 2019, 58, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Tarnowski, C.A.; Wardle, S.L.; O’Leary, T.J.; Gifford, R.M.; Greeves, J.P.; Wallis, G.A. Measurement of Energy Intake Using the Principle of Energy Balance Overcomes a Critical Limitation in the Assessment of Energy Availability. Sport Med. Open 2023, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Staal, S.; Sjodin, A.; Fahrenholtz, I.; Bonnesen, K.; Melin, A.K. Low RMR(ratio) as a Surrogate Marker for Energy Deficiency, the Choice of Predictive Equation Vital for Correctly Identifying Male and Female Ballet Dancers at Risk. Int. J. Sport Nutr. Exerc. Metab. 2018, 28, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Antonio, J.; Kenyon, M.; Ellerbroek, A.; Carson, C.; Burgess, V.; Tyler-Palmer, D.; Mike, J.; Roberts, J.; Angeli, G.; Peacock, C. Comparison of Dual-Energy X-ray Absorptiometry (DXA) Versus a Multi-Frequency Bioelectrical Impedance (InBody 770) Device for Body Composition Assessment after a 4-Week Hypoenergetic Diet. J. Funct. Morphol. Kinesiol. 2019, 4, 23. [Google Scholar] [CrossRef] [PubMed]
- Esco, M.R.; Snarr, R.L.; Leatherwood, M.D.; Chamberlain, N.A.; Redding, M.L.; Flatt, A.A.; Moon, J.R.; Williford, H.N. Comparison of total and segmental body composition using DXA and multifrequency bioimpedance in collegiate female athletes. J. Strength. Cond. Res. 2015, 29, 918–925. [Google Scholar] [CrossRef]

| Characteristic | Cadets (n = 13 Males) |
|---|---|
| Age (yrs.) | 22.2 ± 4.1 |
| Height (cm) | 179.6 ± 6.9 |
| Body mass (kg) | 84.2 ± 10.7 |
| BMI (kg/m2) | 26.1 ± 2.3 |
| FM (kg) | 17.1 ± 6.0 |
| %BF | 20.0 ± 6.0 |
| FFM (kg) | 67.2 ± 7.9 |
| SMM (kg) | 38.3 ± 4.7 |
| Low EA (n = 8) | Non-Low EA (n = 5) | |
|---|---|---|
| BM (kg) | 86.8 ± 11.2 | 80.2 ± 9.5 |
| FM (kg) | 19.6 ± 3.8 | 13.0 ± 7.0 * |
| %BF | 22.7 ± 3.9 | 15.7 ± 6.7 * |
| FFM (kg) | 67.2 ± 9.9 | 67.2 ± 3.8 |
| EEE (kcal/d) | 488.8 ± 324.6 | 456.1 ± 349.7 |
| Energy availability (kcal/kg FFM) | 23.3 ± 5.8 | 36.2 ± 4.2 *** |
| Energy intake (kcal/d) | 2059.6 ± 557.4 | 2880.6 ± 306.1 ** |
| Relative energy intake (kcal/kg/d) | 23.6 ± 4.9 | 36.1 ± 4.3 *** |
| Carbohydrate intake (g/d) | 257.6 ± 85.5 | 322.4 ± 33.7 * |
| Relative carbohydrate intake (g/kg/d) | 3.0 ± 0.9 | 4.1 ± 0.6 *** |
| Protein intake (g/d) | 102.6 ± 61.2 | 127.4 ± 25.6 |
| Relative protein intake (g/kg/d) | 1.1 ± 0.6 | 1.6 ± 0.5 |
| Fat intake (g/d) | 75.8 ± 30.8 | 112.0 ± 23.5 ^ |
| Relative fat intake (g/kg/d) | 0.9 ± 0.3 | 1.4 ± 0.3 ** |
| Fat intake (% kcals) | 33.5 ± 9.1 | 34.8 ± 5.7 |
| Meal | Reported Number | Kcals |
|---|---|---|
| Breakfast | 31 | 597.3 ± 389.1 |
| Breakfast skipped | 8 | |
| Lunch | 30 | 710.0 ± 555.3 |
| Lunch skipped | 9 | |
| Dinner | 38 | 794.4 ± 670.8 |
| Dinner skipped | 1 | |
| Snack | 2 | 101.6 ± 300.7 |
| Component | Range (Min, Max) | Score |
|---|---|---|
| Subjective sleep quality | (0, 2) | 1.1 ± 0.5 |
| Sleep latency | (0, 3) | 1.7 ± 1.1 |
| Sleep duration | (0, 3) | 1.4 ± 0.9 |
| Habitual sleep efficiency | (0, 1) | 0.5 ± 0.5 |
| Sleep disturbance | (0, 1) | 0.9 ± 0.3 |
| Use of sleeping medication | (0, 1) | 0.1 ± 0.3 |
| Daytime dysfunction | (1, 2) | 1.2 ± 0.4 |
| Global PSQI | (3, 11) | 6.8 ± 2.5 |
| Mean EA (kcal/kg FFM) | p-Value | Mean EI (kcal/d) | p-Value | |
|---|---|---|---|---|
| BM (kg) | −0.333 | 0.267 | −0.307 | 0.307 |
| %BF | −0.578 * | 0.039 | −0.610 * | 0.029 |
| FFM (kg) | −0.031 | 0.919 | 0.0399 | 0.897 |
| FM (kg) | −0.554 * | 0.049 | −0.602 * | 0.030 |
| SMM (kg) | −0.020 | 0.949 | 0.0396 | 0.897 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garron, T.; Klein, D.J. Male Army ROTC Cadets Fail to Meet Military Dietary Reference Intakes and Exhibit a High Prevalence of Low Energy Availability and Poor Sleep Quality. J. Funct. Morphol. Kinesiol. 2023, 8, 95. https://doi.org/10.3390/jfmk8030095
Garron T, Klein DJ. Male Army ROTC Cadets Fail to Meet Military Dietary Reference Intakes and Exhibit a High Prevalence of Low Energy Availability and Poor Sleep Quality. Journal of Functional Morphology and Kinesiology. 2023; 8(3):95. https://doi.org/10.3390/jfmk8030095
Chicago/Turabian StyleGarron, Taylor, and Dylan J. Klein. 2023. "Male Army ROTC Cadets Fail to Meet Military Dietary Reference Intakes and Exhibit a High Prevalence of Low Energy Availability and Poor Sleep Quality" Journal of Functional Morphology and Kinesiology 8, no. 3: 95. https://doi.org/10.3390/jfmk8030095
APA StyleGarron, T., & Klein, D. J. (2023). Male Army ROTC Cadets Fail to Meet Military Dietary Reference Intakes and Exhibit a High Prevalence of Low Energy Availability and Poor Sleep Quality. Journal of Functional Morphology and Kinesiology, 8(3), 95. https://doi.org/10.3390/jfmk8030095






