Psychological Wellbeing and Perceived Fatigue in Competitive Athletes after SARS-CoV-2 Infection 2 Years after Pandemic Start: Practical Indications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Procedures
2.4. Statistical Analysis
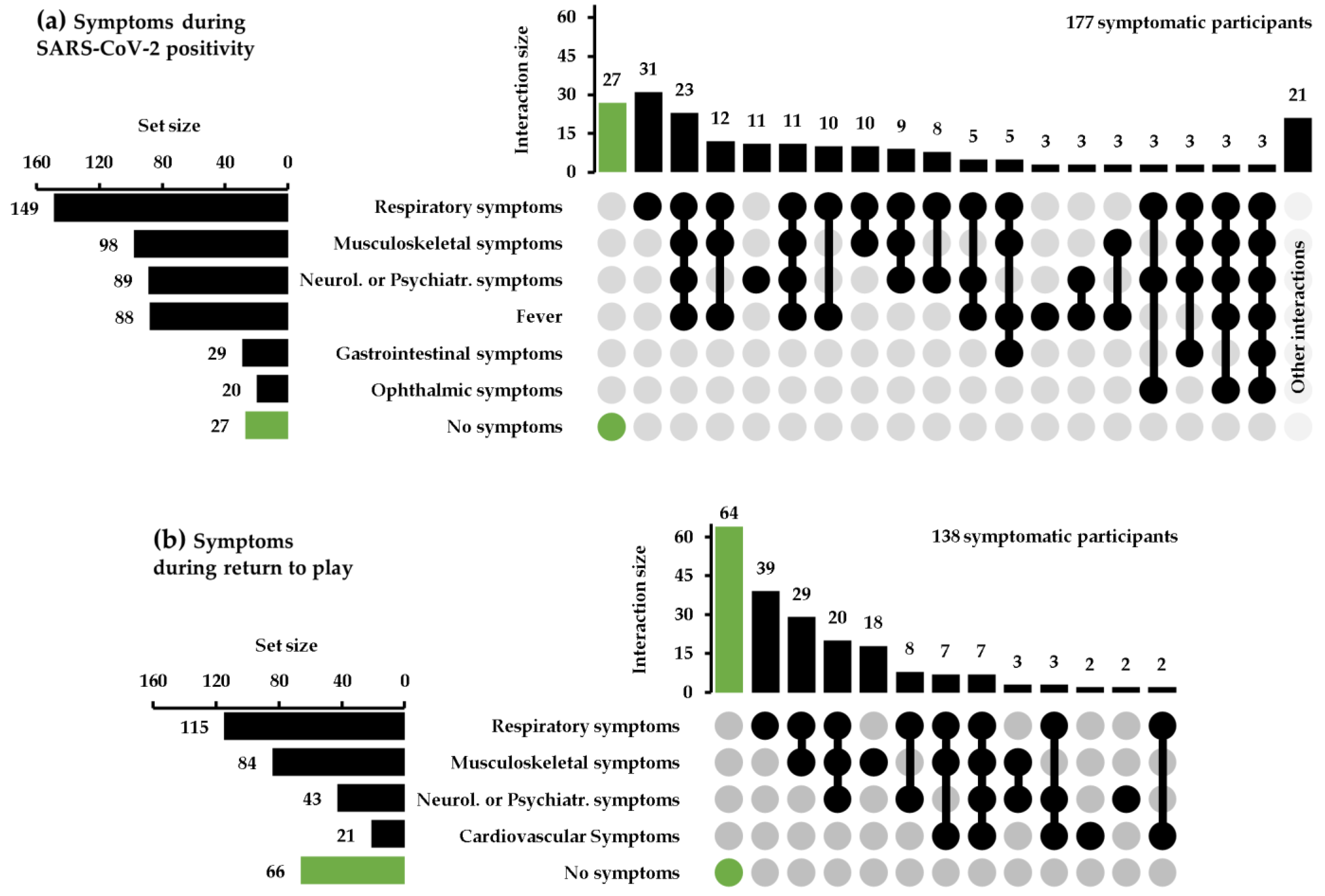
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vancini, R.L.; Borges Viana, R.; dos Santos Andrade, M.; Andre Barbosa de Lira, C.; Theodoros Nikolaidis, P.; Aparecido de Almeida, A.; Knechtle, B. YouTube as a Source of Information about Physical Exercise during COVID-19 Outbreak. Int. J. Sport. Stud. Health 2022, 4, e123312. [Google Scholar] [CrossRef]
- Sportesalute.eu—Un Anno di Pandemia: Gli Effetti del COVID-19 Sul Sistema Sportivo Italiano. Available online: https://www.sportesalute.eu/images/articoli/Un_anno_di_pandemia_impatto_su_ASD_SSD_Sport_e_Salute.pdf (accessed on 9 December 2022).
- Andreato, L.V.; Coimbra, D.R.; Andrade, A. Challenges to Athletes during the Home Confinement Caused by the COVID-19 Pandemic. Strength Cond. J. 2020, 42, 1–5. [Google Scholar] [CrossRef]
- Fiorilli, G.; Buonsenso, A.; Davola, N.; di Martino, G.; Baralla, F.; Boutious, S.; Centorbi, M.; Calcagno, G.; di Cagno, A. Stress Impact of COVID-19 Sports Restrictions on Disabled Athletes. Int. J. Environ. Res. Public Health 2021, 18, 12040. [Google Scholar] [CrossRef]
- di Cagno, A.; Buonsenso, A.; Baralla, F.; Grazioli, E.; di Martino, G.; Lecce, E.; Calcagno, G.; Fiorilli, G. Psychological Impact of the Quarantine-Induced Stress during the Coronavirus (COVID-19) Outbreak among Italian Athletes. Int. J. Environ. Res. Public Health 2020, 17, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Fiorilli, G.; Grazioli, E.; Buonsenso, A.; di Martino, G.; Despina, T.; Calcagno, G.; di Cagno, A. A National COVID-19 Quarantine Survey and Its Impact on the Italian Sports Community: Implications and Recommendations. PLoS ONE 2021, 16, e0248345. [Google Scholar] [CrossRef]
- Sheikh, A.; Kerr, S.; Woolhouse, M.; McMenamin, J.; Robertson, C.; Simpson, C.R.; Millington, T.; Shi, T.; Agrawal, U.; Shahul Hameed, S.; et al. Severity of Omicron Variant of Concern and Effectiveness of Vaccine Boosters against Symptomatic Disease in Scotland (EAVE II): A National Cohort Study with Nested Test-Negative Design. Lancet Infect. Dis. 2022, 22, 959–966. [Google Scholar] [CrossRef]
- Lauring, A.S.; Tenforde, M.W.; Chappell, J.D.; Gaglani, M.; Ginde, A.A.; Mcneal, T.; Ghamande, S.; Douin, D.J.; Talbot, H.K.; Casey, J.D.; et al. Clinical Severity of, and Effectiveness of MRNA Vaccines against, COVID-19 from Omicron, Delta, and Alpha SARS-CoV-2 Variants in the United States: Prospective Observational Study. Br. Med. J. 2022, 376, e069761. [Google Scholar] [CrossRef]
- Good, M.K.; Czarnik, M.; Harmon, K.G.; Aukerman, D.; O’Neal, C.S.; Day, C.; Goerl, K.; Sifre, K.; Fink, S.; Riggs, M.A. SARS-CoV-2 Infections and Reinfections among Fully Vaccinated and Unvaccinated University Athletes -15 States, January-November 2021. Clin. Infect. Dis. 2022, 75 (Suppl. S2), S236–S242. [Google Scholar] [CrossRef]
- Uroh, C.C.; Adewunmi, C.M. Psychological Impact of the COVID-19 Pandemic on Athletes. Front. Sports Act. Living 2021, 3, 603415. [Google Scholar] [CrossRef]
- Shi, H.; Han, X.; Jiang, N.; Cao, Y.; Alwalid, O.; Gu, J.; Fan, Y.; Zheng, C. Radiological Findings from 81 Patients with COVID-19 Pneumonia in Wuhan, China: A Descriptive Study. Lancet Infect. Dis. 2020, 20, 425–434. [Google Scholar] [CrossRef]
- Mahase, E. COVID-19: What do we know about “long covid”? Br. Med. J. 2020, 370, m2815. [Google Scholar] [CrossRef] [PubMed]
- Lemes, I.R.; Smaira, F.I.; Ribeiro, W.J.D.; Favero, N.K.; Matos, L.D.N.J.; Pinto, A.L.d.S.; Dolan, E.; Gualano, B. Acute and Post-Acute COVID-19 Presentations in Athletes: A Systematic Review and Meta-Analysis. Br. J. Sport. Med. 2022, 56, 941–947. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.G.; Hull, J.H.; Rogers, J.; Pollock, N.; Dodd, M.; Haines, J.; Harris, S.; Loosemore, M.; Malhotra, A.; Pieles, G.; et al. Cardiorespiratory Considerations for Return-to-Play in Elite Athletes after COVID-19 Infection: A Practical Guide for Sport and Exercise Medicine Physicians. Br. J. Sport. Med. 2020, 54, 1157–1161. [Google Scholar] [CrossRef] [PubMed]
- Alba-Jiménez, C.; Moreno-Doutres, D.; Peña, J. Trends Assessing Neuromuscular Fatigue in Team Sports: A Narrative Review. Sports 2022, 10, 33. [Google Scholar] [CrossRef]
- Ross, R.; Irvin, L.; Severin, R.; Ellis, B. Return-to-Play Considerations After COVID-19 Infection in Elite Athletes. J. Athl. Train. 2021, 56, 1061–1063. [Google Scholar] [CrossRef]
- Hull, J.H.; Wootten, M.; Moghal, M.; Heron, N.; Martin, R.; Walsted, E.S.; Biswas, A.; Loosemore, M.; Elliott, N.; Ranson, C. Clinical Patterns, Recovery Time and Prolonged Impact of COVID-19 Illness in International Athletes: The UK Experience. Br. J. Sport. Med. 2022, 56, 4–11. [Google Scholar] [CrossRef]
- Hughes, D.C.; Orchard, J.W.; Partridge, E.M.; la Gerche, A.; Broderick, C. Return to Exercise Post-COVID-19 Infection: A Pragmatic Approach in Mid-2022. J. Sci. Med. Sport. 2022, 544–547. [Google Scholar] [CrossRef]
- Boutios, S.; Fiorilli, G.; Buonsenso, A.; Daniilidis, P.; Centorbi, M.; Intrieri, M.; di Cagno, A. The Impact of Age, Gender and Technical Experience on Three Motor Coordination Skills in Children Practicing Taekwondo. Int. J. Environ. Res. Public Health 2021, 18, 5998. [Google Scholar] [CrossRef]
- Dal Monte, A. The Italian classification of different sports in relation to cardiovascular risk. In Arrhythmias and Sudden Death in Athletes, 1st ed.; Bayés Luna, A., Furlanello, F., Maron, B.J., Zipes, D.P., Eds.; Springer: Dordrecht, The Netherlands, 2000; pp. 11–24. [Google Scholar]
- Krupp, L.B.; LaRocca, N.G.; Muir-Nash, J.; Steinberg, A.D. The fatigue severity scale: Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 1989, 46, 1121–1123. [Google Scholar] [CrossRef]
- Goldberg, D.P. Manual of the General Health Questionnaire; NFER Publishing: Windsor, UK, 1978. [Google Scholar]
- Halper, J.; Holland, N.J. Multiple Sclerosis: A Self-Care Guide to Wellness, 2nd ed.; Demos Medical Publishing: New York, NY, USA, 2005. [Google Scholar]
- Goldberg, D.; Williams, P. A User’s Guide to the General Health Questionnaire; NFER-Nelson Publishing: Windsor, UK, 1988. [Google Scholar]
- Agha-Alinejad, H.; Hekmatikar, A.H.A.; Ruhee, R.T.; Shamsi, M.M.; Rahmati, M.; Khoramipour, K.; Suzuki, K. A Guide to Different Intensities of Exercise, Vaccination, and Sports Nutrition in the Course of Preparing Elite Athletes for the Management of Upper Respiratory Infections during the COVID-19 Pandemic: A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 1888. [Google Scholar] [CrossRef]
- Starekova, J.; Bluemke, D.A.; Bradham, W.S.; Eckhardt, L.L.; Grist, T.M.; Kusmirek, J.E.; Purtell, C.S.; Schiebler, M.L.; Reeder, S.B. Evaluation for Myocarditis in Competitive Student Athletes Recovering from Coronavirus Disease 2019 with Cardiac Magnetic Resonance Imaging. JAMA Cardiol. 2021, 6, 945–950. [Google Scholar] [CrossRef] [PubMed]
- Nieman, D.C.; Wentz, L.M. The Compelling Link between Physical Activity and the Body’s Defense System. J. Sport. Health Sci. 2019, 8, 201–217. [Google Scholar] [CrossRef]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological Findings of COVID-19 Associated with Acute Respiratory Distress Syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef] [PubMed]
- Ezzatvar, Y.; Ramirez-Velez, R.; Izquierdo, M.; Garcia-Hermoso, A. Physical Activity and Risk of Infection, Severity and Mortality of COVID-19: A Systematic Review and Non-Linear Dose-Response Meta-Analysis of Data from 1,853,610 Adults. Br. J. Sport. Med. 2022. [Google Scholar] [CrossRef] [PubMed]
- Udelson, J.E.; Rowin, E.J.; Maron, B.J. Return to Play for Athletes after COVID-19 Infection: The Fog Begins to Clear. JAMA Cardiol. 2021, 6, 997–999. [Google Scholar] [CrossRef] [PubMed]
- Efremidis, M.; Vlachos, K.; Kyriakopoulou, M.; Mililis, P.; Martin, C.A.; Bazoukis, G.; Dragasis, S.; Megarisiotou, A.; Unger, P.; Frontera, A.; et al. The RV1-V3 Transition Ratio: A Novel Electrocardiographic Criterion for the Differentiation of Right versus Left Outflow Tract Premature Ventricular Complexes. Heart Rhythm O2 2021, 2, 521–528. [Google Scholar] [CrossRef]
- Porcedda, G.; Brambilla, A.; Favilli, S.; Spaziani, G.; Mascia, G.; Giaccardi, M. Frequent Ventricular Premature Beats in Children and Adolescents: Natural History and Relationship with Sport Activity in a Long-Term Follow-Up. Pediatr. Cardiol. 2020, 41, 123–128. [Google Scholar] [CrossRef]
- Boraita, A.; Heras, M.E.; Valenzuela, P.L.; Diaz-Gonzalez, L.; Morales-Acuna, F.; Alcocer-Ayuga, M.; Bartolomé-Mateos, S.; Santos-Lozano, A.; Lucia, A. Holter-determined arrhythmias in young elite athletes with suspected risk: Insights from a 20-year experience. Front. Cardiovasc. Med. 2022, 9, 896148. [Google Scholar] [CrossRef]
- Saeed, U.; Sellevoll, H.B.; Young, V.S.; Sandbæk, G.; Glomsaker, T.; Mala, T. COVID-19 May Present with Acute Abdominal Pain. Br. J. Surg. 2020, 107, e186–e187. [Google Scholar] [CrossRef]
- Danthuluri, V.; Grant, M.B. Update and Recommendations for Ocular Manifestations of COVID-19 in Adults and Children: A Narrative Review. Ophthalmol. Ther. 2020, 853–875. [Google Scholar] [CrossRef]
- Venturelli, M.; Mancini, A.; di Cagno, A.; Fiorilli, G.; Paneroni, M.; Roggio, F.; Musumeci, G.; Buono, P.; Schena, F.; Paoli, A. Adapted Physical Activity in Subjects and Athletes Recovering from COVID-19: A Position Statement of the Società Italiana Scienze Motorie e Sportive. Sport. Sci. Health 2022, 18, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 Long-Term Effects of COVID-19: A Systematic Review and Meta-Analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, F.M.; Lam, K.; Sounderajah, V.; Clarke, J.M.; Ashrafian, H.; Darzi, A. Characteristics and Predictors of Acute and Chronic Post-COVID Syndrome: A Systematic Review and Meta-Analysis. EClinicalMedicine 2021, 36, 100899. [Google Scholar] [CrossRef]
- Doykov, I.; Hällqvist, J.; Gilmour, K.C.; Grandjean, L.; Mills, K.; Heywood, W.E. The Long Tail of COVID-19—The Detection of a Prolonged Inflammatory Response after a SARS-CoV-2 Infection in Asymptomatic and Mildly Affected Patients. F1000Research 2020, 9, 1349. [Google Scholar] [CrossRef]
- Amruta, N.; Rahman, A.A.; Pinteaux, E.; Bix, G. Neuroinflammation and Fibrosis in Stroke: The Good, the Bad and the Ugly. J. Neuroimmunol. 2020, 346, 577318. [Google Scholar] [CrossRef]
- Sahu, A.; Mathew, R.; Aggarwal, P.; Nayer, J.; Bhoi, S.; Satapathy, S.; Ekka, M. Clinical Determinants of Severe COVID-19 Disease—A Systematic Review and Meta-Analysis. J. Glob. Infect. Dis. 2021, 13, 13–19. [Google Scholar] [CrossRef]
- Peghin, M.; Palese, A.; Venturini, M.; de Martino, M.; Gerussi, V.; Graziano, E.; Bontempo, G.; Marrella, F.; Tommasini, A.; Fabris, M.; et al. Post-COVID-19 Symptoms 6 Months after Acute Infection among Hospitalized and Non-Hospitalized Patients. Clin. Microbiol. Infect. 2021, 27, 1507–1513. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Martín-Guerrero, J.D.; Pellicer-Valero, Ó.J.; Navarro-Pardo, E.; Gómez-Mayordomo, V.; Cuadrado, M.L.; Arias-Navalón, J.A.; Cigarán-Méndez, M.; Hernández-Barrera, V.; Arendt-Nielsen, L. Female Sex Is a Risk Factor Associated with Long-Term Post-COVID Related-Symptoms but Not with COVID-19 Symptoms: The LONG-COVID-EXP-CM Multicenter Study. J. Clin. Med. 2022, 11, 413. [Google Scholar] [CrossRef]
- Clarkson, B.G.; Culvin, A.; Pope, S.; Parry, K.D. COVID-19: Reflections on Threat and Uncertainty for the Future of Elite Women’s Football in England. Manag. Sport. Leis. 2022, 27, 44–55. [Google Scholar] [CrossRef]
- Slavin, L.E.; Palmateer, T.M.; Petrie, T.A.; Moore, E.W.G. Collegiate student-athlete psychological distress and counseling utilization during COVID-19. J. Clin. Sport. Psychol. 2022, 1, 1–14. [Google Scholar] [CrossRef]
- Hunter, S.K. Sex Differences in Human Fatigability: Mechanisms and Insight to Physiological Responses. Acta Physiol. 2014, 210, 768–789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keshkar, S.; Dickson, G.; Ahonen, A.; Swart, K.; Addesa, F.; Epstein, A.; Dodds, M.; Schwarz, E.C.; Spittle, S.; Wright, R.; et al. The Effects of Coronavirus Pandemic on the Sports Industry: An Update. Ann. Appl. Sport. Sci. 2021, 9, 1–23. [Google Scholar] [CrossRef]
- Salamanna, F.; Veronesi, F.; Martini, L.; Landini, M.P.; Fini, M. Post-COVID-19 Syndrome: The Persistent Symptoms at the Post-Viral Stage of the Disease. A Systematic Review of the Current Data. Front. Med. 2021, 8, 653516. [Google Scholar] [CrossRef] [PubMed]
- Nopp, S.; Moik, F.; Klok, F.A.; Gattinger, D.; Petrovic, M.; Vonbank, K.; Koczulla, A.R.; Ay, C.; Zwick, R.H. Outpatient Pulmonary Rehabilitation in Patients with Long COVID Improves Exercise Capacity, Functional Status, Dyspnea, Fatigue, and Quality of Life. Respiration 2022, 101, 593–601. [Google Scholar] [CrossRef]
- Evidence.nihr.ac.uk—Living with COVID-19, Second Review. Available online: https://evidence.nihr.ac.uk/wp-content/uploads/2021/03/NIHR_COVID_REPORT_FINAL-150321-1_1_.pdf (accessed on 9 December 2022).
- Simpson, R.J.; Campbell, J.P.; Gleeson, M.; Krüger, K.; Nieman, D.C.; Pyne, D.B.; Turner, J.E.; Walsh, N.P. Can exercise affect immune function to increase susceptibility to infection? Exerc. Immunol. Rev. 2020, 26, 8–22. [Google Scholar]
- Derman, W.; Badenhorst, M.; Eken, M.; Gomez-Ezeiza, J.; Fitzpatrick, J.; Gleeson, M.; Kunorozva, L.; Mjosund, K.; Mountjoy, M.; Sewry, N.; et al. Risk Factors Associated with Acute Respiratory Illnesses in Athletes: A Systematic Review by a Subgroup of the IOC Consensus on “Acute Respiratory Illness in the Athlete. Br. J. Sport. Med. 2022, 56, 639–650. [Google Scholar] [CrossRef]
- Salcinovic, B.; Drew, M.; Dijkstra, P.; Waddington, G.; Serpell, B.G. Factors Influencing Team Performance: What Can Support Teams in High-Performance Sport Learn from Other Industries? A Systematic Scoping Review. Sport. Med. 2022, 8, 25. [Google Scholar] [CrossRef]
- Chopra, V.; Flanders, S.A.; O’Malley, M.; Malani, A.N.; Prescott, H.C. Sixty-day outcomes among patients hospitalized with COVID-19. Ann. Intern. Med. 2021, 174, 576–578. [Google Scholar] [CrossRef]
- Martin, K.; Meeusen, R.; Thompson, K.G.; Keegan, R.; Rattray, B. Mental Fatigue Impairs Endurance Performance: A Physiological Explanation. Sports. Med. 2018, 2041–2051. [Google Scholar] [CrossRef]
- Boksem, M.A.S.; Meijman, T.F.; Lorist, M.M. Mental Fatigue, Motivation and Action Monitoring. Biol. Psychol. 2006, 72, 123–132. [Google Scholar] [CrossRef]
- Martin, K.; Thompson, K.G.; Keegan, R.; Ball, N.; Rattray, B. Mental Fatigue Does Not Affect Maximal Anaerobic Exercise Performance. Eur. J. Appl. Physiol. 2015, 115, 715–725. [Google Scholar] [CrossRef] [PubMed]
- Dergaa, I.; Ammar, A.; Souissi, A.; Fessi, M.S.; Trabelsi, K.; Glenn, J.M.; Ghram, A.; Taheri, M.; Irandoust, K.; Chtourou, H.; et al. COVID-19 lockdown: Impairments of objective measurements of selected physical activity, cardiorespiratory and sleep parameters in trained fitness coaches. EXCLI J. 2022, 21, 1084–1098. [Google Scholar] [CrossRef] [PubMed]
| Categories | Groups | n | Age (Years) | GHQ-12 Score | FSS Score |
|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | |||
| Gender | Males | 111 | 24 (21–28) 1 | 17 (15–18) 1 | 25 (15.5–35) 1 |
| Females | 93 | 22 (17–27) 1 | 17 (16–20) 1 | 34 (22–41) 1 | |
| Sport type | Individual | 106 | 23 (18–27) | 17 (15–19) | 27 (17.25–39) |
| Team | 98 | 24 (21–28) | 17 (15–19) | 28 (19–37) | |
| Metabolic demands | Aerobic | 48 | 23 (21–31) 2 | 17 (16–19.25) | 35 (21.75–39) 3 |
| Anaerobic | 95 | 24 (21–28) | 17 (15–19) | 26 (17–33) 3 | |
| Mixed | 61 | 21 (16–26) 2 | 17 (15–19) | 30 (19–40) | |
| Technical Level | Elite | 96 | 24 (19–29) | 17 (15–19) | 30.5 (19–40.25) |
| Sub-elite | 108 | 23 (20–27) | 17 (15–19) | 27 (18–35.25) | |
| COVID-19 variant | Delta | 75 | 24 (19.5–27) | 17 (15–19.5) | 30 (16.5–39.5) |
| Omicron | 129 | 23 (20–28) | 17 (15–19) | 27 (19–38) | |
| Severity of infection | Slight | 86 | 22 (17–26) | 17 (15–18) 4 | 26 (15–34) 4,6 |
| Moderate | 113 | 24 (21–28) | 17 (15–19) 5 | 31 (19–40) 6 | |
| Severe | 5 | 29 (25–57) | 21 (20–26) 4,5 | 45 (35–47) 4 | |
| Total number of participants | 204 | 23 (20–28) | 17 (15–19) | 27.5 (18–38) |
| Analysis | Dependent Variable | Significant Independent Variables Included by Analysis | r and Adjusted r2 Values | F-Value and p-Value |
|---|---|---|---|---|
| FSS score vs. symptoms that occurred during the infection | FSS score | Dyspnea, Fatigue, Respiratory failure | r = 0.463 r2 = 0.202 | F = 18.148 p < 0.001 |
| GHQ-12 score vs. symptoms that occurred during the infection | GHQ-12 score | Respiratory failure, Abdominal pain, Joint pain | r = 0.422 r2 = 0.165 | F = 14.418 p < 0.001 |
| FSS score vs. symptoms that occurred in return to play after infection | FSS score | Dyspnea, Joint pain, Dizziness | r = 0.594 r2 = 0.340 | F = 27.129 p < 0.001 |
| GHQ-12 score vs. symptoms that occurred in return to play after infection | GHQ-12 score | Cough, Muscle fatigue, Agitation, Dyspnea | r = 0.495 r2 = 0.230 | F = 16.133 p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buonsenso, A.; Murri, A.; Centorbi, M.; Di Martino, G.; Calcagno, G.; di Cagno, A.; Fiorilli, G.; Iuliano, E. Psychological Wellbeing and Perceived Fatigue in Competitive Athletes after SARS-CoV-2 Infection 2 Years after Pandemic Start: Practical Indications. J. Funct. Morphol. Kinesiol. 2023, 8, 1. https://doi.org/10.3390/jfmk8010001
Buonsenso A, Murri A, Centorbi M, Di Martino G, Calcagno G, di Cagno A, Fiorilli G, Iuliano E. Psychological Wellbeing and Perceived Fatigue in Competitive Athletes after SARS-CoV-2 Infection 2 Years after Pandemic Start: Practical Indications. Journal of Functional Morphology and Kinesiology. 2023; 8(1):1. https://doi.org/10.3390/jfmk8010001
Chicago/Turabian StyleBuonsenso, Andrea, Arianna Murri, Marco Centorbi, Giulia Di Martino, Giuseppe Calcagno, Alessandra di Cagno, Giovanni Fiorilli, and Enzo Iuliano. 2023. "Psychological Wellbeing and Perceived Fatigue in Competitive Athletes after SARS-CoV-2 Infection 2 Years after Pandemic Start: Practical Indications" Journal of Functional Morphology and Kinesiology 8, no. 1: 1. https://doi.org/10.3390/jfmk8010001













