COVID-19 Surveillance and Competition in Sport: Utilizing Sport Science to Protect Athletes and Staff during and after the Pandemic
Abstract
1. Introduction
2. Perspectives
2.1. COVID and Collegiate Strength and Conditioning (S&C): Insights from a Director of S&C at a Power 5 University
2.2. COVID and NFL Athletes: Insights from a Director of Player Performance in the NFL
3. Approach
4. Data Strategy
4.1. COVID-19-Specific Tracking
4.2. Performance Tracking
4.3. Dual-Purpose Tracking
5. Phases
5.1. Phase I: Quarantine
5.2. Phase II: Return to Facility
5.3. Phase III: Return to Strength and Conditioning
5.4. Phase IV: Return to Practice
5.5. Phase V: Return to Competition
6. Implementation of COVID-19 Sport Science Strategies
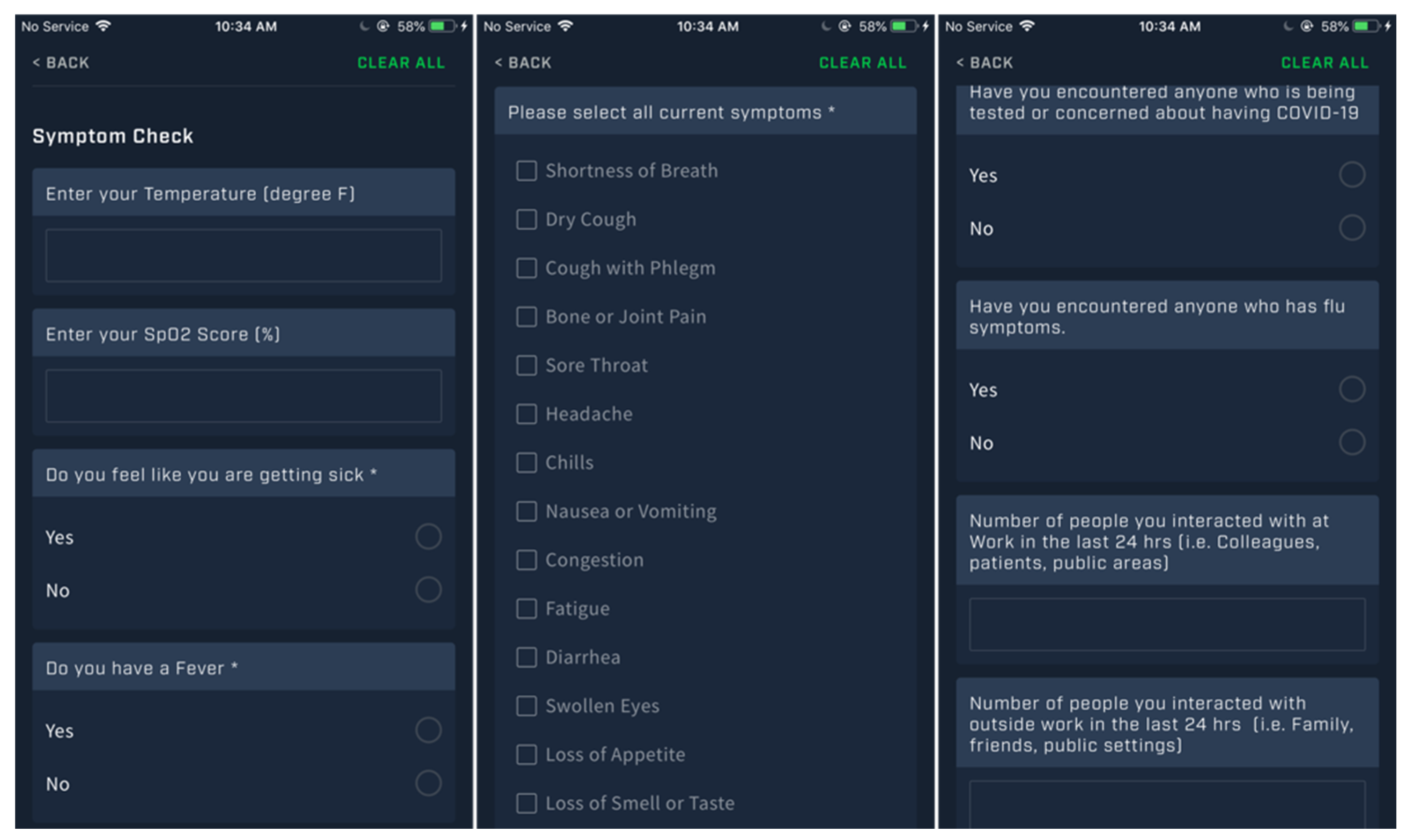
6.1. Measure: COVID-19 Symptom Tracking
6.2. Measure: Health and Wellness
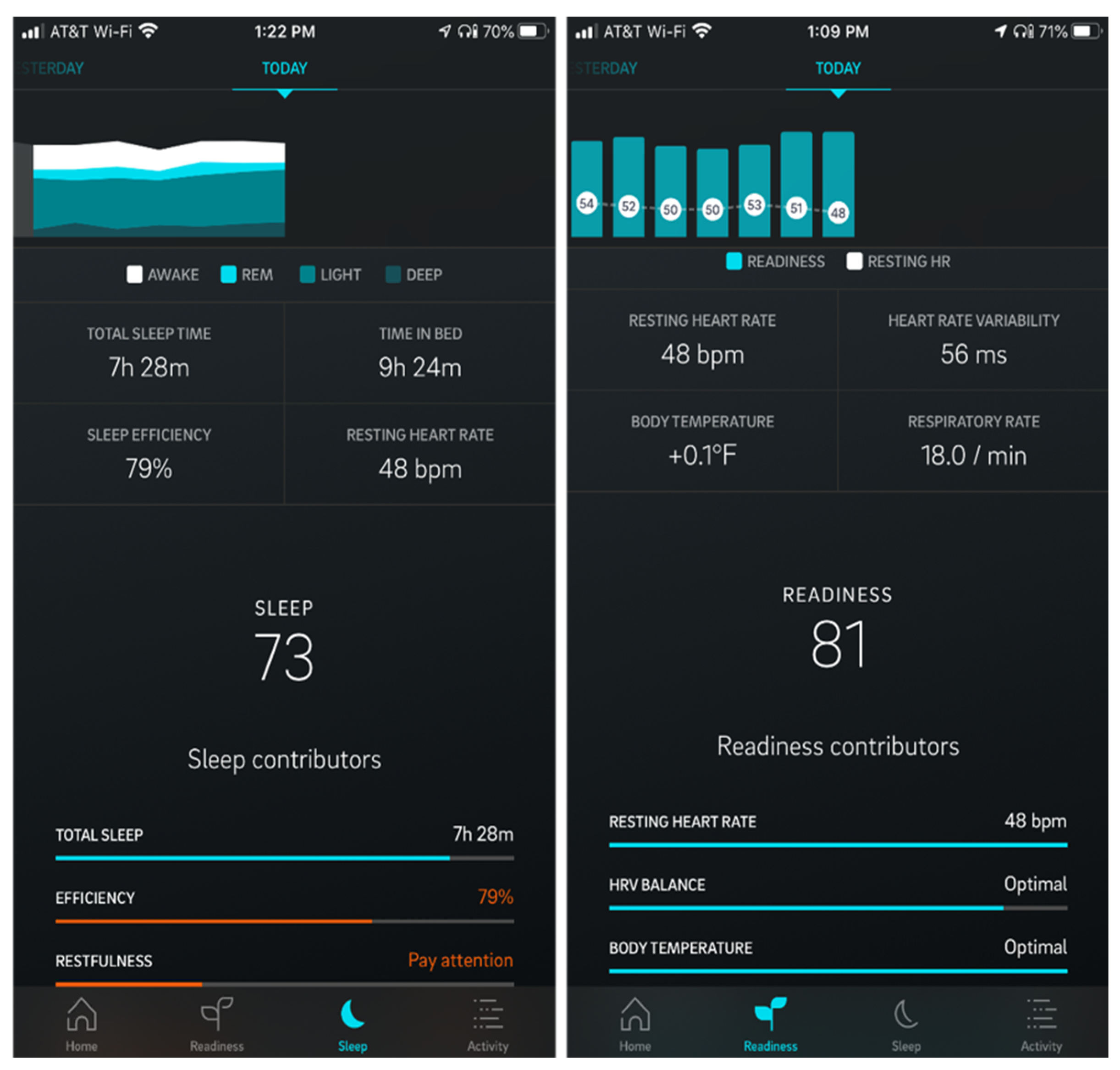
6.3. Measure: Sleep Behaviors and Sleep Physiology
6.4. Track: Data Approaches
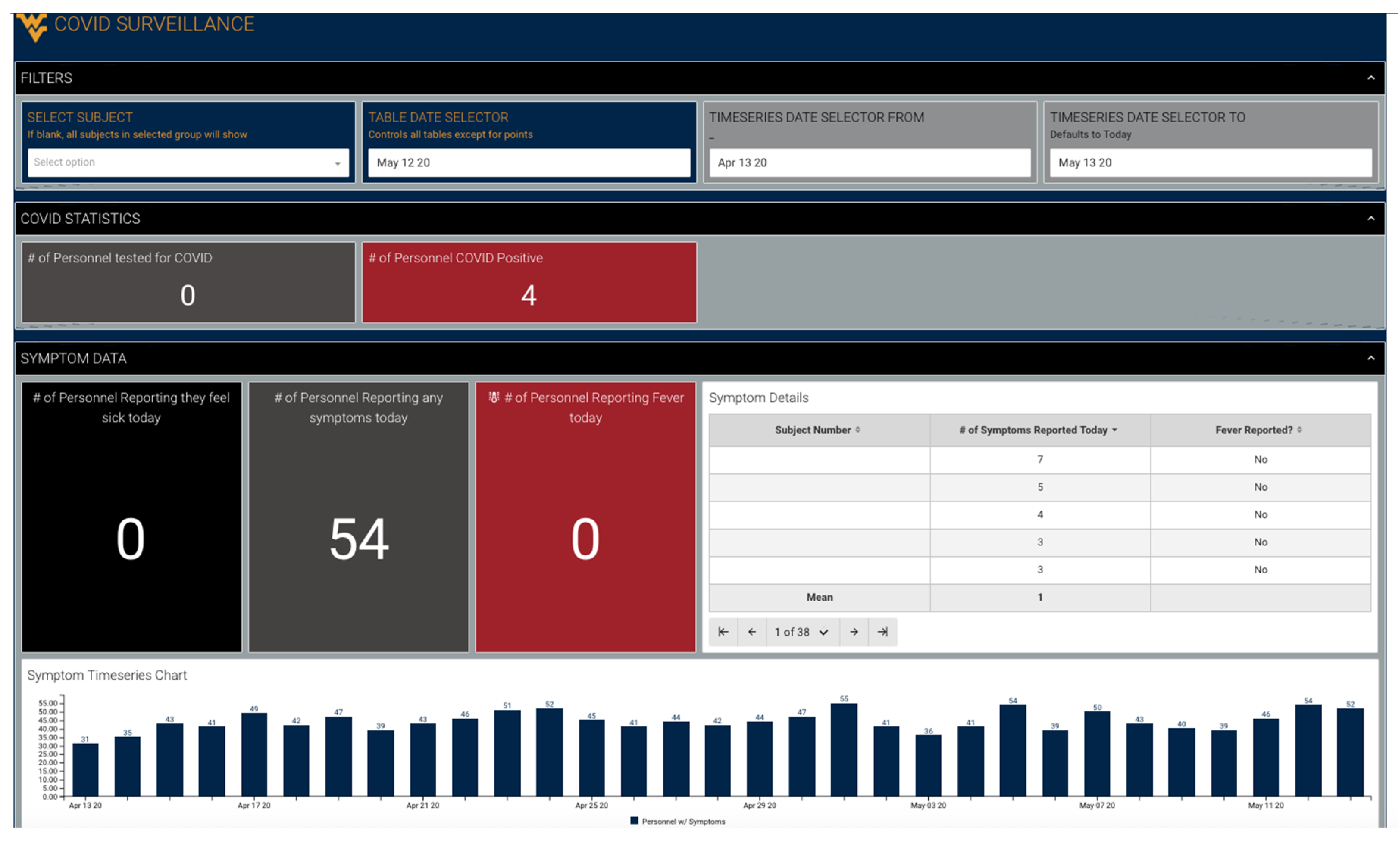
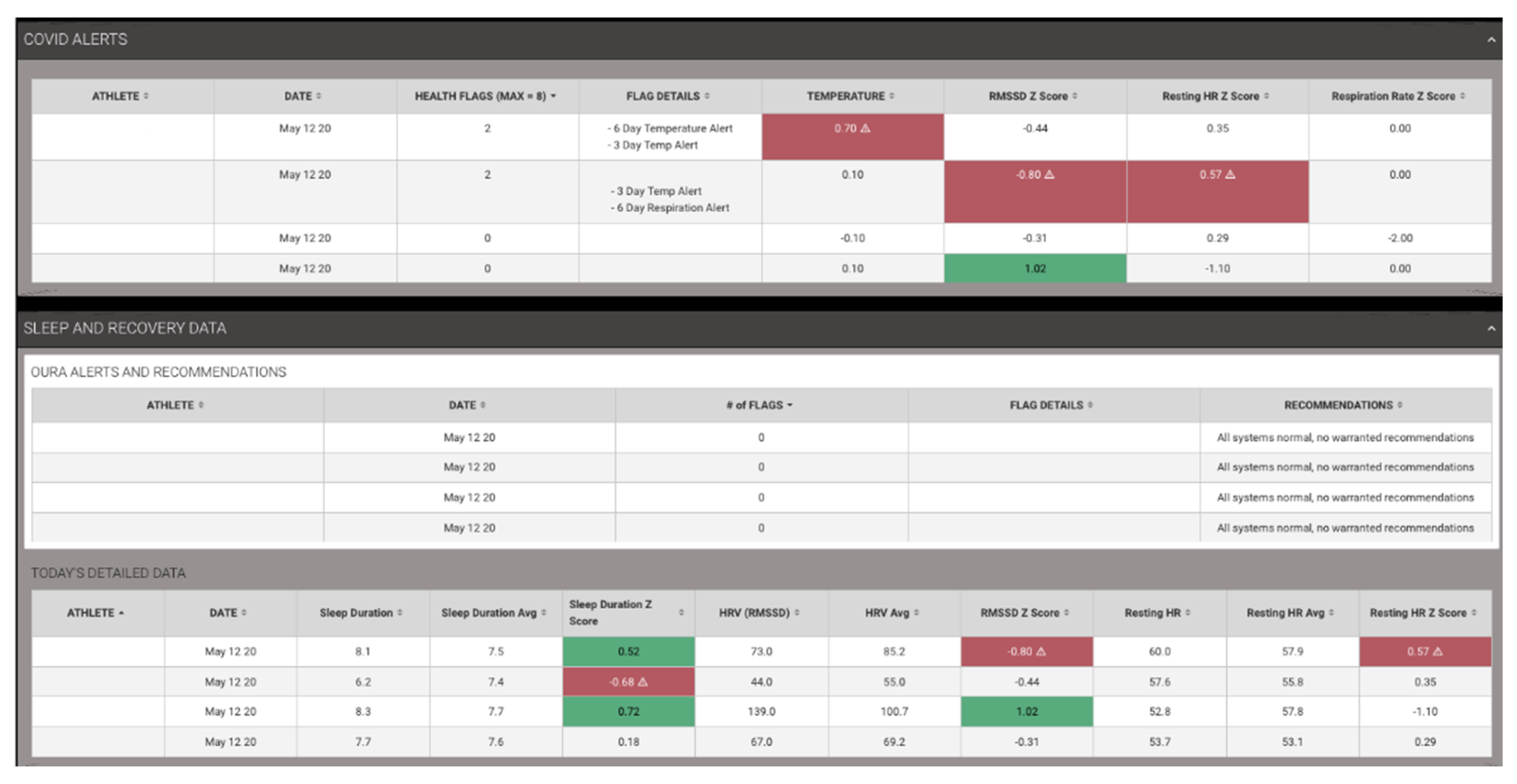
6.5. Track: COVID-19 Symptoms
6.6. Track: Sleep Behavior and Sleep Physiology
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Gallego, V.; Nishiura, H.; Sah, R.; Rodriguez-Morales, A.J. The COVID-19 outbreak and implications for the Tokyo 2020 Summer Olympic Games. Travel Med. Infect. Dis. 2020, 34, 101604. [Google Scholar] [CrossRef]
- Gilat, R.; Cole, B.J. Editorial Commentary: COVID-19, Medicine, and Sports. Arthrosc. Sports Med. Rehabil. 2020, e1–e2. [Google Scholar] [CrossRef]
- Parnell, D.; Widdop, P.; Bond, A.; Wilson, R. COVID-19, networks and sport. Manag. Sport Leis. 2020, 1–7. [Google Scholar] [CrossRef]
- Sarto, F.; Impellizzeri, F.M.; Spörri, J.; Porcelli, S.; Olmo, J.; Requena, B.; Suarez-Arrones, L.; Arundale, A.; Bilsborough, J.; Buchheit, M. Impact of potential physiological changes due to COVID-19 home confinement on athlete health protection in elite sports: A call for awareness in sports programming. Sports Med. 2020, 50, 1417–1419. [Google Scholar] [CrossRef]
- Hughes, D.; Saw, R.; Perera, N.K.P.; Mooney, M.; Wallett, A.; Cooke, J.; Coatsworth, N.; Broderick, C. The Australian Institute of Sport framework for rebooting sport in a COVID-19 environment. J. Sci. Med. Sport 2020. [Google Scholar] [CrossRef]
- Carmody, S.; Murray, A.; Borodina, M.; Gouttebarge, V.; Massey, A. When can professional sport recommence safely during the COVID-19 pandemic? Risk assessment and factors to consider. Br. J. Sports Med. 2020. [Google Scholar] [CrossRef]
- Phelan, D.; Kim, J.H.; Chung, E.H. A Game Plan for the Resumption of Sport and Exercise After Coronavirus Disease 2019 (COVID-19) Infection. JAMA Cardiol. 2020. [Google Scholar] [CrossRef]
- Jukic, I.; Calleja-González, J.; Cos, F.; Cuzzolin, F.; Olmo, J.; Terrados, N.; Njaradi, N.; Sassi, R.; Requena, B.; Milanovic, L.; et al. Strategies and Solutions for Team Sports Athletes in Isolation due to COVID-19. Sports 2020, 8, 56. [Google Scholar] [CrossRef]
- Yamey, G.; Schäferhoff, M.; Hatchett, R.; Pate, M.; Zhao, F.; McDade, K.K. Ensuring global access to COVID-19 vaccines. Lancet 2020, 395, 1405–1406. [Google Scholar] [CrossRef]
- ACHA. Considerations for Reopening Institutions of Higher Education in the COVID-19 Era; ACHA: Silver Spring, MD, USA, 2020. [Google Scholar]
- Finnoff, J. Return to Training Considerations Post-COVID-19: United States Olympic & Paralympic Committee; USOC: Colorado Springs, CO, USA, 2020. [Google Scholar]
- NSCA. COVID-19 Return to Training: Guidance on Safe. Return to Training For Athletes; NSCA: Colorado Springs, CO, USA, 2020. [Google Scholar]
- Oura. Available online: https://ouraring.com (accessed on 15 June 2020).
- Science, F. Understand the Impact of Sleep on Your Organization’s Risk and Performance. Available online: https://www.fatiguescience.com (accessed on 15 June 2020).
- Sport, F. Use Your Data to Improve Performance and Reduce Injury. Available online: https://www.fusionsport.com/smartabase-athlete-data-management-software/ (accessed on 15 June 2020).
- TeamBuildr. Available online: https://www.teambuildr.com (accessed on 15 June 2020).
- Catapult. Available online: https://www.catapultsports.com/ (accessed on 15 June 2020).
- Firstbeat. Available online: https://www.firstbeat.com/en/professional-sports/team-solutions/ (accessed on 15 June 2020).
- He, X.; Lau, E.H.Y.; Wu, P.; Deng, X.; Wang, J.; Hao, X.; Lau, Y.C.; Wong, J.Y.; Guan, Y.; Tan, X.; et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 2020, 26, 672–675. [Google Scholar] [CrossRef]
- Day, M. Covid-19: Four fifths of cases are asymptomatic, China figures indicate. BMJ 2020, m1375. [Google Scholar] [CrossRef]
- Saw, A.E.; Main, L.C.; Gastin, P.B. Monitoring athletes through self-report: Factors influencing implementation. J. Sports Sci. Med. 2015, 14, 137–146. [Google Scholar]
- Saw, A.E.; Main, L.C.; Gastin, P.B. Monitoring the athlete training response: Subjective self-reported measures trump commonly used objective measures: A systematic review. Br. J. Sports Med. 2016, 50, 281–291. [Google Scholar] [CrossRef]
- Starr, B. US Army Pushing to Develop Wearable Sensors to Detect Coronavirus Symptoms. Available online: https://www.cnn.com/2020/05/09/politics/us-army-wearable-sensors-coronavirus/index.html (accessed on 11 May 2020).
- Sands, W.A.; Kavanaugh, A.A.; Murray, S.R.; McNeal, J.R.; Jemni, M. Modern Techniques and Technologies Applied to Training and Performance Monitoring. Int. J. Sports Physiol. Perform. 2017, 12, S263–S272. [Google Scholar] [CrossRef]
- Sands, W.; Cardinale, M.; McNeal, J.; Murray, S.; Sole, C.; Reed, J.; Apostolopoulos, N.; Stone, M. Recommendations for Measurement and Management of an Elite Athlete. Sports 2019, 7, 105. [Google Scholar] [CrossRef]
- Stone, M.H.; Sands, W.A.; Pierce, K.C.; Carlock, J.; Cardinale, M.; Newton, R.U. Relationship of maximum strength to weightlifting performance. Med. Sci. Sports Exerc. 2005, 37, 1037–1043. [Google Scholar] [CrossRef]
- Case, M.J.; Knudson, D.V.; Downey, D.L. Barbell Squat Relative Strength as an Identifier for Lower Extremity Injury in Collegiate Athletes. J. Strength Cond. Res. 2020, 34, 1249–1253. [Google Scholar] [CrossRef]
- Kellmann, M.; Bertollo, M.; Bosquet, L.; Brink, M.; Coutts, A.J.; Duffield, R.; Erlacher, D.; Halson, S.L.; Hecksteden, A.; Heidari, J.; et al. Recovery and Performance in Sport: Consensus Statement. Int. J. Sports Physiol. Perform. 2018, 13, 240–245. [Google Scholar] [CrossRef]
- CDC. Available online: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html (accessed on 15 June 2020).
- Long, Q.-X.; Liu, B.-Z.; Deng, H.-J.; Wu, G.-C.; Deng, K.; Chen, Y.-K.; Liao, P.; Qiu, J.-F.; Lin, Y.; Cai, X.-F.; et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat. Med. 2020. [Google Scholar] [CrossRef]
- Berkelmans, D.M.; Dalbo, V.J.; Kean, C.O.; Milanovic, Z.; Stojanovic, E.; Stojiljkovic, N.; Scanlan, A.T. Heart Rate Monitoring in Basketball: Applications, Player Responses, and Practical Recommendations. J. Strength Cond. Res. 2018, 32, 2383–2399. [Google Scholar] [CrossRef]
- Brink, M.S.; Visscher, C.; Coutts, A.J.; Lemmink, K.A.P.M. Changes in perceived stress and recovery in overreached young elite soccer players. Scand. J. Med. Sci. Sports 2012, 22, 285–292. [Google Scholar] [CrossRef]
- Halson, S.L. Monitoring Training Load to Understand Fatigue in Athletes. Sports Med. 2014, 44, 139–147. [Google Scholar] [CrossRef]
- Plews, D.J.; Laursen, P.B.; Stanley, J.; Kilding, A.E.; Buchheit, M. Training adaptation and heart rate variability in elite endurance athletes: Opening the door to effective monitoring. Sports Med. 2013, 43, 773–781. [Google Scholar] [CrossRef]
- Bourdon, P.C.; Cardinale, M.; Murray, A.; Gastin, P.; Kellmann, M.; Varley, M.C.; Gabbett, T.J.; Coutts, A.J.; Burgess, D.J.; Gregson, W.; et al. Monitoring Athlete Training Loads: Consensus Statement. Int. J. Sports Physiol. Perform. 2017, 12, S2-161–S2-170. [Google Scholar] [CrossRef]
- Bailey, C.; Sato, K.; Alexander, R.; Chiang, C.-Y.; Stone, M.H. Isometric force production symmetry and jumping performance in collegiate athletes. J. Trainol. 2013, 2, 1–5. [Google Scholar] [CrossRef]
- Bailey, C.A.; Sato, K.; Hornsby, W.G. Predicting offensive performance in collegiate baseball players using isometric force production characteristics. In Proceedings of the ISBS-Conference Proceedings Archive, Taipei, Taiwan, 7–11 July 2013. [Google Scholar]
- Beckham, G.; Suchomel, T.; Mizuguchi, S. Force plate use in performance monitoring and sport science testing. New Stud. Athl. 2014, 29, 25–37. [Google Scholar]
- Gleason, B.H.; Bellon, C.R.; Szymanski, D.J. Practitioner-Driven Recommendations for the Professional Evaluation of the Strength and Conditioning Coach. Strength Cond. J. 2019, 42, 82–94. [Google Scholar] [CrossRef]
- Hornsby, G.; Gleason, B.; Wathen, D.; Deweese, B.; Stone, M.; Pierce, K.; Wagle, J.; Szymanski, D.J.; Stone, M.H. Servant or Service? The Problem and a Conceptual Solution. J. Intercoll. Sport 2017, 10, 228–243. [Google Scholar] [CrossRef]
- Ascensão, A.; Rebelo, A.; Oliveira, E.; Marques, F.; Pereira, L.; Magalhães, J. Biochemical impact of a soccer match—Analysis of oxidative stress and muscle damage markers throughout recovery. Clin. Biochem. 2008, 41, 841–851. [Google Scholar] [CrossRef]
- Caterisano, A.; Decker, D.; Snyder, B.; Feigenbaum, M.; Glass, R.; House, P.; Sharp, C.; Waller, M.; Witherspoon, Z. CSCCa and NSCA Joint Consensus Guidelines for Transition Periods: Safe Return to Training Following Inactivity. Strength Cond. J. 2019, 41, 1–23. [Google Scholar] [CrossRef]
- Vestberg, T.; Gustafson, R.; Maurex, L.; Ingvar, M.; Petrovic, P. Executive functions predict the success of top-soccer players. PLoS ONE 2012, 7, e34731. [Google Scholar] [CrossRef]
- Fullagar, H.H.; Skorski, S.; Duffield, R.; Hammes, D.; Coutts, A.J.; Meyer, T. Sleep and athletic performance: The effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015, 45, 161–186. [Google Scholar] [CrossRef]
- Boneva, R.S.; Decker, M.J.; Maloney, E.M.; Lin, J.-M.; Jones, J.F.; Helgason, H.G.; Heim, C.M.; Rye, D.B.; Reeves, W.C. Higher heart rate and reduced heart rate variability persist during sleep in chronic fatigue syndrome: A population-based study. Auton. Neurosci. 2007, 137, 94–101. [Google Scholar] [CrossRef]
- Hall, M.; Vasko, R.; Buysse, D.; Ombao, H.; Chen, Q.; Cashmere, J.D.; Kupfer, D.; Thayer, J.F. Acute Stress Affects Heart Rate Variability During Sleep. Psychosom. Med. 2004, 66, 56–62. [Google Scholar] [CrossRef]
- Zhang, L.; Wu, H.; Zhang, X.; Wei, X.; Hou, F.; Ma, Y. Sleep heart rate variability assists the automatic prediction of long-term cardiovascular outcomes. Sleep Med. 2020, 67, 217–224. [Google Scholar] [CrossRef]
- Al-Khalidi, F.Q.; Saatchi, R.; Burke, D.; Elphick, H.; Tan, S. Respiration rate monitoring methods: A review. Pediatr. Pulmonol. 2011, 46, 523–529. [Google Scholar] [CrossRef]
- Jongstra, S.; Wijsman, L.W.; Cachucho, R.; Hoevenaar-Blom, M.P.; Mooijaart, S.P.; Richard, E. Cognitive Testing in People at Increased Risk of Dementia Using a Smartphone App: The iVitality Proof-of-Principle Study. JMIR Mhealth Uhealth 2017, 5, e68. [Google Scholar] [CrossRef]
- Kraska, J.M.; Ramsey, M.W.; Haff, G.G.; Fethke, N.; Sands, W.A.; Stone, M.E.; Stone, M.H. Relationship Between Strength Characteristics and Unweighted and Weighted Vertical Jump Height. Int. J. Sports Physiol. Perform. 2009, 4, 461–473. [Google Scholar] [CrossRef]
- Suchomel, T.J.; Nimphius, S.; Bellon, C.R.; Stone, M.H. The importance of muscular strength: Training considerations. Sports Med. 2018, 48, 765–785. [Google Scholar] [CrossRef]
- Dos’Santos, T.; Thomas, C.; Comfort, P.; McMahon, J.J.; Jones, A.P. Relationships between Isometric Force-Time Characteristics and Dynamic Performance. Sports 2017, 5, 68. [Google Scholar] [CrossRef]
- Sands, W.; McNeal, J. Predicting Athlete Preparation and Performance: A Theoretical Perspective. J. Sport Behav. 2000, 23, 289–310. [Google Scholar]
- Stone, M.H.; O’Bryant, H.S.; Hornsby, G.; Cunanan, A.; Mizuguchi, S.; Suarez, D.G.; South, M.; Marsh, D.; Haff, G.G.; Ramsey, M.W. Using the isometric mid-thigh pull in the monitoring of weighlifters: 25+ years of experience. Proform. Strength Cond. 2019, 54, 19–26. [Google Scholar]
- Mayberry, J.; Mullen, S.; Murayama, S. What Can a Jump Tell Us About Elbow Injuries in Professional Baseball Pitchers? Am. J. Sport Med. 2020, 48, 1220–1225. [Google Scholar] [CrossRef]
- Nimphius, S.; McBride, J.M.; Rice, P.E.; Goodman-Capps, C.L.; Capps, C.R. Comparison of Quadriceps and Hamstring Muscle Activity during an Isometric Squat between Strength-Matched Men and Women. J. Sports Sci. Med. 2019, 18, 101–108. [Google Scholar]
- Wing, C.; Bishop, C. Hamstring Strain Injuries: Incidence, Mechanisms, Risk Factors, and Training Recommendations. Strength Cond. J. 2020, 42, 40–57. [Google Scholar]
- Fry, A.C.; Kraemer, W.J.; van Borselen, F.; Lynch, J.M.; Marist, J.L.; Roy, E.P.; Triplett, N.T.; Knuttgen, H.G. Performance decrements with high-intensity resistance exercise overtraining. Med. Sci. Sport Exerc. 1994, 26, 1165–1173. [Google Scholar]
- Moore, C.A.; Fry, A.C. Nonfunctional overreaching during off-season training for skill position players in collegiate American football. J. Strength Cond. Res. 2007, 21, 793–800. [Google Scholar]
- Gabbett, T.J.; Whyte, D.G.; Hartwig, T.B.; Wescombe, H.; Naughton, G.A. The Relationship Between Workloads, Physical Performance, Injury and Illness in Adolescent Male Football Players. Sports Med. 2014, 44, 989–1003. [Google Scholar] [CrossRef]
- Rhea, M.R.; Alderman, B.L. A Meta-Analysis of Periodized versus Nonperiodized Strength and Power Training Programs. Res. Q. Exerc. Sport 2004, 75, 413–422. [Google Scholar] [CrossRef]
- Cunanan, A.J.; DeWeese, B.H.; Wagle, J.P.; Carroll, K.M.; Sausaman, R.; Hornsby, W.G.; Haff, G.G.; Triplett, N.T.; Pierce, K.C.; Stone, M.H. The general adaptation syndrome: A foundation for the concept of periodization. Sports Med. 2018, 48, 787–797. [Google Scholar] [CrossRef]
- Buller, M.J.; Tharion, W.J.; Cheuvront, S.N.; Montain, S.J.; Kenefick, R.W.; Castellani, J.; Latzka, W.A.; Roberts, W.S.; Richter, M.; Jenkins, O.C. Estimation of human core temperature from sequential heart rate observations. Physiol. Meas. 2013, 34, 781. [Google Scholar] [CrossRef]
- Buller, M.J.; Tharion, W.J.; Duhamel, C.M.; Yokota, M. Real-time core body temperature estimation from heart rate for first responders wearing different levels of personal protective equipment. Ergonomics 2015, 58, 1830–1841. [Google Scholar] [CrossRef]
- Buller, M.J.; Welles, A.P.; Friedl, K.E. Wearable physiological monitoring for human thermal-work strain optimization. J. Appl. Physiol. 2018, 124, 432–441. [Google Scholar] [CrossRef]
- Gamage, P.J.; Fortington, L.V.; Finch, C.F. Epidemiology of exertional heat illnesses in organised sports: A systematic review. J. Sci. Med. Sport 2020. [Google Scholar] [CrossRef]
- Nassi, A.; Ferrauti, A.; Meyer, T.; Pfeiffer, M.; Kellmann, M. Development of two short measures for recovery and stress in sport. Eur. J. Sport Sci. 2017, 17, 894–903. [Google Scholar] [CrossRef]
- Sayre, M. WVU Rockefeller Neuroscience Institute and Oura Health Unveil Study to Predict the Outbreak of COVID-19 in Healthcare Professionals. WVU Today, 8 April 2020. [Google Scholar]
- Patringenaru, I. Creating an Early Alert System for COVID-19; UC San Diego: San Diego, CA, USA, 2020. [Google Scholar]
- Bonnar, D.; Bartel, K.; Kakoschke, N.; Lang, C. Sleep interventions designed to improve athletic performance and recovery: A systematic review of current approaches. Sports Med. 2018, 48, 683–703. [Google Scholar] [CrossRef]
- Fowler, P.M.; Knez, W.; Crowcroft, S.; Mendham, A.E.; Miller, J.; Sargent, C.; Halson, S.; Duffield, R. Greater effect of east vs. west travel on jet-lag, sleep and team-sport performance. Med. Sci. Sports Exerc. 2017. [Google Scholar] [CrossRef]
- Fullagar, H.H.; Duffield, R.; Skorski, S.; Coutts, A.J.; Julian, R.; Meyer, T. Sleep and Recovery in Team Sport: Current Sleep-Related Issues Facing Professional Team-Sport Athletes. Int. J. Sports Physiol. Perform. 2015, 10, 950–957. [Google Scholar] [CrossRef]
- Grandou, C.; Wallace, L.; Fullagar, H.H.K.; Duffield, R.; Burley, S. The Effects of Sleep Loss on Military Physical Performance. Sports Med. 2019, 49, 1159–1172. [Google Scholar] [CrossRef]
- Mah, C.D.; Mah, K.E.; Kezirian, E.J.; Dement, W.C. The Effects of Sleep Extension on the Athletic Performance of Collegiate Basketball Players. Sleep 2011, 34, 943–950. [Google Scholar] [CrossRef]
- Milewski, M.D.; Skaggs, D.L.; Bishop, G.A.; Pace, J.L.; Ibrahim, D.A.; Wren, T.A.L.; Barzdukas, A. Chronic Lack of Sleep is Associated With Increased Sports Injuries in Adolescent Athletes. J. Pediatr. Orthop. 2014, 34, 129–133. [Google Scholar] [CrossRef]
- Oliver, S.J.; Costa, R.J.S.; Laing, S.J.; Bilzon, J.L.J.; Walsh, N.P. One night of sleep deprivation decreases treadmill endurance performance. Eur. J. Appl. Physiol. 2009, 107, 155–161. [Google Scholar] [CrossRef]
- Ritland, B.M.; Simonelli, G.; Gentili, R.J.; Smith, J.C.; He, X.; Mantua, J.; Balkin, T.J.; Hatfield, B.D. Effects of sleep extension on cognitive/motor performance and motivation in military tactical athletes. Sleep Med. 2019, 58, 48–55. [Google Scholar] [CrossRef]
- Steenland, K.; Deddens, J.A. Effect of Travel and Rest on Performance of Professional Basketball Players. Sleep 1997, 20, 366–369. [Google Scholar] [CrossRef][Green Version]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015. [Google Scholar] [CrossRef]
- Reid, C.; Stewart, E.; Thorne, G. Multidisciplinary Sport Science Teams in Elite Sport: Comprehensive Servicing or Conflict and Confusion? Sport Psychol. 2004, 18, 204–217. [Google Scholar] [CrossRef]



| Data Type | Purpose | Form Factor | Frequency of Data | Description of Data |
|---|---|---|---|---|
| Symptom Tracking | COVID-19 Tracking | Smartphone App, Spreadsheet, Pen/Paper | 1–2× daily | Subjective symptoms following CDC guidelines Currently 18 Yes/No questions |
| Viral Load Testing | COVID-19 Tracking | Nasal Swab | Every 2 weeks, or onset of symptoms | Quantitative assessment of COVID-19 diagnosis |
| Antibody Testing | COVID-19 Tracking | Blood (venous or finger prick) | Every 2 weeks | Quantitative assessment of IgM and IgG antibody time course |
| Health/Wellness Tracking | Dual Purpose | Smartphone App, Spreadsheet, Pen/Paper | 1–2× daily | Subjective stress and recovery assessments Generally, 3–10 questions using Likert scales |
| Sleep and Sleep Physiology | Dual Purpose | Smart Ring | Pervasive during sleep | Objective measures of sleep quantity, quality, heart rate, heart rate variability, respiration rate, and temperature |
| Cognitive Testing | Dual Purpose | Smartphone App | 1–2× daily | Objective measures of reaction time, working memory, and impulsivity |
| Training Load | Performance Monitoring | Wearable Technology, Smartphone App, Spreadsheet, Pen/Paper | Per training session, weekly to monthly for performance assessments | External (motion, force plates) and internal (heart rate) workload measures during training |
| Phase | Challenge | Main Objectives | Data Acquired |
|---|---|---|---|
| I: Quarantine | No access to facilities, staff | Deploy and monitor training plans Monitor physical and mental health and wellness |
|
| II: Return to facility | Limited access to facilities, first concern for exposure to COVID-19 | Screen athletes for previous exposure Assess physical condition to begin planning to return to training |
|
| III: Return to S&C training | Limited control of chronic training workload during Phase I Moderate level of interaction between athletes and staff raising risk of virus spread | Ramp athletes back into S&C safely Keep risk of virus spread low |
|
| IV: Return to practice | Managing training loads in potentially compressed timeframe in preparation for competition High level of interaction between athletes | Keep athletes safe from acute heat and musculoskeletal injury during practice Keep risk of virus spread low |
|
| V: Return to competition | Highest risk factor for exposure to virus due to travel, interacting with athletes from other teams/cities | Optimize player performance Reduce risk of virus exposure |
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hagen, J.; Stone, J.D.; Hornsby, W.G.; Stephenson, M.; Mangine, R.; Joseph, M.; Galster, S. COVID-19 Surveillance and Competition in Sport: Utilizing Sport Science to Protect Athletes and Staff during and after the Pandemic. J. Funct. Morphol. Kinesiol. 2020, 5, 69. https://doi.org/10.3390/jfmk5030069
Hagen J, Stone JD, Hornsby WG, Stephenson M, Mangine R, Joseph M, Galster S. COVID-19 Surveillance and Competition in Sport: Utilizing Sport Science to Protect Athletes and Staff during and after the Pandemic. Journal of Functional Morphology and Kinesiology. 2020; 5(3):69. https://doi.org/10.3390/jfmk5030069
Chicago/Turabian StyleHagen, Joshua, Jason D. Stone, W. Guy Hornsby, Mark Stephenson, Robert Mangine, Michael Joseph, and Scott Galster. 2020. "COVID-19 Surveillance and Competition in Sport: Utilizing Sport Science to Protect Athletes and Staff during and after the Pandemic" Journal of Functional Morphology and Kinesiology 5, no. 3: 69. https://doi.org/10.3390/jfmk5030069
APA StyleHagen, J., Stone, J. D., Hornsby, W. G., Stephenson, M., Mangine, R., Joseph, M., & Galster, S. (2020). COVID-19 Surveillance and Competition in Sport: Utilizing Sport Science to Protect Athletes and Staff during and after the Pandemic. Journal of Functional Morphology and Kinesiology, 5(3), 69. https://doi.org/10.3390/jfmk5030069







