Reliability of an Integrated Inertial Sensor for the Continuous Measurement of Active Cervical Range of Motion in a Group of Younger and Elderly Individuals
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measurement Instruments
2.3. Procedure
2.4. Data Post-Processing and Statistical Analysis
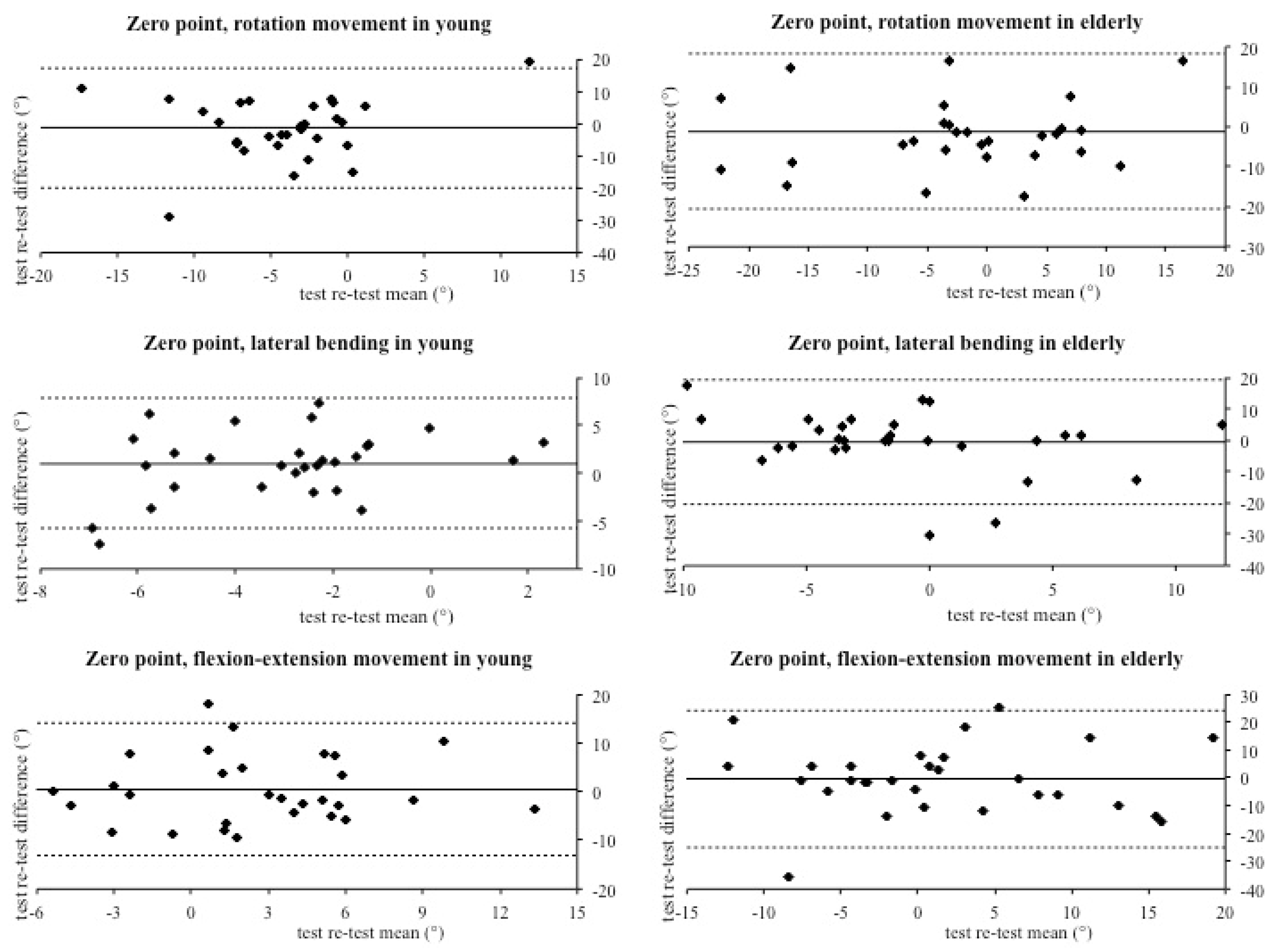
- Zero point (ZP): the difference between the start position and the ending position;
- Maximal range of motion (ROM-max): the higher range of motion value among the three repetitions;
- Mean range of motion (ROM-med): the mean of the three ranges of motion;
- Absolute maximum excursion (Max-abs): the higher maximum excursion value from the starting position (right rotation, right lateral bending, and flexion);
- Mean maximum excursion (Max-med): the mean of the three maximum excursion values from the starting position (right rotation, right lateral bending, and flexion);
- Absolute minimum excursion (Min-abs): the higher maximum excursion value from the starting position (left rotation, left lateral bending, and extension);
- Mean minimum excursion (Min-med): the mean of the three maximum excursion values from the starting position (left rotation, left lateral bending, and extension);
3. Results
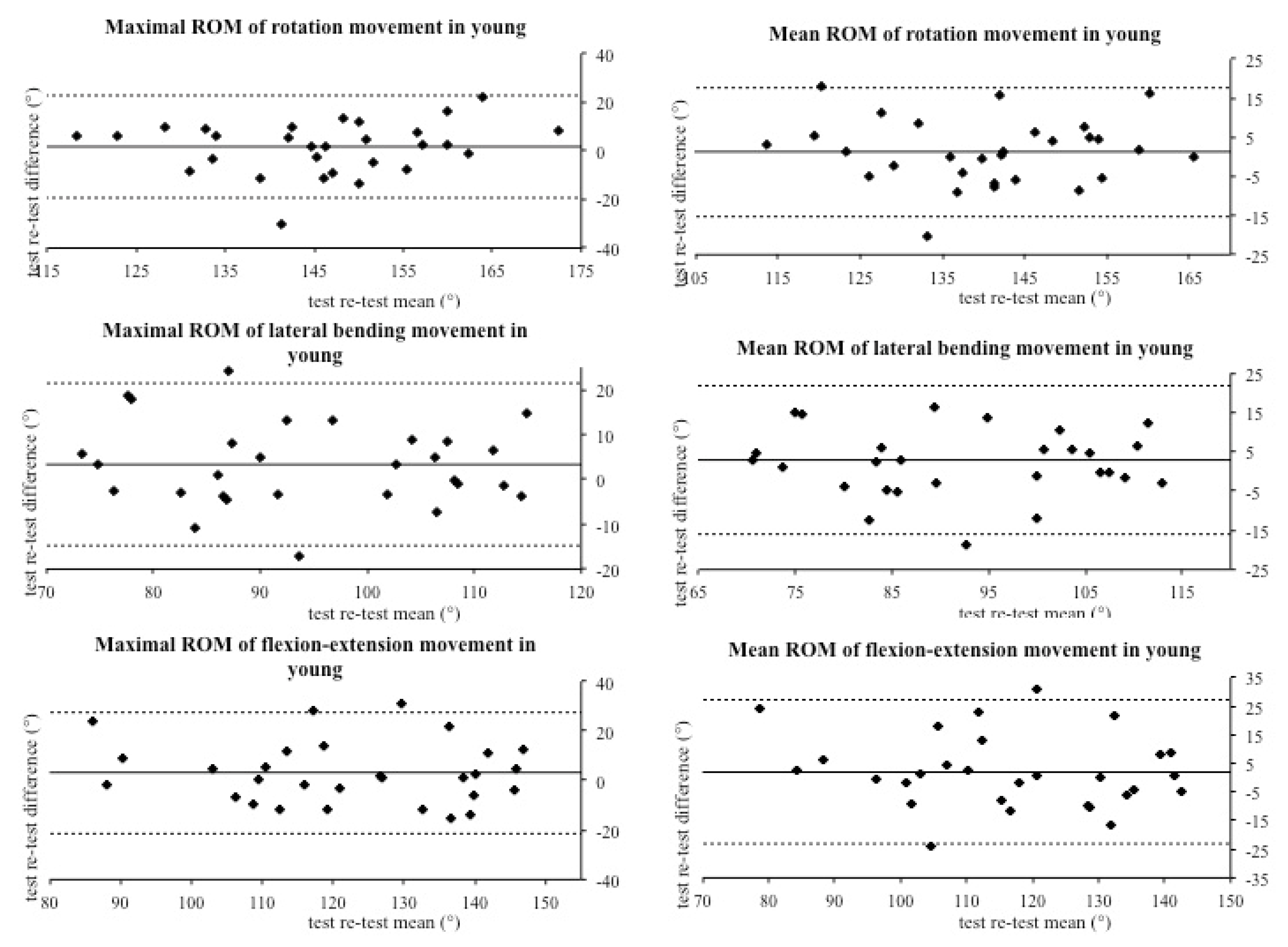
3.1. Test Re–Test Reliability in Young Subjects
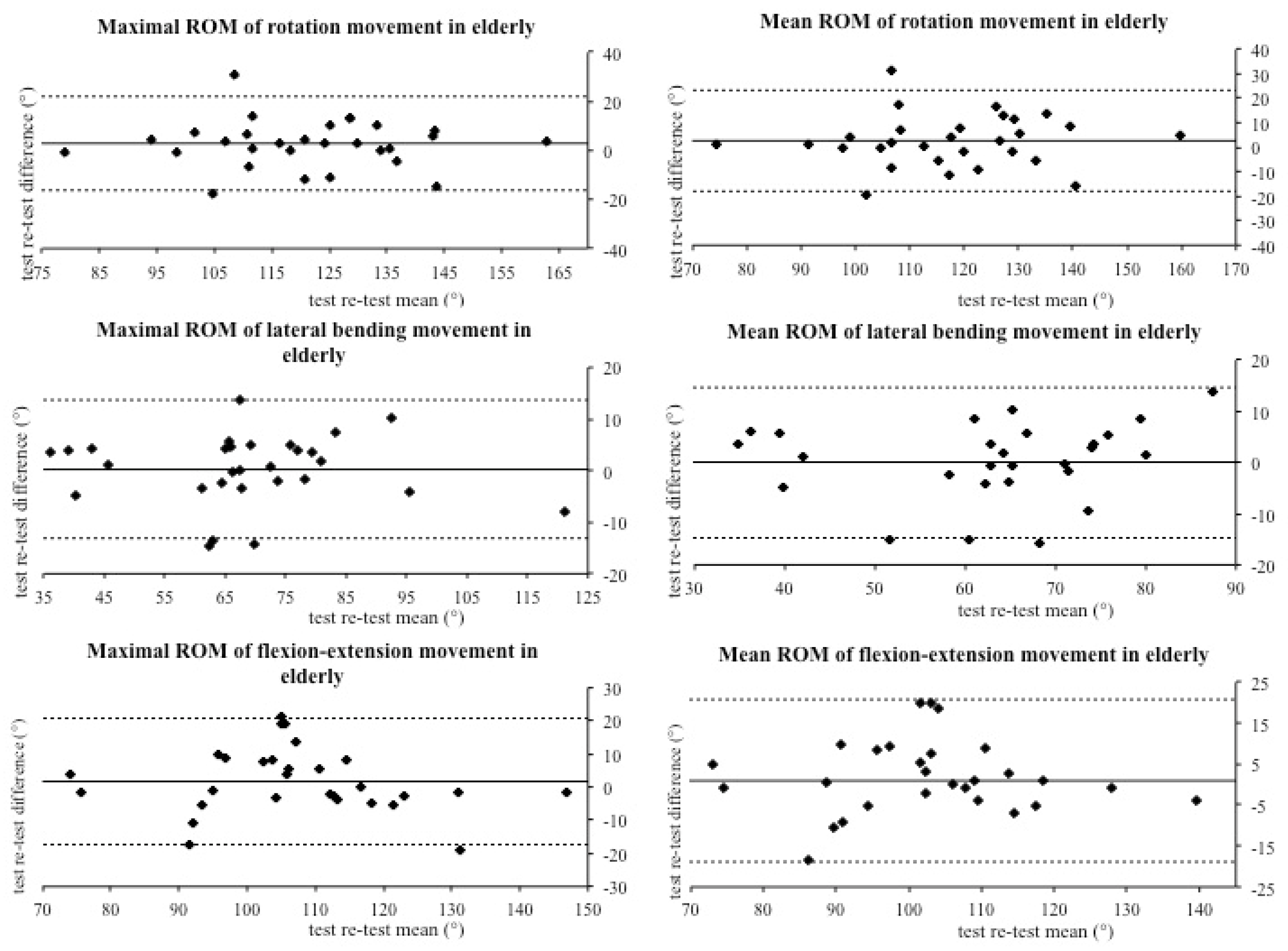
3.2. Test Re–Test Reliability in Elderly Subjects
4. Discussion
4.1. Limitations
4.2. Future Investigations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Safiri, S.; Kolahi, A.A.; Hoy, D.; Buchbinder, R.; Mansournia, M.A.; Bettampadi, D.; Ashrafi-Asgarabad, A.; Almasi-Hashiani, A.; Smith, E.; Sepidarkish, M.; et al. Global, regional, and national burden of neck pain in the general population, 1990–2017: Systematic analysis of the Global Burden of Disease Study 2017. BMJ 2020, 368, m791. [Google Scholar] [CrossRef] [PubMed]
- Paladini, A.; Fusco, M.; Coaccioli, S.; Skaper, S.D.; Varrassi, G. Chronic Pain in the Elderly: The Case for New Therapeutic Strategies. Pain Phys. 2015, 18, E863–E876. [Google Scholar]
- Hirase, T.; Okubo, Y.; Sturnieks, D.L.; Lord, S.R. Pain Is Associated With Poor Balance in Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. J. Am. Med. Dir. Assoc. 2020, 21, 597–603.e8. [Google Scholar] [CrossRef]
- Uthaikhup, S.; Jull, G.; Sungkarat, S.; Treleaven, J. The influence of neck pain on sensorimotor function in the elderly. Arch. Gerontol. Geriatr. 2012, 55, 667–672. [Google Scholar] [CrossRef]
- Cohen, S.P. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin. Proc. 2015, 90, 284–299. [Google Scholar] [CrossRef] [PubMed]
- Theobald, P.S.; Jones, M.D.; Williams, J.M. Do inertial sensors represent a viable method to reliably measure cervical spine range of motion? Man. Ther. 2012, 17, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Antonaci, F.; Ghirmai, S.; Bono, G.; Nappi, G. Current methods for cervical spine movement evaluation: A review. Clin. Exp. Rheumatol. 2000, 18, S45–S52. [Google Scholar]
- Cleland, J.A.; Childs, J.D.; Fritz, J.M.; Whitman, J.M. Interrater reliability of the history and physical examination in patients with mechanical neck pain. Arch. Phys. Med. Rehabil. 2006, 87, 1388–1395. [Google Scholar] [CrossRef]
- Kim, H.; Shin, S.H.; Kim, J.K.; Park, Y.J.; Oh, H.S.; Park, Y.B. Cervical coupling motion characteristics in healthy people using a wireless inertial measurement unit. Evid. Based Complement. Alternat. Med. 2013, 2013, 570428. [Google Scholar] [CrossRef]
- Saber-Sheikh, K.; Bryant, E.C.; Glazzard, C.; Hamel, A.; Lee, R.Y. Feasibility of using inertial sensors to assess human movement. Man. Ther. 2010, 15, 122–125. [Google Scholar] [CrossRef]
- Chambers, R.; Gabbett, T.J.; Cole, M.H.; Beard, A. The Use of Wearable Microsensors to Quantify Sport-Specific Movements. Sports Med. 2015, 45, 1065–1081. [Google Scholar] [CrossRef] [PubMed]
- Jasiewicz, J.M.; Treleaven, J.; Condie, P.; Jull, G. Wireless orientation sensors: Their suitability to measure head movement for neck pain assessment. Man. Ther. 2007, 12, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Kubas, C.; Chen, Y.W.; Echeverri, S.; McCann, S.L.; Denhoed, M.J.; Walker, C.J.; Kennedy, C.N.; Reid, W.D. Reliability and Validity of Cervical Range of Motion and Muscle Strength Testing. J. Strength Cond. Res. 2017, 31, 1087–1096. [Google Scholar] [CrossRef] [PubMed]
- Bujang, M.; Baharum, N. A simplified guide to determination of sample size requirements for estimating the value of intraclass correlation coefficient: A review. Arch. Orofac. Sci. 2017, 12, 1–11. [Google Scholar]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Kopinska, A.; Harris, L.R. Spatial representation in body coordinates: Evidence from errors in remembering positions of visual and auditory targets after active eye, head, and body movements. Can. J. Exp. Psychol. 2003, 57, 23–37. [Google Scholar] [CrossRef]
- Basteris, A.; Pedler, A.; Sterling, M. Evaluating the neck joint position sense error with a standard computer and a webcam. Man. Ther. 2016, 26, 231–234. [Google Scholar] [CrossRef]
- Michiels, S.; De Hertogh, W.; Truijen, S.; November, D.; Wuyts, F.; Van de Heyning, P. The assessment of cervical sensory motor control: A systematic review focusing on measuring methods and their clinimetric characteristics. Gait Posture 2013, 38, 1–7. [Google Scholar] [CrossRef]
- Jonsson, A.; Rasmussen-Barr, E. Intra- and inter-rater reliability of movement and palpation tests in patients with neck pain: A systematic review. Physiother. Theory Pract. 2018, 34, 165–180. [Google Scholar] [CrossRef]
- Hubble, R.P.; Naughton, G.A.; Silburn, P.A.; Cole, M.H. Wearable sensor use for assessing standing balance and walking stability in people with Parkinson’s disease: A systematic review. PLoS ONE 2015, 10, e0123705. [Google Scholar] [CrossRef] [PubMed]

| N. Subjects | Weight (kg) | Height (m) | BMI (kg/m2) | Age (Years) |
|---|---|---|---|---|
| 30 young (15 M, 15 F) | 67.90 ± 14.66 | 1.74 ± 8.30 | 22.17 ± 3.08 | 22.43 ± 1.69 |
| 30 elderly (15 M, 15 F) | 76.23 ± 15.79 | 1.70 ± 10.23 | 26.30 ± 3.44 | 68.13 ± 2.80 |
| Variables | Test (°) | Retest (°) | Δ% | ICC (CI 95%) | Δ° (ULA-LLA 95%) |
|---|---|---|---|---|---|
| ZP Rotation | −4.84 ± 7.73 | −3.42 ± 6.24 | −29.27 | 0.1 (−0.27; 0.44) | −1.4 (17.13; −19.96) |
| ROM-max Rotation | 146.72 ± 14.44 | 145.26 ± 13.05 | −0.99 | 0.71 (0.47; 0.85) | 1.46 (22.38; −19.47) |
| ROM-med Rotation | 141.02 ± 13.69 | 139.83 ± 13.82 | −0.84 | 0.82 (0.66; 0.91) | 1.19 (17.65; −15.27) |
| Max-abs Rotation | 79.23 ± 8.78 | 77.75 ± 7.94 | −1.87 | 0.71 (0.47; 0.85) | 1.48 (14.23; −11.27) |
| Max-med Rotation | 75.34 ± 8.02 | 74.36 ± 8.21 | −1.3 | 0.78 (0.59; 0.89) | 0.98 (11.75; −9.79) |
| Min-abs Rotation | −68.59 ± 7.55 | −68.87 ± 8.05 | −0.4 | 0.54 (0.22; 0.75) | 0.28 (15.18; −14.62) |
| Min-med Rotation | −65.69 ± 6.95 | −65.48 ± 7.76 | −0.32 | 0.66 (0.39; 0.83) | −0.21 (11.92; −12.34) |
| ZP Lat-bending | −2.54 ± 3.33 | −3.52 ± 2.39 | 38.54 | 0.29 (−0.08; 0.59) | 0.98 (7.79; −5.83) |
| ROM-max Lat-bend | 96.28 ± 13.5 | 93.01 ± 14.3 | −3.4 | 0.79 (0.6; 0.9) | 3.27 (21.45; −14.91) |
| ROM-med Lat-bend | 93.53 ± 13.63 | 90.64 ± 14.56 | −3.09 | 0.78 (0.58; 0.89) | 2.89 (21.77; −16) |
| Max-abs Lat-bend | 49.96 ± 7.27 | 48.09 ± 7.32 | −3.75 | 0.8 (0.62; 0.9) | 1.87 (11.1; −7.35) |
| Max-med Lat-bend | 48.42 ± 7.25 | 46.33 ± 7.35 | −4.33 | 0.77 (0.56; 0.88) | 2.10 (12.16; −7.97) |
| Min-abs Lat-bend | −47.04 ± 7.42 | −46.06 ± 7.76 | −2.07 | 0.75 (0.54; 0.88) | −0.98 (9.77; −11.72) |
| Min-med Lat-bend | −45.11 ± 7.67 | −44.32 ± 8.12 | −1.75 | 0.74 (0.52; 0.87) | −0.79 (10.57; −12.15) |
| ZP Flex-ext | 2.77 ± 5.65 | 2.37 ± 5.48 | −14.53 | 0.22 (−0.15; 0.54) | 0.4 (14.05; −13.25) |
| ROM-max Flex-ext | 123.82 ± 18.1 | 120.83 ± 19.35 | −2.42 | 0.79 (0.6; 0.9) | 2.99 (27.44; −21.46) |
| ROM-med Flex-ext | 117.55 ± 17.83 | 115.64 ± 19.88 | −1.62 | 0.78 (0.59; 0.89) | 1.19 (26.89; −23.07) |
| Max-abs Flex-ext | 57.79 ± 10.37 | 54.61 ± 10.63 | −5.5 | 0.78 (0.58; 0.89) | 3.18 (17.2; −10.84) |
| Max-med Flex-ext | 54.22 ± 9.98 | 51.77 ± 11.26 | −4.52 | 0.78 (0.58; 0.89) | 2.45 (16.8; −11.89) |
| Min-abs Flex-ext | −67.07 ± 12.91 | −67.03 ± 14.23 | −0.06 | 0.74 (0.51; 0.87) | −0.04 (19.77; −19.84) |
| Min-med Flex-ext | −63.32 ± 13.21 | −63.87 ± 14.19 | 0.86 | 0.76 (0.54; 0.88) | 0.54 (19.77; −18.68) |
| Variables | Test (°) | Retest (°) | Δ% | ICC (CI 95%) | Δ° (ULA-LLA 95%) |
|---|---|---|---|---|---|
| ZP Rotation | −2.96 ± 10.98 | −1.76 ± 10.7 | −40.6 | 0.59 (0.3; 0.79) | −1.2 (18.31; −20.71) |
| ROM-max Rotation | 122.25 ± 18.23 | 119.61 ± 18.31 | −2.16 | 0.87 (0.74; 0.93) | 2.64 (21.74; −16.47) |
| ROM-med Rotation | 118.71 ± 18.27 | 116.16 ± 17.73 | −2.15 | 0.84 (0.69; 0.92) | 2.55 (23.05; −17.95) |
| Max-abs Rotation | 68.63 ± 12.06 | 67.36 ± 10.99 | −1.84 | 0.7 (0.45; 0.85) | 1.27 (19.23; −16.69) |
| Max-med Rotation | 66.31 ± 12.03 | 64.85 ± 10.19 | −2.21 | 0.7 (0.45; 0.85) | 1.47 (18.84; −15.91) |
| Min-abs Rotation | −54.58 ± 10.43 | −53.6 ± 9.61 | −1.79 | 0.7 (0.46; 0.85) | −0.98 (14.51; −16.46) |
| Min-med Rotation | −52.4 ± 10.31 | −51.31 ± 9.52 | −2.07 | 0.65 (0.37; 0.82) | −1.09 (15.61; −17.78) |
| ZP Lat-bending | −1.36 ± 6 | −0.79 ± 8.16 | −41.77 | 0 (−0.36; 0.36) | −0.57 (19.26; −20.4) |
| ROM-max Lat-bend | 68.67 ± 17.98 | 68.46 ± 18.29 | −0.3 | 0.93 (0.87; 0.97) | 0.2 (13.54; −13.13) |
| ROM-med Lat-bend | 65.51 ± 17.71 | 65.64 ± 18.02 | 0.21 | 0.92 (0.83; 0.96) | −0.14 (14.6; −14.87) |
| Max-abs Lat-bend | 37.7 ± 10.23 | 36.47 ± 10.99 | −3.27 | 0.89 (0.79; 0.95) | 1.23 (11.14; −8.68) |
| Max-med Lat-bend | 35.67 ± 9.88 | 34.33 ± 10.74 | −3.78 | 0.89 (0.78; 0.95) | 1.35 (11.12; −8.42) |
| Min-abs Lat-bend | −31.47 ± 9.52 | −33.14 ± 9.54 | 5.31 | 0.8 (0.62; 0.9) | 1.67 (13.81; −10.47) |
| Min-med Lat-bend | −29.83 ± 9.47 | −31.32 ± 9.31 | 4.97 | 0.79 (0.61; 0.9) | 1.48 (13.64; −10.68) |
| ZP Flex-ext | 1.23 ± 10.3 | 1.74 ± 10.44 | 41.59 | 0.28 (−0.09; 0.58) | −0.51 (24.06; −25.09) |
| ROM-max Flex-ext | 108.11 ± 15.48 | 106.43 ± 16.99 | −1.56 | 0.83 (0.67; 0.92) | 1.69 (20.73; −17.36) |
| ROM-med Flex-ext | 103.83 ± 14.93 | 102.9 ± 16.17 | −0.89 | 0.8 (0.62; 0.9) | 0.92 (20.77; −18.86) |
| Max-abs Flex-ext | 44.58 ± 9.98 | 47.33 ± 9.93 | 6.17 | 0.42 (0.07; 0.68) | −2.75 (18.56; −24.07) |
| Max-med Flex-ext | 42.54 ± 10.33 | 45.24 ± 9.81 | 6.33 | 0.37 (0.01; 0.65) | −2.69 (19.66; −25.04) |
| Min-abs Flex-ext | −64.29 ± 14.31 | −60.39 ± 16.83 | −6.08 | 0.72 (0.48; 0.86) | −3.91 (19.61; −27.42) |
| Min-med Flex-ext | −61.28 ± 14.2 | −57.66 ± 16.2 | −5.9 | 0.71 (0.47; 0.85) | −3.62 (19.63; −26.86) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gobbo, S.; Vendramin, B.; Roma, E.; Duregon, F.; Bocalini, D.S.; Rica, R.L.; Di Blasio, A.; Cugusi, L.; Bergamo, M.; Cruz-Díaz, D.; et al. Reliability of an Integrated Inertial Sensor for the Continuous Measurement of Active Cervical Range of Motion in a Group of Younger and Elderly Individuals. J. Funct. Morphol. Kinesiol. 2020, 5, 58. https://doi.org/10.3390/jfmk5030058
Gobbo S, Vendramin B, Roma E, Duregon F, Bocalini DS, Rica RL, Di Blasio A, Cugusi L, Bergamo M, Cruz-Díaz D, et al. Reliability of an Integrated Inertial Sensor for the Continuous Measurement of Active Cervical Range of Motion in a Group of Younger and Elderly Individuals. Journal of Functional Morphology and Kinesiology. 2020; 5(3):58. https://doi.org/10.3390/jfmk5030058
Chicago/Turabian StyleGobbo, Stefano, Barbara Vendramin, Enrico Roma, Federica Duregon, Danilo Sales Bocalini, Roberta Luksevicius Rica, Andrea Di Blasio, Lucia Cugusi, Manuele Bergamo, David Cruz-Díaz, and et al. 2020. "Reliability of an Integrated Inertial Sensor for the Continuous Measurement of Active Cervical Range of Motion in a Group of Younger and Elderly Individuals" Journal of Functional Morphology and Kinesiology 5, no. 3: 58. https://doi.org/10.3390/jfmk5030058
APA StyleGobbo, S., Vendramin, B., Roma, E., Duregon, F., Bocalini, D. S., Rica, R. L., Di Blasio, A., Cugusi, L., Bergamo, M., Cruz-Díaz, D., Lima Alberton, C., Bullo, V., Ermolao, A., & Bergamin, M. (2020). Reliability of an Integrated Inertial Sensor for the Continuous Measurement of Active Cervical Range of Motion in a Group of Younger and Elderly Individuals. Journal of Functional Morphology and Kinesiology, 5(3), 58. https://doi.org/10.3390/jfmk5030058







